Abstract
Background
The magnitude of, and factors associated with, prolonged delay in seeking medical care in patients with acute myocardial infarction has been well described. It is unknown, however, what the extent of, and factors associated with, prehospital delay are in patients hospitalized with acute heart failure.
Purpose
The purpose of this study was to examine patterns of prehospital delay, and factors associated with delay in seeking medical care, in patients hospitalized with acute heart failure at all 11 medical centers in the Worcester, MA, metropolitan area.
Methods
The medical records of 2,587 greater Worcester residents with decompensated heart failure who were hospitalized in 2000 were reviewed for the collection of information about prehospital delay and demographic and clinical factors associated with extent of delay.
Results
Information about acute symptom onset and duration of delay in seeking medical care was available in only 44% of the hospital charts of patients with heart failure. The average delay time was 13.3 hours while the median was 2.0 hours. Male sex, multiple presenting symptoms, absence of a history of heart failure, and seeking medical care between midnight and 6 a.m. were associated with prolonged prehospital delay.
Conclusions
The results of this study in residents of a large New England metropolitan area suggest that patients hospitalized with acute heart failure exhibit considerable delays in seeking medical care. Several demographic and clinical characteristics were associated with prolonged delay. More research is needed to better understand the reasons why patients with this serious and increasingly prevalent clinical syndrome delay seeking medical care in a timely fashion.
Keywords: heart failure, care seeking behavior, prehospital delay
Clinical Significance
Patients hospitalized with acute heart failure exhibited considerable delays in seeking medical care.
Several demographic and clinical characteristics were associated with delays in seeking hospital treatment.
Efforts remain needed to improve the collection of information about acute symptom onset and delays in seeking medical care in patients with heart failure and to more fully understand the reasons why patients with this clinical syndrome do not seek medical care in a more timely fashion after the development of acute symptoms.
Introduction
Mortality from coronary heart disease has been consistently declining in the United States over the past several decades1,2. In concert with these declining death rates, an increase in the pool of patients who are at risk for heart failure is occurring and heart failure is projected to be the next cardiovascular “epidemic”3.
While heart failure is a chronic condition, it is characterized by recurrent acute exacerbations, each of which can be associated with significant morbidity and mortality. Although considerable advances have been made in the management of patients with chronic heart failure, significant gains have not been accomplished in the more effective treatment of patients presenting with acute heart failure4. Given our present understanding of the pathophysiology of acute heart failure, it is reasonable to assume that early identification and treatment of the acutely decompensated state is beneficial. Despite this, the extent of, and factors associated with, delay in seeking medical care after the development of acute symptoms of heart failure has not been systematically explored. This is in contrast with the study of prehospital delay in patients with acute coronary syndromes where considerable information has been accrued and community intervention programs developed to reduce extent of prehospital delay in these high risk patients5-11.
Using data from an ongoing population-based surveillance study of acute heart failure among residents of the Worcester (MA) metropolitan area12,13, we examined the extent of prehospital delay, as well as patient characteristics associated with prolonged delay in seeking acute medical care, in patients hospitalized with decompensated heart failure. A secondary study goal was to describe the documentation of information about prehospital delay in clinical charts.
Methods
Adult male and female residents of all ages from the Worcester metropolitan area hospitalized for possible heart failure at all 11 greater Worcester medical centers during 2000 comprised the population of interest. The details of the Worcester Heart Failure Study have been previously described12,13. In brief, the medical records of patients with primary and/or secondary International Classification of Disease (ICD)-9 discharge diagnoses consistent with the possible presence of acute heart failure were reviewed in a standardized manner12,13. Patients with a discharge diagnosis of heart failure (ICD-9 code 428) comprised the primary diagnostic rubric reviewed. Patients who developed heart failure secondary to admission for another acute illness, such as after acute myocardial infarction, or after an interventional procedure, were not included.
Data Collection
The hospital records of greater Worcester residents with independently validated heart failure were abstracted for demographic and clinical data including age, sex, means of hospital transport (ambulance vs other means), area of residence (urban vs rural), medical history, acute presenting symptoms, time of acute symptom onset, and hospital survival status.
Although a variety of factors (e.g., patient, provider, and emergency medical services system) contribute to time to hospital presentation in persons experiencing signs and symptoms of acute illness, the term prehospital delay was used to represent all of the components of delay. This term was used because information about each of the components of delay was not able to be systematically collected. The time during which the patient reported becoming acutely or severely ill was used as the working definition of acute symptom onset time. Duration of prehospital delay was defined as the interval between acute symptom onset and arrival time in the emergency department of all greater Worcester hospitals. We also examined the occurrence of subacute symptoms, or early symptoms related to heart failure exacerbation, and the duration of delay in seeking medical care in patients with these more nonspecific symptoms. These symptoms were defined as those occurring prior to the onset of the acute symptoms, representing a change from usual health, but not of sufficient magnitude to prompt the patient to seek hospital treatment.
Results
A total of 2,587 greater Worcester residents were hospitalized at all metropolitan Worcester medical centers in 2000 with decompensated heart failure. The average age of the study sample was 76.3 years, 43.3% were men, and 92.7% were white; 75.1% of patients had been previously diagnosed with heart failure.
Information about acute symptom onset and extent of prehospital delay was able to be ascertained by our trained nurse and physician data abstractors from the medical records of 44% of patients hospitalized with acute heart failure. Inasmuch, the present report is based on the 1,142 Worcester residents diagnosed with heart failure in 2000 in whom data were available in hospital charts about duration of prehospital delay. Of the patients in whom information was available about prehospital delay, we were only able to calculate delay time after acute symptoms to a broad level of precision (<12 hours) in 171 patients (15% of all patients with delay times) based on the information contained in hospital charts. Information about extent of prehospital delay in patients who experienced subacute symptoms of a heart failure exacerbation was available in 1,553 patients (60% of study sample).
Characteristics of Patients with Delay Time Information
Patients with delay time information available were significantly more likely to be transported to Central Massachusetts hospitals by ambulance, were less likely to be of normal body weight, had slightly lower heart rates, were more likely to have been previously diagnosed with diabetes or coronary heart disease, were more likely to have presented with symptoms of chest pain, dyspnea, orthopnea, or palpitations, but were less likely to have presented with fatigue (Table 1). Patients with delay time information were also less likely to have died during hospitalization (Table 1).
Table 1.
Factors Associated with Availability of Delay Time Information in Patients with Acute Heart Failure
| Characteristic | Information available (+) (n=1,142) | Information not available (-) (n=1,445) | P value |
|---|---|---|---|
| % | % | ||
| Age (mean, yrs) | 76.2 | 76.5 | 0.61 |
| Male | 43.0 | 43.6 | 0.79 |
| White race/ethnicity | 93.8 | 91.9 | 0.08 |
| Transported by ambulance | 66.7 | 53.5 | <0.001 |
| Urban residence | |||
| Body Mass Index | |||
| <25 | 40.6 | 44.9 | |
| 25-30 | 28.2 | 26.9 | <0.05 |
| ≥30 | 31.2 | 28.1 | |
| Heart Rate (mean, bpm) | 88.5 | 90.6 | <.05 |
| Medical history | |||
| Angina (+) | 21.5 | 14.3 | <0.001 |
| Diabetes (+) | 42.2 | 38.1 | <0.05 |
| Heart failure (+) | 76.2 | 74.2 | 0.26 |
| Myocardial infarction (+) | 50.5 | 40.8 | <0.001 |
| Stroke (+) | 15.0 | 14.6 | 0.84 |
| Symptoms | |||
| Chest pain | 37.3 | 24.4 | <0.001 |
| Dyspnea | 95.6 | 91.1 | <0.001 |
| Orthopnea | 41.9 | 32.7 | <0.001 |
| Fatigue | 4.6 | 10.4 | <0.001 |
| Palpitations | 10.0 | 6.2 | <0.005 |
| Died during hospitalization | 3.4 | 7.1 | <0.001 |
Delay Times
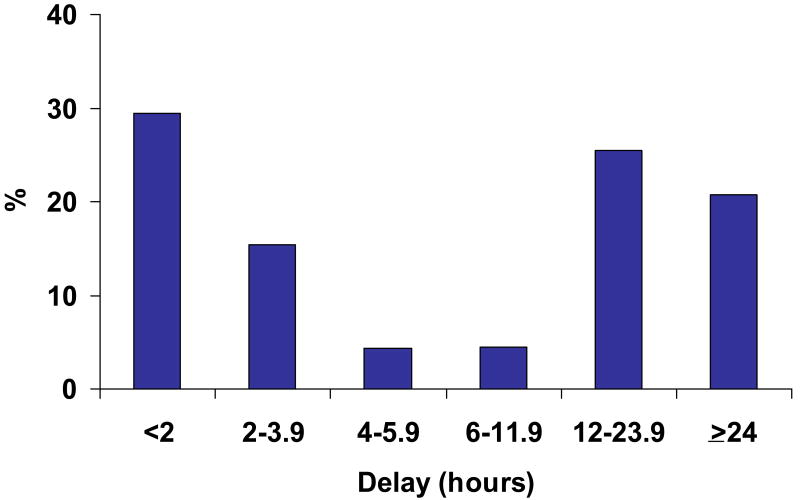
The average delay times were relatively long in patients who experienced acute symptoms of decompensated heart failure (mean = 13.3 hrs) whereas their median delay times were 2.0 hours. Consistent with the average delay times, the distribution of delay times was skewed to the right (Figure 1). Approximately 1 in 5 patients hospitalized for decompensated heart failure delayed seeking medical care by 1 day or longer. Among patients who reported experiencing subacute more nonspecific symptoms of heart failure, mean and median delay times were considerably longer (234 and 108 hours, respectively).
Figure 1. Distribution of Delay Times in Patients With Acute Heart Failure: Metropolitan Worcester, MA.
Characteristics Associated with Time to Hospital Presentation
We examined the association between a variety of clinical and demographic factors with duration of prehospital delay after acute symptoms, using the median cutpoint of 2 hours to distinguish those seeking care early from those seeking care after more prolonged delay (Table 2). Patients who exhibited prolonged delay (≥2 hours) were more likely to be younger, male, to arrive in the emergency department by means other than by ambulance, to be from an urban setting, to be heavier, to present with a lower heart rate at the time of hospital admission, and to not have been previously diagnosed with heart failure. Patients who experienced prolonged delay were more likely to present to area emergency departments with orthopnea. Similar factors were associated with extent of delay when we examined the demographic and clinical characteristics of those who sought care within the first 12 hours of acute symptom onset (approximate average duration of delay) as compared to those who delayed seeking hospital care by 12 hours or longer. In addition, when we further characterized the cutpoints of prehospital delay at <2 hours, 2-11.9 hours, and at ≥12 hours, relatively similar demographic and clinical factors were associated with prolonged delay in seeking acute medical care.
Table 2.
Factors Associated with Delays in Seeking Hospital Care in Patients With Acute Heart Failure
| Factor | <2 hours
(n=286) |
≥2 hours
(n=856) |
P value | ||
|---|---|---|---|---|---|
| Age (yrs) | n | % | n | % | |
| <65 | 25 | 8.7 | 148 | 17.3 | <.005 |
| 65-74 | 52 | 18.2 | 159 | 18.6 | |
| 75-84 | 123 | 43.0 | 344 | 40.2 | |
| ≥85 | 86 | 30.1 | 205 | 23.9 | |
| Sex | |||||
| Male | 99 | 34.6 | 392 | 45.8 | <.001 |
| Female | 187 | 65.4 | 464 | 54.2 | |
| Race/ethnicity | |||||
| White | 269 | 94.1 | 802 | 93.7 | 0.94 |
| Non-white | 17 | 5.9 | 54 | 6.3 | |
| Transported by Ambulance | |||||
| Yes | 234 | 81.8 | 528 | 61.7 | <.001 |
| No | 52 | 18.2 | 328 | 38.3 | |
| Place of residence | |||||
| Urban | 92 | 32.2 | 356 | 41.6 | <.005 |
| Not urban | 194 | 67.8 | 500 | 58.4 | |
| Body Mass Index | |||||
| <25 | 111 | 46.6 | 290 | 38.7 | <.05 |
| 25-30 | 63 | 26.5 | 216 | 28.8 | |
| ≥30 | 64 | 26.9 | 244 | 32.5 | |
| Heart Rate (bpm) | |||||
| <80 | 79 | 27.7 | 301 | 35.3 | <.01 |
| 80-99 | 97 | 34.0 | 285 | 33.3 | |
| 100-119 | 70 | 24.6 | 178 | 20.8 | |
| ≥120 | 39 | 13.7 | 91 | 10.6 | |
| Estimated glomerular filtration rate (ml/min per 1.732) | |||||
| ≥60 | 43 | 15.3 | 126 | 14.9 | 0.90 |
| 30-59 | 92 | 32.7 | 285 | 33.6 | |
| ≤30 | 146 | 52.0 | 437 | 51.5 | |
| Medical history | |||||
| Angina (+) | 72 | 25.2 | 174 | 20.3 | 0.10 |
| Angina (-) | 214 | 74.8 | 682 | 79.7 | |
| Diabetes (+) | 133 | 46.5 | 349 | 40.8 | 0.10 |
| Diabetes (-) | 153 | 53.5 | 507 | 59.2 | |
| Heart failure (+) | 51 | 17.8 | 221 | 25.8 | <.01 |
| Heart failure (-) | 235 | 82.2 | 635 | 74.2 | |
| Myocardial infarction (+) | 140 | 49.0 | 437 | 51.1 | 0.58 |
| Myocardial infarction (-) | 146 | 51.0 | 419 | 48.9 | |
| Stroke (+) | 47 | 16.4 | 124 | 14.5 | 0.48 |
| Stroke (-) | 239 | 83.6 | 732 | 85.5 | |
| Symptoms | |||||
| Chest pain (+) | 114 | 39.9 | 312 | 36.5 | 0.34 |
| Dyspnea (+) | 273 | 95.5 | 819 | 95.7 | 0.87 |
| Orthopnea (+) | 95 | 33.2 | 383 | 44.7 | <.01 |
| Fatigue (+) | 13 | 4.6 | 39 | 4.6 | 0.99 |
| Palpitations (+) | 29 | 10.1 | 85 | 9.9 | 0.92 |
| Discharge Status | |||||
| Alive | 276 | 96.5 | 827 | 96.6 | 0.93 |
| Dead | 10 | 3.5 | 29 | 3.4 | |
| Time of acute symptom onset | |||||
| 6:00 am -11:59 am | 75 | 27.5 | 117 | 27.2 | 0.88 |
| 12:00 pm -5:59 pm | 57 | 21.0 | 112 | 26.0 | |
| 6:00 pm – 11:59 pm | 71 | 26.1 | 100 | 23.3 | |
| 12:00 pm – 5:59 am | 69 | 25.4 | 101 | 23.5 | |
Based on the results of our regression analyses, male sex, not being transported to greater Worcester hospitals by ambulance, not having a prior diagnosis of heart failure, having orthopnea, and seeking care between midnight and six in the morning were associated with prolonged prehospital delay (Table 3). When we included the number of acute symptoms patients experienced prior to seeking medical care, patients who experienced any 3 or more (O.R. 1.35; 95% CI 0.67, 2.70) acute symptoms were more likely to delay seeking care than patients who experienced fewer acute symptoms.
Table 3.
Multivariable Model of Factors Associated with Prolonged Prehospital Delay in Patients With Acute Heart Failure
| Characteristic | Adjusted OR | 95% CI |
|---|---|---|
| Age (years) | ||
| 55-64 | 1.96 | 0.78,4.89 |
| 65-74 | 0.73 | 0.34,1.57 |
| 75-84 | 0.73 | 0.35,1.52 |
| ≥85 | 0.72 | 0.34,1.54 |
| Male | 1.42 | 1.04,1.96 |
| Transported by Ambulance | 0.44 | 0.30,0.63 |
| Urban residence | 1.24 | 0.89,1.71 |
| Initial heart rate (bpm) | ||
| 60-79 | 0.92 | 0.45,1.92 |
| 80-99 | 0.77 | 0.37,1.58 |
| 100-119 | 0.66 | 0.29,1.29 |
| ≥120 | 0.58 | 0.26,1.29 |
| Estimated glomerular filtration rate (ml/min/1.73m2) | ||
| 30-59 | 1.04 | 0.66,1.63 |
| ≥60 | 0.88 | 0.58,1.36 |
| Medical History (+) | ||
| Angina | 0.79 | 0.54,1.15 |
| Diabetes | 0.76 | 0.55,1.04 |
| Heart failure | 0.68 | 0.46,1.01 |
| Stroke | 1.09 | 0.72,1.66 |
| Myocardial infarction | 1.10 | 0.80,1.51 |
| Acute symptoms (+) | ||
| Fatigue | 1.60 | 0.80,3.20 |
| Chest pain | 0.88 | 0.64,1.21 |
| Rapid heart rate | 0.73 | 0.44,1.23 |
| Dyspnea | 1.10 | 0.54,2.25 |
| Orthopnea | 1.39 | 1.01,1.90 |
| Acute symptom onset time | ||
| 6:00-11:59 a.m. | 0.41 | 0.28,0.62 |
| 12:00-5:59 p.m. | 0.43 | 0.28,0.65 |
| 6:00-11:59 p.m. | 0.35 | 0.23,0.53 |
referent categories: <55 years, female, not transported by ambulance, rural residence, heart rate <60 bpm, body mass index <25, estimated glomerular filtration rate <30 ml/min per 1.732, absence of selected comorbidities, absence of various symptoms, acute symptom onset between 12 p.m. and 5:59 a.m.
Discussion
The results of this study among residents of a large New England metropolitan area suggest that a considerable proportion of patients hospitalized for heart failure exhibit prolonged delay in seeking medical care and that patients who seek care in a protracted manner can be characterized in advance. Our data also suggest that a substantial proportion of patients have a prolonged period of subacute, likely more nonspecific, symptoms prior to hospital presentation that is measured in days as opposed to hours for patients experiencing acute symptoms of heart failure. Disappointingly, information about duration of prehospital delay from acute symptom onset was missing in more than one half of the medical charts of hospitalized patients we reviewed, due either to inadequate questioning or recording of this information by health care providers or due to poor recall on the part of patients.
Extent of Delay in Seeking Medical Care
Due to the time dependent benefits associated with the early administration of coronary reperfusion strategies in patients with an evolving acute myocardial infarction, considerable attention has been devoted to examining extent of prehospital delay in these patients, factors associated with prolonged delay in seeking care, and in the development of educational programs designed to reduce duration of delay14,15.
In contrast, the profile of symptoms, extent of delay in seeking medical care, and factors associated with prolonged delay among patients with heart failure has not been examined in any detail. This stems partially from a lack of data documenting any association between delays in seeking treatment and subsequent morbidity and mortality. To the best of our knowledge there have been no published studies examining associations between delays in treatment and increased risk of adverse outcomes in patients with acute heart failure. Nevertheless, the natural history of acute heart failure suggests a spiraling course in which early intervention may reduce the risk of subsequent morbidity and mortality. Facilitation of the early recognition of heart failure associated symptoms and initiation of prompt therapy is the underlying premise for specialized heart failure management clinics16-18.
Our findings mirror the results of several smaller studies in which a substantial proportion of patients with acute heart failure delayed seeking medical attention by more than 12 hours. In an observational study of 57 patients treated for acute heart failure at a single urban hospital, the majority (90%) of hospitalized patients stated that dyspnea was their primary reason for seeking hospital care19. Duration of dyspnea was reported to be 6 days or longer for approximately one-third of the patients studied. In another small observational study of 83 patients admitted to an urban general hospital with heart failure20, the principal symptoms reported were dyspnea (98%) and edema (77%). Worsening of these symptoms was noted an average of 8 and 12 days prior to hospitalization, respectively. In a review of the medical records of 181 patients 60 years and older admitted with heart failure to a single hospital, the symptoms of heart failure were experienced by patients an average of 24 hours prior to hospital admission21. In a large study (n=753) of a predominantly male population treated at a single Veteran's Administration Medical Center in the late 1990's with a primary diagnosis of heart failure, dyspnea and edema were the 2 most frequently reported symptoms22. The average time from the onset of worsening symptoms to hospital arrival was 2.9 days and less than 5% of patients sought care within 1 day.
These studies in relatively small and select populations of patients with heart failure clearly document a longer duration of symptoms than is typically seen in patients with acute coronary disease where the average delay times range from approximately 4 to 6 hours. These findings suggest that while patients may experience acute symptoms of severe dyspnea in the 24 hours prior to hospital admission, many patients, if carefully questioned, will recall earlier more nonspecific symptoms of several days duration. Increased recognition of these symptoms by both patients and their providers may lead to significantly earlier intervention.
Factors Associated with Delay Patterns
The extended duration of symptoms prior to presentation for medical care in patients with an acute exacerbation of heart failure suggest considerable potential for success with interventions aimed at decreasing extent of delay. However, there has been very little prior study of factors associated with delay in seeking medical care among patients with acute heart failure. In the study of elderly patients admitted with heart failure to a New York hospital, decreasing age, history of heart failure, and development of multiple acute symptoms were modestly associated with increased prehospital delay21. A more recent study revealed no association between age and extent of delay but was limited in its findings by an even smaller study sample19.
The results of our investigation suggest that men, patients without prior heart failure, patients experiencing multiple acute symptoms, especially orthopnea, patients seeking hospital care by means other than by ambulance, and those presenting to greater Worcester hospitals at night were more likely to delay seeking hospital care. Additional studies remain needed to characterize the nature and duration of acute and premonitory symptoms associated with heart failure, heart disease patients' knowledge of heart failure and its symptoms, and psychosocial factors impacting patient responses to various symptoms23. A better understanding of these and other potential factors contributing to delays in seeking medical care will inform healthcare providers in the design of patient, provider, and/or community-based educational interventions aimed at decreasing delay times in patients with signs and symptoms of decompensated heart failure.
Collection of Information About Prehospital Delay from Medical Records
Disappointingly, a large proportion of the medical records of patients with decompensated heart failure were missing information about extent of delay. In a prior report from the Worcester Heart Attack Study, more than one-third of patients with a confirmed heart attack either failed to mention the time of onset of acute coronary symptoms, their self-reports were inadequately detailed to allow for the calculation of delay time, or this information was not recorded in hospital records24.
In our study, several patient characteristics were associated with the failure to collect delay time information. While the reasons for these observed associations are unknown, our findings suggest that patients may be differentially interviewed about their acute symptoms, patients may be too sick to be interviewed, or that patients who exhibit certain signs and symptoms, as well as those who have been previously diagnosed with selected conditions, may be more (or less) likely to be queried about the circumstances surrounding their episode of acute heart failure. While the collection of accurate information about the time of onset of symptoms suggestive of acute heart failure is challenging, it remains of considerable importance to collect and record these data in as systematic a manner as possible. Interestingly, patients were more likely to recall, or provide information about, premonitory symptoms associated with heart failure rather than about the acute symptoms of heart failure. This may be partially attributed to the chronicity of this clinical syndrome and subtle differences in patient's recall or perception of these symptoms. Efforts to improve the collection of this information should be a quality assurance initiative.
Study Strengths and Limitations
The strengths of our study include the large sample of patients hospitalized with heart failure from a New England metropolitan area whose sociodemographic characteristics reflect those of the nation as a whole, enhancing the generalizability of our study findings. The limitations of this study include the large proportion of patients without information on delay time and the lack of standardized questioning of patients about the onset of acute symptoms and recording of this information by different providers. We were also unable to measure the severity of acute symptoms, which may have been associated with care seeking patterns, and patients with systolic from those with diastolic heart failure. Lastly, we did not examine the association between delay care seeking patterns and overall mortality in the setting of decompensated heart failure since information was not collected about patients who died from acute heart failure outside of participating greater Worcester hospitals.
Conclusions
The results of this study reinforce the need for the systematic collection of data about symptom onset times in patients hospitalized with acute heart failure by medical care personnel. Failure to collect this information may affect physician's decisions to administer certain treatment modalities. Efforts remain needed to more systematically identify the reasons why patients delay seeking medical care in the setting of this serious clinical syndrome.
Acknowledgments
This research was made possible through funding support provided by the National Institutes of Health (R37 HL69874).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Morbidity and Mortality: 2004 Chartbook on Cardiovascular, Lung, and Blood Diseases. U.S. Department of Health and Human Services. National Institutes of Health; [Google Scholar]
- 2.American Heart Association. Heart Disease and Stroke Statistics – 2007 Update. Dallas, Texas: American Heart Association; 2007. [Google Scholar]
- 3.Braunwald E. Shattuck lecture – Cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360–1369. doi: 10.1056/NEJM199711063371906. [DOI] [PubMed] [Google Scholar]
- 4.Poole-Wilson PA. Treatment of Acute Heart Failure: Out with the old, in with the new. JAMA. 2002;287:1578–1580. doi: 10.1001/jama.287.12.1578. [DOI] [PubMed] [Google Scholar]
- 5.Burnett RE, Blumenthal J, Mark DB, Leimberger JD, Califf RM. Distinguishing between early and late responders to symptoms of acute myocardial infarction. Am J Cardiol. 1995;75:1019–1022. doi: 10.1016/s0002-9149(99)80716-4. [DOI] [PubMed] [Google Scholar]
- 6.Dracup K, Alonzo A, Atkins J, et al. The physician's role in minimizing delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Ann Intern Med. 1997;126:645–651. doi: 10.7326/0003-4819-126-8-199704150-00010. [DOI] [PubMed] [Google Scholar]
- 7.McGinn AP, Rosamond WD, Goff DC, Taylor HA, Miles JS, Chambless L. Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: Experience in 4 communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 8.DeLuca G, Suryapranata J, Ottervanger J, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends (1986-1997), and factors associated with, time to hospital presentation in patients with acute myocardial infarction (The Worcester Heart Attack Study) Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 10.Goff DC, Jr, Feldman HA, McGovern PG, Goldberg RJ, Simons-Morton DG, Cornell CE, Osganian SK, Cooper LS, Hedges JR. for the Rapid Early Action for Coronary Treatment (REACT) Study Group. Prehospital delay in patients hospitalized with heart attack symptoms in the United States: the REACT trial. Am Heart J. 1999;138:1046–1057. doi: 10.1016/s0002-8703(99)70069-4. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg RJ, Steg PG, Sadiq I, Granger CB, Jackson EA, Budaj A, Brieger D, Avezum A, Goodman S. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (the GRACE Registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RJ, Spencer FA, Farmer C, Meyer TE, Pezzella S. Incidence and hospital death rates associated with heart failure: A community-wide perspective. Am J Med. 2005;118:728–734. doi: 10.1016/j.amjmed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Spencer FA, Farmer C, Lessard D, Pezzella SM, Meyer T. Use of disease modifying therapies in patients hospitalized with heart failure: A population-based perspective. Am J Med. 2007;120(98):e1–8. doi: 10.1016/j.amjmed.2006.05.051. [DOI] [PubMed] [Google Scholar]
- 14.Luepker R, Raczynski J, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical services use in acute coronary heart disease: the Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA. 2000;274:60–67. doi: 10.1001/jama.284.1.60. [DOI] [PubMed] [Google Scholar]
- 15.Kainth A, Hewitt A, Sowden A, Duffy S, Pattenden J, Lewin R, Watt I, Thompson D. Systematic review of interventions to reduce delay in patients with suspected heart attack. Emerg Med J. 2004;21:506–508. doi: 10.1136/emj.2003.013276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 17.Stewart S, Vandenbroek AJ, Pearson S, Horowitz JD. Prolonged beneficial effects of a home-based intervention on unplanned readmissions and mortality among patients with congestive heart failure. Arch Intern Med. 1999;159:257–261. doi: 10.1001/archinte.159.3.257. [DOI] [PubMed] [Google Scholar]
- 18.Rich MW, Vinson JM, Speery JC, et al. Prevention of readmission in elderly patients with congestive heart failure: results of a prospective, randomized pilot study. J Gen Intern Med. 1993;8:585–590. doi: 10.1007/BF02599709. [DOI] [PubMed] [Google Scholar]
- 19.Parshall MB, Welsh JD, Brockopp DY, et al. Dyspnea duration, distress, and intensity in emergency department visits for heart failure. Heart Lung. 2001;30:47–56. doi: 10.1067/mhl.2001.112492. [DOI] [PubMed] [Google Scholar]
- 20.Schiff GD, Fung S, Speroff T, McNutt RA. Decompensated heart failure: symptoms, patterns of onset, and contributing factors. Am J Med. 2003;114:625–630. doi: 10.1016/s0002-9343(03)00132-3. [DOI] [PubMed] [Google Scholar]
- 21.Friedman M. Older adults' symptoms and their duration before hospitalization for heart failure. Heart Lung. 1997;26:169–176. doi: 10.1016/s0147-9563(97)90053-4. [DOI] [PubMed] [Google Scholar]
- 22.Evangelista LS, Dracup K, Doering LV. Treatment-seeking delays in heart failure patients. J Heart Lung Transplant. 2000;19:932–938. doi: 10.1016/s1053-2498(00)00186-8. [DOI] [PubMed] [Google Scholar]
- 23.Tsuyuki RT, McKelvie RS, Arnold JM, et al. Acute precipitants of congestive heart failure exacerbations. Arch Intern Med. 2001;161:2337–2342. doi: 10.1001/archinte.161.19.2337. [DOI] [PubMed] [Google Scholar]
- 24.Yarzebski J, Goldberg R, Gore J, et al. Temporal trends and factors associated with extent of delay to hospital arrival in patients with acute myocardial infarction: the Worcester Heart Attack Study. Am Heart J. 1994;128:255–63. doi: 10.1016/0002-8703(94)90477-4. [DOI] [PubMed] [Google Scholar]