Abstract
Simultaneous bilateral TKAs subject patients to more arduous and painful functional recovery and increased risk of hemodynamic complications than staged bilateral TKAs. Minimally invasive TKA (MIS-TKA) reportedly results in more rapid return of function by limiting the amount of soft tissue disruption. We asked whether bilateral MIS-TKA had advantages over conventional TKA with respect to faster functional recovery. We prospectively randomized 30 patients into an MIS group (mini-medial parapatellar approach, 15 patients) and a conventional group (conventional medial parapatellar approach, 15 patients). We recorded range of motion and the time required to regain the ability to walk without assistance. Functional recovery in the MIS group was faster in rehabilitation milestones of walking without assistance and gain in range of motion. Minimally invasive TKA may benefit patients undergoing simultaneous bilateral procedures with faster functional recovery.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Functional recovery during the early postoperative period after simultaneous bilateral TKAs often is arduous and painful despite decreased overall rehabilitation time and economic costs compared with staged bilateral TKAs [3, 5, 9]. Also, increased blood loss from the bilateral simultaneous procedures poses greater risks for hemodynamic complications and transfusion-related problems [9, 11].
Minimally invasive TKA (MIS-TKA) reportedly results in more rapid achievement of rehabilitation milestones and range of motion and reduces pain during the postoperative period [1, 7, 8, 19]. Minimally invasive TKA also may reduce blood loss and the incidence of hemodynamic complications by limiting the amount of soft tissue disruption over conventional TKA [10, 13, 18–20]. However, prolonged operative time and limited exposure in MIS-TKA may increase the risk of perioperative complications such as thromboembolic complications and malpositioning of the components [1, 7, 19]. We questioned whether bilateral MIS-TKAs diminish the disadvantages of bilateral conventional TKAs.
We asked whether bilateral MIS-TKAs result in faster functional recovery in terms of achieving the ability to walk without assistance and range of motion (ROM) than bilateral conventional TKAs.
Materials and Methods
We prospectively recruited all 32 consecutive patients who had bilateral simultaneous primary TKAs between November 2004 and May 2005. All 32 patients agreed to participate in the study. Inclusion criteria were: (1) age younger than 70 years; (2) no cardiopulmonary comorbidities; (3) flexion contracture of 30° or less; (4) body mass index of 33 kg/m2 or less; and (5) diagnosis of osteoarthritis. Approval was obtained from the Institutional Review Board, and all patients provided informed consent after receiving a complete description of the study.
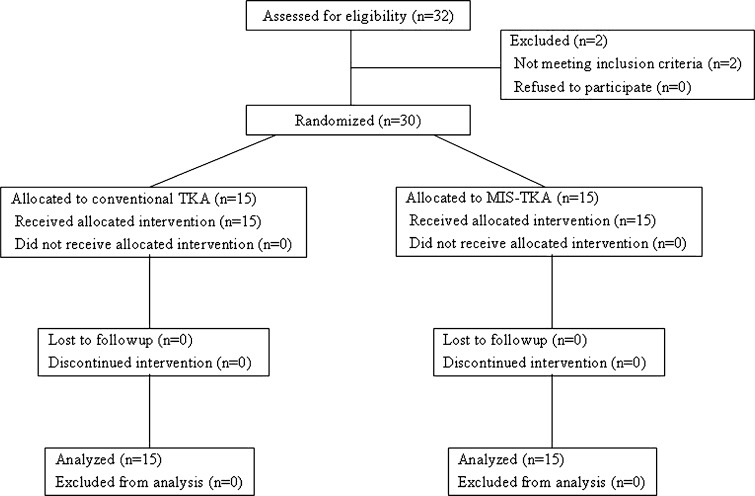
We performed a power analysis on the primary outcomes of the time to regain ability to walk without assistance and amount of range of motion (ROM) achieved during the postoperative 2 weeks. For the time to regain ability to walk without assistance, Tashiro et al. [19] reported a standard deviation of 4.9 days in a cohort of patients undergoing unilateral MIS-TKA. If similar variability is observed in our patients, then a sample of 15 subjects in each study group (30 subjects total), will provide 80% power (α = 0.05) to detect a difference of 5 days [19]. For ROM, Laskin et al. [10] reported a standard deviation of 12° in a cohort of patients undergoing unilateral MIS-TKA. If similar variability is observed in our patients, then a sample of 15 subjects in each study group (30 subjects total) will provide 80% power (α = 0.05) to detect a difference of 10o [10]. Thus, 30 patients were needed. One patient who had a flexion contracture greater than 30° and one patient with a diagnosis of rheumatoid arthritis were excluded (Fig. 1) [14]. Thus, 30 patients (28 females; two males) were randomized into one of two groups using a table of random numbers: bilateral MIS-TKAs or conventional TKA. Patients with even numbers were assigned to the conventional group, and those with odd numbers were assigned to the MIS group. All patients received allocated treatment and no patient was lost to followup in either group. Patients were followed a minimum of 24 months (mean, 28 months; range, 24–31 months). There were no noteworthy differences in the preoperative variables between the two groups (Table 1).
Fig. 1.
A CONSORT flow diagram of our subjects is presented. MIS-TKA = minimally invasive TKA.
Table 1.
Preoperative variables (mean ± standard deviation)
| Variables | MIS group (N = 15)* | Conventional group (N = 15)* | p Value |
|---|---|---|---|
| Age (years) | 66 (± 3.8) | 64 (± 6.4) | 0.306 |
| Gender* (female/male) | 28/2 | 28/2 | 1.000 |
| Height (cm) | 153 (± 4.9) | 153 (± 5.9) | 0.965 |
| Weight (kg) | 63 (± 6.8) | 62 (± 8.1) | 0.704 |
| Body mass index (kg/m2) | 26.9 (± 2.5) | 26.4 (± 2.7) | 0.609 |
| Tibiofemoral angle† (varus°) | 5.8 (± 4.5) | 5.8 (± 6.3) | 0.972 |
| Flexion contracture† (°) | 13 (± 6.3) | 16 (± 7.6) | 0.102 |
| Further flexion† (°) | 122 (± 13.1) | 128 (± 14.6) | 0.161 |
| Range of motion† (°) | 111 (± 14.3) | 110 (± 13.8) | 0.684 |
*The values are given as the number of patients; †the mean value of both knees in each patient was used for analyses; MIS = minimally invasive.
All surgeries were performed by the senior author (MCL), and the Nexgen LPS-Flex total knee system (Zimmer, Warsaw, IN) was used in all patients. The bilateral procedures were performed sequentially using a single anesthetic. Patients were placed in the supine position with both legs free on the operating table. A tourniquet was inflated throughout the procedure until the implants were cemented in both groups. For the MIS group, a straight midline skin incision was made from the superior pole of the patella to the level just medial to the tibial tuberosity. A mini-median parapatellar capsular incision was made extending proximally approximately 2 to 4 cm along the medial border of the quadriceps tendon. The patella was not everted throughout the procedure. Osteophytes and infrapatellar fat pad were removed to ease soft tissue tension and allow better exposure. Distal cutting of the femur was performed first with the knee flexed 90°. An intramedullary referenced cutting block was used that allowed for distal femoral valgus angles in 1° increments. The proximal tibia then was resected using an extramedullary alignment guide with special care taken to avoid injuring the patellar ligament. Next, a symmetric extension gap was ascertained using spacer blocks. After determination of femoral external rotation according to the symmetry of the flexion gap, the anterior and posterior chamfer cuts of the femur were performed. Soft tissue releases were performed as needed. The instruments that were used in the conventional group were modified to a smaller size for use in the MIS group, which allowed a smaller incision. For the conventional group, a median parapatellar incision was made extending approximately 10 cm to the interval just central to the junction of the rectus femoris and vastus medialis muscles. The patella was left everted throughout the procedure. In both groups, the patella was resected with a freehand technique after preparations for the femur and the tibia were completed. The components were implanted using standard cementing techniques in the order of the tibia, femur, and patella. All patients were monitored in the intensive care unit for the initial postoperative 24 hours. Closed suction drainage was used for 48 hours in both groups.
The same postoperative rehabilitation protocol was used for both groups. Patients began knee flexion exercises using a continuous passive motion exercise machine on the first day after surgery. They were allowed to perform straight leg raising exercises immediately while in the recovery room and were allowed to stand or walk using a knee immobilizer for support and a walker for balance on the first day after surgery. Intravenous patient-controlled anesthesia was used in 27 patients (14 in the MIS group and 13 in the conventional group), and epidural patient-controlled anesthesia was used in three (one in the MIS group and two in the conventional group). Patient-controlled anesthesia was continued as needed during the hospital stay. Most of the patients were discharged after approximately 2 weeks of hospitalization.
Postoperative blood loss, recorded as total closed suction drainage output, was less in the MIS group than in the conventional group (609 versus 871 mL), however, tourniquet time was longer in the MIS group (77 versus 63 minutes) (Table 2). The length of the skin incision, measured with the knee extended, was shorter in the MIS group than in the conventional group (13.4 versus 10.6 cm). There were no complications related to the operative procedure or clinically detectable deep vein thrombosis in either group. The amount of medication used for intravenous or epidural patient-controlled anesthesia and the number of intramuscular injections of analgesics required by each patient were similar between the two groups. The position of the components and alignment of the limb (tibiofemoral angle), measured with standing anteroposterior, lateral, and tangential patella radiographs with the knee in 30° flexion by one of the investigators (JHY) who was blind to the type of operative procedure, were similar between the two groups.
Table 2.
Perioperative variables (mean ± standard deviation)*
| Variables | MIS group (N = 15)* | Conventional group (N = 15)* | p Value |
|---|---|---|---|
| Length of skin incision† (cm) | 10.6 (± 1.0) | 13.4 (± 1.2) | < 0.001‡ |
| Blood loss† (mL) | 609 (± 281) | 871 (± 318) | 0.022‡ |
| Tourniquet time† (minutes) | 77 (± 14.4) | 63 (± 12.7) | < 0.001‡ |
| Tibiofemoral angle (valgus°)§ | 4.6 (± 3.1) | 5.5 (± 1.3) | 0.203 |
| Pain medication | |||
| Patient-controlled anesthesia (duration [days]/refills [numbers]) | 4.3 (± 1.4)/1.1 (± 0.5) | 4.6 (± 1.7)/1.0 (± 0.7) | 0.667/0.353 |
| Rescue injections (numbers) | 3.7 (± 2.5) | 3.3 (± 3.5) | 0.501 |
| Position of components§ | |||
| α angle (°) | 92 (± 5.7) | 90 (± 4.8) | 0.252 |
| β angle (°) | 89 (± 1.8) | 89 (± 1.4) | 0.323 |
| γ angle (°) | 5 (± 2.1) | 6 (± 2.3) | 0.103 |
| δ angle (°) | 88 (± 3.0) | 88 (± 2.3) | 0.945 |
*The values are given as the number of patients; †values represent the data for one knee; ‡statistically significant (p < 0.05); §the mean value of both knees in each patient was used for analyses; MIS = minimally invasive.
The time to regain the ability to walk without assistance was recorded and reported by the patients at the outpatient clinic followup. Patients were followed up 2 weeks, 6 weeks, 3 months, 6 months, and yearly thereafter. Range of motion was measured daily until 1 week postoperative and then at 10 and 14 days postoperative by one of the investigators (IH) using a goniometer and the standardized technique.
For comparison of ROM, the mean value of both knees of each patient was used for statistical analyses to account for within-subject correlation. Range of motion and time to walk without assistance was compared by independent unpaired t-tests as continuous variables that met the parametric assumptions. A p value less than 0.05 was considered significant for the time to walk without assistance. The p value of ROM was adjusted to 0.005 to correct for multiple comparisons using the Bonferroni method. Analyses were performed using SPSS for Windows statistical package (version 11.5; SPSS, Chicago, IL).
Results
The time to regain the ability to walk without assistance was significantly faster in the MIS group (p = 0.043). Patients in the MIS group averaged 32 days (± 11) and patients in the conventional group averaged 45 days (± 21). The gain of ROM was faster in the MIS group at postoperative Day 4 (100 ± 15 vs. 87 ± 14; p = 0.005), Day 5 (108 ± 13 vs. 94 ± 14; p = 0.001), Day 6 (115 ± 11 vs. 100 ± 14; p < 0.001), and Day 7 (118 ± 10 vs. 105 ± 15; p = 0.002).
Discussion
Simultaneous bilateral TKAs provide the advantages of a quicker return of function with fewer days of hospitalization and reduced economic costs than staged bilateral TKAs [12, 15]. However, increased acute blood loss during the simultaneous bilateral total knee procedures poses greater risks of hemodynamic complications and transfusion-related problems for patients. Minimally invasive TKA apparently results in a more rapid return of function and less blood loss by limiting the amount of soft tissue disruption than conventional TKA [10, 18]. We hypothesized the proposed faster functional recovery of patients having MIS-TKAs would be more considerable in the simultaneous bilateral procedure.
There are limitations in this study. First, a relatively small number of patients limits interpretation and the generalizability of the study. The number of patients recruited in this study was determined to show differences in rehabilitation milestones, the primary outcomes of the study. To compare the incidence of complications of TKA, a larger number of patients is required. Moreover, owing to limited power some potential benefits of the MIS-TKA might have gone undetected. Second, the results might not be generalizable owing to referral or selection bias. Third, no intraobserver and interobserver observations were performed for the outcome variables. Although the variables were measured by one investigator who was blind to the type of procedure the patient underwent, intraobserver and interobserver analyses could have made the data more reliable. Fourth, the use of general linear models framework using generalized estimating equations would have been proper to account for the within-subject correlation of knee-specific variables analyzed in this study. The mean of both knees was used to account for the within-subject correlation in this study. Finally, the odd/even number method of randomization using a table of random numbers has the potential for selection bias. Other methods of randomization would have been more appropriate.
One advantage of simultaneous bilateral TKAs is reduced overall rehabilitation time and consequent reduction in economic costs [4, 16]. However, this advantage is only noted when the simultaneous bilateral procedure is compared with the sum of two of the separate unilateral TKAs. When compared with one separate unilateral TKA, postoperative rehabilitation after simultaneous bilateral TKAs is slow and difficult because of a twofold increase in the need for postoperative rehabilitation facilities [9]. Also, the time needed for independent ambulation and to achieve acceptable ROM is prolonged in the simultaneous bilateral group [9]. Our data suggest the time to achieve independent ambulation and the progression of ROM were faster in the MIS-TKA group. The advantages of MIS-TKA in early restoration of function have been reported for the unilateral TKA [10, 19]. These advantages of MIS-TKA may be beneficial to patients during the early postoperative period after simultaneous bilateral TKAs.
The greater amount of acute blood loss, which caused greater fluid shift and consequently resulted in cardiopulmonary complications, was reported for the simultaneous bilateral procedures but not for the staged unilateral procedures [6, 9, 11]. Also, the risk of transfusion complications increases with increasing amounts of allogeneic transfusions [4]. Although the amount of blood loss was considerably smaller in the MIS group, the incidence of cardiopulmonary complications was not considerably different in both groups. A relatively small number of patients and the rather strict inclusion criteria of the study might have contributed to this finding.
A higher incidence of thromboembolic complications during the perioperative period has been reported after simultaneous bilateral TKAs [2, 17]. The prolonged operative time in MIS procedures may pose greater risk of thromboembolic complications. However, we observed no clinically detectable deep vein thrombosis or pulmonary embolism in the MIS or conventional group. Faster rehabilitation in the MIS group might have offset the possible increase in the risk of thromboembolic complications by the longer operating time required for the MIS procedure.
The MIS approach in simultaneous bilateral TKAs is advantageous for faster functional recovery when compared with the conventional approach.
Acknowledgments
We thank the Medical Research Collaborating Center at Seoul National University Hospital for statistical help. This study was supported by a grant from the Innovative Research Institute for Cell Therapy, Republic of Korea (Grant no. A062260).
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Aglietti P, Baldini A, Sensi L. Quadriceps-sparing versus mini-subvastus approach in total knee arthroplasty. Clin Orthop Relat Res. 2006;452:106–111. doi: 10.1097/01.blo.0000238789.51972.16. [DOI] [PubMed] [Google Scholar]
- 2.Barrett J, Baron JA, Losina E, Wright J, Mahomed NN, Katz JN. Bilateral total knee replacement: staging and pulmonary embolism. J Bone Joint Surg Am. 2006;88:2146–2151. doi: 10.2106/JBJS.E.01323. [DOI] [PubMed] [Google Scholar]
- 3.Bullock DP, Sporer SM, Shirreffs TG., Jr. Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am. 2003;85:1981–1986. doi: 10.2106/00004623-200310000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Dennis DA. Debate: bilateral simultaneous total knee arthroplasty. Clin Orthop Relat Res. 2004;428:82–83. doi: 10.1097/01.blo.0000147650.90507.84. [DOI] [PubMed] [Google Scholar]
- 5.Hutchinson JR, Parish EN, Cross MJ. A comparison of bilateral uncemented total knee arthroplasty: simultaneous or staged? J Bone Joint Surg Br. 2006;88:40–43. doi: 10.1302/0301-620X.88B1.16454. [DOI] [PubMed] [Google Scholar]
- 6.Jankiewicz JJ, Sculco TP, Ranawat CS, Behr C, Tarrentino S. One-stage versus 2-stage bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;309:94–101. [PubMed] [Google Scholar]
- 7.King J, Stamper DL, Schaad DC, Leopold SS. Minimally invasive total knee arthroplasty compared with traditional total knee arthroplasty: assessment of the learning curve and the postoperative recuperative period. J Bone Joint Surg Am. 2007;89:1497–1503. doi: 10.2106/JBJS.F.00867. [DOI] [PubMed] [Google Scholar]
- 8.Kolisek FR, Bonutti PM, Hozack WJ, Purtill J, Sharkey PF, Zelicof SB, Ragland PS, Kester M, Mont MA, Rothman RH. Clinical experience using a minimally invasive surgical approach for total knee arthroplasty: early results of a prospective randomized study compared to a standard approach. J Arthroplasty. 2007;22:8–13. doi: 10.1016/j.arth.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Lane GJ, Hozack WJ, Shah S, Rothman RH, Booth RE, Jr, Eng K, Smith P. Simultaneous bilateral versus unilateral total knee arthroplasty: outcomes analysis. Clin Orthop Relat Res. 1997;345:106–112. doi: 10.1097/00003086-199712000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Laskin RS, Beksac B, Phongjunakorn A, Pittors K, Davis J, Shim JC, Pavlov H, Petersen M. Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res. 2004;428:74–81. doi: 10.1097/01.blo.0000148582.86102.47. [DOI] [PubMed] [Google Scholar]
- 11.Leonard L, Williamson DM, Ivory JP, Jennison C. An evaluation of the safety and efficacy of simultaneous bilateral total knee arthroplasty. J Arthroplasty. 2003;18:972–978. doi: 10.1016/S0883-5403(03)00282-1. [DOI] [PubMed] [Google Scholar]
- 12.Liu TK, Chen SH. Simultaneous bilateral total knee arthroplasty in a single procedure. Int Orthop. 1998;22:390–393. doi: 10.1007/s002640050284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lombardi AV, Jr, Viacava AJ, Berend KR. Rapid recovery protocols and minimally invasive surgery help achieve high knee flexion. Clin Orthop Relat Res. 2006;452:117–122. doi: 10.1097/01.blo.0000238824.56024.7a. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Schulz KF, Altman D, CONSORT Group (Consolidated Standards of Reporting Trials). The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–1991. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- 15.Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13:172–179. doi: 10.1016/S0883-5403(98)90095-X. [DOI] [PubMed] [Google Scholar]
- 16.Ritter MA, Harty LD. Debate: simultaneous bilateral knee replacements: the outcomes justify its use. Clin Orthop Relat Res. 2004;428:84–86. doi: 10.1097/01.blo.0000148784.17187.2f. [DOI] [PubMed] [Google Scholar]
- 17.Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty: a survival analysis. J Bone Joint Surg Am. 2003;85:1532–1537. doi: 10.2106/00004623-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Scuderi GR, Tenholder M, Capeci C. Surgical approaches in mini-incision total knee arthroplasty. Clin Orthop Relat Res. 2004;428:61–67. doi: 10.1097/01.blo.0000148574.79874.d0. [DOI] [PubMed] [Google Scholar]
- 19.Tashiro Y, Miura H, Matsuda S, Okazaki K, Iwamoto Y. Minimally invasive versus standard approach in total knee arthroplasty. Clin Orthop Relat Res. 2007;463:144–150. [PubMed] [Google Scholar]
- 20.Tria AJ, Jr, Coon TM. Minimal incision total knee arthroplasty: early experience. Clin Orthop Relat Res. 2003;416:185–190. doi: 10.1097/01.blo.0000093030.56370.d9. [DOI] [PubMed] [Google Scholar]