Abstract
Diaphyseal malunion of the forearm may cause loss of pronation and supination, a painful distal radioulnar joint, and aesthetic problems. Seventeen patients (10 males, seven females; mean age, 20.6 ± 9.3 years) were operated on because of symptomatic malunion after a pediatric forearm fracture. Six patients had predominant loss of pronation (Group 1), four had predominant loss of supination (Group 2), and seven had a painful distal radioulnar joint (Group 3). An osteotomy of the radius was performed in seven patients and of both forearm bones in 10. All patients were available for clinical and radiologic assessments at a minimum followup of 6 months (mean ± standard deviation, 3.7 ± 2.3 years; range, 0.5–9.9 years). Release of the contracted interosseous membrane frequently was necessary for patients in Groups 1 and 2 to allow for correction and did not result in weakness, instability of the distal radioulnar joint, or synostosis. The overall improvement in range of motion after osteotomies for patients with a supination deficit was much better than in those with a pronation deficit. All patients in Group 3 gained a pain-free and stable distal radioulnar joint and their range of motion was unchanged. Therefore, ability to improve overall range of motion through forearm osteotomies is dependent on the patients’ preoperative complaint.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Posttraumatic diaphyseal malunion of the radius and the ulna can cause limited forearm range of motion (ROM) in pronation-supination, a painful distal radioulnar joint (DRUJ), and appearance problems [38]. Anatomic open reduction and internal fixation has become the benchmark procedure in treating forearm fractures in adults to avoid malunion [1, 15]. In children, however, bone healing in less than anatomic position is still compatible with later unrestricted function because of the corrective potential during skeletal growth [18]. Forearm fractures in children, therefore, usually are treated with closed reduction and immobilization and only unstable fractures are treated surgically [35]. Recommendations regarding maximum acceptable displacement in children are dependent on age, fracture level, and type of displacement and remain controversial [7, 9, 14, 18, 30]. Nonetheless, some malunions of the forearm in children result in functional impairment and a high rate of refracture [5, 13, 30, 41].
Forearm malunions are responsible for impairment in ROM through different mechanisms. Angular deformities of the radius and ulna produce tension in the interosseous membrane and bone impingement that impair free rotation of the radius around the mechanical axis of the forearm [16]. Conversely, modification in alignment of the proximal and distal radioulnar joints observed in axial malunions may account for limitations in forearm rotation because both joints’ sectors of mobility are not perfectly overlapped [16]. Numerous biomechanical studies have investigated the effects of angular and axial malunions of the forearm bones on limitation of ROM and DRUJ instability [3, 4, 6, 8, 12, 19, 20, 24, 25, 31, 33, 37]. Different isolated or combined axial malunions of the radius and ulna may result in comparable forearm stiffness [12]. Identifying the most likely origin of the stiffness can be difficult, especially because no method is available to assess axial malunions less than 35° for the radius and less than 20° for the ulna, although axial malunion below these limits can produce forearm stiffness [2, 10–12, 37, 39]. There is clinical and experimental evidence that all kinds of osteotomies are not equal in their ability to improve overall ROM. Derotation osteotomy of one forearm bone improves motion in the direction of the osteotomy at the expense of motion in the other direction resulting in no change in overall ROM [12, 23]. Conversely, overall ROM is improved by correcting an angular deformity of the radius greater than 15° toward the interosseous membrane because this deformity alone impairs pronation and supination [24, 38]. Therefore, ability to improve overall ROM through forearm osteotomies is related to the type of osteotomy that is performed, which in turn depends on the characteristics of the malunion.
Contracture of the interosseous membrane can result in limited forearm rotation in paralytic conditions [42]. To our knowledge, there is no such clinical evidence for posttraumatic conditions nor has release of the interosseous membrane been used for treatment of forearm stiffness associated with forearm malunion [38]. Therefore, the effect of interosseous membrane release is not known either on improvement of forearm rotation or whether predicted instability of the forearm or other complications like synostosis or DRUJ instability would occur.
We hypothesized that characteristics of preoperative functional impairment depend on the type and extent of the forearm malunion and may help define groups of patients with different potential for improvement in overall ROM after osteotomy. Specifically, if patients are grouped according to the preoperative complaint that results from forearm malunion, can the improvement from osteotomy be better predicted? Additionally, we hoped to ascertain how the type of preoperative complaint affects the functional outcome of the forearm osteotomy and whether the release of the interosseous membrane induces complications in these patients.
Materials and Methods
We retrospectively reviewed 17 patients with symptomatic diaphyseal malunions of the forearm resulting from pediatric forearm fractures treated by corrective osteotomy. Patients were grouped into three categories according to their main preoperative complaints. We assessed preoperative and postoperative ROM and radiographs, and strength, symptoms, and the occurrence of complications. Statistical analysis was used to assess how the type of preoperative complaint affected ROM and functional improvements after osteotomies.
This series included all patients consecutively operated on by the two senior authors (LN, CED) between 1994 and 2001 in the Department of Orthopaedic Surgery at the University of Zurich and the Division of Hand Surgery at the University of Bern. We based the indication for the osteotomy on stiffness of forearm ROM in pronation-supination or the occurrence of painful snapping at the DRUJ during pronation and supination that impaired activities of daily living. The patient records and radiographs were reviewed at last followup by one independent observer (LJ) who was blinded to the results. The patients’ mean age at the time of surgery was 20.6 years (range, 12.8–41.6 years). There were six female patients and 11 male patients (Table 1). We treated nine right and eight left extremities. The dominant arm was affected in six patients and the nondominant arm in 11 patients. They were no Monteggia or Galeazzi fractures based on the normal anatomy of the humeroradial and the distal radioulnar joints assessed on the initial radiographs. The treatment for a forearm fracture occurred at a mean age of 12.8 years (range, 7.1–19.2 years); the mean delay from fracture to corrective osteotomy was 7.8 years (range, 0.4–30.2 years); and the minimum followup was 6 months (mean, 3.7 years; range, 6 months–9.9 years).
Table 1.
Patient details
| Group | Patient number | Gender | Injured side | Dominant side | Age at fracture (years) | Age at osteotomy (years) | Osteotomy radius/ulna | Release interosseous membrane | Followup (years) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | F | R | R | 11.8 | 18.4 | RA, U | Yes | 9.94 |
| 2 | F | R | L | 11.4 | 41.6 | RA, U | Yes | 3.24 | |
| 3 | M | R | R | 13.7 | 15.6 | RA, U | Yes | 1.01 | |
| 4 | F | L | R | 12.8 | 13.7 | RA, U | Yes | 0.51 | |
| 5 | F | L | R | 14.6 | 16.2 | RA, U | No | 3.05 | |
| 6 | F | R | R | 11.9 | 40.9 | RA, U | Yes | 1.78 | |
| 2 | 7 | M | L | R | 19.2 | 19.6 | RA | Yes | 2.85 |
| 8 | M | L | R | 14.3 | 18.4 | RA, U | Yes | 3.81 | |
| 9 | M | R | R | 11.2 | 13.3 | RA, U | Yes | 1.48 | |
| 10 | M | L | R | 7.1 | 17.8 | RA, U | No | 3.85 | |
| 3 | 11 | M | R | R | 13.3 | 35.3 | RA, U | No | 3.35 |
| 12 | M | R | L | 10.3 | 21.3 | RA | No | 4.43 | |
| 13 | M | R | R | 16.8 | 17.6 | RA | No | 2.24 | |
| 14 | F | R | L | 11.6 | 14.3 | RA | No | 6.79 | |
| 15 | M | L | R | 13.4 | 18.0 | RA | No | 4.89 | |
| 16* | M | L | R | 11.2 | 12.8 | RA | No | 4.44 | |
| 17 | M | L | R | 12.7 | 15.8 | RA | No | 5.27 |
*Double-level osteotomy; F = female; M = male; R = right; L = left; RA = radius; U = ulna.
Three groups of patients were defined according to the main clinical problem (Table 2). Six patients (gender ratio, 1:5 male:female; mean age at fracture, 12.7 years; mean age at osteotomy, 24.4 years) had predominant loss of pronation (Group 1), four (gender ratio, 4:0 male:female; mean age at fracture, 13.0 years; mean age at osteotomy, 17.3 years) had predominant loss of supination (Group 2), and seven (gender ratio, 6:1 male:female; mean age at fracture, 12.8 years; mean age at osteotomy, 19.3 years) had a painful DRUJ but no major pronation-supination impairment in comparison to the healthy side (Group 3).
Table 2.
Functional assessment
| Group | Patient number | Pronation/supination (degrees) | ROM difference (degrees) | Assessment at last followup | ||||
|---|---|---|---|---|---|---|---|---|
| Injured side preoperatively | Injured side postoperatively | Healthy side | Postoperatively-preoperatively | Postoperatively-healthy side | Relative grip strength (%) | DASH score | ||
| 1 | 1 | 15-0-75 | 50-0-20 | 70-0-80 | −20 | −80 | 112% | 9 |
| 2 | 0-10-85 | 40-0-65 | 70-0-95 | 30 | −60 | 81% | 25 | |
| 3 | 10-0-75 | 60-0-80 | 65-0-90 | 55 | −15 | 89% | ND | |
| 4 | 5-0-90 | 50-0-90 | 80-0-80 | 45 | −20 | 76% | ND | |
| 5 | 40-0-60 | 65-0-50 | 75-0-90 | 15 | −50 | 74% | 30 | |
| 6 | 20-0-70 | 40-0-80 | 75-0-85 | 30 | −40 | 103% | 13 | |
| 2 | 7 | 45-0-10 | 55-0-80 | 55-0-85 | 80 | −5 | 83% | 37 |
| 8 | 70-0-0 | 60-0-90 | 65-0-90 | 80 | −5 | 92% | 1 | |
| 9 | 90-0-10 | 80-0-90 | 90-0-90 | 70 | −10 | 97% | 0 | |
| 10 | 60-10-0 | 25-0-70 | 75-0-70 | 45 | −50 | 109% | 3 | |
| 3 | 11 | 70-0-100 | 75-0-95 | 85-0-110 | 0 | −25 | 105% | 1 |
| 12 | 70-0-95 | 70-0-95 | 70-0-95 | 0 | 0 | 96% | 0 | |
| 13 | 75-0-70 | 90-0-90 | 70-0-90 | 35 | −20 | 91% | 3 | |
| 14 | 65-0-100 | 65-0-120 | 50-0-120 | 20 | 15 | 72% | 17 | |
| 15 | 65-0-80 | 75-0-90 | 75-0-90 | 20 | 0 | 93% | 7 | |
| 16* | 50-0-80 | 55-0-75 | 55-0-85 | 0 | −10 | 91% | 1 | |
| 17 | 80-0-90 | 80-0-120 | 80-0-120 | 30 | 0 | 120% | 0 | |
*Double-level-osteotomy; ROM = range of motion; DASH = Disabilities of the Arm, Shoulder and Hand; ND = not determined.
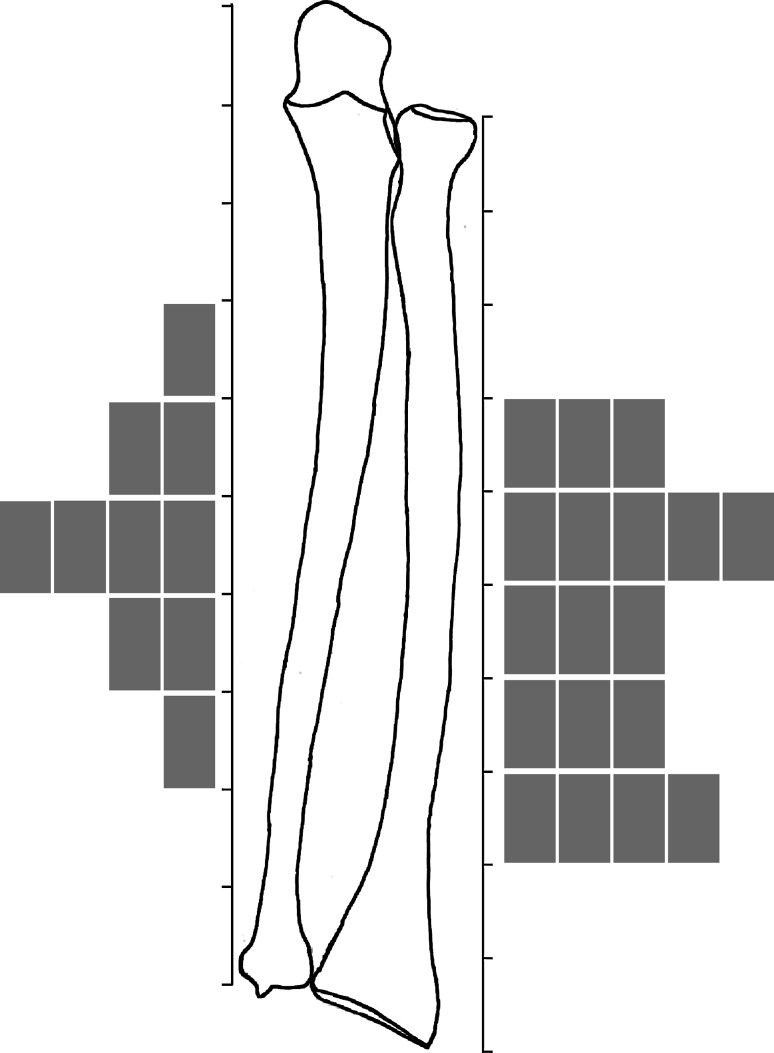
The level of the deformity was defined as percent of the entire length of the bone (Fig. 1). Seventy-two percent of malunions were located in the middle third of the radius and 90% in the middle third of the ulna (Fig. 1). In Group 1, all malunions were located in the proximal two-thirds of the radius and the ulna with both forearm bones always involved with angular deformities (Fig. 2). Four patients in this group also had axial malunions of 30° or greater affecting one of the forearm bones. In Group 2, all but one patient (Patient 7) had combined angular malunions of the radius and the ulna. Only one (Patient 5) had the malunion located in the distal third of the radius. No patient in this group had a rotational malunion of the radius of 30° or greater, and only one patient (Patient 8) had a combined rotational malunion of the ulna equal to 25°. Conversely, all but one patient (Patient 11) in Group 3 had an isolated malunion of the radius. All patients in this group had malunions of the radius located in the distal half of the bone, six of seven were in the distal third.
Fig. 1.
The levels of malunions of the radius and the ulna are shown. The number of rectangles indicates the number of osteotomies that were performed at this level of the radius and the ulna.
Fig. 2A–D.
Preoperative (A) anteroposterior and (B) lateral and postoperative (C) anteroposterior and (D) lateral radiographs show the forearm with malunions of the radius and the ulna corrected with osteotomies of both forearm bones (Patient 8).
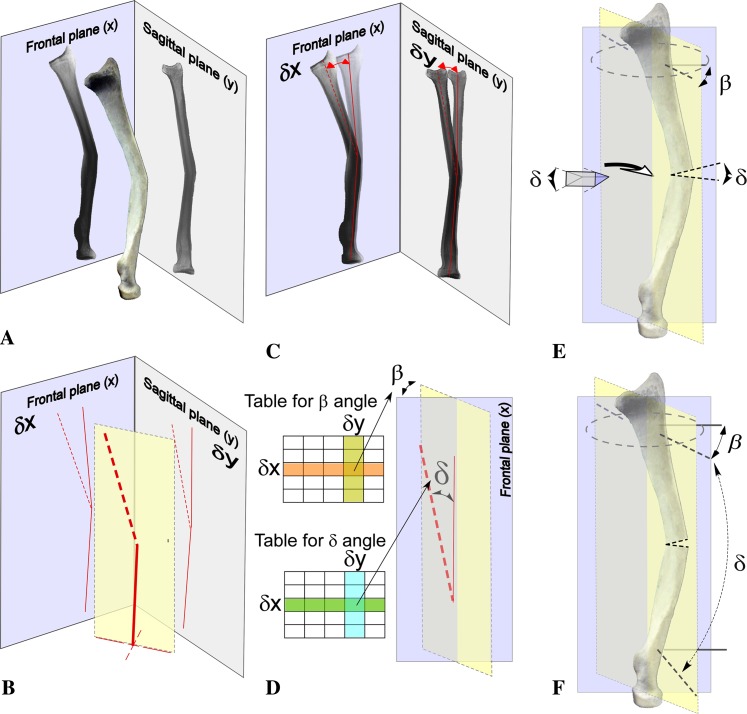
For preoperative planning, the opposite healthy side served as a template because the correctional osteotomy intended to reproduce the osseous geometry of the normal side. Therefore, we obtained plain radiographs of both forearms in full length. For anteroposterior and lateral projections of the radius, the distal joint surface was considered, whereas for the ulna, the humeroulnar joint was used as assessed under the image intensifier. The contours of the healthy and deformed bones in both projections were drawn on separate sheets of tracing paper. By simple superposition, we determined the location of maximal deformity and angular deformity in both planes (Fig. 3). From these projections, the true angle of deformity (δ), corresponding to the maximal angulation, and its orientation in space (β) were calculated using established tables [29]. If the anatomic relationship of the radial styloid and the bicipital tuberosity and that of the ulnar styloid and the coronoid process were different on both sides, we suspected an axial malunion. The level of the axial malunion was determined as the level of the initial fracture as assessed in percentages of the entire length of the bone or was considered at the same level as the angular deformity if both deformities were present. The exact amount of radial and ulnar torsion was defined on comparative MR images of both forearms in nine patients (Table 3) [4, 11]. Side difference in the torsion profile of the radius exceeding 30° or 20° in the ulna was a reason to correct the axial malunion, because side differences greater than these limits are considered nonphysiologic [10]. The site of the osteotomy determined the type of exposure. We marked the position of the planned osteotomy with a Kirschner wire placed under fluoroscopic control. Two Kirschner wires marked the frontal plane in both fragments using the distal radius and the humeroulnar joint as landmarks for the radius and the ulna, respectively (Fig. 3). At the planned site, a wedge of bone usually was excised (incorporating the true angle of deformity = δ) in the proper orientation (in the plane of the true deformity = β) allowing for a closing wedge osteotomy, which was instrumented with a 3.5-mm compression plate. Opening wedge osteotomy with interposition of a structural graft was performed when facing relative shortening of the radius to produce ± 1 mm ulnar variance. In case of combined angular and axial malunions, a transverse osteotomy was performed and derotation of the forearm bone was performed using bone clamps to stabilize the bone extremities with the plate. Intraoperative orthogonal radiographs were obtained and the angular deformity was further corrected with attention paid to restoration of the radial bow [34]. After completion of the correction, the plate was definitively fixed to the bone with screws. Intraoperatively, we checked correctness of spatial reconstruction by standard biplanar radiographs. If reconstruction of the true anatomic shape of the forearm bones did not result in free motion, we identified the interosseous membrane and released it from its ulnar insertion, except in Patient 7, in whom the release was performed from radial insertion. In some cases, reduction of the osteotomy proved difficult or impossible because of the overly tense, contracted interosseous membrane. In these cases, we split the interosseous membrane from ulnar insertion to permit reduction.
Fig. 3A–F.
A radius malunion consists of an angulation at the middle third of the bone in the radial-dorsal to ulnar-volar plane. The orientation of the deformity in space and the value of the maximal angular deformity, termed true angle of deformity, are assessed with (A) orthogonal radiographs. (B) The projections of the deformity in frontal and sagittal planes are shown as assessed with an orthogonal radiograph. (C) Preoperative planning is started with superposition of the radiograph of both sides. This allows assessment of the angular deformity in frontal (δx) and sagittal planes (δy). δx and δy are used to assess the value of the true angle of deformity (δ) and the orientation of the deformity in space (β) using the established table (D) [29]. (E) δ also defines the angle of the bone wedge that must be removed for a closed wedge osteotomy or the wedge of the structural bone graft to be inserted in an open wedge osteotomy to correct the deformity. (F) The correction must be performed in the plane of maximum deformity, defined by β in respect to the frontal plane. Intraoperatively, two Kirschner wires (plain line) are placed in the frontal plane using the distal radius as a landmark. The level of the osteotomy also is marked with a Kirschner wire. Subsequently, the plane of correction is marked with two Kirschner wires (dotted line) inserted with a β angle in respect to the Kirschner wires in the frontal plane. The second of these wires is inserted with a δ angle in respect to the first one. After completion of the osteotomy, the two Kirschner wires must be parallel (δ = 0) but the β angle is still the same.
Table 3.
Preoperative and postoperative radiologic assessments
| Group | Patient number | Radius | Ulna | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||||||||||||
| Loc (%) | δ (°) | β (°) | π (°) | δ (°) | β (°) | π (°) | Loc (%) | δ (°) | β (°) | π (°) | δ (°) | β (°) | π (°) | ||
| 1 | 1 | 47 | 15 | 26 | 45 | 0 | 0 | −50 | 56 | 9 | 41 | 0 | 0 | 0 | −15 |
| 2 | 49 | 13 | 48 | 30 | 0 | 0 | 0 | 43 | 10 | 0 | 0 | 0 | 0 | 0 | |
| 3 | 56 | 20 | 0 | 0 | 0 | 0 | 0 | 56 | 23 | 40 | 30 | 8 | 0 | 0 | |
| 4 | 32 | 16 | 45 | ND | 0 | 0 | 0 | 43 | 7 | 0 | ND | 0 | 0 | 0 | |
| 5 | 71 | 16 | 0 | 0 | 14 | 57 | −10 | 65 | 10 | 0 | 10 | 12 | 90 | 0 | |
| 6 | 45 | 18 | 40 | 45 | 0 | 0 | −14 | 55 | 7 | 0 | 7 | 0 | 0 | −6 | |
| 2 | 7 | 40 | 12 | 0 | ND | 0 | 0 | 0 | None | 0 | 0 | ND | 0 | 0 | 0 |
| 8 | 40 | 16 | 0 | 0 | 0 | 0 | 10 | 39 | 11 | 31 | −25 | 7 | 0 | 15 | |
| 9 | 55 | 30 | 45 | ND | 0 | 0 | 0 | 62 | 10 | 0 | ND | 0 | 0 | 0 | |
| 10 | 35 | 10 | 0 | −20 | 0 | 0 | 50 | 78 | 10 | 0 | 0 | 0 | 0 | 12 | |
| 3 | 11 | 56 | 13 | 18 | ND | 0 | 0 | 0 | 55 | 9 | 0 | ND | 0 | 0 | 0 |
| 12 | 66 | 7 | 0 | ND | 0 | 0 | 0 | None | 0 | 0 | ND | 0 | 0 | 0 | |
| 13 | 77 | 18 | 40 | 20 | 0 | 0 | 0 | None | 0 | 0 | 0 | 0 | 0 | 0 | |
| 14 | 68 | 13 | 32 | ND | 0 | 0 | 0 | None | 0 | 0 | ND | 0 | 0 | −30 | |
| 15 | 70 | 20 | 0 | ND | 0 | 0 | 20 | None | 0 | 0 | ND | 0 | 0 | 35 | |
| 16* | 37 | 19 | 47 | ND | 11 | 0 | 0 | None | 0 | 0 | ND | 0 | 0 | −10 | |
| 78 | 7 | 0 | ND | ||||||||||||
| 17 | 65 | 20 | 0 | ND | 8 | 90 | 0 | None | 0 | 0 | ND | 0 | 0 | 0 | |
*Double-level osteotomy; Loc = location of the apex of the deformity in percent of whole length starting from the proximal apex of the bone; δ = maximum angulation of the deformity in degrees; β = angle between the plane carrying the maximum angulation of the bone deformity and the frontal plane in degrees; π = torsional deformity in degrees; positive values for supination of the distal fragment in respect to the proximal one, negative values for pronation of the distal fragment in respect to the proximal one; ND = not determined.
We performed 17 osteotomies (one double osteotomy) of the radius, 10 osteotomies of the ulna, two interpositional corticocancellous bone grafts in open-wedge osteotomy of the radius, and eight releases of the interosseous membrane. The forearm was immobilized with a resting splint for 6 weeks. All patients started forearm active motion exercises within the first 2 postoperative weeks. Dynamic stretching splints, passive motion, and strengthening were started after 6 weeks. Overall, six patients had hardware removal before the last followup.
We measured forearm pronation-supination with a gravity goniometer and the value was indicated according to the neutral-null method [40]. Stability of the distal radioulnar joint was assessed clinically in neutral rotation by manually stressing the joint palmarly and dorsally [22]. We clinically assessed ulnar impaction syndrome that should have resulted from inadequate shortening of the radius or longitudinal instability of the forearm after splitting the interosseous membrane with a compression test of the ulnocarpal joint and finger palpation of the triangular fibrocartilage complex (TFCC) [21]. A Jamar dynamometer (Jamar Hand Dynamometer; Sammons Preston Inc, Bollingbrook, IL) at setting II was used to measure grip strength using the average of three measurements. Percentage of strength between sides, termed relative grip strength, was calculated. The first part of the Disabilities of the Arm, Shoulder and Hand (DASH; www.dash.iwh.on.ca) score was administered as a self-report questionnaire to measure function and symptoms at the last followup [17]. It contains 23 questions to assess impairment in activities of daily living with a scale ranging from 1 (not limited at all) to 5 (unable), six questions to assess pain with a scale ranging from 1 (none) to 5 (extreme), and one question about influence of pain on sleep with a scale ranging from 1 (no difficulty) to 5 (so much difficulty that I cannot sleep). We then normalized the score (observed score-30/1.2) to obtain a linear scale ranging from 0 to 100. The overall scaling direction indicated the higher the score, the worse the functional outcome. We obtained full-length conventional radiographs of both forearms, anteroposterior and lateral in neutral rotation and with the elbow flexed at 90°, and any angular residual deformity was measured in the same way as preoperatively. Residual axial malunions were determined systematically at the last followup with fluoroscopy coupled with goniometry [10].
Measurements were recorded on a Microsoft® Office Excel® 2003 data sheet (Microsoft Corp, Walisellen, Switzerland). Mean values and standard deviations were calculated. We used a paired t-test to compare preoperative and postoperative ROM, one-way analysis of variance with Tukey’s honestly significant difference post hoc test to compare gain in ROM among groups of patients, Mann-Whitney U test (release versus nonrelease of the interosseous membrane), or Kruskal-Wallis one-way analysis of variance by ranks to compare age at fracture and osteotomy, grip strength, and DASH scores among groups of patients using StatView 5.01 (SAS Institute, Cary, NC). Significance was set at p < 0.05.
Results
The ages of the patients at the time of fracture and osteotomy were not statistically different among groups of patients, but gender ratios differed widely.
The type of preoperative complaint defined groups of patients with different potential for improvement in overall ROM after osteotomy. Patients in Group 1 gained 38° ± 13° pronation (p < 0.001) but lost 6° ± 28° supination (p = 0.63) on average. Patients in Group 2 gained 80° ± 8° supination (p < 0.0005) but lost 11° ± 18° pronation (p = 0.31). All patients in Group 3 gained a stable and pain-free DRUJ, and their ROM statistically was unchanged (5° ± 6° gain in pronation [p = 0.06], 10° ± 14° gain in supination [p = 0.10]). The overall ROM (pronation + supination) was improved by 29° ± 20° in Group 1, 69° ± 17° in Group 2, and 15° ± 15° in Group 3. The improvement in ROM was greater (p < 0.002) in Group 2 than in Group 1. Among the five patients with residual impairment of ROM greater than 30° with respect to the healthy side, four were in Group 1 and one was in Group 2; none was in Group 3.
The type of preoperative complaint had no significant influence on strength and functional impairment at last followup. The mean grip strength in Groups 1, 2, and 3 were 89% ± 15%, 95% ± 11%, and 95% ± 15%, respectively. The relative grip strength was greater than 80% in all but three patients. These three patients (Patients 4, 5, 14) were all operated on the nondominant side and had a relative grip strength greater than 70% with respect to the healthy side. The mean DASH scores in Groups 1, 2, and 3 were 19 ± 10, 10 ± 18, and 5 ± 6, respectively. There were no statistically significant differences for mean grip strength (p = 0.60) and DASH score (p = 0.14) among groups of patients.
The release of the interosseous membrane did not induce complications and had no deleterious effect on strength. No patients had compartment syndromes, delayed unions, infections, refractures, ossification of the interosseous membrane, radioulnar synostosis, or degeneration of the proximal or distal radioulnar joints. There were no statistically significant differences for grip strength between patients with a released interosseous membrane and those with a nonreleased interosseous membrane (p = 0.70). No patients had postoperative instability of the DRUJ or signs of ulnar impaction syndrome.
Discussion
In this study, we assessed improvement of ROM after forearm osteotomies performed in patients with symptomatic malunions after pediatric fractures of the forearm according to their preoperative complaint. Three groups of patients with limitation of pronation, supination, or the presence of painful snapping of the DRUJ were identified. We also characterized the pattern of malunion in these three groups, which in turn served to determine the type of osteotomy that was performed. It was our major assumption, based on clinical and anatomic studies, that all osteotomies are not equal in their ability to improve overall ROM and we tested this assumption with statistical analysis. Release of the interosseous membrane was used in some patients along with the osteotomy, and we then assessed if the release produced complications or decreased the strength compared with those of patients who did not have release.
There were several limitations in this study. The overall number of patients was small with Group 2 containing only four patients. One observer blinded to the study reviewed records and radiographs; therefore, intraobserver and interobserver assessments could not be done. The study design did not allow assessment of the influence of the release of the interosseous membrane on improvement of ROM. Also, this series was too small to assess the correlation between particular patterns of forearm malunions and a ROM deficit predominating in pronation or supination.
A few retrospective studies have reported on outcomes after osteotomies for malunited fractures of the forearm in children [5, 26, 30, 41] and adults [38]. These studies assessed changes in ROM produced by different kinds of osteotomies in skeletally immature and mature patients with forearm malunions. Some authors recommended not postponing the osteotomy when the malunion is obvious, because improvement in ROM was better if the osteotomy was performed within 1 year after the injury [38, 41]. We cannot assess this correlation in this series of patients because only three of 17 patients had osteotomy performed within this time. Children had a higher gain in ROM if the osteotomy was performed before 10 years of age probably because some residual bone deformities improved with additional skeletal growth [41]. Similarly, we cannot test this correlation because no patients younger than 10 years had surgery.
Several investigations assessed the effect of experimental angular malunions of the radius and ulna on pronation and supination. Angulation of 10° of one forearm bone has little impact on motion, but combined deformities of 10° of the radius and ulna toward the interosseous membrane considerably decreases supination but not pronation [24]. Conversely, isolated 20° angulation of the radius reduces pronation in dorsal angulation and supination in volar angulation, and the same angulation toward the interosseous membrane decreases supination and pronation. Combined angular deformities of the radius and ulna in different directions reduce substantially more ROM than combined angulation in the same direction [37]. Proximal deformities had less impact on ROM than equivalent deformities produced at the middle or the distal third of the radius [33]. Similarly, several investigations assessed the effect of experimental axial malunions of the radius and ulna on pronation and supination [12, 19, 37, 39]. Isolated axial malunion of the radius in supination markedly reduced pronation but did not change supination, and malunion of the radius in pronation reduced supination but did not change pronation. Axial malunion of the ulna in supination had little effect on ROM, and an axial malunion in pronation decreased supination to a lesser extent than the radius malunion. Only combined axial malunions of the ulna and radius in the opposite direction reduced pronation and supination simultaneously.
Patients with reduced motion or a painful DRUJ revealed different patterns of bone deformities in this series of patients. The most complex deformities were in Group 1 with both bones involved and with four of six patients having combined angular and axial deformities. The least complex deformities were in Group 3, with six of seven patients having isolated deformities of the radius mostly located at the distal third of the bone. Patients in Group 2 had an intermediate pattern of deformity consisting mostly of bone involved with angular deformities at the proximal or middle third of the forearm bones. For these reasons, the complexity of the osteotomies differed widely among patients, the most complex correction having been done in Group 1 and the least in Group 3. We observed the major deficit in pronation or supination in some patients in Groups 1 and 2 outweighed the deficit corresponding to the observed bone deformities as documented in experimental studies [12, 24, 37]. We postulated that posttraumatic contracture of the interosseous membrane contributed to increase the deficit in ROM. Surgical release of the contracted interosseous membrane has been described for paralytic fixed supination deformities after obstetric brachial plexus lesions, poliomyelitis, or tetraplegia [42]. Surgical sectioning of the interosseous membrane does not entail instability of the forearm or the DRUJ in neurologic conditions. In our series of patients, there was evidence of a posttraumatic contracture of the interosseous membrane, because in numerous instances, the tension exerted by the interosseous membrane on the forearm bones did not permit correction of the bone deformity. Thus, release already was warranted to achieve the planned reduction after osteotomy as reported in experimental studies [24, 33]. No clinical instability symptoms, statistically significant loss in grip strength, or occurrence of postoperative synostosis occurred in our patients after interosseous membrane release with respect to patients without membrane release. In this study, it was not possible to prove release of the interosseous membrane improved ROM because of important differences in terms of bone deformities and osteotomies performed among patients with or without release. However, patients with painful DRUJ but no limitation in ROM did not require an interosseous membrane release and regained a pain-free and stable DRUJ with osteotomies alone.
Although the occurrence of DRUJ instability resulting from shaft deformity was reported , it is far less common than after malunion of the distal radius [6, 8, 38]. Cases of DRUJ instability resulting from forearm malunions in which bone osteotomies alone resulted in joint stabilization have been reported [38]. We preferred to use the term painful DRUJ instead of DRUJ instability because pain was the main preoperative complaint and therefore the main reason why patients decided to undergo an osteotomy. The different pattern of DRUJ instability and the difficulty to assess instability with radiographs make use of this term inaccurate without assessing the TFCC with imaging or arthroscopy [36]. However, we assume surgical treatment of a painful DRUJ obviously resulting from forearm malunion primarily should address the bone deformity. There is recent clinical evidence, however, of TFCC tears associated with distal forearm fractures in the pediatric population so until now, specific investigation of the TFCC should be considered in case of painful or DRUJ instability after a distal forearm fracture [43].
Among the three patients with residual angulation or axial malunion after osteotomies, one lost 20° motion and two others had a residual deficit of 50° with respect to the healthy side despite some improvement in ROM. These residual deformities obviously were the result of incorrect planning or inaccuracy in the surgical correction, or in one case, possibly because the interosseous membrane was not released. Combining correction of angular and axial deformities is difficult because rotation around an oblique osteotomy automatically induces a change in angulation. Mathematical models have been developed to perform both corrections through one bone cut but are difficult to use during surgery [27, 28, 32]. A geometric tool was designed to facilitate preoperative planning of osteotomies for complex deformities [28]. However, accuracy of preoperative planning is dependent on correct assessment of the angular and axial components of the deformity. Therefore, the lack of reliable assessments of radius and ulna axial malunions impair accurate planning of osteotomies of complex deformities in the radius and ulna [10, 11]. The overall improvement in ROM after osteotomies for patients with a predominant deficit in supination was much better than for patients with a pronation deficit. Patients with deficits in pronation are at risk for fewer improvements in ROM than patients with deficits in supination. This could be attributable to the higher complexity of the malunions observed in Group 1 than in Group 2 so that difficult osteotomies, ending in lesser reliability, were performed in the first group. Another explanation might be that the deficit in pronation is easily compensated through the shoulder but not compensated in a supination deficit, resulting in increased motivation for patients to improve supination. Nonetheless, these surgeries did not induce weakness, and the functional outcome was good in all groups of patients.
Symptomatic malunions of the forearm are rare but pose challenging issues in patients with complex deformities. Bone angulations are easily discernible on radiographs, but those involving the radius must be assessed with respect to a plane of reference taking into account the axial rotation of this bone during pronation-supination to make side comparison possible. Axial malunions are difficult to be estimated with two-plane radiographs, and therefore we recommend systematically assessing axial malunions preoperatively with MRI and fluoroscopy coupled with goniometry before planning corrective osteotomy of the forearm [10, 11]. However, axial malunions of the radius and the ulna are difficult to quantify because the healthy side is the only available reference, and there are important side differences in the healthy population [4, 10, 11]. This may jeopardize accurate preoperative planning, especially when angular and axial malunions are present, with the risk of performing an incorrect three-dimensional bone reconstruction. Patients should be informed about this limitation. Release of the interosseous membrane may be required to get enough bone fragment mobility to correct the deformity. This release does not induce complications like synostosis or DRUJ instability and may contribute to postoperative improvement in ROM. Patients with complex deformities requiring derotation osteotomy, especially those with impaired pronation, may experience residual forearm stiffness or acquire only a shift in ROM. Conversely, surgery in case of a deficit in supination or simple angular bone deformity will reliably improve ROM or decrease pain in the DRUJ if it was the main preoperative complaint. Therefore, all kinds of malunions of the forearm are not equal in terms of postoperative improvement. Development of three-dimensional models and computer simulation of diaphyseal malunions of the forearm will help in planning the osteotomy and therefore improve reliability of this surgery in complex deformities.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his institution has waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Anderson LD, Sisk D, Tooms RE, Park WI., 3rd Compression-plate fixation in acute diaphyseal fractures of the radius and the ulna. J Bone Joint Surg Am. 1975;57:287–289. [PubMed] [Google Scholar]
- 2.Bade H, Lobeck F. Gelenkflachenverhalten der Articulatio radioulnaris distalis bei fehlgestelltem distalem Radius. Unfallchirurgie. 1991;17:213–217. doi: 10.1007/BF02588689. [DOI] [PubMed] [Google Scholar]
- 3.Bade H, Strickling H, Rutt J. Bewegungseinschränkungen im proximalen und distalen radioulnargelenk bei postraumatischer angulation und torsion des radius. Aktuelle Traumatol. 1991;21:274–278. [PubMed] [Google Scholar]
- 4.Bindra RR, Cole RJ, Yamaguchi K, Evanoff BA, Pilgram TK, Gilula LA, Gelberman RH. Quantification of the radial torsion angle with computerized tomography in cadaver specimens. J Bone Joint Surg Am. 1997;79:833–837. doi: 10.2106/00004623-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Blackburn N, Ziv I, Rang M. Correction of the malunited forearm fracture. Clin Orthop Relat Res. 1984;188:54–57. [PubMed] [Google Scholar]
- 6.Bowers WH. Instability of the distal radioulnar articulation. Hand Clin. 1991;7:311–327. [PubMed] [Google Scholar]
- 7.Cooper RR. Management of common forearm fractures in children. J Iowa Med Soc. 1964;54:689–698. [PubMed] [Google Scholar]
- 8.Crisco JJ, Moore DC, Marai GE, Laidlaw DH, Akelman E, Weiss AP, Wolfe SW. Effects of distal radius malunion on distal radioulnar joint mechanics: an in vivo study. J Orthop Res. 2007;25:547–555. doi: 10.1002/jor.20322. [DOI] [PubMed] [Google Scholar]
- 9.Daruwalla JS. A study of radioulnar movements following fractures of the forearm in children. Clin Orthop Relat Res. 1979;139:114–120. [PubMed] [Google Scholar]
- 10.Dumont CE, Nagy L, Ziegler D, Pfirrmann CW. Fluoroscopic and magnetic resonance cross-sectional imaging assessments of radial and ulnar torsion profiles in volunteers. J Hand Surg Am. 2007;32:501–509. doi: 10.1016/j.jhsa.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Dumont CE, Pfirrmann CWA, Ziegler D, Nagy L. Assessment of radial and ulnar torsion profiles with cross-sectional magnetic resonance imaging: a study of volunteers. J Bone Joint Surg Am. 2006;88:1582–1588. doi: 10.2106/JBJS.E.01042. [DOI] [PubMed] [Google Scholar]
- 12.Dumont CE, Thalmann R, Macy JC. The effect of rotational malunion of the radius and the ulna on supination and pronation. J Bone Joint Surg Br. 2002;84:1070–1074. doi: 10.1302/0301-620X.84B7.12593. [DOI] [PubMed] [Google Scholar]
- 13.Filipe G, Dupont JY, Carlioz H. Les fractures itératives des deux os de l’avant-bras de l’enfant. Chir Pédiatr. 1979;20:421–426. [PubMed] [Google Scholar]
- 14.Fuller DJ, McCullough CJ. Malunited fractures of the forearm in children. J Bone Joint Surg Br. 1982;64:364–367. doi: 10.1302/0301-620X.64B3.7096406. [DOI] [PubMed] [Google Scholar]
- 15.Grace TG, Eversmann WW., Jr Forearm fractures: treatment by rigid fixation with early motion. J Bone Joint Surg Am. 1980;62:433–438. [PubMed] [Google Scholar]
- 16.Graham TJ, Fischer TJ, Hotchkiss RN, Kleinman WB. Disorders of the forearm axis. Hand Clin. 1998;14:305–316. [PubMed] [Google Scholar]
- 17.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand). The Upper Extremity Collaborative Group (UEGC) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.Hughston JC. Fracture of the forearm in children. J Bone Joint Surg Am. 1962;44:1678–1693. [Google Scholar]
- 19.Kasten P, Krefft M, Hesselbach J, Weinberg AM. How does torsional deformity of the radial shaft influence the rotation of the forearm? A biomechanical study. J Orthop Trauma. 2003;17:57–60. doi: 10.1097/00005131-200301000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Kasten P, Krefft M, Schneider S, Hesselbach J, Weinberg AM. Pro- und Supinationseinschränkungen bei Torsionsfehlstellungen der Radiusdiaphyse vor und nach Ulnaosteotomie. Orthopade. 2004;33:455–461. doi: 10.1007/s00132-003-0544-9. [DOI] [PubMed] [Google Scholar]
- 21.Kleinman WB, Graham TJ. Distal ulnar injury and dysfunction. In: Peimer AC, editor. Surgery of the Hand and Upper Extremity. New York, NY: McGraw-Hill; 1996. pp. 667–709. [Google Scholar]
- 22.Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J Hand Surg Am. 2000;25:464–468. doi: 10.1053/jhsu.2000.6467. [DOI] [PubMed] [Google Scholar]
- 23.Lipskeir E, Weizenbluth M. Derotation osteotomy of the forearm in management of paralytic supination deformity. J Hand Surg Am. 1993;18:1069–1074. doi: 10.1016/0363-5023(93)90404-Q. [DOI] [PubMed] [Google Scholar]
- 24.Matthews LS, Kaufer H, Garver DF, Sonstegard DA. The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. J Bone Joint Surg Am. 1982;64:14–17. [PubMed] [Google Scholar]
- 25.McHenry TP, Pierce WA, Lais RL, Schacherer TG. Effect of displacement of ulna-shaft fractures on forearm rotation: a cadaveric model. Am J Orthop. 2002;31:420–424. [PubMed] [Google Scholar]
- 26.Meier R, Prommersberger KJ, Lanz U. Die operative Korrektur posttraumatischer Deformitäten am Unterarm nach Frakturen im Wachstumalter. Z Orthop Ihre Grenzgeb. 2003;141:328–335. doi: 10.1055/s-2003-40086. [DOI] [PubMed] [Google Scholar]
- 27.Merle d’Aubigné R, Descamps L. L’ostéotomie plane oblique dans la correction des déformations des membres. Bull Mem Arch Chirurgie. 1952;8:271–276. [PubMed] [Google Scholar]
- 28.Meyer DC, Siebenrock KA, Schiele B, Gerber C. A new methodology for the planning of single-cut corrective osteotomies of mal-aligned long bones. Clin Biomech (Bristol, Avon) 2005;20:223–227. doi: 10.1016/j.clinbiomech.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 29.Nagy L. Malunion of the distal end of the radius. In: Fernandez DL, Jupiter JB, editors. Fractures of the Distal Radius, a Practical Approach to Management. New York, NY: Springer; 2002. pp. 289–344. [Google Scholar]
- 30.Price CT, Knapp DR. Osteotomy for malunited forearm shaft fractures in children. J Pediatr Orthop. 2006;26:193–196. doi: 10.1097/01.bpo.0000194699.29269.76. [DOI] [PubMed] [Google Scholar]
- 31.Prommersberger KJ, Van Schoonhoven J, Lanz UB. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg Br. 2002;27:55–60. doi: 10.1054/jhsb.2001.0693. [DOI] [PubMed] [Google Scholar]
- 32.Sangeorzan BP, Judd RP, Sangeorzan BJ. Mathematical analysis of single-cut osteotomy for complex long bone deformity. J Biomech. 1989;22:1271–1278. doi: 10.1016/0021-9290(89)90230-3. [DOI] [PubMed] [Google Scholar]
- 33.Sarmiento A, Ebramzadeh E, Brys D, Tarr R. Angular deformities and forearm function. J Orthop Res. 1992;10:121–133. doi: 10.1002/jor.1100100115. [DOI] [PubMed] [Google Scholar]
- 34.Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74:1068–1078. [PubMed] [Google Scholar]
- 35.Schmittenbecher PP. State-of-the-art treatment of forearm shaft fractures. Injury. 2005;36(suppl 1):A25–34. doi: 10.1016/j.injury.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 36.Szabo RM. Distal radioulnar joint instability. Instr Course Lect. 2007;56:79–89. [PubMed] [Google Scholar]
- 37.Tarr RR, Garfinkel AI, Sarmiento A. The effects of angular and rotational deformities of both bones of the forearm: an in vitro study. J Bone Joint Surg Am. 1984;66:65–70. [PubMed] [Google Scholar]
- 38.Trousdale RT, Linscheid RL. Operative treatment of malunited fractures of the forearm. J Bone Joint Surg Am. 1995;77:894–902. doi: 10.2106/00004623-199506000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Tynan MC, Fornalski S, McMahon PJ, Utkan A, Green SA, Lee TQ. The effect of ulnar axial malalignment on supination and pronation. J Bone Joint Surg Am. 2000;82:1726–1731. doi: 10.2106/00004623-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Urban V, Kalberer F, Roos M, Dumont CE. Reproduzierbarkeit der Messung der aktiven Unterarmdrehung: vergleich von 3 Methoden. Z Orthop Ihre Grenzgeb. 2002;140:72–76. doi: 10.1055/s-2002-22094. [DOI] [PubMed] [Google Scholar]
- 41.van Geenen RC, Besselaar PP. Outcome after corrective osteotomy for malunited fractures of the forearm sustained in childhood. J Bone Joint Surg Br. 2007;89:236–239. doi: 10.1302/0301-620X.89B2.18208. [DOI] [PubMed] [Google Scholar]
- 42.Zancolli EA. Paralytic supination contracture of the forearm. J Bone Joint Surg Am. 1967;49:1275–1284. [PubMed] [Google Scholar]
- 43.Zimmermann R, Rudisch A, Fritz D, Gschwentner M, Arora R. MRT zur Beurteilung von Begleitverletzungen distaler Unterarmbrüche im Wachstumsalter. Handchir Mikrochir Plast Chir. 2007;39:60–67. doi: 10.1055/s-2007-964926. [DOI] [PubMed] [Google Scholar]