Abstract
Although neutrophil gelatinase-associated lipocalin (NGAL) may play a pivotal role in the innate immune response, there are currently no data on NGAL levels in human immunodeficiency virus (HIV)-infected patients. In this study we aimed to examine the regulation of NGAL in HIV infection. The regulation of NGAL in HIV infection was examined by different experimental approaches, including studies in peripheral blood and mononuclear cells (MNC) from bone marrow aspirates before and during highly active anti-retroviral therapy (HAART). We found that: before initiating HAART, HIV-infected patients (n = 37) had significantly decreased serum NGAL levels compared with healthy controls (n = 26); (ii) during HAART, there was a gradual and significant increase in NGAL concentrations reaching levels comparable to those in healthy controls after 12 months; (iii) this increase was seen primarily in virological responders to HAART (HIV RNA level <200 copies/ml after 24 months); (iv) phytohaemagglutinin-stimulated NGAL release in MNC cells from bone marrow aspirates was decreased in untreated HIV-infected patients compared with healthy controls, but increased after 26 weeks on HAART; and (v) there was a significant positive correlation between neutrophil counts and NGAL levels at all time-points during HAART. We have shown decreased NGAL levels in HIV-infected patients, potentially reflecting decreased number and function of neutrophils as well as impaired bone marrow myelopoiesis. These abnormalities were reversed by successful HAART. Our findings underscore further the involvement of neutrophils and innate immunity in HIV-related immunodeficiency.
Keywords: bone marrow, HAART, HIV, lipocalin-2, neutrophils
Introduction
Lipocalin-2, in humans named neutrophil gelatinase-associated lipocalin (NGAL), is a 25-kDa glycoprotein belonging to the lipocalin superfamily whose members share a barrel-shaped tertiary structure with a hydrophobic pocket that can bind lipophilic molecules [1]. NGAL is found to be synthesized constitutively during a narrow window of maturation in the granulocyte precursors (myelocyte/metamyelocyte) in the bone marrow, and is stored in specific granules of mature neutrophils as a monomer, a homodimer or a heterodimer in complex with gelatinase [2]. NGAL has also been detected in other cell types with a particularly prominent expression in epithelial cells [3–5].
Although increased NGAL levels have been reported during inflammation, possibly involving Toll-like receptor (TLR)-related mechanisms [6–8], its biological function in humans is far from clear. However, it has been proposed as a scavenger of bacterial products at sites of inflammation and as a modulator of inflammatory responses [9]. Moreover, recent studies in lipocalin-2-deficient mice have shown that the mouse homologue to NGAL, 24p3, has an essential bacteriostatic role under iron-limited conditions, acting as an iron-depleting factor in the innate immune response by limiting bacterial iron supply through binding bacterial siderophores [10,11].
A progressive CD4+ T cell depletion accompanied by defective T cell function is the immunological hallmark of untreated human immunodeficiency virus (HIV) infection [12]. However, HIV-related immunodeficiency also includes other abnormalities, such as impaired innate immune responses involving decreased function and numbers of neutrophils [13], potentially also associated with dysregulation of NGAL. Although NGAL may have a pivotal role in the innate immune response to bacterial infection, there are at present no data on NGAL levels in HIV-infected patients. In this study we examined the regulation of NGAL in HIV infection by different experimental approaches, including studies in peripheral blood and bone marrow samples procured before and during highly active anti-retroviral therapy (HAART).
Materials and methods
Patients and control subjects
A group of 37 patients (median age 40 years; range, 24–64 years; 24 men and 13 women) was followed during HAART with serum samples taken before 3, 6, 12 and 24 months after initiation of therapy. Before start of therapy, median laboratory values (interquartile range) were as follows: CD4+ T cell count, 200 × 106 cells/l (90–360 × 106 cells/l); CD8+ T cell count, 690 × 106 cells/l (520–860 × 106 cells/l); and HIV RNA load, 34 300 copies/ml (5845–122 500 copies/ml). Blood samples were obtained in periods without any acute infection or exacerbation of chronic infection. For comparison, 26 HIV-seronegative healthy controls (median age 38 years; range, 19–50 years; 18 men and eight women) were also included in the study. In another group of HIV-infected patients (n = 12, median age 45 years; range 24–57 years; 11 men and one woman) bone marrow aspirates were obtained before and 4 and 26 weeks after initiating HAART. Before start of therapy, median laboratory values (interquartile range) were as follows: CD4+ T cell count, 190 × 106 cells/l (135–210 × 106 cells/l); CD8+ T cell count, 780 × 106 cells/l (605–1230 × 106 cells/l); and HIV RNA load, 71 050 copies/ml (12 637–684 750 copies/ml). Informed consent for blood and bone marrow sampling was obtained from all study participants. The study was conducted in accordance with the ethical guidelines at our hospital and the Helsinki Declaration and was approved by the hospital authorities.
Blood sampling protocol
Blood samples were drawn into pyrogen-free blood collection tubes without any additives (Becton Dickinson, San Jose, CA, USA), immersed immediately in melting ice, and allowed to clot for 1 h before centrifugation (1000 g for 10 min). Serum specimens were stored at −80°C and were thawed less than three times.
Bone marrow culture
Heparinized bone marrow samples were obtained by aspiration from the posterior iliac crest and mononuclear cells (MNC) were prepared by density gradient centrifugation (Lymphoprep; Nycomed Pharma, Oslo, Norway). MNC from bone marrow aspirates were incubated in flat-bottomed 96-well trays (2 × 106/ml; Costar, Cambridge, MA, USA), in medium alone [RPMI-1640 with 2 mM l-glutamine and 25 mM HEPES buffer (Gibco, Paisley, UK) supplemented with 10% of fetal calf serum (FCS); Sigma, St Louis, MO, USA)] or stimulated with phytohaemagglutinin (PHA); final dilution 1 : 100; Murex, Dartford, UK). After 24 h, cell-free supernatants were harvested and stored at −80°C until analysed. The concentration of PHA was based on previous dose–response experiments (data not shown).
Whole blood culture
Venous blood was collected into sterile glass tubes (BD Vacutainer; Becton Dickinson, Franklin Lakes, NJ, USA) containing Lepuridin (final concentration 50 μg/ml; Hoechst, Frankfurt am Main, Germany). The blood sample was aliquoted (1 ml) into polypropylene tubes (NUNC A/S, Roskilde, Denmark), capped and incubated at 37°C under constant tilting with or without tumour necrosis factor (TNF)-α (10 ng/ml; R&D Systems, Minneapolis, MN, USA), recombinant HIV-1 tat protein (rHIV-tat; 5 μg/ml; ImmunoDiagnostics, Inc., Woburn, MA, USA), lipopolysaccharide from Escherichia coli O26:B6 (LPS; 10 ng/ml; Sigma), or a combination of TNF-α and rHIV-tat. After 6 h of incubation, the samples were centrifuged (2500 g for 10 min at 4°C) and plasma was stored at −80°C until analysed.
Isolation and stimulation of peripheral blood mononuclear cells (PBMC)
PBMC, obtained from heparinized blood by Isopaque-Ficoll (Lymphoprep; Nycomed Pharma) gradient centrifugation, were incubated in flat-bottomed 96-well trays (2 × 106/ml; Costar) in medium alone [RPMI-1640 with 2 mM l-glutamine and 25 mM HEPES buffer (PAA Laboratories, Pasching, Austria) supplemented with 10% FCS (PAA Laboratories)] or stimulated with PHA (Murex; final dilution 1:200) or LPS from Escherichia coli O26:B6 (Sigma; final concentration 10 ng/ml). Cell-free supernatants were harvested after 24 and 72 h and stored at −80°C until analysed.
Enzyme-linked immunoassay (ELISA) for detection of NGAL
An ELISA specific for NGAL was developed by coating microtitre plates (96-well ½ area; Costar) overnight at room temperature with a rabbit affinity-purified anti-NGAL antibody (developed by Trude H. Flo with protein provided generously by Dr Roland Strong, FHCRC, Seattle, WA, USA). Plates were blocked with buffer containing 1% bovine serum albumin (BSA; PAA Laboratories). Samples (25 μl) or standards (NGAL concentrations ranging from 0·078 to 10 ng/ml, R&D Systems) were added to each well and incubated for 2 h. For detection, incubation with a biotinylated mouse monoclonal antibody raised against NGAL (no. HYB211-05; Antibody Shop, Gentofte, Denmark) were followed by avidin-conjugated horseradish peroxidase (R&D Systems). Tetramethylbenzidine substrate (Zymed, San Francisco, CA, USA) was added for colour development, which was read after 20 min at 450 nm against 540 nm with a microplate reader (Multiskan RC; Labsystems OY, Helsinki, Finland). The detection limit of the assay was 0·06 ng/ml and the intra- and interassay coefficient of variation was < 6%. NGAL may be found in complex with metalloproteinase 9 (MMP-9), but there was no cross-reactivity with MMP-9 in the current ELISA.
Miscellaneous
Plasma HIV RNA levels were measured by quantitative reverse polymerase chain reaction (Amplicor HIV Monitor; Roche Diagnostic Systems, Branchburg, NJ, USA). The limit of detection was 200 copies/ml plasma. Neutrophil counts were determined using Cell-Dyn 4000 (Abbott Laboratories, Abbott Park, IL, USA).
Statistical analysis
Differences between two groups were compared using the Mann–Whitney U-test for unpaired data. The Wilcoxon signed-rank test was used for comparison of paired data. Coefficients of correlation were calculated by Spearman's rank test. Probability was two-sided and considered to be significant when P < 0·05.
Results
Serum levels of NGAL during HAART
Before initiating HAART, the HIV-infected patients (n = 37) had significantly decreased serum levels of NGAL compared with healthy controls (n = 21) (Fig. 1). During HAART, there was a pronounced fall in virus load and a marked increase in CD4+ T cell counts (data not shown). Notably, these changes were accompanied by a gradual and significant increase in NGAL concentrations reaching levels comparable to those in healthy controls after 12 months of therapy (Fig. 1).
Fig. 1.
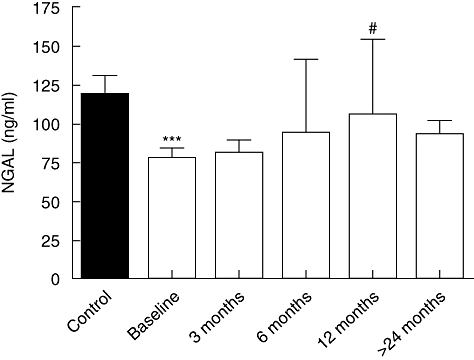
Serum levels of neutrophil gelatinase-associated lipocalin (NGAL) in 21 healthy controls (ctr) and 37 human immunodeficiency virus (HIV)-infected patients at baseline and after different time-points after initiating highly active anti-retroviral therapy (HAART). Data are mean ± standard deviation. Differences between patients and controls were compared using the Mann–Whitney U-test for unpaired data. The Wilcoxon signed-rank test was used for comparison of paired data during HAART. ***P < 0·001 versus controls; #P < 0·05 versus baseline.
NGAL levels in relation to virological response during HAART
To examine the relationship between virological response and NGAL levels during HAART, the patients were classified as virological responders (plasma HIV RNA level < 200 copies/ml; n = 26) and non-responders (plasma HIV RNA level >200 copies/ml; n = 11) after 24 months of therapy. At baseline there were no significant differences in viral load, history of anti-retroviral treatment or CD4+ and CD8+ T cell count between these two groups of patients. However, while there was a significant increase in NGAL levels during HAART in virological responders (P < 0·05 versus baseline after 12 months of therapy), this was not seen in non-responders (Fig. 2). In contrast, NGAL levels were not related to immunological responses during HAART, as assessed by changes in CD4+ T cell counts (data not shown).
Fig. 2.
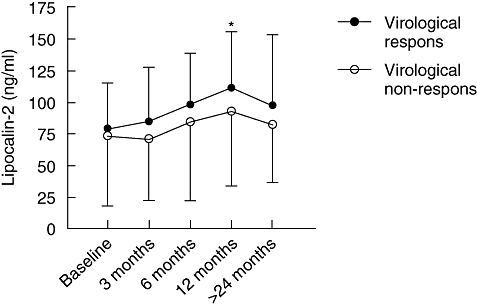
Serum levels of neutrophil gelatinase-associated lipocalin (NGAL) in virological responders (n = 26) and non-responders (n = 11) before (baseline) and at different time-points after initiating highly active anti-retroviral therapy (HAART). Data are mean ± standard deviation. The Wilcoxon-signed rank test was used for comparison of paired data during HAART. *P < 0·05 versus baseline levels.
NGAL levels in bone marrow culture during HAART
Bone marrow cells have been reported to synthesize NGAL [14], and therefore we examined next the release of NGAL in MNC from bone marrow aspirates in 12 HIV-infected patients before and 4 and 26 weeks after initiating HAART and in six healthy controls. As reported previously [15], bone marrow cellularity was within normal limits in all patients before start of therapy and no significant changes were observed during HAART (erythropoietic cells represented 15–35%, lymphopoietic cells < 15% and myelopoietic cells 50–70% of the nucleated cells in bone marrow aspirates from all patients). As shown in Fig. 3, MNC from bone marrow aspirates released large amounts of NGAL in both HIV-infected patients and controls, reaching maximum after culturing for 72 h. However, while PHA induced a marked increase in NGAL levels in healthy controls, the PHA-mediated NGAL response was somewhat modest in untreated HIV-infected patients. In fact, after culturing for 72 h, the NGAL levels tended to decrease after PHA stimulation in these patients (Fig. 3a). Moreover, while there was no or only a modest increase in PHA-stimulated NGAL release compared with unstimulated levels at baseline and after 4 weeks on HAART, bone marrow aspirates from these patients showed a marked PHA-mediated NGAL release after 26 weeks of therapy with a similar pattern after culturing for 24 and 72 h (Fig. 3b).
Fig. 3.
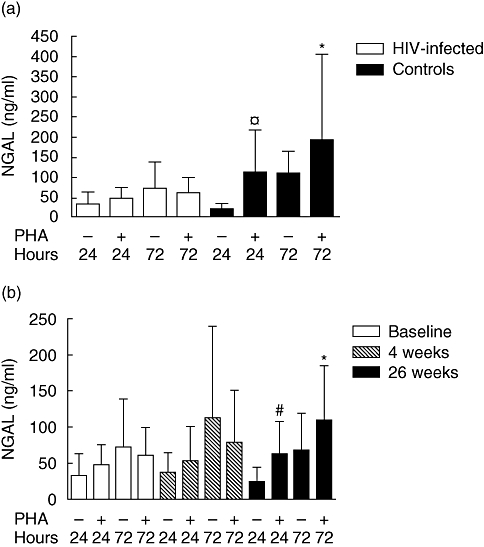
(a) Neutrophil gelatinase-associated lipocalin (NGAL) levels in unstimulated and phytohaemagglutinin (PHA)-stimulated mononuclear cells (MNC) from 12 human immunodeficiency virus (HIV)-infected patients without highly active anti-retroviral therapy (HAART) and six healthy controls after culturing for 24 and 72 h. Data are mean ± standard deviation. Differences between patients and controls were compared using the Mann–Whitney U-test for unpaired data. *P < 0·05 and  P = 0·1 versus PHA-stimulated release in HIV-infected patients after culturing for 72 and 24 h, respectively. (b) NGAL levels in unstimulated and PHA-stimulated MNC from 12 HIV-infected patients at different time-points after initiating HAART after culturing for 24 and 72 h. Data are mean ± standard deviation. The Wilcoxon signed-rank test was used for comparison of paired data during HAART. *P < 0·02 and #P < 0·07 versus baseline comparing the difference between PHA and unstimulated responses.
P = 0·1 versus PHA-stimulated release in HIV-infected patients after culturing for 72 and 24 h, respectively. (b) NGAL levels in unstimulated and PHA-stimulated MNC from 12 HIV-infected patients at different time-points after initiating HAART after culturing for 24 and 72 h. Data are mean ± standard deviation. The Wilcoxon signed-rank test was used for comparison of paired data during HAART. *P < 0·02 and #P < 0·07 versus baseline comparing the difference between PHA and unstimulated responses.
Release of NGAL in whole blood culture
We next examined the ability of different stimuli with relevance to HIV infection to induce NGAL release in whole blood culture from six healthy controls. As seen in Fig. 4, while TNF-α (10 ng/ml) induced a marked increase in NGAL release after culturing for 6 h, the response to LPS (10 ng/ml) and rHIV-tat (5 μg/ml) stimulation was more modest, with no further enhancement of the TNF-α-mediated NGAL response when this stimulus was combined with rHIV-tat. The same pattern of NGAL response was seen in HIV-infected patients (n = 8; four on HAART and four without therapy), irrespectively, on ongoing HAART (data not shown), suggesting that the neutrophil-mediated NGAL release respond adequately to these stimuli in HIV-infected individuals. In contrast to the marked NGAL release in whole blood cultures, there was no release of NGAL from PBMC activated by LPS (10 ng/ml) and PHA (final dilution 1 : 100) for 24 and 72 h in either patients or controls (data not shown).
Fig. 4.
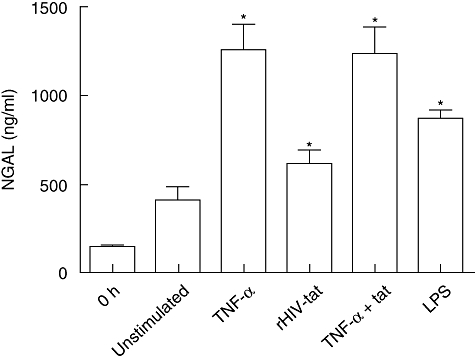
The release of neutrophil gelatinase-associated lipocalin (NGAL) in unstimulated (unstim) and tumour necrosis factor (TNF)-α (10 ng/ml), recombinant human immunodeficiency virus (rHIV)-tat (5 μg/ml), lipopolysaccharide (10 ng/ml) and TNF-α + rHIV-tat-stimulated whole blood culture after culturing for 6 h in six healthy controls. Data are mean ± standard error of the mean. The Wilcoxon signed-rank test was used for comparison of paired data. *P < 0·05 versus levels in unstimulated samples.
NGAL in relation to neutrophils
Neutrophils are known to be a major cellular source of NGAL in human circulation [3,14], and within the HIV-infected patients there was a significant positive correlation between neutrophil counts and NGAL levels at baseline (r = 0·45, P < 0·05) as well as at all time-points during HAART, as illustrated by a representative correlation plot after 12 months of therapy (Fig. 5). Moreover, the numbers of neutrophils showed a similar pattern as for serum levels of NGAL, with increasing levels during HAART (Table 1). In contrast, there was no significant correlation between neutrophil counts and NGAL within the healthy control group (r = 0·22, P = 0·208).
Fig. 5.
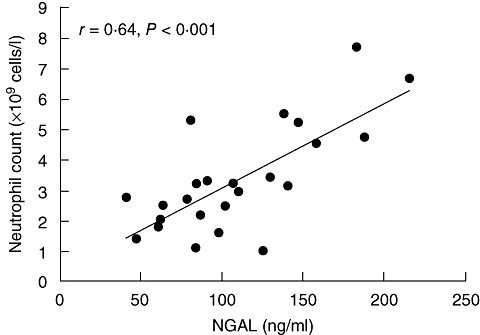
The correlation (Spearman's rank test) between serum levels of neutrophil gelatinase-associated lipocalin (NGAL) and neutrophil count in human immunodeficiency virus-infected patients at 12 months after initiating highly active anti-retroviral therapy.
Table 1.
Neutrophil counts in peripheral blood in human immunodeficiency virus (HIV)-infected patients (n = 24) before and at various time-points during highly active anti-retroviral therapy.
| Neutrophil count (109/l) | |||
|---|---|---|---|
| Total* | VL < 200 | VL > 200 | |
| Baseline | 2·20 ± 1·79 | 2·61 ± 2·19 | 1·50 ± 0·60 |
| 3 months | 2·61 ± 2·01 | 2·71 ± 2·31 | 2·37 ± 0·96 |
| 6 months | 2·93 ± 1·75 | 3·18 ± 1·93 | 2·28 ± 1·02 |
| 12 months | 3·35 ± 1·75 | 3·35 ± 1·71 | 3·37 ± 2·01 |
| 24 months | 3·08 ± 1·39 | 3·12 ± 1·45 | 2·96 ± 1·31 |
Data for virological responders (n = 17) and non-responders (n = 7), defined as viral load (VL) < or >200 HIV RNA copies/ml plasma after 24 months of therapy, respectively, are given separately.
Neutrophil counts were not available in all patients. Data are mean ± standard deviation.
Discussion
NGAL has been proposed previously to be involved in various inflammatory and infectious conditions [3]. In the present study we report decreased NGAL levels in untreated HIV-infected patients with a trend towards normalization during HAART, with a similar pattern in serum and bone marrow aspirates. These findings suggest that dysregulated NGAL levels should be added to the list of abnormalities that characterize immunodeficient HIV-infected patients. It also underscores the involvement of neutrophils and innate immune responses in HIV-related immunodeficiency.
Expression of NGAL in epithelial cells, as well as release from granulocytes, has been found to be induced strongly during inflammation, as also suggested by the present study showing a marked TNF-α-mediated NGAL release in whole blood culture. This association between inflammation and NGAL is also supported by clinical studies demonstrating increased circulating NGAL levels in various inflammatory conditions, such as ischaemic cardiovascular disorders [16] and autoimmune diseases [4,17,18]. There have also been some reports of markedly raised serum levels of NGAL during bacterial infections, correlated significantly with other inflammatory markers (e.g. C-reactive protein) [19]. HIV-related immunodeficiency is characterized by persistently raised levels of inflammatory cytokines such as TNF-α[20], and our finding of decreased NGAL levels in untreated HIV-infected patients may apparently seem to be in conflict with previous studies, suggesting a link between inflammation and raised NGAL levels. However, as the plasma level of NGAL may be a reliable parameter of neutrophil activation, superior to other markers such as lactoferrin and myeloperoxidase [21,22], it is possible that the decreased NGAL levels in immunodeficient HIV-infected patients could reflect decreased function and/or numbers of neutrophils. Indeed, impaired neutrophil chemotaxis and killing activity as well as defective neutrophil degranulation in response to inflammatory stimuli have been found previously in HIV-infected patients [23,24].
NGAL may be released by epithelial cells, renal tubular cells and hepatocytes during inflammation or injury, and has been found to be expressed in endothelial cells, smooth muscle cells and macrophages in atherosclerotic plaques, as well as in adipose tissue [5,16,25], However, neutrophils have been known as the major cellular source of serum levels of NGAL, and in the present study we found a significant correlation between NGAL and numbers of neutrophils at all time-points during HAART. However, although serum levels of NGAL in HIV-infected patients were correlated with neutrophil counts, this does not exclude that the NGAL release from neutrophils could, at least partly, also reflect the function of these cells. Furthermore, we found no significant correlation between NGAL levels and numbers of neutrophils within the control group, suggesting further that serum levels of NGAL are not merely a reflection of neutrophil counts. Finally, the marked release of NGAL in activated bone marrow cells may suggest other cellular sources of NGAL than circulating neutrophils. However, our data are linked only indirectly to serum levels, and at present we have no firm information on the cellular source of NGAL in HIV infection.
In bone marrow, NGAL is synthesized almost exclusively in myelocytes and metamyelocytes [14]. While granules that are acquired at the myeloblast and promyelocyte stage may be found in either granulocytes or monocytes, specific granules that are formed at the myelocyte–metamyelocyte stage are found only in cells of the granulocyte linage [2,21]. Previously, we have reported decreased proportions of CD34+ cells with myeloid-associated surface molecules (myeloid progenitors) in bone marrow from immunodeficient HIV-infected patients [15]. Although PHA may activate myeloid progenitors only indirectly in the bone marrow suspension [26], our findings in the present study with decreased PHA-stimulated NGAL release in MNC cells from bone marrow aspirates in untreated HIV-infected patients further suggest impaired bone marrow myelopoiesis in these patients, at least partly involving defective myelocyte-metamyelocyte maturation. It has been reported previously that HAART improves anti-microbial and secretory activity of neutrophils in HIV-infected patients [27], as well as increases in neutrophil counts by reversal of viral suppression on multi-lineage haematopoiesis in bone marrow [28]. Whether the increase in NGAL levels during HAART reflects improved synthesis, increased neutrophil counts, enhanced capacity of these cells to release NGAL upon activation, improved bone marrow function or a combination thereof will have to be investigated further.
Recent studies in lipocalin-2-deficient mice suggest that a mouse homologue to NGAL, 24p3, may limit bacterial growth by iron sequestration, and the absence of this defence mechanism can lead to sepsis and death in these animals [10]. This defect can be mimicked in wild-type mice by providing siderophore iron, which cannot be sequestered by NGAL, testifying to the specific role of NGAL as a siderophore binding protein in innate immunity [10]. Moreover, although the role of NGAL in innate immune responses in man is far from clear, some recent in vitro studies also suggest that NGAL may have growth-inhibiting effects on bacteria through its ability to bind siderophores [11]. AIDS patients exhibit abnormalities in the metabolism of iron [29], which may contribute to an increased susceptibility of AIDS patients to bacterial infections. However, although it is tempting to hypothesize that the decreased serum levels of NGAL observed in untreated HIV-infected patients may be associated with a higher risk of infections with certain bacteria, possibly also predisposing to a more serious course, the role of NGAL in innate immune responses in human is far from clear.
In the present study we show for the first time decreased NGAL levels in immunodeficient HIV-infected patients, potentially reflecting decreased number and function of neutrophils as well as impaired bone marrow myelopoiesis. Importantly, these abnormalities were reversed by successful HAART. Our findings underscore the involvement of neutrophils and innate immunity in the HIV-related immunodeficiency. Forthcoming studies should examine further the cellular source of NGAL in HIV infection as well as whether the decreased NGAL levels in untreated HIV-infected patients could contribute to their impaired anti-microbial defence.
Acknowledgments
This work was supported by grants from the Research Council of Norway, University of Oslo and the Medinnova Foundation. We thank Azita Rashidi for excellent technical assistance.
References
- 1.Akerstrom B, Flower DR, Salier JP. Lipocalins: unity in diversity. Biochim Biophys Acta. 2000;1482:1–8. doi: 10.1016/s0167-4838(00)00137-0. [DOI] [PubMed] [Google Scholar]
- 2.Kjeldsen L, Bainton DF, Sengelov H, Borregaard N. Identification of neutrophil gelatinase-associated lipocalin as a novel matrix protein of specific granules in human neutrophils. Blood. 1994;83:799–807. [PubMed] [Google Scholar]
- 3.Borregaard N, Cowland JB. Neutrophil gelatinase-associated lipocalin, a siderophore-binding eukaryotic protein. Biometals. 2006;19:211–15. doi: 10.1007/s10534-005-3251-7. [DOI] [PubMed] [Google Scholar]
- 4.Xu S, Venge P. Lipocalins as biochemical markers of disease. Biochim Biophys Acta. 2000;1482:298–307. doi: 10.1016/s0167-4838(00)00163-1. [DOI] [PubMed] [Google Scholar]
- 5.Friedl A, Stoesz SP, Buckley P, Gould MN. Neutrophil gelatinase-associated lipocalin in normal and neoplastic human tissues. Cell type-specific pattern of expression. Histochem J. 1999;31:433–41. doi: 10.1023/a:1003708808934. [DOI] [PubMed] [Google Scholar]
- 6.Draper DW, Bethea HN, He YW. Toll-like receptor 2-dependent and -independent activation of macrophages by group B streptococci. Immunol Lett. 2006;102:202–14. doi: 10.1016/j.imlet.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi F, Smith KD, Ozinsky A, et al. The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature. 2001;410:1099–103. doi: 10.1038/35074106. [DOI] [PubMed] [Google Scholar]
- 8.Poltorak A, He X, Smirnova I, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282:2085–8. doi: 10.1126/science.282.5396.2085. [DOI] [PubMed] [Google Scholar]
- 9.Sengelov H, Boulay F, Kjeldsen L, Borregaard N. Subcellular localization and translocation of the receptor for N-formylmethionyl-leucyl-phenylalanine in human neutrophils. Biochem J. 1994;299:473–9. doi: 10.1042/bj2990473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flo TH, Smith KD, Sato S, et al. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature. 2004;432:917–21. doi: 10.1038/nature03104. [DOI] [PubMed] [Google Scholar]
- 11.Goetz DH, Holmes MA, Borregaard N, Bluhm ME, Raymond KN, Strong RK. The neutrophil lipocalin NGAL is a bacteriostatic agent that interferes with siderophore-mediated iron acquisition. Mol Cell. 2002;10:1033–43. doi: 10.1016/s1097-2765(02)00708-6. [DOI] [PubMed] [Google Scholar]
- 12.Pantaleo G, Fauci AS. Immunopathogenesis of HIV infection. Annu Rev Microbiol. 1996;50:825–54. doi: 10.1146/annurev.micro.50.1.825. [DOI] [PubMed] [Google Scholar]
- 13.Kuritzkes DR. Neutropenia, neutrophil dysfunction, and bacterial infection in patients with human immunodeficiency virus disease: the role of granulocyte colony-stimulating factor. Clin Infect Dis. 2000;30:256–60. doi: 10.1086/313642. [DOI] [PubMed] [Google Scholar]
- 14.Borregaard N, Sehested M, Nielsen BS, Sengelov H, Kjeldsen L. Biosynthesis of granule proteins in normal human bone marrow cells. Gelatinase is a marker of terminal neutrophil differentiation. Blood. 1995;85:812–17. [PubMed] [Google Scholar]
- 15.Muller F, Tjonnfjord GE, Nordoy I, et al. Immunophenotypic analyses of CD34(+) cell subsets in bone marrow from HIV-infected patients during highly-active antiretroviral therapy. Eur J Clin Invest. 2002;32:535–40. doi: 10.1046/j.1365-2362.2002.00995.x. [DOI] [PubMed] [Google Scholar]
- 16.Hemdahl AL, Gabrielsen A, Zhu C, et al. Expression of neutrophil gelatinase-associated lipocalin in atherosclerosis and myocardial infarction. Arterioscler Thromb Vasc Biol. 2006;26:136–42. doi: 10.1161/01.ATV.0000193567.88685.f4. [DOI] [PubMed] [Google Scholar]
- 17.Biezeveld MH, van Mierlo G, Lutter R, et al. Sustained activation of neutrophils in the course of Kawasaki disease: an association with matrix metalloproteinases. Clin Exp Immunol. 2005;141:183–8. doi: 10.1111/j.1365-2249.2005.02829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mallbris L, O'Brien KP, Hulthen A, et al. Neutrophil gelatinase-associated lipocalin is a marker for dysregulated keratinocyte differentiation in human skin. Exp Dermatol. 2002;11:584–91. doi: 10.1034/j.1600-0625.2002.110611.x. [DOI] [PubMed] [Google Scholar]
- 19.Xu SY, Pauksen K, Venge P. Serum measurements of human neutrophil lipocalin (HNL) discriminate between acute bacterial and viral infections. Scand J Clin Lab Invest. 1995;55:125–31. doi: 10.3109/00365519509089604. [DOI] [PubMed] [Google Scholar]
- 20.Aukrust P, Liabakk NB, Muller F, Lien E, Espevik T, Froland SS. Serum levels of tumor necrosis factor-alpha (TNF alpha) and soluble TNF receptors in human immunodeficiency virus type 1 infection − correlations to clinical, immunologic, and virologic parameters. J Infect Dis. 1994;169:420–4. doi: 10.1093/infdis/169.2.420. [DOI] [PubMed] [Google Scholar]
- 21.Borregaard N, Cowland JB. Granules of the human neutrophilic polymorphonuclear leukocyte. Blood. 1997;89:3503–21. [PubMed] [Google Scholar]
- 22.Paulsson J, Dadfar E, Held C, Jacobson SH, Lundahl J. Activation of peripheral and in vivo transmigrated neutrophils in patients with stable coronary artery disease. Atherosclerosis. 2007;192:328–34. doi: 10.1016/j.atherosclerosis.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Ellis M, Gupta S, Galant S, et al. Impaired neutrophil function in patients with AIDS or AIDS-related complex: a comprehensive evaluation. J Infect Dis. 1988;158:1268–76. doi: 10.1093/infdis/158.6.1268. [DOI] [PubMed] [Google Scholar]
- 24.Roilides E, Mertins S, Eddy J, Walsh TJ, Pizzo PA, Rubin M. Impairment of neutrophil chemotactic and bactericidal function in children infected with human immunodeficiency virus type 1 and partial reversal after in vitro exposure to granulocyte–macrophage colony-stimulating factor. J Pediatr. 1990;117:531–40. doi: 10.1016/s0022-3476(05)80684-5. [DOI] [PubMed] [Google Scholar]
- 25.Kratchmarova I, Kalume DE, Blagoev B, et al. A proteomic approach for identification of secreted proteins during the differentiation of 3T3-L1 preadipocytes to adipocytes. Mol Cell Proteomics. 2002;1:213–22. doi: 10.1074/mcp.m200006-mcp200. [DOI] [PubMed] [Google Scholar]
- 26.Reid CD, Stackpoole A, Meager A, Tikerpae J. Interactions of tumor necrosis factor with granulocyte–macrophage colony-stimulating factor and other cytokines in the regulation of dendritic cell growth in vitro from early bipotent CD34+ progenitors in human bone marrow. J Immunol. 1992;149:2681–8. [PubMed] [Google Scholar]
- 27.Monari C, Casadevall A, Baldelli F, et al. Normalization of anti-cryptococcal activity and interleukin-12 production after highly active antiretroviral therapy. AIDS. 2000;14:2699–708. doi: 10.1097/00002030-200012010-00009. [DOI] [PubMed] [Google Scholar]
- 28.Huang SS, Barbour JD, Deeks SG, et al. Reversal of human immunodeficiency virus type 1-associated hematosuppression by effective antiretroviral therapy. Clin Infect Dis. 2000;30:504–10. doi: 10.1086/313714. [DOI] [PubMed] [Google Scholar]
- 29.Boelaert JR, Weinberg GA, Weinberg ED. Altered iron metabolism in HIV infection: mechanisms, possible consequences, and proposals for management. Infect Agents Dis. 1996;5:36–46. [PubMed] [Google Scholar]


