Abstract
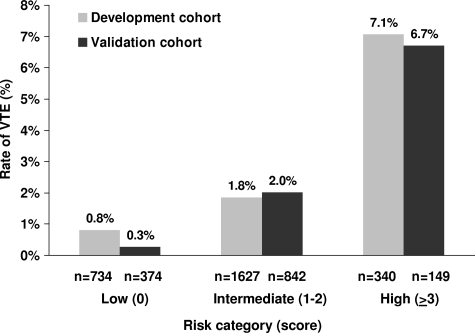
Risk of venous thromboembolism (VTE) is elevated in cancer, but individual risk factors cannot identify a sufficiently high-risk group of outpatients for thromboprophylaxis. We developed a simple model for predicting chemotherapy-associated VTE using baseline clinical and laboratory variables. The association of VTE with multiple variables was characterized in a derivation cohort of 2701 cancer outpatients from a prospective observational study. A risk model was derived and validated in an independent cohort of 1365 patients from the same study. Five predictive variables were identified in a multivariate model: site of cancer (2 points for very high-risk site, 1 point for high-risk site), platelet count of 350 × 109/L or more, hemoglobin less than 100 g/L (10 g/dL) and/or use of erythropoiesis-stimulating agents, leukocyte count more than 11 × 109/L, and body mass index of 35 kg/m2 or more (1 point each). Rates of VTE in the derivation and validation cohorts, respectively, were 0.8% and 0.3% in low-risk (score = 0), 1.8% and 2% in intermediate-risk (score = 1-2), and 7.1% and 6.7% in high-risk (score ≥ 3) category over a median of 2.5 months (C-statistic = 0.7 for both cohorts). This model can identify patients with a nearly 7% short-term risk of symptomatic VTE and may be used to select cancer outpatients for studies of thromboprophylaxis.
Introduction
Cancer and antineoplastic therapy are frequently complicated by the development of venous thromboembolism (VTE). Several risk factors for cancer-associated VTE have been described in recent studies and include primary site of cancer, presence of metastatic disease, and use of antineoplastic therapy including chemotherapy, hormonal therapy, surgery, and erythropoiesis-stimulating agents.1–4 Cancer patients on active therapy are at greatest risk for development of VTE. In a population-based study, cancer was associated with a 4.1-fold greater risk of thrombosis, whereas the use of chemotherapy increased the risk 6.5-fold.5,6 In women with stage II breast cancer, the risk of VTE decreases dramatically after chemotherapy is completed.7,8 The occurrence of VTE has important implications for the cancer patient including requirement for chronic anticoagulation, possible delays in delivering chemotherapy, a high risk of recurrent VTE, risk of bleeding complications on anticoagulation, decreased quality of life, and consumption of health care resources.9,10 Furthermore, cancer patients with VTE have a 2-fold or greater increase in mortality compared with cancer patients without VTE, even after adjusting for stage.11,12 Indeed, thromboembolism is a leading cause of death in cancer patients.13
Primary VTE prophylaxis can reduce deep vein thrombosis (DVT), pulmonary embolism (PE), and fatal PE in several high-risk populations such as hospitalized patients or in the postoperative setting.14–18 In the cancer population, identification of patients most at risk for VTE followed by institution of effective prophylaxis could improve morbidity, mortality, delivery of cancer therapy, cancer-related outcomes, quality of life, and use of health care resources. Clinical trials of thromboprophylaxis have been conducted in cancer outpatients selected by individual risk factors, such as metastatic breast and lung cancer or presence of intravenous catheters.19–22 However, with a single exception,19 these studies have not shown a benefit for primary thromboprophylaxis. Current consensus guidelines do not recommend prophylaxis in cancer outpatients.23,24
To reduce the burden and consequences of VTE, it is therefore important to identify a population of cancer patients at highest risk for VTE that would benefit from thromboprophylaxis. A rate of symptomatic VTE of approximately 5% to 7% would be similar or greater than that reported in hospitalized or postoperative patients for whom VTE prophylaxis has been shown to be highly effective.25–27 Formal risk assessment models for DVT and PE in other populations have been developed and are used clinically.28–34 However, no such risk models exist for the cancer population.
We therefore developed a simple risk model for predicting rates of VTE using data from a multicenter prospective observational study of cancer outpatients receiving chemotherapy, using baseline clinical and laboratory variables. We also performed a validation of this model in an independent cohort of patients derived from the same observational study.
Methods
Study population
The study population comprised consecutively enrolled patients in the Awareness of Neutropenia in Chemotherapy (ANC) Study Group Registry, an observational study of cancer patients initiating a new chemotherapy regimen at 115 sites within the United States, balanced for practice volume and geographic location. Detailed methodology as well as frequency and risk factors for VTE in a preliminary analysis of this study have previously been reported.2 Briefly, patients were followed prospectively for a maximum of 4 cycles of chemotherapy. Patients enrolled between March 2002 and October 2005 who had completed at least one cycle were included in this analysis. The study was approved by a central institutional review board (IRB) as well as the University of Rochester IRB.
Patients were required to have a histologically confirmed diagnosis of cancer, with targeted enrollment of specific tumor types (breast, lung, ovarian, sarcoma, colon, and lymphomas), although eligible patients with other primary sites were allowed on study. Patients were also required to be at the start of a new chemotherapy regimen, expected to complete 4 cycles of chemotherapy, be age 18 years or older with no upper age limit, and to provide informed consent in accordance with the Delcaration of Helsinki. Patients were excluded if they were receiving concurrent cytotoxic, biologic, or immunologic therapy for other conditions, or continuous single-agent chemotherapy, if they had a diagnosis of acute leukemia, were pregnant or lactating, had an active infection requiring treatment, were currently participating in a double-blinded study, or had received stem cell transplant. VTE was diagnosed by the treating clinician. Arterial thrombotic events were not included. Only 3% of patients were lost to follow-up.
Derivation of model
Model derivation and validation were based on a split-sample method. Two-thirds of the study participants were randomly assigned to a model derivation cohort (n = 2701), and one-third (n = 1365) were reserved as an independent validation cohort. Both cohorts were compared with respect to clinical and laboratory variables.
The model was developed based on data from the derivation cohort only. Clinical variables known to be associated with VTE as well as potential risk factors including patient demographics, performance status, ethnicity, site and stage of cancer, type of chemotherapy, body mass index (BMI), comorbid conditions including history of myocardial infarction, peripheral vascular disease, recurrent infections, liver disease, pulmonary disease, diabetes mellitus and connective tissue disorders, recent surgery, use of prophylactic myeloid growth factors, prior use of chemotherapy, use of diuretics, use of corticosteroids, and available baseline laboratory variables including complete blood count and liver function tests were considered. Variables measured after the initiation of chemotherapy such as the occurrence of infection or hospitalization were excluded since the goal was to identify high-risk patients prior to starting therapy. All covariates were assessed for missing values that were grouped with either the largest category or the category with a similar relation to outcome. Among variables considered during initial analysis, missing values were rare. Serum albumin had the most missing values (n = 125, 3.1%). For numeric variables, platelet count and hemoglobin level were categorized on the basis of a prior analysis,2 while other laboratory variables were categorized based on elevation beyond the upper limit of standard reference values.35 Variables were evaluated in univariate analysis using a χ2 test. A multivariate logistic regression model was developed using a stepwise selection process. Variables associated with an increased risk of VTE (P ≤ .10) in univariate analysis as well as variables selected a priori based on known relevance were included in the pool of variables for the forward stepwise regression model. Primary site of cancer and stage of disease were built into the model at every step. Hemoglobin and use of erythropoiesis-stimulating agents (ESAs) were combined into one variable based on prior analysis.2 To avoid model instability, we required covariates to have an individual category sample size of at least 75 patients. The covariates in the final model were evaluated for collinearity, using the variance inflation factor (VIF). First-order interaction terms were explored in the final model between the primary site of cancer and all other variables in the model. No significant interactions were found. A risk score was developed based on regression coefficients from the final multivariate model.
Validation of model
Once the final model was developed, it was assessed in the separate validation cohort of 1365 patients. The predictive accuracy of the model was assessed using tests for discrimination and calibration. Model discrimination performance was evaluated using the standard measures of sensitivity, specificity, and predictive value. For overall assessment, discrimination was evaluated using the c-statistic representing the area under the receiver operating characteristic curve with larger values indicating better discrimination. The Hosmer-Lemeshow statistic was used to assess model calibration or its fit to the data based on agreement between predicted risk score probabilities using the model and the actual observed probabilities. Statistical analysis was conducted using SAS statistical software (SAS Institute, Cary, NC).
Results
Patient characteristics
The study population comprised 4066 patients, split into 2701 patients in the derivation cohort and 1365 patients in the validation cohort. Overall, 88 patients (2.2%) developed VTE over a median follow up of 73 days, (range, 5-364 days). There were 65 reported venous thrombotic events (1.6%) and 27 embolic events (0.7%), including 4 patients with both. Seventy-five percent of VTE events occurred in the first 2 cycles. General characteristics of the derivation and validation cohorts are presented in Table 1. Patient characteristics in the 2 cohorts were well balanced, with the exception of recent history of surgery.
Table 1.
Characteristics of patients in the derivation and validation cohorts
| Category | Derivation cohort, no. (%) | Validation cohort, no. (%) | P |
|---|---|---|---|
| All patients | 2701 (100) | 1365 (100) | |
| All VTE | 60 (2.2) | 28 (2.1) | .72 |
| Age | .14 | ||
| Younger than 65 y | 1618 (59.9) | 850 (62.3) | |
| 65 y or older | 1083 (40.1) | 515 (37.7) | |
| Sex | .66 | ||
| Male | 882 (32.7) | 455 (33.3) | |
| Female | 1819 (67.3) | 910 (66.7) | |
| Performance status, ECOG | .54 | ||
| 0 to 1 | 2473 (91.6) | 1242 (91.0) | |
| 2 to 4 | 228 (8.4) | 123 (9.0) | |
| Primary site of cancer | .13 | ||
| Breast | 935 (34.6) | 472 (34.6) | |
| Colorectal | 297 (11.0) | 163 (11.9) | |
| Lung | 554 (20.5) | 236 (17.3) | |
| Gynecologic | 259 (9.6) | 142 (10.40) | |
| Gastric and pancreatic | 54 (2.0) | 19 (1.4) | |
| Lymphoma | 328 (12.1) | 184 (13.5) | |
| Other sites | 274 (10.1) | 149 (10.9) | |
| Stage | .06 | ||
| 1 to 3 | 1653 (61.2) | 873 (64.0) | |
| 4 | 997 (36.9) | 477 (34.9) | |
| Unknown | 51 (1.9) | 15 (1.1) | |
| Prior chemotherapy | 645 (23.9) | 306 (22.4) | .3 |
| Comorbidities | |||
| Cerebrovascular disease | 54 (2.0) | 23 (1.7) | .49 |
| Moderate or severe renal disease | 27 (1.0) | 18 (1.3) | .36 |
| Chronic pulmonary disease | 217 (8.0) | 110 (8.1) | .98 |
| Surgery within past month | 829 (30.7) | 473 (34.7) | .01 |
| Diabetes mellitus | 312 (11.6) | 169 (12.4) | .44 |
| BMI 35 kg/m2 or more | 332 (12.3) | 166 (12.2) | .90 |
| Baseline laboratory values | |||
| Platelet count 350 × 109/L or more | 604 (22.4) | 295 (21.6) | .59 |
| Hemoglobin level less than 100 g/L | 178 (6.6) | 73 (5.3) | .12 |
| WBC count more than 11 × 109/L | 344 (12.7) | 169 (12.4) | .75 |
| Bilirubin level more than 17.1 μmol/L | 103 (3.8) | 60 (4.4) | .37 |
| Albumin level less than 35 g/L | 544 (20.1) | 267 (19.6) | .66 |
| Creatinine level more than 114.4 μmol/L | 89 (3.3) | 45 (3.3) | .999 |
| Drugs | |||
| Erythropoiesis-stimulating agents reported up to cycle 2 | 764 (28.3) | 358 (26.2) | .17 |
| Prophylactic myeloid growth factors | 566 (21.0) | 299 (21.9) | .48 |
| Antibiotics | 131 (4.9) | 62 (4.5) | .66 |
| Corticosteroids | 712 (26.4) | 357 (26.2) | .89 |
Development of risk model
In the derivation cohort, 60 patients (2.2%) developed VTE. In univariate analysis, the following covariates were statistically significantly associated with the development of symptomatic VTE: primary site of cancer, prechemotherapy platelet count of 350 × 109/L or more, hemoglobin level less than 100 g/L (10 g/dL), use of ESAs, leukocyte count more than 11 × 109/L, and body mass index of 35 kg/m2 or more. VTE rates were higher in patients with poor performance status (2.6% with performance status ≥ 2, n = 228) but this difference was not statistically significant. Prophylactic myeloid growth factors were associated with leukocytosis (prophylactic use in 21% of patients with white blood cell [WBC] count ≤11 × 109/L and in 26% with WBC count ≥11 × 109/L, P = .01) but not with VTE. For further analysis, sites of cancer were categorized into “very high risk” with VTE rates 3-fold or higher than the average risk for the population (gastric, pancreatic), “high risk” with rates higher than average (lung, lymphoma, gynecologic, genitourinary excluding prostate), and “others” with rates at or below average (breast, colorectal, prostate, and others). There was a strong association between hemoglobin level less than 100 g/L (10 g/dL) and use of ESAs, with 75% of patients with a baseline hemoglobin level less than 100 g/L (10 g/dL) receiving ESAs by the beginning of cycle 2. These were analyzed as one variable. Age was not significantly associated with VTE either when the population was dichotomized at 65 years or categorized as younger than 40 years, 40 to younger than 65 years, and 65 years or older. In the final multivariate analysis, the following variables were independently associated with risk of VTE: primary site of cancer (very high risk or high risk), prechemotherapy platelet count of 350 × 109/L or more, hemoglobin level less than 100 g/L (10 g/dL) and/or use of red cell growth factors, leukocyte count more than 11 × 109/L, and body mass index of 35 kg/m2 or more (Table 2). We assigned points for the risk model based on the regression coefficients obtained from the final model and divided the population into 3 risk categories based on the score from the risk model: low (score 0), intermediate (score 1-2), and high (score ≥ 3; Table 3).
Table 2.
Predictors of venous thromboembolism in the derivation cohort by multivariate logistic regression analysis
| Patient characteristic | β | Odds ratio* (95% CI) |
|---|---|---|
| Site of cancer | ||
| Very high risk (stomach, pancreas) | 1.46 | 4.3 (1.2-15.6) |
| High risk (lung, lymphoma, gynecologic, genitourinary excluding prostate) | 0.43 | 1.5 (0.9-2.7) |
| Low risk (breast, colorectal, head and neck) | 0.0 | 1.0 (reference) |
| Prechemotherapy platelet count 350 × 109/L or more | 0.60 | 1.8 (1.1-3.2) |
| Hemoglobin level less than 100 g/L or use of red cell growth factors | 0.89 | 2.4 (1.4-4.2) |
| Prechemotherapy leukocyte count more than 11 × 109/L | 0.77 | 2.2 (1.2-4) |
| BMI 35 kg/m2 or more | 0.90 | 2.5 (1.3-4.7) |
Odds ratios are adjusted for stage.
Table 3.
Predictive model for chemotherapy-associated VTE
| Patient characteristic | Risk score |
|---|---|
| Site of cancer | |
| Very high risk (stomach, pancreas) | 2 |
| High risk (lung, lymphoma, gynecologic, bladder, testicular) | 1 |
| Prechemotherapy platelet count 350 × 109/L or more | 1 |
| Hemoglobin level less than 100 g/L or use of red cell growth factors | 1 |
| Prechemotherapy leukocyte count more than 11 × 109/L | 1 |
| BMI 35 kg/m2 or more | 1 |
Accuracy and validation of risk model
The risk model was tested in the validation cohort of 1365 patients of whom 28 (2.1%) developed VTE. At the cutoff point for high risk (score ≥ 3), the model had a negative predictive value (probability of no VTE in those designated low risk) of 98.5%, a positive predictive value (probability of VTE in those designated high risk) of 7.1%, a sensitivity (probability of high risk in those experiencing VTE) of 40.0%, and a specificity (probability of low risk in those not experiencing VTE) of 88% in the derivation cohort. Similarly, in the validation cohort, the model had a negative predictive value of 98.5%, a positive predictive value of 6.7%, a sensitivity of 35.7%, and a specificity of 89.6%. In both the derivation and validation cohorts, the C statistic was 0.7. The model also demonstrated good calibration. The Hosmer-Lemeshow goodness-of-fit test results were nonsignificant (P = .75 for derivation cohort and P = .15 for validation cohort), indicating that the observed and predicted numbers of patients with and without VTE were not significantly different. The observed rates of VTE according to the prespecified risk category for both cohorts are shown in Figure 1. The accuracy of the score and the proportion of patients classified into each risk category were similar in the derivation and validation cohorts.
Figure 1.
Rates of VTE according to scores from the risk model in the derivation and validation cohorts.
Discussion
In this analysis of data from an observational study, we identified 5 clinical and laboratory parameters that were independently predictive of symptomatic VTE in cancer patients initiating a new chemotherapy regimen. These parameters were combined into a simple risk assessment model that allows providers to classify patients into 3 discrete categories corresponding to the risk of chemotherapy-associated VTE. The model was then validated in an independent cohort of patients from the same observational study. In the validation cohort, the rates of symptomatic VTE over a median period of follow up of 2.5 months in the low-, intermediate-, and high-risk categories were 0.3%, 2%, and 6.7%, respectively (Figure 1).
Many of the risk factors identified in this analysis agree with earlier studies. Our findings of a strong association of VTE with gastrointestinal, gynecologic and lung cancer, and lymphoma are consistent with prior reports.1–3,12,36,37 Our study did not include sufficient numbers of patients with brain or renal cancers and myeloma, all of which have also been strongly associated with VTE. The association of an elevated prechemotherapy platelet count with VTE was previously reported in an initial analysis of this study,2 and has also recently been suggested in lung cancer.38 A retrospective study of medical inpatients including cancer patients also identified an admission platelet count of more than 350 × 109/L as predictive for VTE during hospitalization.39 Obesity is a known risk factor for VTE in the general population (reviewed in Ageno et al40), although it has not been studied specifically in cancer patients. In a recent meta-analysis, use of ESAs was associated with a 1.67-fold increase in thromboembolic events.41 The association of leukocytosis with VTE reported in this study is novel. Recent large studies have described an association of leukocyte count with vascular events in the general population,42 and particularly with venous thrombotic events in patients with myeloproliferative disorders (reviewed in Tefferi et al43) possibly driven by cross-talk between granulocytes and platelets and/or endothelial cells. In cancer patients, leukocytosis may also be a surrogate for advanced disease burden not captured by stage classification.44 There did not appear to be a correlation of VTE with use of prophylactic myeloid growth factors in our study. Further investigations into the role of leukocytes in cancer-associated thrombosis would be of interest.
Older age and stage of disease were not associated with VTE in our analysis, in contrast to previous reports.1,12,36 This may be a reflection of the excellent performance status of most patients enrolled in this study. Rates of VTE were indeed higher in the small number of patients with poor performance status in our study. Recent data demonstrate that the risk of VTE remains high for a prolonged period after surgery in cancer patients.45 Although history of recent surgery was not a significant predictor of VTE in our analysis, postsurgical prophylaxis and patient selection for chemotherapy may be potential confounding factors. VTE in cancer patients often occurs in the initial period after diagnosis.1 In our analysis, VTE was more frequent in chemotherapy-naive patients than in those who had undergone chemotherapy (2.3% vs 1.6%) but this difference was not statistically significant; however, 75% of events occurred in the first 2 cycles of chemotherapy suggesting the initial period of chemotherapy remains high risk for VTE.
VTE prophylaxis is effective in settings where the incidence of VTE is high, such as in hospitalized patients, or in the postoperative setting.14–18,46 However, trials of prophylaxis conducted in cancer patients identified as high risk by individual factors, such as primary site of cancer or use of venous access devices, have been largely unsuccessful. The goal of our analysis was to develop a risk assessment model that would incorporate multiple variables and allow providers to identify patients at high risk. Formal risk assessment models for DVT in other high-risk populations have been developed and are used clinically.28–33 We focused on variables that are simple to evaluate and routinely collected before initiating chemotherapy. According to the model, approximately 27% of patients had a risk of VTE as low as 0.3%; an additional 60% of patients had a risk of VTE of approximately 2%. It is unlikely that patients classified in these groups would benefit from thromboprophylaxis. In contrast, patients in the high-risk group had a nearly 7% risk of developing VTE over a period of only 2.5 months (2.7%/month). This risk is comparable with that observed in other high-risk settings such as hospitalized medically ill patients for whom prophylaxis has been shown to be effective and safe.46 This rate of 7% in the high-risk group is higher than the rate of 4.4% symptomatic VTE seen in the placebo arm of the Levine et al study, which showed a benefit of prophylaxis in breast cancer patients,19 and also higher than the 3.4% rate of symptomatic VTE in the TOPIC-II lung study, which showed a trend toward benefit for prophylaxis.22 However, cancer patients are also paradoxically at increased risk of bleeding complications as well,9 and the safety of prophylaxis in the high-risk group identified by this model needs to be evaluated in clinical trials. Future trials of prophylaxis should focus on identifying and testing patients in the high-risk group identified by this model.
The statistical issues surrounding the derivation and validation of risk models merit discussion. A commonly accepted rule for modeling specifies that the number of events should be at least 10 times the number of variables included in the model.47,48 In the derivation cohort, 60 patients developed VTE and our final model comprised only 5 variables. We followed accepted recommendations for development of the model, including identifying a list of potential predictors, using logistic regression to identify the most powerful predictors, using regression coefficients to develop the score, and validating the model.49,50 Since patients accrued on this study represented a heterogeneous population across 115 community-based practices nationwide, we believe that the results of our analysis can be generalized. External validation represents the ideal approach to validating models, but we were unable to identify a dataset of cancer patients that had reliably collected data regarding VTE as well as the variables identified in this model. We therefore chose to conduct a split-sample validation. It would certainly be important to further validate this model in other large observational studies that are currently in accrual and are collecting the required data. The value of the C statistic suggests that incorporating additional variables may increase the robustness of this model. Since the goal of this analysis was to identify pretreatment predictors of VTE, we did not study variables developing during treatment, although these could certainly have influenced the development of VTE. Promising new data suggest that tissue factor expression by tumor cells may be a predictive biomarker for VTE.51 We plan to test this model further and evaluate tissue factor and other biomarkers in a prospective outcomes study.
Despite advantages of a large sample size and the ability to conduct a split-sample validation, our study had some limitations. The observational study from which these data were derived was designed to assess febrile neutropenia and related complications as its primary end point, and not the occurrence of VTE. However, data regarding VTE were prospectively collected, and the sample size is adequate for an analysis of this nature. Certain cancers known to be strongly associated with VTE, such as brain tumors (n = 4), and poor performance status patients were underrepresented in the study population. For clinical use, the score for high-risk sites may be generalized to these cancers based on multiple studies documenting high rates of VTE. There may be an association between specific antineoplastic agents and VTE. Initial exploratory analyses in this dataset suggested such relationships (data not shown), but there was significant overlap between type of chemotherapy drug and primary site of cancer. In many instances, the number of events per drug category was too small to be characterized definitively. Further, there were few patients in this study receiving known thrombogenic agents such as thalidomide, lenalidomide, and bevacizumab since only a few myeloma patients were enrolled and the study ended in October 2005, only a short period after bevacizumab was made available. Therefore, larger studies including these agents are needed. Data regarding central venous catheters, a potential risk factor for VTE, were not collected. However, results from recent randomized studies show that the risk of catheter-associated thrombosis is too low to warrant routine prophylaxis, and this is supported by a recent consensus guideline.23,52,53 Data regarding prior history of VTE, use of anticoagulation, or correlation with response to chemotherapy were not available. Finally, VTE was diagnosed by treating physicians based on symptoms and VTE events were not independently adjudicated. However, this suggests that clinically important VTE events were observed, although the true rate may be overestimated or underestimated. In this regard, it is important to note that in clinical trials of medically ill patients, rates of asymptomatic thrombosis are several-fold increased over symptomatic VTE.25,26 Studies in other settings that included cancer patients have furthermore shown a strong association between asymptomatic DVT and subsequent development of symptomatic VTE54–57 as well as a possible association with mortality.58
In summary, this study demonstrates that the risk of VTE in cancer patients initiating chemotherapy can be reliably predicted using a simple risk assessment model based on 5 clinical and laboratory parameters. Cancer-associated thrombosis is an important cause of morbidity and mortality in cancer patients, and it may be preventable with effective prophylaxis strategies. This risk model may be used by clinicians for assessing risk for VTE in patients seen in clinical practice, as well as in the design of future trials involving cancer outpatients who would benefit from thromboprophylaxis.
Acknowledgments
This work was supported by a Career Development Award to A.A.K. from the National Cancer Institute K23 CA120587. The Awareness of Neutropenia in Chemotherapy (ANC) Study Group received research grant support from Amgen for the development of the patient registry. N.M.K. is supported by a National Institutes of Health grant T32HL07152-30.
Footnotes
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: A.A.K. contributed to study design, analysis and interpretation of data, and writing of paper; N.M.K. contributed to analysis and interpretation of data and writing of paper; E.C. contributed to statistical analysis and writing of paper; G.H.L. and C.W.F. contributed to study design, data analysis, and writing of paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Alok A. Khorana, 601 Elmwood Ave, Box 704, Rochester, NY 14642; e-mail: alok_khorana@urmc.rochester.edu.
References
- 1.Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293:715–722. doi: 10.1001/jama.293.6.715. [DOI] [PubMed] [Google Scholar]
- 2.Khorana AA, Francis CW, Culakova E, Lyman GH. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer. 2005;104:2822–2829. doi: 10.1002/cncr.21496. [DOI] [PubMed] [Google Scholar]
- 3.Sallah S, Wan JY, Nguyen NP. Venous thrombosis in patients with solid tumors: determination of frequency and characteristics. Thromb Haemost. 2002;87:575–579. [PubMed] [Google Scholar]
- 4.Kroger K, Weiland D, Ose C, et al. Risk factors for venous thromboembolic events in cancer patients. Ann Oncol. 2006;17:297–303. doi: 10.1093/annonc/mdj068. [DOI] [PubMed] [Google Scholar]
- 5.Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., III Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158:585–593. doi: 10.1001/archinte.158.6.585. [DOI] [PubMed] [Google Scholar]
- 6.Heit JA, Silverstein MD, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., III Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med. 2000;160:809–815. doi: 10.1001/archinte.160.6.809. [DOI] [PubMed] [Google Scholar]
- 7.Levine MN, Gent M, Hirsh J, et al. The thrombogenic effect of anticancer drug therapy in women with stage II breast cancer. N Engl J Med. 1988;318:404–407. doi: 10.1056/NEJM198802183180703. [DOI] [PubMed] [Google Scholar]
- 8.Saphner T, Tormey DC, Gray R. Venous and arterial thrombosis in patients who received adjuvant therapy for breast cancer. J Clin Oncol. 1991;9:286–294. doi: 10.1200/JCO.1991.9.2.286. [DOI] [PubMed] [Google Scholar]
- 9.Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood. 2002;100:3484–3488. doi: 10.1182/blood-2002-01-0108. [DOI] [PubMed] [Google Scholar]
- 10.Elting LS, Escalante CP, Cooksley C, et al. Outcomes and cost of deep venous thrombosis among patients with cancer. Arch Intern Med. 2004;164:1653–1661. doi: 10.1001/archinte.164.15.1653. [DOI] [PubMed] [Google Scholar]
- 11.Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343:1846–1850. doi: 10.1056/NEJM200012213432504. [DOI] [PubMed] [Google Scholar]
- 12.Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006;166:458–464. doi: 10.1001/archinte.166.4.458. [DOI] [PubMed] [Google Scholar]
- 13.Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost. 2007;5:632–634. doi: 10.1111/j.1538-7836.2007.02374.x. [DOI] [PubMed] [Google Scholar]
- 14.Prevention of fatal postoperative pulmonary embolism by low doses of heparin: an international multicentre trial. Lancet. 1975;2:45–51. [PubMed] [Google Scholar]
- 15.Sevitt S, Gallagher NG. Prevention of venous thrombosis and pulmonary embolism in injured patients: a trial of anticoagulant prophylaxis with phenindione in middle-aged and elderly patients with fractured necks of femur. Lancet. 1959;2:981–989. doi: 10.1016/s0140-6736(59)91464-3. [DOI] [PubMed] [Google Scholar]
- 16.Sagar S, Massey J, Sanderson JM. Low-dose heparin prophylaxis against fatal pulmonary embolism. Br Med J. 1975;4:257–259. doi: 10.1136/bmj.4.5991.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halkin H, Goldberg J, Modan M, Modan B. Reduction of mortality in general medical in-patients by low-dose heparin prophylaxis. Ann Intern Med. 1982;96:561–565. doi: 10.7326/0003-4819-96-5-561. [DOI] [PubMed] [Google Scholar]
- 18.Collins R, Scrimgeour A, Yusuf S, Peto R. Reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin: overview of results of randomized trials in general, orthopedic, and urologic surgery. N Engl J Med. 1988;318:1162–1173. doi: 10.1056/NEJM198805053181805. [DOI] [PubMed] [Google Scholar]
- 19.Levine M, Hirsh J, Gent M, et al. Double-blind randomised trial of a very-low-dose warfarin for prevention of thromboembolism in stage IV breast cancer. Lancet. 1994;343:886–889. doi: 10.1016/s0140-6736(94)90008-6. [DOI] [PubMed] [Google Scholar]
- 20.Couban S, Goodyear M, Burnell M, et al. Randomized placebo-controlled study of low-dose warfarin for the prevention of central venous catheter-associated thrombosis in patients with cancer. J Clin Oncol. 2005;23:4063–4069. doi: 10.1200/JCO.2005.10.192. [DOI] [PubMed] [Google Scholar]
- 21.Verso M, Agnelli G, Bertoglio S, et al. Enoxaparin for the prevention of venous thromboembolism associated with central vein catheter: a double-blind, placebo-controlled, randomized study in cancer patients. J Clin Oncol. 2005;23:4057–4062. doi: 10.1200/JCO.2005.06.084. [DOI] [PubMed] [Google Scholar]
- 22.Haas SK, Kakkar AK, Kemkes-Mathes B, et al. Prevention of venous thromboembolism with low molecular weight heparin in patients with metastatic breast or lung cancer-results of the TOPIC studies. J Thromb Haemost. 2005;3 Abstract OR059. [Google Scholar]
- 23.Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126:338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 24.Wagman LD, Baird MF, Bennett CL, et al. Venous thromboembolic disease: clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2006;4:838–869. doi: 10.6004/jnccn.2006.0071. [DOI] [PubMed] [Google Scholar]
- 25.Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients: Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med. 1999;341:793–800. doi: 10.1056/NEJM199909093411103. [DOI] [PubMed] [Google Scholar]
- 26.Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004;110:874–879. doi: 10.1161/01.CIR.0000138928.83266.24. [DOI] [PubMed] [Google Scholar]
- 27.Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006;332:325–329. doi: 10.1136/bmj.38733.466748.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Risk of and prophylaxis for venous thromboembolism in hospital patients: Thromboembolic Risk Factors (THRIFT) Consensus Group. BMJ. 1992;305:567–574. doi: 10.1136/bmj.305.6853.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Samama MM. Applying risk assessment models in general surgery: effective risk stratification. Blood Coagul Fibrinolysis. 1999;10(suppl 2):S79–S84. [PubMed] [Google Scholar]
- 30.Samama MM, Dahl OE, Quinlan DJ, Mismetti P, Rosencher N. Quantification of risk factors for venous thromboembolism: a preliminary study for the development of a risk assessment tool. Haematologica. 2003;88:1410–1421. [PubMed] [Google Scholar]
- 31.Caprini JA, Arcelus JI, Hasty JH, Tamhane AC, Fabrega F. Clinical assessment of venous thromboembolic risk in surgical patients. Semin Thromb Hemost. 1991;17(suppl 3):304–312. [PubMed] [Google Scholar]
- 32.Ageno W. Applying risk assessment models in general surgery: overview of our clinical experience. Blood Coagul Fibrinolysis. 1999;10(suppl 2):S71–S78. [PubMed] [Google Scholar]
- 33.Heinemann LA, Dominh T, Assmann A, et al. VTE risk assessment: a prognostic model: BATER Cohort Study of young women. Thromb J. 2005;3:5. doi: 10.1186/1477-9560-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le Gal G, Righini M, Roy PM, et al. Prediction of pulmonary embolism in the emergency department: the revised Geneva score. Ann Intern Med. 2006;144:165–171. doi: 10.7326/0003-4819-144-3-200602070-00004. [DOI] [PubMed] [Google Scholar]
- 35.Kratz A, Ferraro M, Sluss PM, Lewandrowski KB. Case records of the Massachusetts General Hospital: weekly clinicopathological exercises: laboratory reference values. N Engl J Med. 2004;351:1548–1563. doi: 10.1056/NEJMcpc049016. [DOI] [PubMed] [Google Scholar]
- 36.Khorana AA, Francis CW, Culakova E, Fisher RI, Kuderer NM, Lyman GH. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol. 2006;24:484–490. doi: 10.1200/JCO.2005.03.8877. [DOI] [PubMed] [Google Scholar]
- 37.Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006;119:60–68. doi: 10.1016/j.amjmed.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 38.Zecchina G, Ghio P, Bosio S, Cravino M, Camaschella C, Scagliotti GV. Reactive thrombocytosis might contribute to chemotherapy-related thrombophilia in patients with lung cancer. Clin Lung Cancer. 2007;8:264–267. doi: 10.3816/CLC.2007.n.004. [DOI] [PubMed] [Google Scholar]
- 39.Zakai NA, Wright J, Cushman M. Risk factors for venous thrombosis in medical inpatients: validation of a thrombosis risk score. J Thromb Haemost. 2004;2:2156–2161. doi: 10.1111/j.1538-7836.2004.00991.x. [DOI] [PubMed] [Google Scholar]
- 40.Ageno W, Squizzato A, Garcia D, Imberti D. Epidemiology and risk factors of venous thromboembolism. Semin Thromb Hemost. 2006;32:651–658. doi: 10.1055/s-2006-951293. [DOI] [PubMed] [Google Scholar]
- 41.Bohlius J, Wilson J, Seidenfeld J, et al. Recombinant human erythropoietins and cancer patients: updated meta-analysis of 57 studies including 9353 patients. J Natl Cancer Inst. 2006;98:708–714. doi: 10.1093/jnci/djj189. [DOI] [PubMed] [Google Scholar]
- 42.Grau AJ, Boddy AW, Dukovic DA, et al. Leukocyte count as an independent predictor of recurrent ischemic events. Stroke. 2004;35:1147–1152. doi: 10.1161/01.STR.0000124122.71702.64. [DOI] [PubMed] [Google Scholar]
- 43.Tefferi A, Gangat N, Wolanskyj A. The interaction between leukocytosis and other risk factors for thrombosis in essential thrombocythemia [letter]. Blood. 2007;109:4105. doi: 10.1182/blood-2007-01-066985. [DOI] [PubMed] [Google Scholar]
- 44.Garcia-Arias A, Cetina L, Candelaria M, Robles E, Duenas-Gonzalez A. The prognostic significance of leukocytosis in cervical cancer. Int J Gynecol Cancer. 2007;17:465–470. doi: 10.1111/j.1525-1438.2007.00816.x. [DOI] [PubMed] [Google Scholar]
- 45.Rasmussen MS. Prolonged thromboprophylaxis with low molecular weight heparin after major abdominal surgery. Curr Opin Pulm Med. 2007;13:389–392. doi: 10.1097/MCP.0b013e3282058ba6. [DOI] [PubMed] [Google Scholar]
- 46.Francis CW. Clinical practice: prophylaxis for thromboembolism in hospitalized medical patients. N Engl J Med. 2007;356:1438–1444. doi: 10.1056/NEJMcp067264. [DOI] [PubMed] [Google Scholar]
- 47.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 48.Wasson JH, Sox HC, Neff RK, Goldman L. Clinical prediction rules: applications and methodological standards. N Engl J Med. 1985;313:793–799. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]
- 49.Altman DG, Royston P. What do we mean by validating a prognostic model? Stat Med. 2000;19:453–473. doi: 10.1002/(sici)1097-0258(20000229)19:4<453::aid-sim350>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 50.McGinn TG, Guyatt GH, Wyer PC, Naylor CD, Stiell IG, Richardson WS. Users' guides to the medical literature: XXII: how to use articles about clinical decision rules: Evidence-Based Medicine Working Group. JAMA. 2000;284:79–84. doi: 10.1001/jama.284.1.79. [DOI] [PubMed] [Google Scholar]
- 51.Khorana AA, Ahrendt SA, Ryan CK, et al. Tissue factor expression, angiogenesis, and thrombosis in pancreatic cancer. Clin Cancer Res. 2007;13:2870–2875. doi: 10.1158/1078-0432.CCR-06-2351. [DOI] [PubMed] [Google Scholar]
- 52.Couban S, Goodyear M, Burnell M, et al. Randomized placebo-controlled study of low-dose warfarin for the prevention of central venous catheter-associated thrombosis in patients with cancer. J Clin Oncol. 2005;23:4063–4069. doi: 10.1200/JCO.2005.10.192. [DOI] [PubMed] [Google Scholar]
- 53.Heaton DC, Han DY, Inder A. Minidose (1 mg) warfarin as prophylaxis for central vein catheter thrombosis. Intern Med J. 2002;32:84–88. [PubMed] [Google Scholar]
- 54.Kakkar VV, Howe CT, Flanc C, Clarke MB. Natural history of postoperative deep-vein thrombosis. Lancet. 1969;2:230–232. doi: 10.1016/s0140-6736(69)90002-6. [DOI] [PubMed] [Google Scholar]
- 55.Haas SB, Tribus CB, Insall JN, Becker MW, Windsor RE. The significance of calf thrombi after total knee arthroplasty. J Bone Joint Surg Br. 1992;74:799–802. doi: 10.1302/0301-620X.74B6.1447236. [DOI] [PubMed] [Google Scholar]
- 56.Eikelboom JW, Quinlan DJ, Douketis JD. Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet. 2001;358:9–15. doi: 10.1016/S0140-6736(00)05249-1. [DOI] [PubMed] [Google Scholar]
- 57.Mismetti P, Laporte S, Darmon JY, Buchmuller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg. 2001;88:913–930. doi: 10.1046/j.0007-1323.2001.01800.x. [DOI] [PubMed] [Google Scholar]
- 58.Vaitkus PT, Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Goldhaber SZ. Mortality rates and risk factors for asymptomatic deep vein thrombosis in medical patients. Thromb Haemost. 2005;93:76–79. doi: 10.1160/TH04-05-0323. [DOI] [PubMed] [Google Scholar]