Abstract
Objective
To establish low-cost easily conducted health promotion interventions for advanced pharmacy practice experience (APPE) students in community pharmacy settings that would increase women's awareness about health issues using Food and Drug Administration (FDA) educational materials.
Methods
Students distributed fact sheets on medication use, heart disease, and diabetes to women over 45 years of age at 6 community pharmacy APPE sites. Interventions completed were either personal medication records (PMR) to identify medication-related problems (MRP) or heart health screenings followed by completion of an anonymous patient satisfaction survey instrument.
Results
Over 1500 fact sheets were distributed. Fifty-eight women (age 61 ± 15 years) completed PMRs, which identified 57 MRPs in 42 patients. Twenty-four women indicated the screening was “useful/very useful” for increasing medication understanding. Sixty-three women completed heart health screenings. Thirty-one of the 40 who completed the survey instrument indicated the screening was “useful/very useful” for learning heart disease risk.
Conclusions
Community pharmacy APPE students interventions identified MRPs and patients at risk for heart disease. These health promotion interventions enhanced women's awareness of these topics while guiding students to achieve the desired curricular outcomes.
Keywords: community pharmacy, wellness, advanced pharmacy practice experience, women's health
INTRODUCTION
Advanced pharmacy practice experiences (APPEs) should provide students with opportunities to develop their ability to promote health improvement, wellness, and disease prevention.1 Albany College of Pharmacy had developed a required community pharmacy APPE based upon the 1998 Center for the Advancement of Pharmaceutical Education (CAPE) outcomes document.2,3 The revised CAPE outcomes identified a need to include structured opportunities for community pharmacy APPE students to participate in the provision of public health.4 Since community pharmacists are readily accessible health care providers, they are uniquely able to provide health information to and screening opportunities for large numbers of individuals. Thus, community pharmacy APPEs provide an ideal setting in which to engage students in wellness promotion activities that benefit the students, preceptors, sites, and patients involved. Targeted areas for pharmacists to be involved in achieving the public health goals outlined in Healthy People 2010 include hypertension, diabetes, asthma, patient education, smoking cessation, and general medication management.5
Community pharmacists have demonstrated their ability to identify patients at risk and increase their awareness of cardiovascular disease, breast cancer, osteoporosis, and obesity.6-10 Although there has been demonstrated success, barriers hinder the implementation of widespread and consistent service development. With increasing student enrollment in pharmacy schools, it is a challenge to ensure that all students have the opportunity to directly engage in these activities during APPEs. A survey conducted by ACPE indicated that a low percentage of APPE students had the opportunity to engage in formal disease management programs, health screenings, and educational workshops.11 Preceptors identified challenges to providing pharmaceutical care such as time spent on prescription third-party billing, lack of reimbursement, and high prescription volume.
Until these challenges are overcome, those services involving the first-defined level of health promotion, “health advocacy,” can be offered in a less time-consuming and labor-intensive manner.12 Advocacy-based methods include the use of educational posters, attachment of flyers to prescription bags, and review of educational material to patients at the time of dispensing and counseling.12 This level of health promotion can be reasonably accomplished in community pharmacy APPE sites. This study describes an advocacy-based approach using materials provided by the Food and Drug Administration Office of Women's Health (FDA OWH) to implement an education and screening program in community pharmacy APPE sites. Previously targeted intervention programs have involved Albany College of Pharmacy community pharmacy APPE students identifying a medication-related problem (indication without medication for aspirin and calcium) in a focused patient population.13,14
The purposes of the study were: (1) to provide structured opportunities for community pharmacy APPE students to increase women's awareness about targeted health topics by using FDA OWH educational materials in conjunction with a screening intervention; (2) to encourage health care providers and the public, especially women, to consider the FDA OWH as a health information resource; and (3) to increase women's understanding of pertinent health topics using the FDA OWH information resources.
METHODS
The study was conducted in 6 community pharmacy APPE sites during three 5-week periods. Pharmacies included 2 independent, 2 chain, and 2 grocery chain pharmacies. The primary preceptors who practiced at the pharmacy site were full-time faculty members (n = 3) or adjunct faculty members (n = 1). The primary preceptors educated the additional onsite pharmacists. The goal was distribution of 300 FDA fact sheets for each of the 3 selected health topics. Albany College of Pharmacy Investigational Review Board expedited review was obtained with waiver of consent due to the minimal risk of the intervention, since patient confidentiality was maintained through de-identification of the data and because patients could decline to participate. Students (n = 18) participating in the program completed de-identified records to document the outcomes of the study. The target population for each intervention program was women over the age of 45 years; however, women over 18 years of age were allowed to participate if they requested. In response to an IRB recommendation, males were not targeted, but were screened upon request. For each intervention period, IRB-approved posters were hung at the store entrance and in the pharmacy area to notify patients of the program. Women were also identified during the prescription-dispensing process or routine blood pressure screenings that occurred at the sites. Interventions were provided free of charge. Participation in the 2 screening interventions (“Using Medicines Wisely” and “Healthy Heart,” described below) which required several minutes of the patient's time, was rewarded with an inexpensive incentive gift. Since the diabetes intervention was solely informational in nature, no incentive was provided. The disease states targeted were scheduled to coincide with national health observance periods.
The FDA OWH fact sheets and booklets are available at the Office of Women's Health Website: www.fda.gov/womens/default.htm free of charge. The “Using Medicines Wisely” sheet covers questions for patients to ask their doctor, nurse, or pharmacist; identifies how to read medication labels; and recommends patients use medicines as directed. The “My Medicines” purse-sized booklet includes similar information and a personal medication record (PMR). The “Heart Disease” sheet provides general information about the risks associated with heart disease, signs and symptoms, and how to lower cardiac risk. The “Strokes” fact sheet covers different types of stroke, individuals at risk, warning signs, what to do if stroke-like symptoms occur, and how to lower the risk of having a stroke. Lastly, the “Diabetes” educational materials provide basic information about diabetes, risk factors and warning signs, how to lower the risk of diabetes, how to use medicines properly, and how to monitor blood sugar. For this study, the color printed flyers and booklets were provided to the investigators through the FDA.
Students were requested to conduct the targeted intervention at their assigned APPE site. During the first week of each 5-week APPE, students were educated by 1 of the study investigators on how to conduct the outreach and intervention. Copies of the posters, fact sheets, booklets, and documentation records were distributed to the participating pharmacies. Students were supervised by the pharmacist preceptors at their sites. Technicians or students gave patients the FDA OWH fact sheet to review while their prescriptions were being filled and offered the intervention when the prescription was picked up. Fact sheets were also attached to the prescription bags of new or refill prescriptions, which alerted the student to recruit the patient when they returned later to collect their prescription. After the intervention was completed, patients were encouraged to fill out the anonymous patient satisfaction survey instrument on site or return it via US mail to the college using the self-addressed stamped envelope provided.
Using Medicines Wisely Intervention
Students counseled targeted patients on all new prescriptions or refills using the questions on the fact sheet. Additionally the students offered to complete the PMR in the “My Medicines” booklet with the patient, offering a free water bottle to the patient as an incentive for participation. For those patients agreeing to participate, their medications (including prescription, nonprescription, and natural products) were reviewed and documented on the “My Medicines” PMR booklet. Any medication-related problems (MRPs) identified during counseling or completion of the PMR were resolved as appropriate through consultation with the patient and/or prescriber and then documented by the student. The impact of the intervention was determined by the number of MRPs identified and the results of the patient satisfaction survey, which was only given to patients who had the PMR completed.
Healthy Heart Screening Intervention
Students counseled patients on the content of the “Heart disease” and “Strokes” fact sheets that were placed on all prescriptions for targeted patients. Students briefly reviewed the purpose of the intervention with patients, which was to increase women's awareness about heart disease and stroke and the role of the FDA as a resource. Patients were invited to participate in the heart health risk assessment screening offering a silver heart-shaped clock keychain as an incentive. Students completed a brief history and measured the patient's blood pressure (BP) and pulse. Blood pressure was measured twice and the readings were averaged. The patient's self-reported height and weight were used to calculate body mass index (BMI). Students identified the patient's cardiovascular risk factors using the fact sheets for heart disease and stroke, and the national guidelines for hypertension, obesity, and cholesterol.15-17 Ten-year cardiovascular risk was calculated using the Framingham algorithm for patients who knew their cholesterol values.18 The fact sheets and risk assessment form were given to the patients and they were encouraged to discuss the results with their physicians and inquire about recommended screenings for diabetes and cardiovascular disease. The impact of the intervention was determined by the number of women who met the national screening recommendations and the patient satisfaction survey instruments submitted by those patients who completed the whole screening process.
Diabetes Awareness Intervention
Due to limitations in funding, a comprehensive diabetes awareness program with counseling was not possible. However, FDA OWH diabetes fact sheets or booklets were distributed during a third intervention period. While the presentation format varied, both the fact sheet and booklets contained the same information.
RESULTS
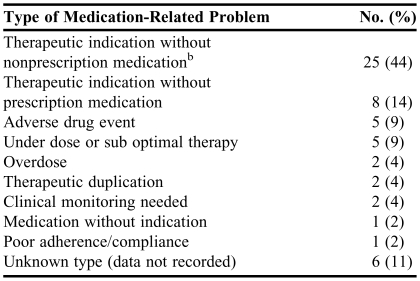
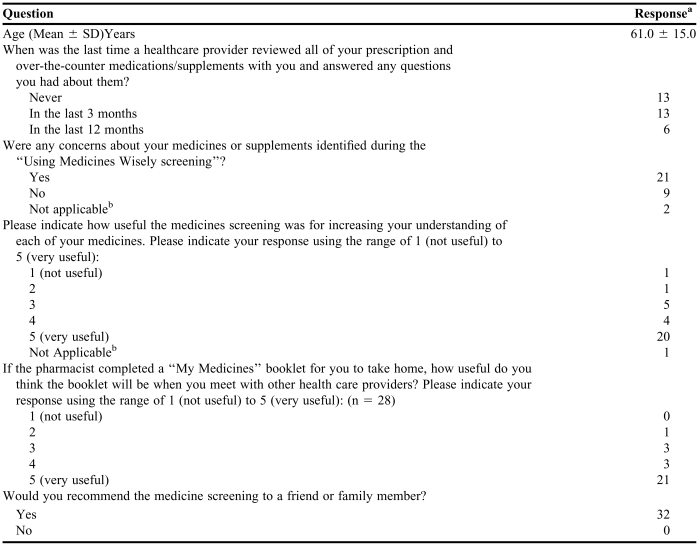
During the intervention period, 545 “Using Medicines Wisely” fact sheets were distributed with prescriptions. Sixteen women were given the “My Medicines” booklet to self-complete. Fifty-eight women had the PMR completed in the “My Medicines” booklet by the students and were given water bottles for their participation. The average number of prescription and nonprescription medications recorded for each patient was 4.6 ± 3.4 and 1.8 ± 1.6 respectively (mean ± SD). Fifty-seven MRPs were identified in 42/58 (72%) patients for whom the student completed PMRs (Table 1). For these 57 MRPs, 30 recommendations were accepted, 2 were not accepted, and the outcome of 25 interventions was unknown. Thirty-two patients completed the survey instrument (Table 2). The majority of patients found the screening to be very useful and all would recommend the service to others. Thirteen patients responded that no health care provider had previously reviewed all their medications and supplements with them. Twenty-one patients responded that concerns related to medicines or supplements were identified during the screening.
Table 1.
Medication-Related Problems Identified Among Female Pharmacy Patients Who Participated in a Screening Conducted by Students in an Advanced Pharmacy Practice Experience (n = 57)a
57 MRP's were identified in 42 of the 58 patients screened
bCalcium (n = 17), low dose aspirin (n = 8)
Table 2.
Using Medications Wisely Survey Results (n = 32)
aNumber of respondents
bPatient not taking medicines or supplements
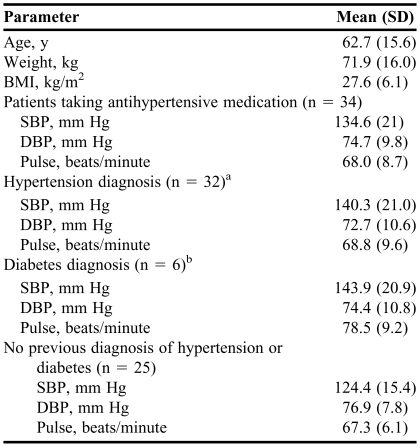
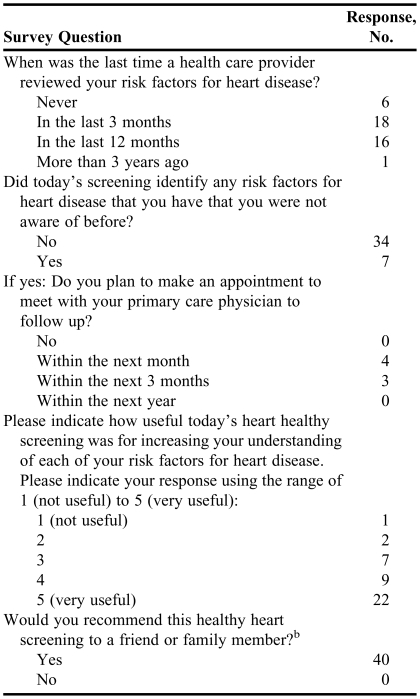
Six hundred eleven “Heart Disease” and 629 “Strokes” fact sheets were distributed. Sixty-three women completed the healthy heart screening intervention. The average age of these patients was 62.7 ± 15.6 years. The mean (±SD) weight and BMI were 71.9 ± 16.0 kg and 27.6 ± 6.1 kg/m2, respectively. The data resulting from the blood pressure screenings are presented in Table 3. Of the 32 patients previously diagnosed with hypertension, 29 were taking medication for blood pressure control and 17 patients were above the JNC VII recommended goal blood pressure of 140/90 mm Hg. Of the 6 patients who had diabetes mellitus, 5 were taking antihypertensive medication. Three of the 6 had blood pressure readings that exceeded the goal of 130/80 mmHg, 1 did not have blood pressure measurements recorded, and 2 had controlled blood pressure. Six of the remaining 25 patients screened who were not previously diagnosed with hypertension or diabetes exceeded the blood pressure goal of 140/90 mm Hg. Overall 38% of patients screened had blood pressures that exceeded the desired goal. Seventeen women had not had their blood pressure (n = 1), blood glucose (n = 7), or cholesterol (n = 9) checked within the nationally recommended timeline. Although 54 patients had their cholesterol checked within the past 5 years, only 6 patients knew their cholesterol values. For these patients, the calculated Framingham risk score was between <1% to 14%. Forty patients who participated in the screening completed the patient satisfaction survey instrument (Table 4). Even though the majority (n = 34) had their heart disease risk factors reviewed by a health care provider within the previous 12 months, the pharmacy intervention was well received and would be recommended to others. Seven patients who were made aware of their risk factors for heart disease planned to make an appointment with their primary care physician to follow up.
Table 3.
Demographic Characteristics and Diagnostic Readings of Participants in a Blood Pressure Screening Conducted by Advanced Pharmacy Practice Experience Students (n = 63)
Abbreviations: BMI: body mass index; SBP = systolic blood pressure; DBP = diastolic blood pressure
aTwenty-nine patients were taking antihypertensive medication
bFive patients were taking antihypertensive medication
Table 4.
Heart Health Screening Patient Satisfaction Survey Results (n = 41a)
Age of respondents, 62.5 ± 15.8 years
b40 respondents
Three hundred ninety-three single-page diabetes fact sheets and 263 diabetes folded brochures were distributed with prescriptions.
DISCUSSION
As barriers to pharmaceutical care are overcome and medication therapy management (MTM) is implemented on a broader scale, it is essential that pharmacy graduates are able to engage in pharmaceutical care and health promotion in the community pharmacy setting. This study demonstrated that APPE students can participate in these 2 core CAPE outcomes and engage approximately 10% of those patients approached in a community pharmacy. Through this intervention, students provided a medication therapy review, completed a personal medication record, and intervened to resolve MRPs, all of which are core elements of a community pharmacy MTM service and pharmaceutical care activities.4,19 Other colleges of pharmacy could implement programs such as this using readily available materials to bridge the gaps in community pharmacy experiential education identified by Zarembski et al until comprehensive community pharmacy programs are widespread.11
Carter et al developed an algorithm for estimating learning opportunities and productivity impact at experiential education sites.20 The algorithm suggests that optimal learning opportunities are those where students perform the activity, know the outcome of the activity, and have their performance evaluated. Being able to resolve MRPs and see the survey results gave students immediate feedback regarding the outcome of their activity. Students were able to use these interventions to fulfill their APPE capabilities requirements (history taking, MRP detection/intervention/documentation, medication counseling, case presentations), which preceptors evaluated.2
The Carter model also suggests that activities with the most positive impact on site productivity are those that students can complete independently, require little training time, and are necessary for the site. These considerations are important when attempting to recruit new rotation sites and maintain existing ones in the busy community pharmacy setting. Although the screening interventions presented met the first 2 criteria, one could state they are not “necessary” for the site. Alternatively, one could argue that these activities are necessary to both the individual pharmacy and the profession in order to promote a positive impression of pharmacy to the public. The interventions described could be readily implemented at other colleges of pharmacy.
This study was limited by the lack of opportunity to provide follow-up and measure longer term outcomes, such as whether patients followed up with their health care provider or made any lifestyle changes as a consequence of receiving the information. This approach would have required a more intensive study protocol with appropriate funding. Full consent may have hampered adequate patient recruitment and increased intervention time. Since most patients did not know their cholesterol values, it was not possible to calculate their Framingham risk score, and in New York State, a pharmacy is not permitted to conduct Clinical Laboratory Improvement Act (CLIA)-waived laboratory testing. Validated survey tools for this study were not available, which would have strengthened the study findings. Patients were encouraged to complete survey instruments on site; however, the majority was mailed back to the investigator, which may have reduced the response rate. Although patients were not asked directly about their future use of the FDA OWH as a resource, all materials used clearly identified the FDA OWH as the source of the information.
CONCLUSION
APPE student health promotion activities were well received by women in the community pharmacy setting. These interventions served to increase awareness and/or remind patients of the health risks associated with heart disease, stroke, and diabetes, as well as of the dangers of inappropriate use of medicines. By collaborating with colleges of pharmacy, community pharmacists can overcome some time and resource constraints to offer needed health promotion activities, and at the same time provide a quality learning opportunity for pharmacy students that is in line with ACPE standards and CAPE outcomes.
ACKNOWLEDGEMENTS
This study was the subject of a poster presentation at the Annual meeting of the American Pharmacists Association, in San Francisco in 2006. Funding and materials for this study were provided by the Food and Drug Administration (FDA) Office of Women's Health (OWH), Washington, DC. The authors thank the following individuals who served as preceptors during the study and provided feedback throughout the study process: Mario M. Zeolla, PharmD, BCPS, who at the time of the study was Associate Professor of Pharmacy Practice, Albany College of Pharmacy, Albany, New York, and Eckerd PatientCARE Pharmacist, Eckerd, Loudonville, NY. Jean Cottrell, PharmD, CGP, who at the time of the study was an Eckerd PatientCARE Pharmacist, Eckerd, Latham, NY. Now clinical pharmacist at Stratton VA Medical Center, Albany, New York. Macary Marciniak, PharmD, BCPS, Associate Professor of Pharmacy Practice, Albany College of Pharmacy, Albany, New York, and clinical pharmacist, Price Chopper Pharmacy, Schenectady, NY.
REFERENCES
- 1.Accreditation standards and guidelines for the professional program in pharmacy leading to the Doctor of Pharmacy Degree adopted January 15, 2006. Accreditation Council for Pharmacy Education (ACPE). Available at http://www.acpe-accredit.org/deans/standards.asp. Accessed March 3, 2007.
- 2.Cerulli J, Malone M. Using CAPE outcome-based goals and objectives to evaluate Community Pharmacy Advanced Practice Experiences. Am J Pharm Educ. 2003;67(2) Article 1. [Google Scholar]
- 3.The AACP Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Education Outcomes. Educational Outcomes 1998. American Association of Colleges of Pharmacy. Available at http://www.aacp.org/site/page.asp?TRACKID=&VID=1&CID=1031&DID=6074. Accessed August 10, 2007.
- 4.The AACP Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Education Outcomes. Educational Outcomes 2004. American Association of Colleges of Pharmacy. Available at http://www.aacp.org/site/page.asp?TRACKID=&VID=1&CID=1031&DID=6074. Accessed August 10, 2007.
- 5.Babb VJ, Babb J. Pharmacist involvement in Healthy People 2010. J Am Pharm Assoc. 2003;43:56–60. [PubMed] [Google Scholar]
- 6.Mangum SA, Kraenow KR, Narducci WA. Identifying at-risk patients through community pharmacy-based hypertension and stroke prevention screening projects. J Am Pharm Assoc. 2003;43:50–5. [PubMed] [Google Scholar]
- 7.Giles JT, Kennedy DT, Dunn EC, et al. Results of a community pharmacy-based breast cancer risk-assessment and education program. Pharmacotherapy. 2001;21:243–53. doi: 10.1592/phco.21.2.243.34100. [DOI] [PubMed] [Google Scholar]
- 8.Cerulli J, Zeolla MM. Impact and feasibility of a community pharmacy bone mineral density screening and education program. J Am Pharm Assoc. 2004;44:161–7. doi: 10.1331/154434504773062618. [DOI] [PubMed] [Google Scholar]
- 9.MacLaughlin EJ, MacLaughlin AA, Snella KA, Winston TS, Fike DS, Raehl CR. Osteoporosis screening and education in community pharmacies using a team approach. Pharmacotherapy. 2005;25:379–86. doi: 10.1592/phco.25.3.379.61604. [DOI] [PubMed] [Google Scholar]
- 10.Dastani HB, Brown CM, O Donnell DC. Combating the obesity epidemic: community pharmacists' counseling on obesity management. Ann Pharmacother. 2004;38:1800–4. doi: 10.1345/aph.1E205. [DOI] [PubMed] [Google Scholar]
- 11.Zarembski DG, Boyer G, Vlasses PH. A Survey of advanced community pharmacy practice experiences in the final year of the PharmD curriculum at US college and schools of Pharmacy. Am J Pharm Educ. 2005;69(1) Article 2. [Google Scholar]
- 12.Ciardulli LM, Goode JVR. Using health observances to promote wellness in community pharmacies. J Am Pharm Assoc. 2003;43:61–8. [PubMed] [Google Scholar]
- 13.Haggerty SA, Cerulli J, Zeolla MM, Cottrell JS, Weck MB, Faragon JJ. A community pharmacy target intervention program (TIP) to improve aspirin use in persons with diabetes. J Am Pharm Assoc. 2005;45:17–22. doi: 10.1331/1544345052843020. [DOI] [PubMed] [Google Scholar]
- 14.Cinelli E, Cerulli J. Target intervention program to promote calcium supplement use in community pharmacy. J Am Pharm Assoc. 2004;44:268. (abstract 169). [Google Scholar]
- 15.The Seventh Report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 16.Executive summary of the Clinical Guidelines on the identification, evaluation and treatment of overweight and obesity in adults. Arch Intern Med. 1998;158:1855-67. [DOI] [PubMed]
- 17.Grundy SM, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel lll guidelines. Circulation. 2004;110:227–39. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 18.NHLBI Framingham risk calculator. Available at http://nih.nhlbi.nih.gov/atpiii/riskcalc.htm. Accessed July 14, 2004.
- 19.American Pharmacists Association, National Association of Chain Drug Stores Foundation. Medication Therapy Management in Community Pharmacy Practice: Core elements of an MTM Service (version 1.0) J Am Pharm Assoc. 2005;45:573–9. doi: 10.1331/1544345055001256. [DOI] [PubMed] [Google Scholar]
- 20.Carter JT, Draugalis JR, Slack MK, Cox ER. Algorithms for estimating learning opportunity and productivity impact at clerkship sites. Am J Pharm Educ. 1998;62:258–65. [Google Scholar]