Abstract
Objective
To incorporate human patient simulation (HPS) into a pharmacotherapy course and evaluate its impact on students' satisfaction and mastery of course objectives.
Design
Various levels of HPS were used for clinical skills assessments, reinforcement of concepts previously introduced in class, and presentation of simulated patient case scenarios requiring critical-thinking and problem-solving abilities. Pre- and post-simulation examinations and a satisfaction survey instrument were administered.
Assessment
Significant improvement was seen in students' knowledge on post-simulation examinations. On problem-solving skills, the majority of student groups received a final case grade >95%. Students indicated high levels of satisfaction with the use of HPS in the course and showed increased levels of confidence in their pharmacotherapy/patient care skills.
Conclusion
Human patient simulation provided a unique opportunity for students to apply what they learned and allowed them to practice problem-solving skills. Students grew in confidence and knowledge through exposure to realistic simulation of clinical scenarios. Students showed improvement in knowledge and ability to resolve patient treatment problems, as well as in self-confidence.
Keywords: patient simulation, simulation-based education, educational technology, problem-solving skills, pharmacotherapy
INTRODUCTION
The Accreditation Council for Pharmacy Education (ACPE) standards recommend that faculty members should use educational technologies and techniques that involve various modes of educational delivery (eg, simulations and case studies) and evaluation.1 These standards increasingly support the use of computer and instructional technology, laboratory experiences, case studies, guided group discussions, and simulations to develop critical-thinking and problem-solving skills.2 Some examples include computer-based simulations,3-5 actor simulations,6 situational pharmacy simulations,7 and standardized assessments such as objective structured clinical examinations.8-9 Simulation-based learning, a new teaching mode that is being incorporated into pharmacy curricula, has potential for a broad range of applications, including human patient simulation (HPS).
HPS technology is a type of simulation-based learning that provides a unique opportunity for students to apply learned principles in a context that realistically mimics patient care, while providing a safe, controlled learning environment. This type of experience immerses the student in an interactive situation that encourages development of problem-solving and critical-thinking skills, as well as interprofessional team training.10 Instruction can be standardized to present consistent, reproducible student experiences and can be customized to meet individual or group needs. In addition, standardized assessment/debriefing capabilities provide an objective means of documenting learner behavior and outcomes.
The University of Pittsburgh School of Pharmacy implemented simulation education into the pharmacy curriculum through a collaborative relationship with the Peter M. Winter Institute for Simulation, Education, and Research (WISER). The WISER Institute is located on the University of Pittsburgh campus. The high fidelity human patient simulators at the WISER Institute have a palpable pulse; audible heart, lung, and abdominal sounds; and hemodynamic parameters (including non-invasive blood pressure and arterial pressure); in addition to having the capability to speak in response to anticipated questions. The patient simulators are controlled by SimMan software (Laerdal Corporation, Stavanger, Norway), which can be programmed with appropriate physiological responses for a patient with the clinical condition that is entered for the simulated case scenario. The simulation room is equipped with medical equipment that is commonly found in a hospital room, as well as a monitor that displays objective information pertinent to the particular case scenario. A facilitator trained in the operation of the SimMan software coordinates the simulation session from a control room adjacent to a simulation room equipped with one-way glass or from within the simulation room.
Simulation technology was used to present patient cases to pharmacy students in order to enhance their classroom learning with an opportunity to apply the knowledge they have gained in a safe setting. While previous studies have assessed the impact of HPS on gaining or reinforcing knowledge,11 within this course the simulation was used to additionally assess students' critical-thinking and problem-solving skills. The purpose of this study was to investigate the use of simulation in developing and assessing pharmacy students' ability to use critical thinking skills and knowledge in order to solve problems related to cardiovascular disease.
DESIGN
Human patient simulation was introduced to the Pharmacotherapy of Cardiovascular Disease course in August 2006 to provide an opportunity for students to practice patient care skills and apply classroom knowledge in a realistic setting. The objective for this second-professional year comprehensive disease-based course was to prepare student pharmacists to identify, resolve, and prevent drug-related problems in patients with or at risk for cardiovascular disease. Simulated patient cases were used to complement traditional teaching methods for developing clinical skills in cardiovascular pharmacotherapy, as well as critical- thinking and problem-solving assessments. Students were exposed to simulation technology in a series of progressively complex applications, which were presented to groups of 6 to 7 students every 1 to 2 weeks throughout the 15-week semester.
The first application of HPS that was implemented within this course took place during the second week of the course in September 2006 and was used for the development of basic clinical assessment skills, such as taking blood pressure and listening for heart and lung sounds, which can be accurately assessed by the reproducible responses of the simulator. Using simulation technology, students learned and practiced taking blood pressure measurements, and subsequently they were tested individually on their ability to obtain accurate and reproducible results.11
Recognizing that the pharmacotherapy of dysrhythmias is a difficult concept for students to master, we designed an observation session for students to visualize the complexity of dysrhythmia management. The simulation program displays heart rhythms on the patient's bedside monitor consistent with the diagnosis selected by the facilitator. As medication is “prescribed” for the simulated patient, the SimMan software automatically adjusts the physiologic parameters accordingly, sending visible hemodynamic parameters, including blood pressure, heart rate, temperature, respiratory rate, oxygen saturation, carbon dioxide, pulmonary artery pressure, arterial blood pressure, and continuous electrocardiogram (EKG), to a monitor. The pharmacodynamic and pharmacokinetic changes previously programmed into the software as trends create consistency in responses for all sessions. Realistic situations are mimicked when an incorrect medication is selected; the simulated patient may become asystolic and cease to breathe if not treated appropriately or if not treated within a specific timeframe.
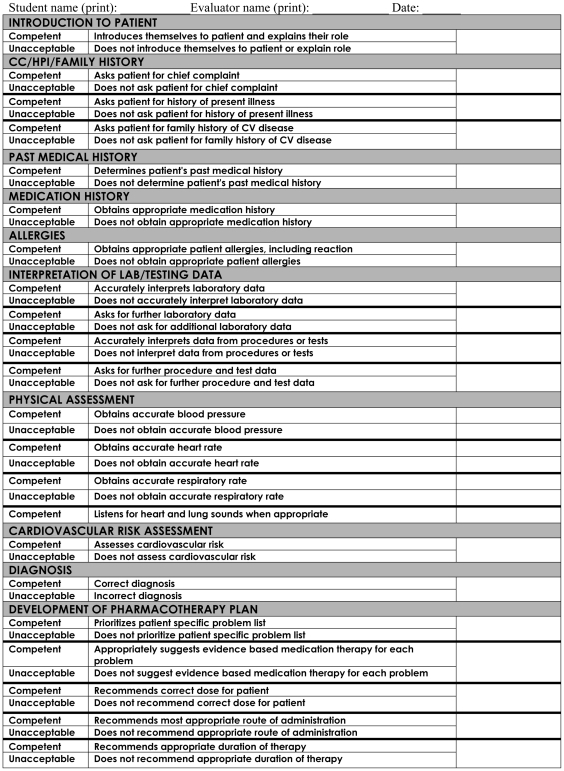
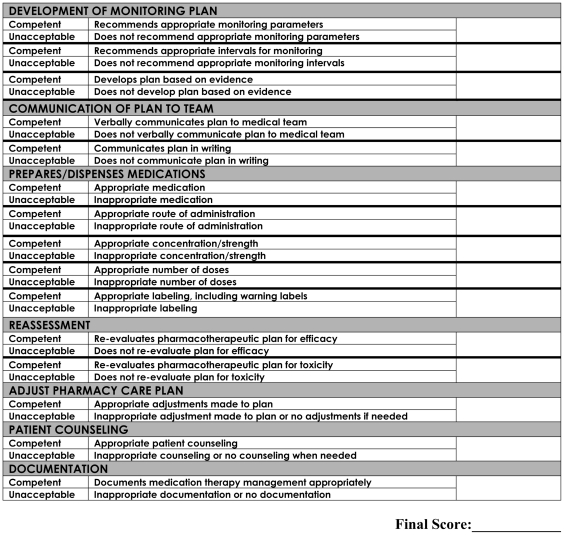
The observation session was part of a progression of exposure to HPS in order to prepare students for the final comprehensive simulation session that was used for the course grade. This final session was an opportunity for students to apply the knowledge gained throughout the semester to the process of critical thinking and problem-solving in cardiovascular medicine. Each student group encountered a simulated patient who presented with one of the following diseases: hypertensive crisis, acute coronary syndrome, acute myocardial infarction, decompensated heart failure, atrial fibrillation, ventricular tachycardia, ventricular fibrillation, or Torsade de Pointes. Student performance was assessed in the following areas: communication with the simulated patient and the session facilitator during the session; data collection and interpretation; problem list development and prioritization; pharmacotherapy plan development; monitoring plan development; and documentation of their clinical pharmacy service. The debriefing tool, which was programmed specifically for each case, provided an objective means for consistent student assessment.
The debriefing tool is a unique feature in the SimMan software programming that allows the facilitator to record each decision made by the student. The computer determined whether decisions were appropriate and given at the appropriate time based on the preprogrammed scenario, and then generated a standardized performance assessment for each simulation session. Appendix 1 includes the basic outline of the debriefing. At the end of the simulation, the facilitator displayed the debriefing tool in the simulation room, allowing immediate feedback to each student in an open environment where all students could ask questions. The log was printed so the students could keep a copy as a study reference. In addition to specific feedback for actions that were taken, each incorrect answer referenced a guideline, publication, textbook, or other learning resource for the students' further reading.
Student satisfaction with the simulated dysrhythmia and myocardial infarction portions of the course was assessed via a survey instrument administered at the end of the course. Student knowledge was determined through objective, written examinations. Completion of the survey instruments and pre- and post-simulation examinations were completely voluntary and anonymous. The data were reported here through description statistics; the chi-square test was used for categorical data. This study was approved by the Institutional Review Board at the University of Pittsburgh.
ASSESSMENT
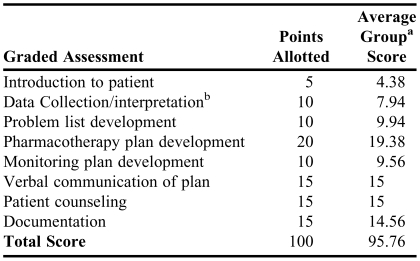
One hundred two students, 40 males and 62 females, completed the course in Fall 2006. Students were divided into 15 groups of 6 to 7 students per group for the simulation sessions. Scoring for the final case scenario is detailed in Table 1. Overall, 10 out of the 15 groups received 100% of available points and the average score for all groups was 95.8%. Student groups scored >95% on 6 out of 8 domains. Data collection and interpretation was the area where student groups received the lowest number of points; the average score was 7.9 out of 10, with only 11 of the 15 groups receiving all 10 points. Areas with the highest level of student performance included verbal communication of the plan, introduction to patient, patient counseling, and problem list development.
Table 1.
Final Case Scenario and Pharmacotherapy Plan Development in a Pharmacotherapy Course Using Human Patient Simulation
aThe class was divided into 15 groups of 6-7 students
bData collection/interpretation included: physical assessment, patient history, medication history, and diagnosis
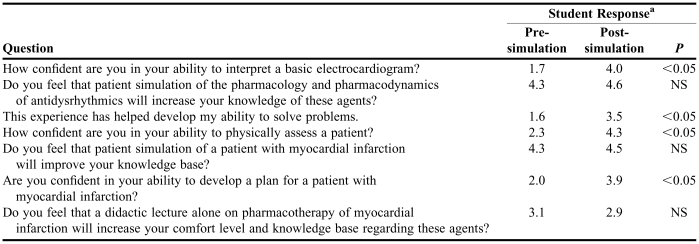
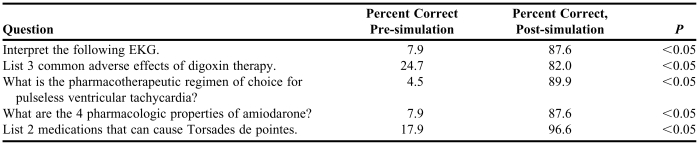
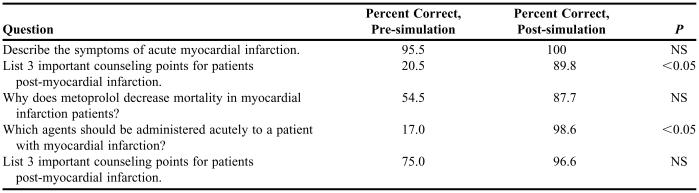
Eighty-nine of the 102 students completed the satisfaction survey (Table 2). Improvement was seen in student confidence related to performing physical assessment and interpreting patient data. Students felt that simulation would improve their ability to solve problems and develop pharmacotherapy plans. Table 3 includes pre- and post-simulation examination scores on dysrhythmia management. After visualizing pharmacokinetic and pharmacodynamic properties of several antidysrhythmic agents during the HPS experience, students' understanding of those properties and the adverse effects they cause improved. In addition, students' knowledge of counseling patients with myocardial infarction at the time of discharge and in selecting appropriate acute pharmacotherapy for these patients improved (Table 4).
Table 2.
Pharmacy Students' Survey Responses Before and After Participation in a Pharmacotherapy Courses Using Human Patient Simulation (N = 89)
aResponses were based on a Likert scale of 1 to 5 on which 1 = poor or strongly disagree and 5 = excellent or strongly agree
Table 3.
Pharmacy Students' Pre- and Post-simulation Examination Scores on Dysrhythmia Management (N = 89)
Table 4.
Pharmacy Students' Pre- and Post-Simulation Examination Scores on Myocardial Infarction (N = 89)
During the final course evaluation for the semester, student comments showed that simulation “…gave us the opportunity to evaluate a patient before the responsibility of a patient's life is placed in our hands. This is an effective teaching and learning method” and that simulation “…was one of the best learning experiences that I've ever had.” Students also commented that “…providing an opportunity to reinforce the skills and knowledge gained in the class helps me remember the information more effectively” and that this “…opportunity to think on our feet is a great chance for us to build our confidence in our knowledge of drugs.”
DISCUSSION
The use of HPS within our course provided an opportunity for pharmacy students to safely practice clinical assessment skills and apply their knowledge at no risk to patients and minimal risk to self. Both objective evaluations of students' knowledge and performance as well as student survey responses show that HPS can be advantageous within a pharmacy curriculum. Student comments show that the immersive learning environment offered by simulation sessions allows for practical application and reinforcement of knowledge. According to the results of student surveys, the HPS experience gave students more confidence in their ability to care for patients. Student pre- and post- simulation examination scores show significant improvement in knowledge, especially in the areas of patient counseling and adverse drug effects.
The systematic and objective approach provided by the computerized debriefing tool was helpful in assessing problem-solving skills and in isolating the areas of weakness in the students' clinical skills assessment ability or critical-thinking process during a clinical case simulation. By employing this unique debriefing capability, the deficiencies in collecting and interpreting patient data become apparent, allowing faculty members to reinforce this area in the debriefing session or throughout the remainder of the course. For example, based on a deficiency noted during simulation sessions, faculty members reviewed the method of the decision-making process regarding laboratory and diagnostic data when evaluating patient data during classroom teaching.
The debriefing tool provides a standardized assessment with an accurate measurement of curricular outcomes upon conclusion of the session. Students learn from the immediate and specific feedback regarding steps that were done well and areas to improve. This type of objective assessment for the students is not always available during experiential rotations, where feedback may be more sporadic or subjective and may not include as much detail. Another benefit to this standardized assessment is for faculty members to easily and objectively evaluate student responses to an entire case scenario, providing a reliable and reproducible score from session to session.
Another advantage of HPS is the ability to use repetitive practice in developing clinical skills. For example, students are able to repeat blood pressure measurements to verify consistency of technique and accuracy of results. This is not easily done using real patients, since the exact blood pressure is not known for each patient as it can vary even from one measurement to the next. Data showing significant improvement in students' knowledge and clinical performance of blood pressure measurements when using HPS in the curriculum have been published previously.11
Published evidence on high-fidelity medical simulations to date suggests that the use of simulation facilitates learning when used under the right conditions.12 Some of these conditions include providing feedback during the learning experience, engaging learners in repetitive practice, integrating simulation sessions into the overall curriculum, individualizing learning experiences, and providing clearly defined and measured outcomes.12 HPS allows for standardized assessments to document achievement of course objectives, thus adding utility and credibility to this type of learning.
Another program using simulation technology documented high levels of student satisfaction, even when simulation is used on a one-time basis within a course.13 However, one analysis reported a positive association between the number of hours of simulation-based practice and attainment of standardized learning outcomes.14 HPS technology can be used for simple and complex scenarios, tailoring the session to meet the needs of the curriculum. The multiple exposures to HPS used within our course in a progression of increasing complexity involved clinical skills assessment, observational learning, and critical-thinking and problem-solving skills assessment. Allowing students to first become comfortable with the patient simulation technology and familiar with the skills and knowledge that would be required for the sessions enabled the fair use of the HPS in evaluations that counted toward the final course grade.
National organizations, including Association of American Medical Colleges (AAMC) and ACPE have supported the use of simulation throughout healthcare education because of the numerous advantages the technology offers, including: presenting realistic situations that can be used to observe or assess application of knowledge, providing a safe and immersive learning environment, allowing an opportunity for repetitive practice, exposing students to critical or rare events that may not be encountered in advance pharmacy practice experiences (APPEs), providing reliable and reproducible responses, and finally, enhancing critical-thinking and problem-solving skills.10 Simulation technology has been successfully incorporated into the pharmacy curriculum at our institution in a number of courses.11,15
The goal of pharmacy curricula is to prepare students to optimize pharmaceutical care at the level of a pharmacotherapy generalist. Repetitive practice with various disease states and a standardized approach to problem solving provide an avenue for preparing students to be generalist pharmacists. This type of practice reinforces concepts gained through traditional education approaches in addition to the experience that the students will gain while on experiential learning rotations. One comparative assessment of the use of simulation in APPEs shows that HPS improves student knowledge to a higher degree than traditional didactic lecture alone.16 Similar results were found in studies with medical students, where simulation-based training was shown to be superior to problem-based learning during experiential learning rotations.17
A limitation of this study is that HPS was incorporated into the curriculum and not added as an independent research study, so it was not possible to establish a control group. Our institution does not allow for such a comparison in large classroom settings. Students are given a grade for this course, so they must all receive the same teaching strategies. The best way to achieve this type of comparison is to perform a crossover trial; however, time constraints and class size make this difficult to perform.
Incorporating human patient simulation teaching technology into pharmacy education has potential benefits, but a drawback to this technology is the accessibility of this type of center and the training that is required to program case scenarios for educational purposes. Obviously, use of HPS technology will not be attainable by every school; however, at the time of this writing, at least 9 schools of pharmacy utilize HPS and 5 more schools plan to utilize HPS in the near future. Pharmacy schools can collaborate with medical or nursing schools that already have simulation capabilities in order to introduce human patient simulation into their curricula. Numerous medical centers have simulation training programs for healthcare providers, so alternatively, pharmacy schools could explore educational partnerships with healthcare centers. Collaborations between pharmacy faculty members in developing and sharing cases that have already been developed will further facilitate use of this technology among schools of pharmacy.
SUMMARY
Human patient simulation provided a unique immersive and engaging learning opportunity for students in a Pharmacotherapy of Cardiovascular Disease course to apply what they learned in the classroom. Simulation technology created a safe environment for students to completely assess a “patient” from the point of introducing themselves to the implementation of a treatment plan they devised during the simulation session. Students grew in confidence and knowledge of cardiovascular pharmacology through exposure to simulation technology. Faculty members may derive an added benefit through the use of computer debriefing capabilities for objectively assessing student performance.
The profession of pharmacy is constantly striving to improve patient care by training future pharmacists to manage medication therapy for patients. Human patient simulation offers a unique immersive and engaging learning environment that fosters achievement of high levels of clinical performance. As we continue to utilize human patient simulation, other applications should be explored throughout our curricula by combining this innovative educational technology with traditional methods of learning.
PHARMACOTHERAPY PLAN: Pharmacotherapy of Cardiovascular Disease
REFERENCES
- 1.ACPE. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, Standard 25.7. Chicago, Ill: 2006. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed on July 13, 2007.
- 2.ACPE. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree, Standard 11.2. Chicago, Ill: 2006. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed on July 13, 2007.
- 3.MacKinnon GE, 3rd, Pitterle ME, Boh LE, DeMuth JE. Computer-based patient simulations: hospital pharmacists' performance and opinions. Am J Health-Syst Pharm. 1992;49:2740–5. [PubMed] [Google Scholar]
- 4.Morrison DJ. Computer simulation as a teaching aid in pharmacy management–Part 2. Stock control. J Clin Pharm Ther. 1987;12:261–5. doi: 10.1111/j.1365-2710.1987.tb00536.x. [DOI] [PubMed] [Google Scholar]
- 5.Wellman GS, Larson R. Using web-based prescription simulations as an active learning tool in an integrated practice skills laboratory. Am J Pharm Educ. 2002;66:411–5. [Google Scholar]
- 6.Nastasic S, Horne R, Davies G. The design and evaluation of a simulated-patient teaching programme to develop the consultation skills of undergraduate pharmacy students. Pharm World Sci. 2001;23:212–6. doi: 10.1023/a:1014512323758. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton WR, Padron VA. Instilling practical knowledge about nonprescription drug use. Am J Pharm Educ. 2005;69(5) Article 84. [Google Scholar]
- 8.Austin Z, O'Byrne C, Pugsley J, Quero Munoz L. Development and validation processes for an objective structured clinical examination (OSCE) for entry-to-practice certification in pharmacy: The Canadian experience. Am J Pharm Educ. 2003;67 Article 76. [Google Scholar]
- 9.Austin Z, Gregory P, Tabak D. Simulated patients vs. standardized patients in objective structured clinical examinations. Am J Pharm Educ. 2006;70 doi: 10.5688/aj7005119. Article 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Association of American Medical Colleges Institute for Improving Medical Education. Effective use of educational technology in medical education: Colloquium on educational technology: recommendations and guidelines for medical educators; 2007. Available at: http://services.aamc.org/Publications/index.cfm?fusaction=Product.displayForm&prd_id=184&prv_id=224&cfid=1&cftoken=69. Accessed on July 13, 2007.
- 11.Seybert AL, Barton CM. Simulation-based learning to teach blood pressure assessment. Am J Pharm Educ. 2007;71 doi: 10.5688/aj710348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005;27:10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez R, Parker D, Kalus JS, Miller D, Compton S. Using a human patient simulation mannequin to teach interdisciplinary team skills to pharmacy students. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710351. Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGaghie WC. Effect of practice on standardized learning outcomes in simulation-based medical education. Med Educ. 2006;40:792–7. doi: 10.1111/j.1365-2929.2006.02528.x. [DOI] [PubMed] [Google Scholar]
- 15.Seybert AL, Laughlin KK, Benedict NJ, Barton CM, Rea RS. Pharmacy student response to use of patient simulation mannequins to teach performance-based pharmacotherapeutics: A novel approach. Am J Pharm Educ. 2006;70 doi: 10.5688/aj700348. Article 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seybert AL, Murray CA, Barton CM. Assessment of simulation-based learning in fourth-year pharmacy students while on an experiential rotation, Abstract. International Meeting on Simulation in Healthcare. 2007 [Google Scholar]
- 17.Steadman RH, Coates WC, Huang YM, Matevosian R, Larmon BR, McCullough L, Ariel D. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–7. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]