Abstract
Objective
To determine the impact of the Patient Empathy Modeling pedagogy on students' empathy towards caring for the underserved during an advanced pharmacy practice experience (APPE).
Design
Pharmacy students completing an APPE at 2 primary care clinics participated in a Patient Empathy Modeling assignment for 10 days. Each student “became the patient,” simulating the life of an actual patient with multiple chronic diseases who was coping with an economic, cultural, or communication barrier to optimal healthcare. Students completed the Jefferson Scale of Physician Empathy (JSPE) before and after completing the assignment, and wrote daily journal entries and a reflection paper.
Assessment
Twenty-six students completed the PEM exercises from 2005-2006. Scores on the JSPE improved. Students' comments in journals and reflection papers revealed 3 major themes: greater appreciation of the difficulty patients have with adherence to medication and treatment regimens, increased empathy for patients from different backgrounds and patients with medical and psychosocial challenges, and improved ability to apply the lessons learned in the course to their patient care roles.
Conclusion
A Patient Empathy Modeling assignment improved pharmacy students' empathy toward underserved populations. Integrating the assignment within an APPE allowed students to immediately begin applying the knowledge and insight gained from the exercise.
Keywords: patient empathy modeling, underserved patients, empathy, cultural competence
INTRODUCTION
Pharmacy education often focuses on didactic knowledge to ensure that quantitative information and clinical skills are learned. However, therapeutic knowledge and skills are only 2 of many essential components in the delivery of pharmacy care. Providing quality patient-centered care also requires students to learn how to interact with diverse patients effectively, as well as appreciate the social, interpersonal, and individual differences that can influence how patients use medications to cope with chronic illnesses and barriers to optimal healthcare.1 Healthcare professionals' limited understanding of caring for patients who face economic, cultural, or linguistic barriers can generate negative attitudes and stereotypes toward this vulnerable population.1-5 This subjectivity can consequently result in social distancing and animosity, which could compromise the quality of care delivered and further exacerbate the effects of health disparities.1
Similar disconcerting observations were evident among pharmacy students during their advanced pharmacy practice experiences (APPEs,) at a primary care clinic that provides care for underserved patients.6 With growing numbers of underserved patients in the United States, multiple opportunities exist where pharmacists can implement much needed patient care services to reduce healthcare disparities among medically underserved communities. Therefore, addressing the unique needs in caring for these patients needs to become prominent throughout the pharmacy school curriculum.1
Recently, health professional curriculums have begun to incorporate content on cultural competence to address this concern.5 Although the term “cultural competence” remains controversial, this concept essentially entails the ability for one to recognize the importance of social and cultural influences on patients, considering how these factors may interact, and devise interventions that take these issues into account.5 The newly revised Accreditation Council for Pharmacy Education (ACPE) standards particularly emphasized cultural competence, health literacy, and healthcare disparity be addressed in the curriculum to further develop student' attitudes, knowledge, skills, and values in order to deliver high-quality care to diverse population.7
Irrespective of patient backgrounds, patient-pharmacist communication is a vital component of the patient's healthcare. A survey that assessed the communication skills taught to students in pharmacy schools concluded that pharmacists needed to recognize communication skills as more than a “one size fits all” clinical counseling session because of the wide variety of interpersonal interactions that occur during a patient encounter.8 Culturally sensitive empathy, defined as the need to “convey empathy in a culturally consistent and meaningful manner,” is a particularly important factor needed in order to effectively work with a culturally diverse population.9 Furthermore, intercultural disposition, which consists of ethnocentrism, empathy, world-mindedness, and attributional complexity, positively correlates with intercultural communication competence, which in turn fosters patient trust and commitment, leading to better patient adherence and improved knowledge and satisfaction with healthcare.10 Although no clear cut definition of empathy has emerged, it has been defined as the “ability to behave in a caring manner toward a patient while demonstrating to the patient that his feelings are understood.”11 It has also been described as a concept “that involves both the cognitive and affective domains.”12
The cognitive domain of empathy involves the ability to understand another person's inner experiences and feelings and a capability to view the outside world from the other person's perspective. The affective domain involves the capacity to enter into or join the experiences and feelings of another person.12
A majority of medical educators concede that empathy is a significant factor in patient care that must be cultivated in students while they are preparing for their careers.13 Particularly in the United States, managed care has contributed to creating a market-driven healthcare system that focuses on populations opposed to individuals, which can be dehumanizing to the patient.14 Spiro et al proposed “doctors can learn empathy by putting themselves in their patient's place.”15 One pedagogy in medical education that encouraged second-year medical students to be more empathetic involved a voluntary hospitalization experience.16 When the study was completed, the students were generally appalled at the low quality of care provided by the attending physicians during their voluntary hospitalization; leading the researchers to believe these students would be more mindful of their patients as future practicing physicians. In another study, preclinical medical students were required to shadow a patient and experience healthcare from the patients' perspective.17 The majority of the medical students felt empathy for the patients they accompanied. In a separate study, St. Louis College of Pharmacy implemented the Geriatric Medication Game, a role-playing board game designed to increase pharmacy students' awareness of the physical and financial challenges elderly patients encounter as they navigate the healthcare system.18 Utilization of the Geriatric Medication Game improved students' empathy and understanding of older patients and helped them realize the need to tailor delivery of healthcare to these patients.18
Thus, both empathy and cultural competence are essential for pharmacists to provide quality patient-centered care, but they remain difficult to foster.7, 19, 20 This pedagogical innovation was designed to address the need to sensitize pharmacy students to the culture, concerns, and perspectives of underserved populations through the development of empathy towards underserved patients, and to encourage understanding of the difficulties and psychosocial challenges these patients encounter.
DESIGN
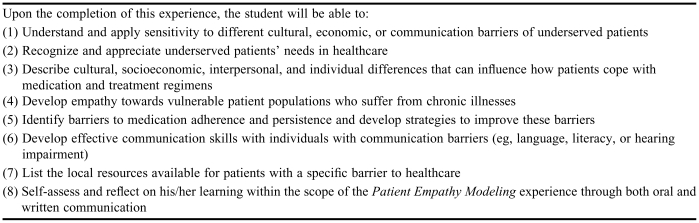
The goal of the Patient Empathy Modeling (PEM) assignment was to enhance pharmacy students' humanistic nature towards caring for underserved patients. In 2004, an APPE student at Purdue School of Pharmacy began the development of the PEM exercise for students at a primary care clinic that provided services for underserved patients (Tippecanoe Community Health Clinic). After several refinements, the PEM assignment was implemented in 2005 as a required component of the rotation at Tippecanoe Community Health Clinic (Purdue University) and at the Burgdorf Clinic (a University of Connecticut ambulatory care site). Students gained personal and professional insights as they simulated the life of an underserved patient with multiple chronic medical conditions and barriers to optimal healthcare. Table 1 lists the learning objectives of the PEM assignment.
Table 1.
Learning Objectives for the Patient Empathy Modeling Assignment
Initial development of the patient scenarios and their associated simulated activities required approximately 7 days. Once these scenarios and activities were developed, assembly of the PEM materials was performed once at the start of each academic year. The estimated assembly time was approximately 15 minutes per patient scenario; thus, the total time required depended on the number of students anticipated. During the year, faculty member and/or preceptor preparation time for each exercise consisted of administering the evaluation empathy scale pre- and post-assignment and explaining each patient scenario and activity as needed. The total time required during each APPE was usually no more than 30 minutes.
Practice environments such as the ambulatory care clinics in which this pedagogy took place provided students opportunities to directly interact with and care for a diverse patient population. Pharmacy students were fully incorporated into these clinics to provide comprehensive pharmacotherapy services and direct patient care activities with the faculty preceptor and other healthcare professionals. Students were often challenged to “think outside the box” to help these patients manage their chronic illnesses and medication regimens. APPEs at these practice sites aimed to help students gain an appreciation of the challenges and rewards of caring for underserved patients.
The Tippecanoe Community Health Clinic (TCHC) is a multidisciplinary, non-profit, Federally Qualified Health Center located in rural Lafayette, Indiana. The service area was considered a medically underserved and “high risk” area due to a lack of participating Medicaid providers. The patient population consisted primarily of Caucasian and Hispanic patients. The clinic was dedicated to serving underserved residents and provided coordinated primary healthcare to all age groups. Two students from Purdue University School of Pharmacy were assigned to TCHC for 2-month APPEs. During their APPEs, students had the opportunity to foster a trusting relationship with their patients, refine their patient counseling skills, and promote continuity of care. Visits to local homeless shelter(s) and contribution in various staff and patient education sessions were also integrated into the rotation.
The Burgdorf Clinic is a multidisciplinary urban primary care clinic that provided a full range of primary care and specialty healthcare services to underserved residents living in the North End of Hartford, Connecticut. The patient population consisted primarily of African-American, West Indian, and Latino patients. Students from the University of Connecticut (UConn) School of Pharmacy assigned to the clinic completed their required ambulatory care APPE there over a 1-month period.
During the PEM assignment (known to students as the “patient challenge simulation”), each student “became the patient” to simulate the life of an actual patient with multiple chronic diseases who also had an economic (eg, homeless), cultural (eg, Hispanic), or communication barrier (eg, illiterate or hearing-impaired) to obtaining optimal healthcare. In these scenarios, students experienced structured, non-threatening situations that challenged them to live the life of an underserved patient coping with medication adherence, and at the same time challenged them to confront any pre-existing personal prejudices.
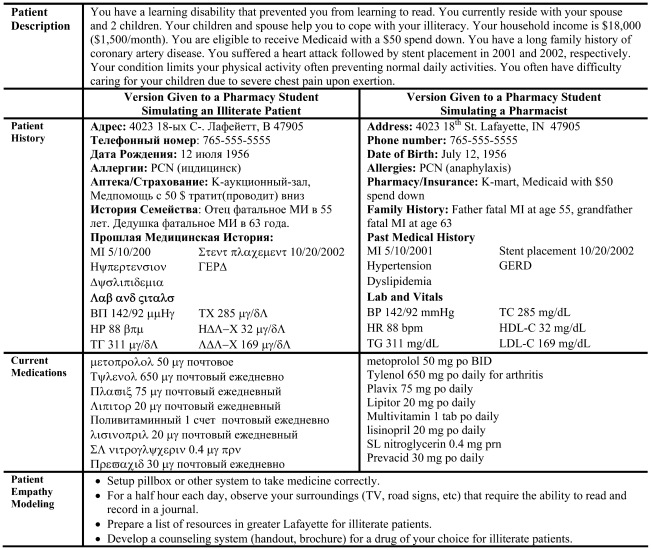
Within the first 2 days of the APPE, students were randomly assigned to complete 1 of 4 PEM patient scenarios. UConn students completing a 1-month APPE at the Burgdorf Clinic were assigned 1 patient scenario to complete over 10 days. Purdue University students completing a 2-month APPE at TCHC were given 2 separate PEM assignments, with 1 patient scenario involving a communication barrier, to complete sequentially over 10 days each. All students received a pass or fail grade for this exercise. Four variations of simulated patient scenarios were developed based on the typical characteristics of commonly encountered patients at the clinics. Each patient scenario contained a detailed patient description, patient history with pertinent social and medical history, current medications, and individualized instructions for the specific PEM assignment. At the time of assignment, the preceptor described the assigned patient scenario to the student. Then students were supplied with a patient profile, blank journal, labeled prescription vials filled with placebos, and earplugs (if the student was simulating a hearing-impaired patient). For example, students assigned to role-play as “Jamie Illiterate,” a patient suffering from a learning disability and inability to read, received the entire patient profile, PEM instructions, and labeled prescription vials written in unintelligible text to mimic a realistic patient situation (Table 2). The student was then instructed to schedule a one-time counseling session with a pharmacist (role-played by another student) who provided proper directions for taking the medications and simulated associated challenges the patient might encounter. The student who role-played as the pharmacist had the entire patient profile in English (Table 2) and provided assistance to help his or her colleague in understanding the medication instructions without disclosing the legible key. Sensitization tasks for students role-playing as “Jamie Illiterate” included observing things in their surroundings that required them to read (eg, road signs, patient education handouts, job applications) and then reflecting on this in their daily journal.
Table 2.
Example Scenario Given to Students Participating in a Patient Empathy Modeling Assignment for an Advanced Pharmacy Practice Experience
Each simulated patient carried diagnoses of multiple chronic diseases commonly evaluated at primary care clinics, including hypertension, type 2 diabetes mellitus, asthma, depression, coronary artery disease, hypothyroidism, arthritis, and/or dyslipidemia. All students received oral “placebo medications” (candy) precounted and placed in labeled prescription vials with patient name and instructions for administration. A placebo dry powder inhaler and metered dose inhaler were also provided to students if the patient scenario required inhalers for asthma control. Prescription vials were labeled in unintelligible text for the “Jamie Illiterate” scenario and in Spanish for the Hispanic patient scenario.
All students were instructed to set up pillboxes or other systems for storing their placebo medications and consciously perform the act of taking their “medications” at the time indicated, and to use devices appropriately and as prescribed to the best of their ability. Students were advised that they were not evaluated based on the degree of medication adherence but on their honesty in journaling their experiences during the learning process.
Common to all the scenarios were the instructions for students to learn about the community resources available for the simulated patients with health barriers. The students were asked to share a list of the resources with the preceptor and other students. This created an opportunity for the students to feel more connected to the community they served and provided them with resources they could later use in patient care.
At the completion of the assignment, a debriefing session was scheduled for students to provide verbal feedback to their preceptor and colleagues regarding their experiences. The preceptor utilized this time with students to provide insights on how actual patients coped with the various medical and psychosocial barriers as well the resources available to healthcare professionals to assist patients in overcoming these barriers. For students, the time required to complete the simulated activities depended on the patient scenario and the skill of each individual student in performing the assigned activities. The PEM activities were designed so they could be incorporated into the students' daily schedule with minimal time investments.
The effectiveness of this pedagogy was quantitatively assessed using the Jefferson Scale of Physician Empathy (JSPE) for physician and health professionals (“HP” version).12 The “HP” version of JSPE is a validated, brief self-report consisting of 20 Likert-type items on a 7-point scale (ranging from 1= strongly disagree to 7 = strongly agree) that encompasses 3 underlying factors: perspective taking, compassionate care, and ability to stand in a patient's shoes.12 The JSPE has been tested and validated in medical students and physicians.13 Responses from the negatively worded items were inverse-scored and the positively worded items were scored directly to compute a summary score. An example of a directly scored item was, “I try to imagine myself in my patients' shoes when providing care to them.” An example of an inverse-scored item was “because people are different, it is almost impossible for me to see things from my patients' perspectives.” A higher score reflected a more empathetic respondent. Students anonymously completed the questionnaire twice, before and after the PEM assignment. All students were encouraged to answer the questionnaire as honestly as possible as their responses were anonymous and therefore not graded.
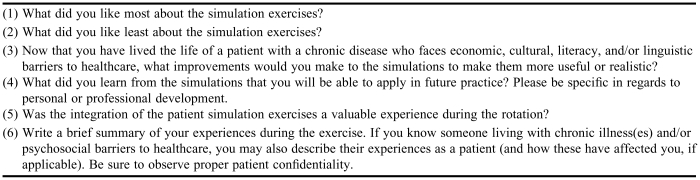
Qualitative learner-focused assessments included journal entries and a final reflection paper. During the exercise(s), students were instructed to reflect daily in journal entries describing their experience of learning to cope with the assigned challenges, as they “became the patient.” After the first 6 students completed PEM, a reflection paper was developed for all subsequent students to use in critically evaluating the assignment (Table 3). Requirements for Institutional Review Board approval have been exempted from Purdue University and UConn to conduct retrospective analyses.
Table 3.
Reflection Assignment for Students Who Completed an Advanced Pharmacy Practice Experience Involving Patient Empathy Modeling
ASSESSMENT
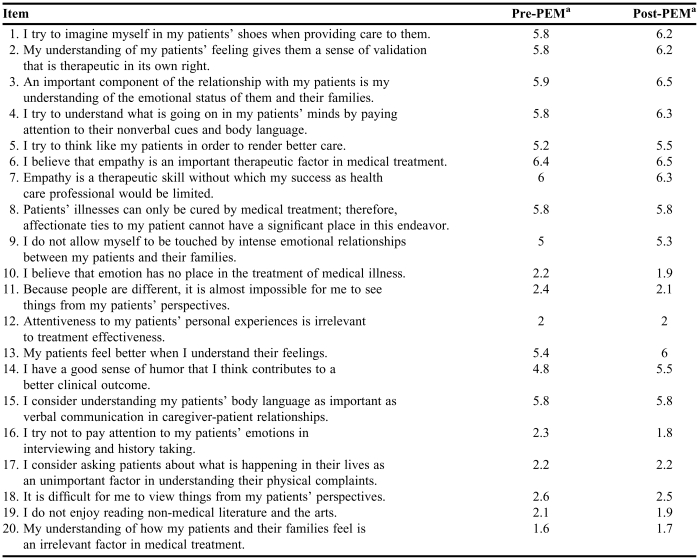
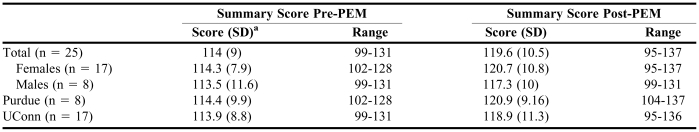
Twenty-six students from both schools completed the PEM exercises between 2005 and 2006. Completed JSPE data are available for 25 students as 1 student did not answer all questions on the pre-PEM JSPE. Students' empathy as measured by the JSPE improved as a result of undergoing the PEM exercises. Changes in the mean scores for each item on the JSPE are shown in Table 4. The post-PEM score improved for 9 of the 10 statements related to perspective taking, 4 of the 7 statements related to compassionate care, and all of the statements related to their ability to stand in the patient's shoes. The post-PEM scores for statements 8, 12, 15, and 17 were unchanged and the post-PEM score for statement 20 only increased slightly from 1.6 to 1.7. Overall, the JSPE summary scores increased after completion of the exercises (Table 5). The JSPE summary scores for both pre- and post-PEM were slightly higher for female students than male students. Similarly, the change in the mean summary score was slightly higher for female students compared to male students and for Purdue University students who completed 2 patient scenarios compared with UConn students who completed only 1 scenario. Due to the small sample size, statistical analyses to identify significant differences between the pre- and post-summary scores or between the subgroups could not be performed.
Table 4.
Mean Scores From the Jefferson Physician Scale of Physician Empathy (HP version) Pre- and Post-Patient Empathy Modeling (n = 25)
Abbreviations: PEM = Patient Empathy Modeling
aItems are scored on a scale of 1 to 7 (1 = strongly disagree, 7 = strongly agree). Items 8-12 and 16-20 are negatively-worded items and are scored accordingly. A higher score on the positively-worded item indicates higher empathy. A lower score on the negatively-worded items indicates higher empathy12,13
Reprinted with permission from Dr. Mohammadreza Hojat, Jefferson Medical College, Thomas Jefferson University. Copyright 2002 Jefferson Medical College. All rights reserved. This scale has been slightly modified. Information about the new version is available at the following web site: www.tju.edu/jmc/crmehc/medu/oempathy.cfm
Table 5.
Summary Scores from the Jefferson Physician Scale of Physician Empathy (“HP” version) Pre- and Post-Patient Empathy Modeling Assignment
Abbreviations: PEM = Patient Empathy Modeling; SD= standard deviation; Purdue = School of Pharmacy and Pharmaceutical Sciences, Purdue University; UConn = University of Connecticut School of Pharmacy
ahigher summary score indicates higher empathy; the maximum score possible is 140
An examination of the journal entries revealed how the students adapted to their patient scenarios and gradually developed an understanding of the challenges faced by patients with chronic illnesses and psychosocial barriers to healthcare. Journal entries were available for all 26 students completing the PEM assignment. A majority of the students (77%) reported at least partial non-adherence to taking the “placebo medications,” especially during weekends, and expressed frustration with their non-adherence. One student commented, “I just feel like my whole day revolves around taking my pills!” Approximately 27% of the students also reported difficulty with carrying out some of their assigned activities, such as sleeping on the floor for 1 night (for the homeless patient scenario). Conversely, a few students stated they especially enjoyed their PEM activities, particularly those students assigned to the Hispanic patient scenario since it gave them a chance to learn Spanish and immerse themselves in some aspect of Hispanic culture. Interestingly, 7 students developed a story line for their assigned simulated character and “invented” challenges their character encountered each day (eg, a homeless patient attempting to find employment who experienced difficulty completing the employment application because he did not have a permanent address). These students reported their imaginations helped them enter the mindset of their character because the life of their assigned character was completely foreign to them.
The reflection paper completed at the end of the PEM period provided a descriptive window into how each student viewed the activities, what they learned, and any self-reported attitude or behavior changes. All students reported that they found the assignment valuable and it made them aware of the challenges faced by patients with chronic illnesses and psychosocial barriers to healthcare. A content analysis of both the reflection paper and journal entries identified 3 main themes that were expressed by at least half of the students. Students expressed they came to appreciate the difficulty of treatment adherence and developed empathy for patients with medical and psychosocial challenges and how underserved patients may cope with these, and therefore, learned valuable lessons that could be applied to their professional practice.
Three themes were identified from student comments. First was an appreciation of the difficulty with medication and treatment regimen adherence faced by patients with chronic illnesses. As one student expressed: “I found it difficult to remember to take my medications everyday. I actually realized how much it changes your everyday routine and how much responsibility it takes to be a compliant patient… Not only do you have to take your medications, but you also have to worry about doctor visits, lab tests, and even refilling your prescriptions.”
A second theme evident in the student's comments was an appreciation of, and empathy for, patients from different backgrounds and with medical and psychosocial challenges. One student commented: “I enjoyed essentially being in someone else's shoes for 10 days. It wasn't easy but it was a good experience to really see life in someone else's perspective. It essentially changed my view and allowed me to think in ways that I had never thought of before.”
A third theme identified was the applicability of the lessons learned to patient care roles. As one student said: “I learned how to put myself in the position of a patient who is non-compliant, and to ask myself why this is the case. Do they have economic or other limitations? What do I have to do as a pharmacist to make it easier for this person to take their medications: ie, cheaper alternatives, filling pillboxes, etc. I also learned how to interact better with patients of other cultures and make resources for illiterate patients.”
DISCUSSION
The goal of the PEM assignment was to enhance pharmacy students' humanistic nature toward caring for the underserved. Our experience has shown that pharmacy students can easily adopt negative stereotypes toward the indigent population.6 Disparities between the qualities, characteristics, and social standing of healthcare professionals and their patients may foster considerable social distancing from this population, negatively affecting the quality of patient care delivered.4 Thus, an important way of reframing negative stereotypes is to bring students into closer contact with patients who are different and increase their understanding of this population.1, 21 The PEM patient scenarios encompass common chronic illnesses and psychosocial challenges facing the underserved. As the students “become the patient” in a structured environment, they become sensitized to the culture, concerns, and perspectives of underserved patients through development of empathy for this population. Furthermore, students gain an understanding of the difficulties and psychosocial circumstances underserved patients encounter. This study suggested that regardless of practice settings (urban [UConn] or rural [Purdue]) or number of PEM assignments completed (1 or 2), improvements in students' empathy scores were similar and applicable across a wide range of patient scenarios.
In accordance with the revised ACPE standards,7 this pedagogy presents an essential and unique learning experience for pharmacy students to help bridge an existing curricular gap: teaching cultural competence and empathy related to the underserved. As one student who completed the exercise reflected, “It opened my eyes to a lot of new things and made me think about other patient issues we normally don't discuss or talk about in classes.”
The nature of this pedagogy is not inherently easy. Students were asked to experience a different walk of life and view the world from a different perspective than what they may be used to. They become aware of the harsh realities behind many issues affecting today's society. As each student “becomes the patient” and attempts to overcome the assigned barrier, s/he becomes engaged in a unique active-learning experience. These patient-centered learning activities enhanced students' ability to think independently and developed creative problem-solving skills. For example, students who role-played as the pharmacist counseling “Jamie Illiterate” designed pictograms to help the “patient” understand proper medications instructions. The essence of this exercise requires students to take initiative in undertaking the assigned tasks. Nonetheless, in spite of the inherent frustrations and difficulties students expressed throughout their journey, many reflected the PEM assignment was a positive and eye-opening learning experience. Integrated as part of a clinical rotation, the assignment reinforced the concept of needing to take into account socioeconomic, cultural, and interpersonal differences in developing patient-specific recommendations while optimizing drug therapy for a diverse patient population. Even for students who had been patients themselves, the outcomes of this exercise are still apparent, as the psychosocial profiles remain unique to each scenario.
It is important to realize that students cannot learn all of the essential pharmacist skills by sitting in a classroom, observing a preceptor, or “practicing” being a pharmacist. Pharmacy students grew to become more sensitive, empathetic and understanding of an underserved patient after “walking in a patient's shoes.” Summary JSPE scores for pharmacy students in this sample increased as a result of completing the PEM assignment. The pharmacy students' pre-PEM summary score of 114 was lower than those for third-year medical students (mean 117)13 and physicians (mean 119.1)12 as reported by the developers of the JSPE. After completion of the PEM assignment, the mean summary score increased to 119.6, a score within the range reported for physicians.12 We were not able to calculate statistical significance in the pre- and post-assignment scores (due to a small sample size) and there are no data to show how much of an increase in JSPE score translates into real clinical practice significance. However, written and verbal feedback from the students showed they viewed the assignment as a valuable experience. One student reflected, “I learned that you have to remember that every patient you deal with is different. Also, you can't be judgmental of the people you are trying to help.” While another student commented, “When we can relate to what they [patients] are going through, it shows and helps us make better clinical decisions.” A student who was assigned to the homeless patient scenario stated, “I have developed more sensitivity to the homeless and how their needs differ almost completely from a person with income. This exercise has shown me how the homeless can go ignored by health care practitioners. It has opened my eyes to the realization that the homeless too are people just like the wealthy that need equal medical attention despite their circumstances.”
It is also important for future pharmacists to consider the impact of language barriers when working with patients to optimize drug therapy outcomes.19,22 A student assigned to the “Jamie Illiterate” scenario indicated, “It gave me a sense of empathy because before this simulation I never even thought about how an illiterate person dealt with every day life.” During the rotation, this student was able to help an actual illiterate patient to locate a support group. The capability for students to instantaneously apply their learning toward daily patient care is a major benefit of implementing this pedagogy during an APPE.
Students learned about the complexities associated with medication adherence and persistence. Practitioners often feel discouraged when a patient is non-adherent to the prescribed regimens. The assignment provided students with a more in-depth perspective of reasons behind patients' difficulties with medication regimens in managing chronic illnesses. As one student shared, “I believe now I will be able to empathize with the patient and know that it takes time to change.” Many students expressed that they were more willing to go the extra mile to ensure that patients truly understand how to take their medications correctly.
The incorporation of the daily journal facilitated a continuous learning process for the students. Integration of the final reflection paper further allowed students to critically evaluate and internalize their personal issues, challenges, values, and insights. Many have developed a change in professional self-concept and attitudes. Students' comments from their final reflection further affirmed the values of this pedagogy. One student summed it up succinctly, “After a full year of rotations, it was a good reminder that as student going into practice, patient care remains the focus and an understanding of the patient's feelings is a key part of the ability to give proper care.”
Limitations
There were 3 potential limitations to our study. First, the JSPE questionnaires were distributed to the students by the preceptor, which may have introduced social desirability bias and resulted in not capturing students' true beliefs or accurately predicting their clinical behaviors. As the questionnaires were completely anonymous and non-graded, each faculty member encouraged the students to answer the questions as honestly as possible to reduce the risk of introducing the social desirability bias. In the future, administering the questionnaire online may eliminate this concern.
Second, a convenience sample was used for this retrospective study. A statistical analysis was not possible to assess changes in JSPE scores due to the small sample size. The complex and multidimensional nature of clinical empathy makes it difficult to measure. The effect of cultural competence was not assessed due to lack of an applicable validated standardized instrument. Incorporating a qualitative approach to obtaining student feedback through the reflection paper may have evaluated a wider range of student experiences and views than self-assessments.23 Ultimately, patient perceptions of how students display empathy effectively across cultures should be assessed to evaluate the effectiveness of this pedagogy.9,24
A third possible limitation was that the PEM exercises were not administered in a controlled environment. A control group was not available to compare study findings. It is unclear whether randomization of the patient scenario affected study results. Unlike other simulations discussed in the pharmacy and medical/nursing education literature, or classroom discussions or lectures conducted in a defined period and controlled environment, our pedagogy required the students to incorporate the activities into their actual lives and experience how barriers permeate all aspects of daily living. The duration of the assignment and variety of activities ensured that each day was different and brought different challenges, and therefore, learning opportunities. Diverse interactions with various patient characteristics, preceptors, healthcare professionals, and colleagues may have confounded the magnitude of our results. The effects of these confounders were too complex to control and evaluate. Nonetheless, results from this pedagogy are generalizable to true-life settings since APPEs do not occur in controlled environments.
Lessons Learned
Practicing at a medically underserved setting often creates dissonance in students' perspectives. Thus, the goal of offering a quality educational experience cannot be met by simply assigning students to a particular underserved setting and employing the PEM assignment. Students must be presented with clear objectives, coherent supervision, and strong mentoring from the preceptor to gain clinical competence and confidence in these often uncomfortable and unique practice environments. With those elements in mind, the PEM pedagogy could easily be adapted to other ambulatory care settings or health professions. With minimal time investment by the preceptors and students, each practice site could develop and integrate specific psychosocial scenarios relevant to the individual practice environment. It would probably be more meaningful to integrate this exercise in a small group rather than in a large classroom setting.
Materials used in the PEM assignment were designed to be as realistic as possible to mimic actual patient experiences. It was important for the exercise to be fully integrated into weekday and weekend activities as medication adherence is often compromised on weekends. Incorporation of food stamps and crutches would add another level of realism to the dietary and physical limitations of an underserved patient. Providing Monopoly money with a limited budget may teach students the financial constraints patients encounter. Although many students expressed a personal understanding of living on a limited budget, they still appreciated the compounded difficulties of adhering to dietary and medication regimens in the presence of financial constraints. Additional educational materials would be beneficial including first-person narratives describing patients' psychosocial challenges, patient videos, and influential films/documentaries. Furthermore, it would also be valuable for students to interview an actual patient with their assigned psychosocial challenges in order for each student to ask relevant questions and acquire a more in-depth understanding of a patient's way of life. We believe the PEM pedagogy further contributes to students' existing rotation experiences. However, the success of PEM partially depends on the amount of effort each student puts into accomplishing assigned tasks, in addition to their backgrounds, personality traits, prior experiences, and preconceived prejudices. To minimize potential confounders, this pedagogy is most effective when incorporated at the beginning of each rotation before students can develop and solidify preconceived judgments towards the underserved population.
Nevertheless, evaluating students who have completed the PEM assignment is just one piece of the puzzle. The ultimate question remaining to be answered is “Does this pedagogy improve the quality of care delivered to underserved patients?” While the literature has suggested improved patient satisfaction, adherence to medical treatments, clinical outcomes, and professional satisfaction are correlated with increased empathy, these evidence remain inconclusive.25 Assessment for durability of effects from this pedagogy was not possible. Thus, it remains uncertain whether the students who completed these brief exercises will, in fact, be more empathetic toward diverse patients in future practice settings. For some students, improved performance may not be evident immediately, but may emerge later in their career. We hope the perceived changes in student values and attitudes will lead to a genuine appreciation of the uniqueness of each patient they encounter in their future practice and further development and use of the skills they learned during these rotations. Such commitment and compassion will enable each pharmacist to deliver quality patient-centered care for patients with limited access to healthcare.
CONCLUSION
There is an increased need for all health professionals to address healthcare disparities among medically underserved communities. The PEM assignment's emphasis on healthcare disparity, health literacy, cultural competency, and issues with medication adherence in chronic disease management appeared to foster empathy among pharmacy students toward underserved patients. Integrated as part of an APPE, the PEM pedagogy promoted heightened sensitivity among students to the experience of real patients. It encouraged the development of patient-specific recommendations and tailoring of healthcare delivery to meet patient's social, cultural, and linguistic needs when optimizing drug therapy for patients of diverse backgrounds. Further studies should evaluate the impact of this pedagogy on other health professionals in their career development or in a classroom setting to enhance students' humanistic nature toward caring for diverse patient populations.
ACKNOWLEDGEMENTS
This study was previously presented at the American Association of Colleges of Pharmacy Annual Meeting and Seminars, San Diego, Calif, July 10, 2006, and at the International Society for the Scholarship of Teaching and Learning Conference, Washington, DC, November 11, 2006.
The authors wish to thank all the students who have participated in the exercise for their efforts. Our appreciations are also extended to Mrs. Melinda Schultz for assistance with the packaging of the supplies, Dr. Kimberly Plake for her helpful suggestions on this project, and Dr. Karen Rausch for assistance with the initial development and design of the Patient Empathy Modeling exercises.
REFERENCES
- 1.Shaya FT, Gbarayor CM. The case for cultural competence in health professions education. Am J Pharm Educ. 2006;70(6) doi: 10.5688/aj7006124. Article 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buchanan D, Rohr L, Kehoe L, Glick SB, Jain S. Changing attitudes toward homeless people. J Gen Intern Med. 2004;19:566–8. doi: 10.1111/j.1525-1497.2004.30111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Toole TP, Hanusa BH, Gibbon JL, Boyles SH. Experiences and attitudes of residents and students influence voluntary service with homeless populations. J Gen Intern Med. 1999;14:211–6. doi: 10.1046/j.1525-1497.1999.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malat JR, van Ryn M, Purcell D. Race, socioeconomic status, and the perceived importance of positive self-presentation in health care. Soc Sci Med. 2006;62:2479–88. doi: 10.1016/j.socscimed.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Beach MC, Price EG, Gary TL, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care. 2005;43:356–73. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen JT, Plake KS, Darbishire PL. Clerkship students' perceptions of caring for underserved patients [abstract]. 106th Annual Meeting, Cincinnati, Ohio, July 9-13, 2005. Am J Pharm Educ. 2005;69(3) Article 60. [Google Scholar]
- 7.Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Accreditation Council for Pharmacy Education. Adopted January 15, 2006; Released February 17, 2006; Effective July 1, 2007. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed October 12, 2006.
- 8.Beardsley RS. Communication skills development in colleges of pharmacy. Am J Pharm Educ. 2001;65:307–14. [Google Scholar]
- 9.Chung RCY, Bernak F. The relationship of culture and empathy in cross-cultural counseling. J Couns Dev. 2002;80:154–9. [Google Scholar]
- 10.Shah MB, King S, Patel AS. Intercultural disposition and communication competence of future pharmacists. Am J Pharm Educ. 2004;68(5) Article 111. [Google Scholar]
- 11.Lonie JM, Alemam R, Dhing C, Mihm D. Assessing pharmacy student self-reported empathic tendencies. Am J Pharm Educ. 2005;69(2) Article 29. [Google Scholar]
- 12.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 13.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77:S58–60. doi: 10.1097/00001888-200210001-00019. [DOI] [PubMed] [Google Scholar]
- 14.Hojat M, Mangione S, Nasca TJ, Gonnella JS, Magee M. Empathy scores in medical school and ratings of empathic behavior in residency training 3 years later. J Soc Psychol. 2005;145:663–72. doi: 10.3200/SOCP.145.6.663-672. [DOI] [PubMed] [Google Scholar]
- 15.Spiro H, Curnen MG, Peschel E, St. James D. Empathy and the Practice of Medicine. New Haven: Yale University Press; 1993. [Google Scholar]
- 16.Wilkes M, Milgrom E, Hoffman JR. Towards more empathic medical students: a medical student hospitalization experience. Med Educ. 2002;36:528–33. doi: 10.1046/j.1365-2923.2002.01230.x. [DOI] [PubMed] [Google Scholar]
- 17.Henry-Tillman R, Deloney LA, Savidge M, Graham CJ, Klimberg VS. The medical student as patient navigator as an approach to teaching empathy. Am J Surg. 2002;183:659–62. doi: 10.1016/s0002-9610(02)00867-x. [DOI] [PubMed] [Google Scholar]
- 18.Evans S, Lombardo M, Belgeri M, Fontane P. The geriatric medication game in pharmacy education. Am J Pharm Educ. 2005;69(3):304–10. [Google Scholar]
- 19.Mullins CD, Blatt L, Gbarayor CM, Yang HW, Baquet C. Health disparities: a barrier to high-quality care. Am J Health-Syst Pharm. 2005;62:1873–82. doi: 10.2146/ajhp050064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spiro H. What is empathy and can it be taught? Ann Intern Med. 1992;116:843–6. doi: 10.7326/0003-4819-116-10-843. [DOI] [PubMed] [Google Scholar]
- 21.Schumann W, Moxley DP, Vanderwill W. Integrating service and reflection in the professional development of pharmacy students. Am J Pharm Educ. 2004;68(2) Article 45. [Google Scholar]
- 22.Westberg SM, Sorensen TD. Pharmacy-related health disparities experienced by non-english-speaking patients: impact of pharmaceutical care. J Am Pharm Assoc. 2005;45:48–54. doi: 10.1331/1544345052843066. [DOI] [PubMed] [Google Scholar]
- 23.Boud D, Keogh R, Walker D. Promoting reflection in learning: a model. In: Richards R, Hanson A, Raggatt P, editors. Boundaries of Adult Learning. New York: Routledge; 1996. pp. 23–46. [Google Scholar]
- 24.Squier RW. A model of empathic understanding and adherence to treatment regimens in practitioner-patient relationships. Soc Sci Med. 1990;30:325–39. doi: 10.1016/0277-9536(90)90188-x. [DOI] [PubMed] [Google Scholar]
- 25.Stepien KA, Baernstein A. Educating for empathy. J Gen Intern Med. 2006;21:524–30. doi: 10.1111/j.1525-1497.2006.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]