Intestinal ischemia is a condition associated with a high degree of morbidity and mortality. Mesenteric venous thrombosis is an uncommon cause of intestinal ischemia accounting for 5%–15% of such cases.1 Surgical intervention in cases of intestinal ischemia resulting from portal/superior mesenteric vein thrombosis is fraught with difficulty owing to the extent of bowel resection required and the inability to address the underlying thrombosis. We present a case report of acute intestinal ischemia secondary to portal and superior mesenteric vein (SMV) thrombosis successfully treated with tissue plasminogen activator (tPA) via the superior mesenteric artery (SMA) and splenic artery (a route not previously used for this purpose).
Case report
A previously healthy 45-year-old man presented with severe diffuse abdominal pain. He described a history of a similar milder episode 3 weeks prior, which had resolved spontaneously. He had no vomiting, melena or hematochezia. He had had no previous abdominal surgery. On presentation, he was afebrile, tachycardic and moderately dehydrated and had diffuse nonrebound abdominal tenderness. Laboratory tests were unremarkable. A contrast-enhanced CT scan of the abdomen and pelvis showed a portal vein and SMV thrombus (Fig. 1a). A heparin infusion was started with an initial bolus of 8000 u then a 1500 u/hr infusion. Over the following few hours, the patient developed peritoneal signs and increasing abdominal pain. A repeat CT scan showed progression of the thrombus and small bowel thickening (Fig. 1b) but no evidence of necrosis or perforation.
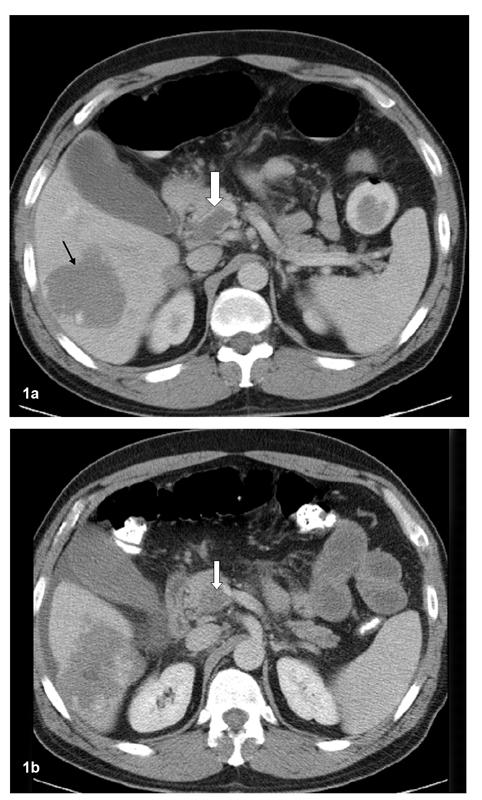
FIG. 1. Filling defect (A: large white arrow) at the confluence of the splenic and superior mesenteric vein (ortal vein). Patient has an incidental finding of hepatic hemangioma. Persistent portal thrombus (B: white arrow) despite overnight treatment with intravenous heparin infusion.
Selective catheterization of the superior mesenteric artery (SMA) and institution of tissue plasminogen activator (t-PA) thrombolysis (10 mg bolus then an infusion of 2 mg/hr) was performed. A CT scan 7 hours later showed a stable thrombus, but angiography showed increased visualization of the SMV. The t-PA infusion was then increased to 4 mg/hr. Angiography 20 hours later showed some thrombus progression within the portal vein but enhanced SMV visualization. The catheter was repositioned in the splenic artery, and the t-PA infusion was continued at 4 mg/hr. Angiography at 48 hours showed marked regression of portal vein (Fig. 2a) and SMV thrombus. The patient's symptoms had almost completely resolved; the t-PA infusion was stopped and IV heparin anticoagulation initiated. He was later discharged on oral systemic anticoagulation, with CT showing resolution of bowel thickening and a partial portal vein thrombus (Fig. 2b). Hematological workup did not reveal any abnormalities.
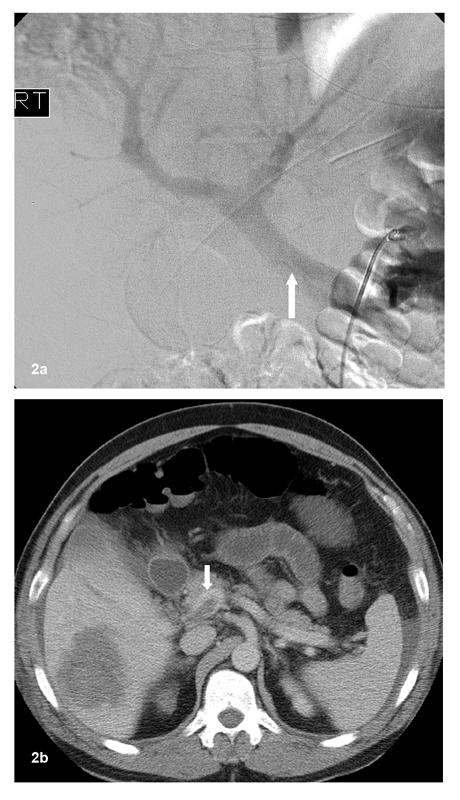
FIG. 2. Venous phase of an arterial injection shows an open portal vein (A). Persistent but nonocclusive thrombus (B: white arrow) in the portal vein.
Discussion
Portal and mesenteric vein thrombosis (MVT) is a rare condition associated with high rates of mortality (up to 50%).2 This is a consequence of 2 main complications: intestinal ischemia and portal hypertension leading to intestinal infarction and shock and gastrointestinal bleeding, respectively. Although the natural history of this condition remains unknown, it is associated with various conditions, such as deficiencies of antithrombin III, protein C and S, factor V Leiden, abdominal infection, trauma, abdominal surgery and myeloproliferative disorders. Clinical presentations of acute MVT can vary from asymptomatic to severe abdominal pain and peritonitis.
In cases where acute MVT has not progressed to infarction and perforation, systemic anticoagulation has been the standard treatment used to halt the progression of thrombus and decrease complications and recurrence. Acute MVT is still associated with 25% of extrahepatic portal vein hypertension and 18% transmural bowel infarction despite systemic anticoagulation.3
More recently, endovascular selective catheterization thrombolytic therapy has been performed with increasing success. Endovascular thrombolytic therapy can be administered directly via percutaneous transhepatic or transjugular-transhepatic routes or indirectly (i.e., intra-arterially). The direct approach offers the advantage of using techniques such as balloon thrombectomy/dilatation and stent placement4 and likely higher thrombolytic activity. It is technically more difficult and associated with an increased risk of bleeding. Indirect thrombolytic therapy is technically simpler, associated with less bleeding risk, and can enable dissolution of clot within capillaries and venules. The SMA has been the artery of choice. A combined direct and indirect approach has been used, as well as intraoperative portal vein and SMV thrombolysis.5 No prospective large series are available, and case reports are limited, but many have reported success with thrombolytic agents such as urokinase streptokinase and t-PA.
With our patient, the diagnosis was made early on presentation, yet the initial clinical and radiological findings were impressive and suggestive of advanced disease. Systemic anticoagulation was ineffective. Indirect endovascular thrombolytic therapy (t-PA) was successfully administered, with complete resolution of symptoms and significant, albeit incomplete, resolution of thrombus. Selective endovascular thrombolytic therapy for acute MVT is a promising approach. However, further study is needed to better determine efficacy and compare the different approaches and various thrombolytic agents.
Competing interests: None declared.
Correspondence to: Dr. Najib Safieddine, #1106–120 St. Patrick St., Toronto ON M5T 2X7; safieddinen@yahoo.ca
References
- 1.Rhee RY, Gloviczki P, Mendonca CT, et al. Mesenteric venous thrombosis: still a lethal disease in the 1990s. J Vasc Surg 1994;20:688-97. [DOI] [PubMed]
- 2.Rhee RY, Gloviczki P. Mesenteric venous thrombosis. Surg Clin North Am 1997;77:327-38. [DOI] [PubMed]
- 3.Brunaud L, Collinet-Adler S, Marchal F, et al. Acute mesenteric venous thrombosis: case for nonoperative management. J Vasc Surg 2001;34:673-9. [DOI] [PubMed]
- 4.Sze DY, O'Sullivan GJ, Johnson DL, et al. Mesenteric and portal venous thrombosis treated by transjugular mechanical thrombolysis. AJR Am J Roentgenol 2000;175:732-4. [DOI] [PubMed]
- 5.Rosen MP, Sheiman R. Transhepatic mechanical thrombectomy followed by infusion of tPA into the superior mesenteric artery to treat acute mesenteric vein thrombosis. J Vasc Interv Radiol 2000;11:195-8. [DOI] [PubMed]


