Abstract
Objective
Centralization of vascular surgery services has resulted in patients being transferred longer distances for treatment of life-threatening conditions. The purpose of this study was to determine whether patient transfer adversely affects the survival of people with a ruptured abdominal aortic aneurysm (RAAA).
Methods
We performed a retrospective review of all patients undergoing attempted repair of an RAAA at our centre, over a recent 3.5-year period (August 2000–December 2003). Patients were divided into those presenting directly to our centre and those transferred from another hospital. The main outcome variable was in-hospital or 30-day mortality, with secondary variables including time to surgical treatment, mortality in the first 24 hours and length of hospitalization.
Results
Eighty-one patients (73% men) underwent attempted open repair of an RAAA at our centre during this period. Twenty-four patients (29.6%) presented directly to our hospital, while 57 (70.4%) were transferred from another institution. The overall mortality rate was 53%. Although transferred patients took twice as long as direct patients to get to the operating room (6.3 v. 3.2 h, p = 0.03), there was no difference in mortality between the 2 groups (50% v. 54%, p = ns). However, deaths of transferred patients were more likely to occur in the first 24 postoperative hours, compared with direct patients (40% v. 33%, p < 0.05). Neither mean intensive care unit stay (5.8 and 8.1 d) nor total hospitalization (20.9 and 18.8 d) differed between the 2 groups.
Conclusions
Although the transfer of patients with RAAA results in a treatment delay, it does not adversely affect the already high mortality rates associated with this condition. These results may be attributed to a preselection of patients who are able to tolerate such a delay.
Abstract
Objectif
À cause de la centralisation des services de chirurgie vasculaire, les patients sont transférés sur de plus longues distances pour le traitement de problèmes qui mettent leur vie en danger. Cette étude visait à déterminer si le transfert des patients a un effet indésirable sur la survie des personnes victimes d'une rupture de l'anévrisme de l'aorte abdominale (RAAA).
Méthodes
Nous avons procédé à une étude rétrospective de tous les patients que l'on a soumis à une tentative de réparation d'une RAAA à notre centre, sur une période récente de 3,5 ans (août 2000-décembre 2003). On a réparti les patients en deux groupes, soit ceux qui se sont présentés directement à notre centre et ceux qui ont été transférés d'un autre hôpital. La principale variable des résultats a été la mortalité à l'hôpital ou dans les 30 jours et les variables secondaires ont inclus le temps écoulé avant le traitement chirurgical, la mortalité au cours de la première période de 24 heures et la durée de l'hospitalisation.
Résultats
Quatre-vingt-un patients (73 % d'hommes) ont subi une tentative de réparation sanglante d'une RAAA à notre centre au cours de cette période. Vingt-quatre des patients (29,6 %) se sont présentés directement à l'hôpital tandis que 57 (70,4 %) ont été transférés d'un autre établissement. Le taux de mortalité global s'est établi à 53 %. Même s'il a fallu aux patients transférés deux fois plus de temps qu'aux patients qui se sont présentés directement pour parvenir à la salle d'opération (6,3 c. 3,2 h, p = 0,03), il n'y a eu aucune différence au niveau du taux de mortalité entre les deux groupes (50 % c. 54 %, p = ns). Les patients transférés étaient toutefois plus susceptibles que les patients qui se sont présentés directement de mourir dans les 24 heures suivant l'intervention (40 % c. 33 %, p < 0,05). Il n'y a pas eu de différence entre les deux groupes quant à la durée moyenne du séjour aux soins intensifs (5,8 et 8,1 j) et à la durée totale de l'hospitalisation (20,9 et 18,8 j).
Conclusions
Même si le transfert des patients victimes d'une RAAA retarde le traitement, le retard n'a pas d'effets indésirables sur les taux de mortalité déjà élevés associés à ce problème. On peut attribuer ces résultats à une présélection de patients qui peuvent tolérer un tel retard.
Rupture of an abdominal aortic aneurysm (RAAA) is often a lethal condition, with an estimated overall mortality rate of 80%–90%.1 Despite advances in operative and perioperative care, the mortality rate of those who survive long enough to undergo an attempt at open repair is close to 50% and has not improved over the last decade.2–4 The next major operative advance is the application of the endovascular technique for the treatment of RAAA. Although large series are yet to be published, several single-centre experiences have reported a reduction in early mortality after endovascular repair of an RAAA, compared with standard open repair.5
Another possible approach to improve survival rates after a ruptured aneurysm is to expedite appropriate diagnosis and treatment. In our own region of southwestern Ontario, where we serve as a regional referral centre for a population of 1.5 million, we've observed an increasing centralization of specialized vascular surgery services during the last 5 years.6 In many reports, regionalization of aneurysm surgery has proven advantageous because decreased mortality rates have been attributed to greater hospital and surgeon case volumes.7,8 However, in a large and relatively sparsely populated country, such as Canada, regionalization often requires patient transfer. Transfer can result in a deadly delay in treatment in life-threatening situations where time is of the essence. This is often the case with ruptured aneurysms. The purpose of the present study was to review our recent experience with RAAAs and to determine whether transferred patients, with their inevitable delay in treatment, were at a survival disadvantage, compared with patients who arrived directly at our centre.
Methods
We reviewed the vascular surgery database at our university-affiliated medical centre to identify patients who underwent attempted open repair of an RAAA during August 2000–December 2003. We included all patients who were confirmed to have an acute hemorrhage from their infrarenal aneurysm, as determined by preoperative imaging and/or intraoperative findings. We excluded from the analysis those who died en route to our hospital's operating room. All patients in the present series arrived in the operating room and underwent an attempt at repair. The primary outcome variable was death during hospitalization or within 30 days of operation. Other outcomes included length of intensive care unit (ICU) stay and total hospitalization. We retrospectively reviewed patients' hospital charts and recorded various clinical factors apparent on presentation. This allowed us to use the Physiologic and Operative Severity Score for enUmeration of Mortality and Morbidity (POSSUM) scoring system.9 We applied the system to patients' clinical features on presentation to our centre and obtained a standardized assessment of patient comorbidities and hemodynamic stability. We divided patients into 2 groups: those who presented directly to our hospital and those who were transferred from another institution.
Proportions were compared with the chi-square test, and means were compared with the Student's t test, with a level of statistical significance of p < 0.05.
Results
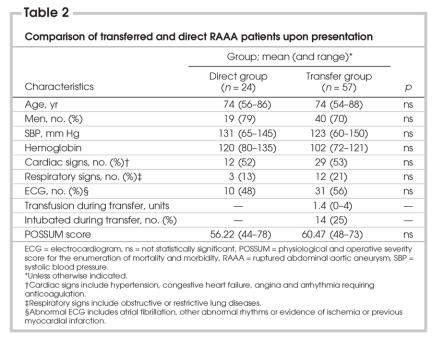
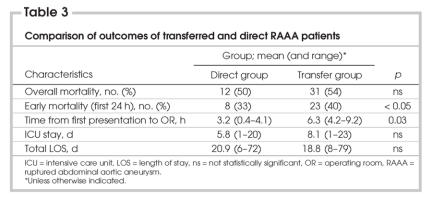
During this 3.5-year period, 81 patients underwent attempted open repair of an RAAA at our medical centre by 1 of 4 vascular surgeons. This group of patients was predominantly male (73%), with a mean age of 74 years and an overall mortality rate of 53%. Of these 81 patients, 57 (70.4%) were originally assessed at 1 of 16 referring hospitals and subsequently transferred to our centre. The remaining 24 (29.6%) patients arrived directly at our hospital. The POSSUM scoring system, whose variables are listed in Table 1, was used to compare these groups with respect to preexisting comorbidities and degree of hemodynamic stability on arrival at our centre. These results are summarized in Table 2, revealing no statistically significant difference between POSSUM-based preoperative scores. Additionally, one-quarter of the transferred patients were intubated on arrival and had received a mean of 1.4 units of red blood cell transfusion. Ventilatory status upon arrival and number of transfused units did not impact survival in the transferred patients.
Table 1
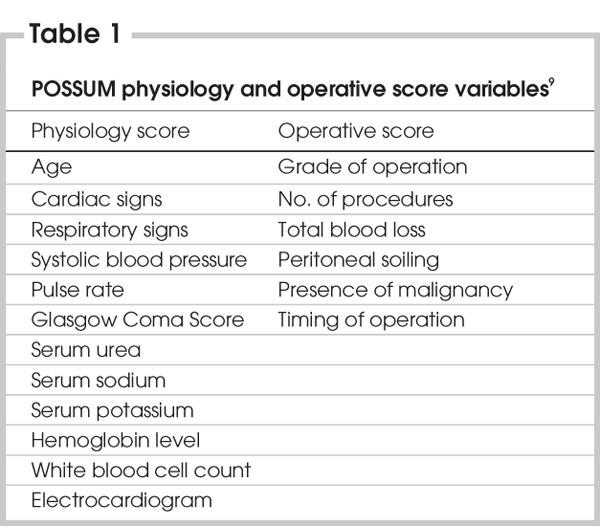
Table 2
It took twice as long for transferred patients to reach the operating room at our centre after presenting to their initial hospital than it did for those presenting directly to our hospital (6.3 v. 3.2 h, p = 0.03). Despite this time delay to treatment, overall mortality did not differ between the 2 groups (50% v. 54%), although deaths of transferred patients were more likely to occur in the first 24 postoperative hours, compared with direct patients (40% v. 33%, p < 0.05). Neither length of ICU stay (8.1 and 5.8 d) nor entire hospitalization (18.8 and 20.9 d) differed between transferred and direct patients (Table 3).
Table 3
Discussion
The overall mortality rate of 53% observed in this patient cohort is similar to those reported previously. A study from our centre reported a 41% early mortality rate over an earlier 2.5-year period,3 whereas a prospective national study of ruptured aneurysms in Canada has reported a 51.4% rate of early mortality, with such presenting factors as hypotension and elevated creatinine proving to be independent predictors.2 In this study, the early mortality rate did not differ when we compared transferred patients with patients who arrived directly to our hospital.
Important variables to consider when comparing mortality in these patient groups are preoperative stability and comorbidities; several techniques allow for this. The POSSUM scoring system requires 12 routine preoperative data points and 6 intraoperative findings (Table 1). These results are then used in previously derived logistic regression equations to provide estimates of the likelihood of morbidity and mortality. Several studies have confirmed the validity of various POSSUM models in predicting mortality after RAAA.9 Additionally, we used the POSSUM system because it has been validated in our RAAA population, where observed and predicted early mortality rates were similar (45.6% and 49.6%, respectively).4 In the present study, this scoring system was used with data available on presentation to our centre and, despite different time intervals between initial presentation and arrival in London, the POSSUM scores were similar. This indicates a relative equivalence of instability and comorbidities between transferred and direct patients at that time.
Transferred patients took twice as long to reach the operating room than direct patients, a consequence of the up to 300 km they were required to travel for treatment between hospitals. Although this time delay might be of concern, by only reviewing the patients who survived to reach the operating room, we preselected patients who were adequately stable to tolerate such a delay. In a time-to-death natural history study, the Leicester group reviewed 56 patients with RAAA who did not undergo operative repair.10 The median time interval between admission to hospital and death was 10 hours 45 minutes, with 12.5% of patients dying in the first 2 hours after admission. This experience would support our results, indicating that the delay in treatment in patient transfer does not negatively impact survival, assuming prompt presentation to the initial hospital. Unfortunately, these data regarding the duration of symptoms is unavailable in the present study; however, the median interval between onset of symptoms and hospital admission in the Leicester study10 was 2 hours 30 minutes.
Although mortality rates between the 2 groups were similar, transferred patients were more likely to die within the initial 24 postoperative hours than were direct patients. This is in contrast to previously reported results,11 but few studies have reviewed this phenomenon. A possible explanation is that, although the time delay to treatment did not negatively impact on survival, it did result in transferred patients being subjected to the physiological stress of an RAAA for a longer period of time. This might have resulted in earlier mortality in patients who were not to survive.
Although a delay to treatment could be a disadvantage, there are benefits to a policy of regionalization of RAAA surgery. Our group has observed an increased trend toward centralization of elective aneurysm surgery with the adoption of our endovascular program, which has resulted in the doubling of our nonurgent aneurysm case volumes over a recent 5-year period.6 A relation between greater hospital volumes for elective aneurysms and lower mortality has been reported.12 Such an increase in nonurgent aortic aneurysm experience has also resulted in improved outcomes (i.e., patient survival) in RAAAs.7,8,12–14 volume-outcome relations have also been reported at the individual surgeon level, with increasing experience with ruptured aneurysms resulting in improved patient survival.3 Over the 3.5 years of the present study, the 57 transferred patients originally sought treatment at 1 of 16 hospitals (1.02 cases/hospital/yr). Even if these hospitals had the appropriate physicians and resources, it is unrealistic to expect such a low patient exposure to result in survival outcomes comparable with larger volume centres.
Our present study has some limitations. Although mortality rates of those RAAA patients presenting to hospital have consistently been reported to be around 50%15; overall mortality, including deaths occurring outside of hospital, is estimated to be 80%–90%.1 The results of this study are consistent with previous reports; however, we did not take into account patients who did not survive to reach our hospital to undergo an attempt at repair. To ensure safe transportation of an RAAA patient, a controlled hypotension approach is advocated. Patients who are salvageable have a contained retroperitoneal hematoma whose expansion, or rupture, is more likely with periods of hypertension. Consequently, a systolic blood pressure, usually between 70 mm Hg and 100 mm Hg, that maintains cognition and urine output is adequate and an appropriate target during transport. Our impression is that there were few patients during the study period who presented to their initial hospital and then died before arriving at our centre. However, this information is not reported or available.
Natural history studies, although rare, are helpful in determining the proportion of patients who may be harmed by a policy of centralization of RAAA therapy. In the Leicester study, the median time to death from onset of symptoms was 16 hours 38 minutes, with only 12.5% of deaths occurring within 2 hours of hospital admission.10 These results, as well as those of the present study, endorse a policy of centralization of RAAA therapy, because most patients who survive to present to their initial hospital are suitably stable to survive the treatment delay necessary for transportation to a centre where definitive care is available.
Centralization of RAAA therapy in high-volume centres with appropriately trained personnel, as well as advances in anesthetic and postoperative intensive care, have maximized survival after standard open repair. Despite these advances, mortality remains close to 50%.15 The next major advance that may improve survival is the endovascular repair of the ruptured aneurysm. Early single-centre experiences have reported impressive improvements in short-term survival, but it remains unclear whether this is due to the less invasive nature of this technique or a preselection of more stable patients who can tolerate the further delay that is often necessary for the endovascular approach.5 Currently, endovascular repair is an attractive alternative in RAAA patients with suitable anatomy at centres with significant elective endovascular experience and a readily available inventory of devices.
Conclusions
Mortality after RAAA remains distressingly high but has been somewhat lessened by the centralization of care at high-volume centres. Unfortunately, such a policy results in a further delay in treatment of some patients. The present study reveals that the penalty of transfer is a doubling of the time interval between initial patient presentation and arrival in the operating room. This, however, did not result in any disadvantage with respect to survival when the group was compared with patients who arrive directly. Our results endorse and support the current policy regarding the transfer of patients with ruptured aneurysms to high-volume specialty centres.
Presented at the 27th Annual Meeting of the Canadian Society for Vascular Surgery September 9th-10th, 2005, Toronto, Ont.
Accepted for publication Sept. 1, 2005
Competing interests: None declared.
Correspondence to: Dr. Thomas L. Forbes, Division of Vascular Surgery, London HSC, University of Western Ontario, 800 Commissioners Rd. E, E2-119, London ON N6A 5W9; fax 519 667-6549; Tom.Forbes@lhsc.on.ca
References
- 1.Krupski WC, Rutherford RB. Update on open repair of abdominal aortic aneurysms: The challenges for endovascular repair. J Am Coll Surg 2004;199:946-61. [DOI] [PubMed]
- 2.Johnston KW. Ruptured abdominal aortic aneurysm: six-year follow-up results of a multicenter prospective study. Canadian Society for Vascular Surgery Aneurysm Study Group. J Vasc Surg 1994;19:888-900. [DOI] [PubMed]
- 3.Forbes TL, DeRose G, Harris KA. A. CUSUM analysis of ruptured abdominal aortic aneurysm repair. Ann Vasc Surg 2002;16:527-33. [DOI] [PubMed]
- 4.Harris JR, Forbes TL, Steiner SH, et al. Risk adjusted analysis of early mortality following ruptured abdominal aortic aneurysm repair. J Vasc Surg 2005;42(3):387-91. [DOI] [PubMed]
- 5.Lee WA, Hirneise CM, Tayyarah M, et al. Impact of endovascular repair on early outcomes of ruptured abdominal aortic aneurysms. J Vasc Surg 2004;40:211-5. [DOI] [PubMed]
- 6.Forbes TL, Lawlor DK, DeRose G, et al. Examination of the trend in Canada towards geographic centralization of aneurysm surgery during the endovascular era. Ann Vasc Surg 2006;20(1):63-8. [DOI] [PubMed]
- 7.Dimick JB, Stanley JC, Axelrod DA, et al. Variation in death rate after abdominal aortic aneurysmectomy in the United States: impact of hospital volume, gender, and age. Ann Surg 2002;235:579-85. [DOI] [PMC free article] [PubMed]
- 8.Dueck AD, Kucey DS, Johnston KW, et al. Long-term survival and temporal trends in patient and surgeon factors after elective and ruptured abdominal aortic aneurysm surgery. J Vasc Surg 2004;39:1261-7. [DOI] [PubMed]
- 9.Prytherch DR, Ridler BM, Beard JD, et al.; Audit and Research Committee of the Vascular Surgical Society of Great Britain and Ireland. A model for national outcome audit in vascular surgery. Eur J Vasc Endovasc Surg 2001;21:477-83. [DOI] [PubMed]
- 10.Lloyd GM, Bown MJ, Norwood MGA, et al. Feasibility of preoperative computer tomography in patients with ruptured abdominal aortic aneurysm: A time-to-death study in patients without operation. J Vasc Surg 2004;39:788-91. [DOI] [PubMed]
- 11.Vogel TR, Nackman GB, Brevetti LS, et al. Resource utilization and outcomes: Effect of transfer on patients with ruptured abdominal aortic aneurysms. Ann Vasc Surg 2005;19:149-53. [DOI] [PubMed]
- 12.Shackley P, Slack R, Booth A, et al. Is there a positive volume-outcome relationship in peripheral vascular surgery? Eur J Vasc Endovasc Surg 2000;20:326-35. [DOI] [PubMed]
- 13.Rutledge R, Oller DW, Meyer A, et al. A statewide, population-based, time-series analysis of the outcome of ruptured abdominal aortic aneurysm. Ann Surg 1996;223:492-505. [DOI] [PMC free article] [PubMed]
- 14.Dardik A, Burleyson GP, Bowman H, et al. Surgical repair of ruptured abdominal aortic aneurysms in the state of Maryland: Factors influencing outcome among 527 recent cases. J Vasc Surg 1998;28:413-21. [DOI] [PubMed]
- 15.Bown MJ, Sutton AJ, Bell PRF, et al. A meta-analysis of 50 years of ruptured aortic aneurysm repair. Br J Surg 2002;89:714-30. [DOI] [PubMed]