Abstract
Objective
The purpose of this prospective study was to determine the positive predictive value (PPV) of the point of maximal posterior joint line tenderness (JLT), as a clinical sign, to diagnose underlying meniscal tears.
Methods
We conducted a prospective study of patients requiring arthroscopic surgery, who consecutively presented to the University of Calgary's Sport Medicine Centre. The femurotibial joint line was palpated for the point of maximal tenderness. We recorded the data on the arthroscopy report. A second examiner (orthopedic sport medicine surgical fellow or sport medicine physician) performed the same protocol. An arthroscopist documented the site of pathology as detected by arthroscopy.
Results
We found a PPV of 60.0% and a negative predictive value of 62.5%, suggesting that maximal posterior JLT may be predictive of meniscal pathology. The sensitivity and specificity were 84.6% and 31.2%, respectively (p = 0.155), with Fisher's exact test. The kappa score assessed interobserver reliability and was good at 0.48. Patients with maximal posterior JLT but no meniscal pathology did have other confounding pathology and patients with no maximal posterior JLT who had meniscal pathology usually had confounding knee pathology.
Conclusions
We found a PPV of 60.0% of maximal posterior JLT and meniscal pathology located at the same anatomical site on arthroscopic examination.
Abstract
Objectif
Cette étude prospective visait à déterminer la valeur prédictive positive (VPP) du point de sensibilité maximale de la ligne articulaire (SLA) postérieure comme signe clinique pour diagnostiquer des déchirures sous-jacentes du ménisque.
Méthodes
Nous avons réalisé une étude prospective portant sur des patients qui avaient besoin d'une chirurgie arthroscopique et se sont présentés consécutivement au Centre de médecine sportive de l'Université de Calgary. On a palpé la ligne articulaire fémorotibiale pour déterminer le point de sensibilité maximale. Nous avons consigné les données sur le rapport d'arthroscopie. Un deuxième examinateur (fellow en chirurgie sportive orthopédique ou médecin spécialisé en médecine sportive) a exécuté le même protocole. Un spécialiste en arthroscopie a documenté le site de la pathologie détecté par l'arthroscopie.
Résultats
Nous avons constaté une VPP de 60,0 % et une valeur prédictive négative de 62,5 %, ce qui indique que la sensibilité maximale de la ligne articulaire postérieure peut être prédictive d'une pathologie du ménisque. La sensibilité et la spécificité se sont établies à 84,6 % et 31,2 %, respectivement (p = 0,155), selon la méthode exacte de Fisher. Le score kappa a permis d'évaluer la fiabilité entre les observateurs et il était bon à 0,48. Les patients ayant une sensibilité maximale de la ligne articulaire postérieure mais sans pathologie du ménisque avaient d'autres problèmes pathologiques qui étaient source de confusion, et les patients qui n'avaient pas de sensibilité maximale de la ligne articulaire postérieure et avaient une pathologie du ménisque présentaient habituellement une pathologie du genou qui était source de confusion.
Conclusions
Nous avons constaté que la sensibilité maximale de la ligne articulaire postérieure présentait une VPP de 60,0 % et l'examen arthroscopique a révélé une pathologie du ménisque au même site anatomique.
Meniscal lesions are common and can be difficult to diagnose. Historically, a combination of physical tests have been used to determine the presence of a meniscal tear.1–5 Controversy continues regarding whether there is a single clinical diagnostic test that is most sensitive and specific to correctly diagnosing a meniscal tear. This controversy likely began with McMurray in 1942, when he suggested that diagnosing meniscal tears must involve a combination of both a case history and a particular physical examination, which became known as “the McMurray test.”6 This test has recently been shown to be specific for meniscal tears but not very sensitive,7 making it of dubious value in screening for surgical pathology.
Palpating the knee joint has been suggested as another means to identify meniscal pathology.6,8–11 McMurray6 also suggested that tenderness over the meniscus may indicate the possibility of it being torn. Abdon and colleagues8 tested this idea and reported a 61% clinical accuracy of diagnosing meniscal injuries using physical indications, including joint-line tenderness (JLT). Abdon further reported that the presence of posterior/medial JLT separated knees with an isolated meniscal tear from those with associated intra-articular changes involving ligament and articular cartilage changes. Fowler and Lubliner4 reported a positive correlation between JLT and meniscal lesions, with a high sensitivity of 85.5% but a low specificity of only 29.4%. This result suggested that patients with meniscal tears would likely have JLT; however, patients with JLT would not exclusively have meniscal tears. Shelbourne agreed with this observation in patients with acute anterior cruciate ligament ruptures, where he found medial JLT was only 34.5% specific for medial meniscal tears, whereas lateral JLT was 49.1% specific for lateral meniscal tears.12 In that series, JLT was also only 44.9% sensitive (medial) and 37.6% sensitive (lateral). Similarly, Akseki and colleagues2 suggested that the accuracy of JLT predicting meniscal pathology decreases in the presence of an ACL tear. Others3,13,14 have also concluded that JLT, despite being sensitive, was not specific for a torn meniscus.
Unfortunately, all of the above-noted studies used a composite of clinical tests in their designs to determine the presence of meniscal tears. This prevents the isolation of any 1 test for its specificity and sensitivity without some bias. Further, some of these studies did not restrict their investigation of each symptom to the area of the meniscus known to have the highest incidence of injury — the posterior horns.15 This is particularly true for JLT, where palpation of the posterior joint lines, specifically, might be expected to give the highest yield of true results, both positive and negative.
This study investigated the effectiveness of one isolated clinical test (JLT), without the benefit of a case history or a complete physical examination. We were specifically interested in palpating the joint lines to test whether the point of maximal tenderness would identify the area of meniscal pathology. Our study focused on JLT in predicting meniscal pathology and comparing it with the gold standard of arthroscopy in a prospective manner. We also wanted to assess inter-observer reliability of JLT to define how these findings could be applied to other observers.
The purpose of this study was to determine the positive predictive value (PPV) of posterior JLT in diagnosing posterior meniscal tears. We hypothesized that, if maximal tenderness was located along either posterior joint line, then meniscal pathology would be found on arthroscopic examination at that specific site in more than 80% of the patients examined.
Methods
We studied 71 consecutive patients who presented to the orthopedic surgeons of the University of Calgary's Sport Medicine Centre. We included all patients who were booked for arthroscopic surgery by the surgeons, on the basis of the case history, physical examination and special tests. If surgery was indicated, by whatever criteria that surgeon used, the patient was booked for surgery. We asked the patients to participate in the study and obtained informed consent at that time. The principle investigator was not made aware of the reasons for the arthroscopy, and no further selection took place.
On the day of surgery, the principle investigator, an orthopedic surgical resident, previously educated by an experienced orthopedic surgeon on systematic palpation of the knee joint, independently and blindly examined each patient. One patient was excluded, being unable to endure a preoperative palpation examination before surgery due to excessive pain with palpation.
In the preoperative holding area, before any sedation and without taking a history, the tibiofemoral joint line was systematically palpated to record the point of maximal tenderness. The joint line was palpated by passively flexing the knee joint to roughly 90°. The hollows that lie over the joint line at the sides of the patellar ligament were then identified. Proper hand positioning over the joint line was confirmed. The soft hollow between the prominence of the femur above and the tibia below was then identified. The joint line of the knee was palpated, starting from the medial border of the patellar ligament and palpating toward the posterior aspect of the knee, while maintaining the position along the medial joint line. The same technique was performed on the lateral aspect of the knee. Beginning on the lateral border of the patellar ligament, the lateral joint line was palpated in a similar fashion in a posterior direction along the joint line. Caution was exercised to palpate the medial and lateral joint lines separately. The borders of the tibial plateau and femoral condyles were then palpated to ensure the presence of isolated posterior JLT. The borders of the patella were not palpated.
By definition, the point of maximal tenderness was the point that exceeded normal discomfort and that was more tender than the nonsurgical leg at the same anatomic location. This point was documented with an “X” on a standard knee arthroscopy report form, which represented a schematic diagram of the knee outlining the patella, the femoral condyles and the tibia (Fig. 1).

FIG. 1. Testing joint-line tenderness.
To assess for interobserver reliability on each patient, 1 of 2 experienced but similarly blinded examiners (either an orthopedic sport medicine fellow or a sport medicine physician) performed the same palpation manoeuvre, also without taking the case history. They also recorded the point of maximal tenderness on a similar but separate knee arthroscopy report form. Examiners were always blind to the patient's presenting history and clinical examination before determining the point of maximal tenderness on the surgical knee. In addition, both examiners performed the knee examination independent of each other to eliminate information bias.
Each patient was then arthroscoped. One of 3 experienced surgeons documented his findings on a standard arthroscopy report form similar to that used for the physical exam. They specifically documented meniscal tears, and their exact anatomic locations were identified. We applied the same criteria for defining meniscal tears used by Shelbourne and others.12 That is, positive meniscal pathology consisted of any meniscal tear or detachment of meniscus from its supporting structures. Normal (intact) menisci were also noted as appropriate. Postoperatively, the principle investigator divided the knee arthroscopy report form into quadrants and labelled it by numbers, according to specific regions of the knee.
The physical exam data of each examiner were recorded on individual data sheets, ensuring that the appropriate numbered region on the knee diagram corresponded to the point of tenderness indicated by the patient. Similarly, each arthroscopic surgeon recorded the specific knee pathology findings on a separate but similar surgical diagram.
A statistical analysis was performed to compare JLT data with the arthroscopic data. We quantified the PPV, the negative predictive value (NPV), the sensitivity and the specificity of JLT in diagnosing meniscal tears. PPV was defined as isolated posterior JLT on clinical examination that correlated with any meniscal tear at that same anatomic location on arthroscopic examination. A true positive test occurred when the point of posterior JLT corresponded to the site of a meniscal tear. A false positive test occurred when maximal JLT was located in an area where no meniscal tear was present.
Sensitivity was the ability for JLT to correctly identify those individuals without posterior JLT and who did not have a meniscal tear. Specificity was the ability of JLT to correctly identify individuals without posterior JLT who did not have a meniscal tear. We used Fisher's exact test and the chi-square test to determine whether JLT would have a PPV of 80% or higher. A kappa score was used to assess the interobserver reliability of JLT.
Results
Of the 71 subjects, 45 were men and 26 were women, aged between 19 and 66 years. Table 1 lists the location of meniscal tears and confounding pathology identified during arthroscopic evaluation.
Table 1
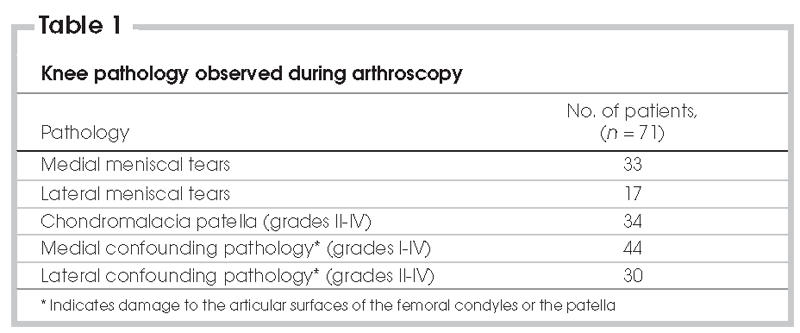
The PPV of JLT for diagnosing meniscal tears was 60.0%, with 33 of 55 patients with positive JLT having a meniscal tear. The NPV was 62.5%, where 10 of 16 subjects with no JLT did not have a meniscal tear.
The overall sensitivity of JLT in detecting meniscal tears was 84.6%, but the specificity was only 31.2%. The false positive rate was 68.8%, and the false negative rate was 15.4%. In 75.8% of patients, all 3 examiners found the same point of maximal tenderness. This corresponded with a kappa score of 0.48, suggesting the interobserver reliability was good.
In a separate set of calculations specifically looking at the confounding pathology of each patient, regarding a PPV of confounding pathology with JLT, there was insufficient power to draw any significant conclusions.
Discussion
This study suggests that, in a population of knee patients preselected for arthroscopic surgery, posterior JLT would be predictive of meniscal tears 60% of the time. That is, 3 of 5 patients with tears and a similar proportion of patients who did not have tears could be correctly diagnosed simply by palpating the tibiofemoral joint line, with no history taken. Unfortunately, these results did not meet our rigorous standard of 80% predictive value, so our initial hypothesis was disproved. JLT was predictive 60% of the time. In addition, a recent study16 also reported high accuracy rates of JLT in the diagnosis of meniscal tears, with lower accuracy reported with confounding pathology.
There was low specificity because of the high false positive rate. The patients with false positive tests had points of maximal posterior JLT but did not actually have meniscal tears. This may be partly explained by the presence of confounding pathology. Specifically, damage to the patella and the surfaces of articular cartilage appeared to induce a synovitis that might have been the reason for tenderness in patients with JLT but no meniscal tears. In this study, we did not account for this. Only the tibiofemoral joint line, and not the patella-femoral joint line, was palpated. We retrospectively speculated that, had we palpated the borders of the patella, some patients would have identified patella-femoral tenderness as their point of maximal tenderness, eliminating at least some of the false positives.
To assess this concept, subjects who had confounding patellar pathology were retrospectively eliminated from the data, and the remaining group was reassessed statistically. The PPV of JLT for meniscal tears increased to 80%, and the NPV was 71.4%. The sensitivity was 89.2%, and specificity was 55.6%, with good interobserver reliability. Thirty-three of 41 patients with positive posterior JLT actually had a meniscal tear in the same anatomic site. Ten of 14 patients with no posterior JLT did not have a tear (p < 0.001). The kappa score assessing interobserver reliability of this negative predictive value was also good, at 0.42 (73.5%). When confounding patellar pathology was removed, only 4 of 37 (10.8%) subjects with no JLT actually had a meniscal tear. This was significant at p < 0.001. Fowler and Lubliner4 also found the specificity of JLT to be low, which could be a result of confounding patellar pathology. This suggests that, to be complete, it is important to palpate the patellofemoral joint lines and the tibiofemoral joint lines. This needs to be further studied.
In addition, among all the false negatives and true positives, there were no isolated meniscal tears. This patient population demonstrated meniscal tears in the presence of either condral damage on the articular surfaces of the patella, femoral condyles or tibial plateau, or an anterior cruciate ligament deficiency.
It is possible that examiners might not have accurately and specifically palpated the joint line, which might explain the false negatives (patients who had no JLT but who presented with tears, 15.4%). Alternatively, the pressure of palpation might not have been great enough to elicit a painful response. These findings suggest that, if clinicians were able to accurately palpate the tibiofemoral joint line and identify the point of maximal tenderness in the knee at the posterior tibiofemoral joint line, then the chances of diagnosing a meniscal tear with JLT alone should be at least 60%. If patellar pathology could be eliminated in some way, this yield would likely increase. We speculate that this may be possible by simply performing peripatellar palpation as part of the examination regime; however, that remains to be proven.
Finally, when considering the optimal physical examination to determine the presence or absence of meniscal tears in a population aged 19 to 66 years, it can be difficult to distinguish between degenerative and nondegenerative tears. Both may present with the same clinical signs and symptoms; however, the response to arthroscopic surgical intervention may vary.17 Menetrey and colleagues17 suggest that patients aged over 50 years who present with degenerative tears are not as satisfied after arthroscopic surgery as those aged over 50 years who have nondegenerative tears. Older patients are more likely to have degenerative tears. The question is how to determine weather a tear is degenerative before offering a patient surgery. Although this is not the focus of this paper, several studies investigating the use of clinical examination and MRI in diagnosing meniscal tears have been undertaken.18–22 Some authors have suggested that a good clinical examination is as good as an MRI when determining the presence of meniscal tears and that MRI should only be used in more complicated cases18; such cases, depending on the radiologist, may be difficult to diagnose even with an MRI.22 Otherwise, the procedure is expensive and unnecessary.21
A major limitation to this study is that we did not account for confounding pathology. We speculate that, if peripatellar tenderness had been elicited as the point of maximal tenderness in patients with JLT and confounding pathology, the sensitivity of JLT in detecting true meniscal pathology would have increased. Another limitation includes the lack of a control group. The fact that subjects were already preselected for surgery before entering the study presents a specific subset of patients, which will likely yield a higher sensitivity when determining the association of JLT and meniscal pathology.
This study was conducted to determine whether a single test, without a case history, performed with precision and in a systematic fashion and involving all 3 joint lines, would help to narrow the diagnosis of intra-articular pathology. Our findings suggest the likeliness for the role of such palpation as an important component of the overall examination of the knee.
Accepted for publication Sept. 13, 2006
Competing interests: None declared.
Correspondence to: Dr. Veronica Wadey, Department of Surgery, Division of Orthopaedic Surgery, Holland Orthopaedic and Arthritic Centre, 43 Wellesley St. E., Toronto ON M4Y 1H1; Veronica.Wadey@cirris.ulaval.ca
References
- 1.Akseki D, Pinar H, Karaoglan O. The accuracy of the clinical diagnosis of meniscal tears with or without associated anterior cruciate ligament tears. Acta Orthop Traumatol Turc 2003;37:193-8. [PubMed]
- 2.Akseki D, Ozcan O, Boya H, et al. A new weight-bearing meniscal test and a comparison with McMurray's test and joint line tenderness. Arthroscopy 2004;20:951-8. [DOI] [PubMed]
- 3.Anderson AF, Lipscomb AB. Clinical diagnosis of meniscal tears–description of a new manipulative test. Am J Sports Med 1986;14:291-3. [DOI] [PubMed]
- 4.Fowler PA, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy 1989;5:184-6. [DOI] [PubMed]
- 5.Solomon DH, Simel DL, Bates DW, et al. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA 2001;286:1610-20. [DOI] [PubMed]
- 6.McMurray T. The semilunar cartilages. Br J Surg 1972;29:407-14.
- 7.Evans PJ, Bell GD, Frank C. Prospective evaluation of the McMurray Test. Am J Sports Med 1993;21:604-8. [DOI] [PubMed]
- 8.Abdon P, Lindstrand A, Thorngren K. Statistical evaluation of the diagnostic criteria for meniscal tears. Int Orthop 1990;14:341-5. [DOI] [PubMed]
- 9.Noble J. Clinical features of the degenerate meniscus with the results of meniscectomy. Br J Surg 1975;62:977-81. [DOI] [PubMed]
- 10.Post WR, Fulkerson JP. Anterior knee pain–a symptom not a diagnosis. Bull Rheum Dis 1993;42:5-7. [PubMed]
- 11.Lantz B, Singer K. Meniscal cysts. Clin Sports Med 1990;9:707-23. [PubMed]
- 12.Shelbourne KD, Martini D, McCarroll J, et al. Correlation of joint line tenderness and meniscal lesions in patients with acute anterior cruciate ligament tears. Am J Sports Med 1995;23:166-9. [DOI] [PubMed]
- 13.Hamilton EB. Diseases associated with CPPD deposition disease. Arthritis Rheum 1976;19(Suppl 3):353-7. [DOI] [PubMed]
- 14.Clancy WG, Keene JS, Goletz TH. Symptomatic dislocation of the anterior horn of the medial meniscus. Am J Sports Med 1984;12:57-64. [DOI] [PubMed]
- 15.De Smet AA. Meniscal tears on knee arthrography: patterns of arthrographic abnormalities. Skeletal Radiol 1985;14:280-5. [DOI] [PubMed]
- 16.Eren OT. The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy 2003;19:850-4. [DOI] [PubMed]
- 17.Menetrey J, Siegrist O, Fritschy D. Medial meniscectomy in patients over the age of fifty: a 6-year follow-up study. Swiss Surg 2002;8:113-9. [DOI] [PubMed]
- 18.Kocabey Y, Tetik O, Isbell WM, et al. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy 2004;20:696-700. [DOI] [PubMed]
- 19.Davis KW, Tuite MJ. MR imaging of the postoperative meniscus of the knee. Semin Musculoskelet Radiol 2002;6:35-45. [DOI] [PubMed]
- 20.Trieshmann HW Jr, Mosure JC. The impact of magnetic resonance imaging of the knee on surgical decision making. Arthro-scopy 1996;12:550-5. [DOI] [PubMed]
- 21.Rose NE, Gold SM. A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruiciate ligament tears. Arthroscopy 1996;12:398-405. [DOI] [PubMed]
- 22.De Smet AA, Tuite MJ, Norris MA, et al. MR diagnosis of meniscal tears: analysis of causes of errors. AJR Am J Roentgenol 1994;163:1419-23. [DOI] [PubMed]


