Abstract
Objective
The purpose of this study was to compare the outcomes of adult (aged > 15 yr) blunt trauma patients with an Injury Severity Score (ISS) ≥ 12 who were transported to a single tertiary trauma centre (TTC) by helicopter emergency medical service (HEMS) versus those transported by ground ambulance.
Methods
We retrospectively analyzed all adult (aged > 15 yr) trauma patients between March 27, 1998 and March 28, 2002 with an ISS score ≥ 12, as identified through the provincial trauma registry. We used the Trauma and Injury Severity Score (TRISS) methodology to determine a difference in outcomes between the 2 groups.
Results
We identified 823 patients; of these, we excluded 32 (3.9%) penetrating trauma patients. Of the blunt trauma cases (n = 791) 237 (30%) patients were transported by air and 554 were transported by ground (70%). A total of 770 (97.3%) patients were eligible for TRISS analysis. Using the TRISS methodology, the air group had a Z statistic of 2.77, yielding a W score of 6.40. This compared with the ground transport group, whose Z statistic was –1.97 and W score was –2.39.
Conclusion
The transport of trauma patients with an ISS ≥ 12 by a provincially dedicated rotor wing air medical service was associated with statistically significantly better outcomes than those transported by standard ground ambulance. This is the first large Canadian study to specifically compare the outcome of patients transported by ground with those transported by air.
Abstract
Objectif
Cette étude vise à comparer les résultats chez les patients adultes (> 15 ans) victimes d'un traumatisme contondant, dont l'indice de gravité de la blessure (IGB) ≥ s'établissait à 12 et qui ont été transportés à un même centre de traumatologie tertiaire (CTT) par un service médical d'urgence par hélicoptère (SMUH), par rapport à ceux qui ont été transportés par ambulance au sol.
Méthodes
Nous avons analysé de façon rétrospective le cas de tous les patients adultes (âge > 15) traumatisés entre le 27 mars 1998 et le 28 mars 2002 dont l'IGB ≥ 3 s'établissait à 12, que nous avons identifiés au moyen du registre provincial des traumatismes. Nous avons utilisé la méthodologie de l'Indice de gravité de la blessure et du traumatisme (Trauma and Injury Severity Score [TRISS]) pour cerner les différences entre les deux groupes au niveau des résultats.
Résultats
Nous avons trouvé 823 patients et nous en avons exclu 32 (3,9 %) qui avaient subi un traumatisme pénétrant. Parmi les victimes d'un traumatisme contondant (n = 791), on en a transporté 237 (30 %) par air et 554 au sol (70 %). Au total, 770 (97,3 %) des patients pouvaient être soumis à l'analyse TRISS. Après application de la méthodologie TRISS, le groupe des patients héliportés présentait une statistique Z de 2,77, ce qui donne un score W de 6,40, comparativement au groupe des patients transportés au sol, dont la statistique Z s'est établie à –1,97 et le score W, à –2,39.
Conclusion
On a établi un lien entre le transport par hélicoptère de patients traumatisés ayant un IGB ≥ de 12 effectué par un service médical spécialisé provincial et des résultats statistiquement significatifs meilleurs que chez les patients transportés par ambulance ordinaire au sol. Il s'agit de la première étude canadienne d'envergure visant à comparer spécifiquement l'évolution de l'état de santé des patients transportés par la route à celui des patients transportés par hélicoptère.
Helicopter emergency medical service (HEMS) plays an increasingly important role in the pre-hospital care and transport of trauma patients. In the current climate of cost-constrained delivery of health care in a publicly funded system, there is a need to prove the efficacy and cost-effectiveness of any health care intervention. There have been several studies involving the air medical transport (AMT) of trauma patients; however, despite over 30 years of civilian use, few data compare AMT with other EMS transport modalities. Among the studies evaluating outcomes, most involve large urban trauma systems. Few studies have explored the role of AMT serving more rural areas.1,2–4 Mann and colleagues found an increase in trauma mortality in the years following the loss of an air medical program for rural interhospital transport.1 The only paper to have explored the role of AMT in a Canadian centre was small in size and focused mainly on cost, with minimal outcome data.2 Nicholl and others also explored the performance and cost of an HEMS program in a rural trauma system.4
The purpose of this study was to compare the mortality of blunt trauma patients transported by air or ground in our provincially integrated prehospital trauma system. It is important to evaluate and document the effectiveness of AMT in the Canadian context. The setting of our trauma system is a predominantly rural province with 7 small regional hospitals (district trauma centres) and only 1 adult tertiary trauma centre (TTC). The TTC receives trauma patients from all of the regional centres and from rural scene transports. This study is unique in that it includes the entire provincial EMS system and a central trauma registry, thus allowing for population-based trauma research. The rural geographical makeup of the province, with 1 central TTC, is well constructed to potentially demonstrate the use and effectiveness of a rapid transport rotor wing service.
Methods
The Nova Scotia EMS system is a provincially integrated system with one central communications and dispatch centre for both ground ambulance transport (GAT) and AMT (see www.gov.ns.ehs/homepage/background.htm). Associated with this program is a comprehensive trauma program and registry that records data from every trauma case in the province. Nova Scotia has a single adult TTC located centrally in Halifax. This institution is the only tertiary care neurosurgical and trauma centre in the province. Nova Scotia is a maritime province with a population of 936 960 people (population density 17.2 per km2). It is a fairly large peninsula (area 55 490 km2), extending into the Atlantic Ocean from the Canadian mainland, with large areas of rural geography and wilderness. Our air medical program has 1 dedicated Sikorsky S-76 helicopter and provides continuous (24 h/d, 7 d/wk) coverage, with a critical care paramedic and registered nurse crew as well as on-line medical oversight.
Using the provincial trauma registry, we retrospectively identified all adult (aged > 15 yr) trauma activations between March 27, 1998 and March 28, 2002 with an Injury Severity Score (ISS) ≥ 12. We excluded penetrating trauma cases from our analysis. The trauma and injury severity score (TRISS) was used to determine whether there was a difference in outcomes between patients transported by air and those transported by ground ambulance. TRISS analysis is used to calculate the probability of survival for a given patient on the basis of their ISS and Revised Trauma Score (RTS).5 This is done with a calculated regression model of data from the Major Trauma Outcomes Study (MTOS). From this, we are provided with a Z statistic and a W score.6 The Z statistic compares the sample population mortality to that of an established database of trauma outcomes. A Z statistic < –1.96 indicates that the sample population did worse than predicted. A Z statistic > 1.96 indicates better than expected outcomes. The W score is a measure of the number of unexpected survivals (+) or deaths (–) per 100 patients. Our software package for TRISS allows the insertion of normal physiological values in places where the physiological data may be missing. This increases the number of patients available for inclusion in the analysis.
Results
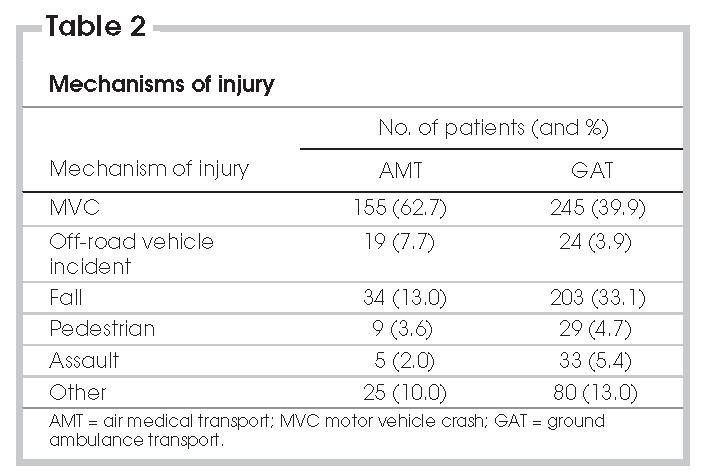
We identified 791 blunt trauma patients with an ISS ≥ 12 from the provincial trauma registry (Table 1). There were 237 (30%) patients transported by air. In this group, there were 43 deaths (18%, 30-day mortality). In the ground transport group (n = 554), the overall 30-day mortality was 18% (n = 103). Median ISSs for the air and ground transport cohorts were 25 and 20, respectively. Mechanisms of injury within the 2 groups are outlined in Table 2.
Table 1
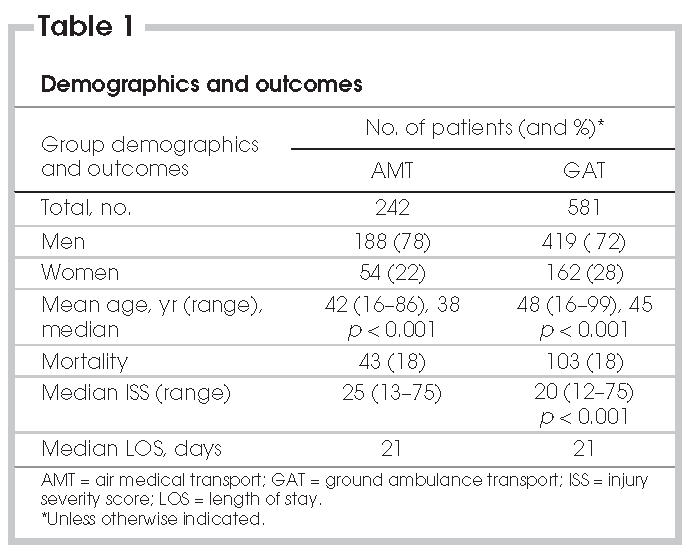
Table 2
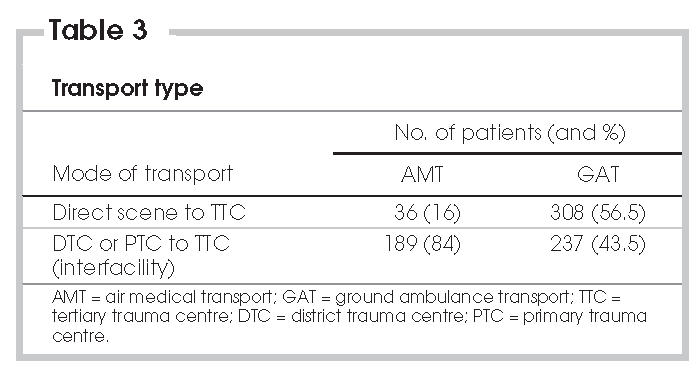
We reviewed transport type data (Table 3). In the air transport cohort, 84% (n = 189) of patients were transported by air from a primary care or regional trauma care centre. The remaining 16% were transported directly from the scene to the TTC. The ground transport group had a very different distribution. Transports from the scene to tertiary care comprised 56% of the patients, with the remainder transported from other regional hospitals.
Table 3
According to the TRISS analysis, 225 (95%) patients in the air transport group and 545 (98%) patients in the ground transport group had sufficient data to undergo the calculations. Results are listed in Table 4. The Z statistic from TRISS for the patients transported by air was 2.77 and for the ground transport group was –1.97. The W scores were 6.40 and –2.39, respectively. On the basis of these results, the air transport group performed better than predicted, with 6.4 more survivors than expected per 100 patients, based on the reference data. In comparison, the ground transport cohort showed outcomes that were worse than expected, based on the Z score of < –1.96. The W score tells us that, in this group, there were 2.4 unexpected nonsurvivors per 100 patients.
Table 4
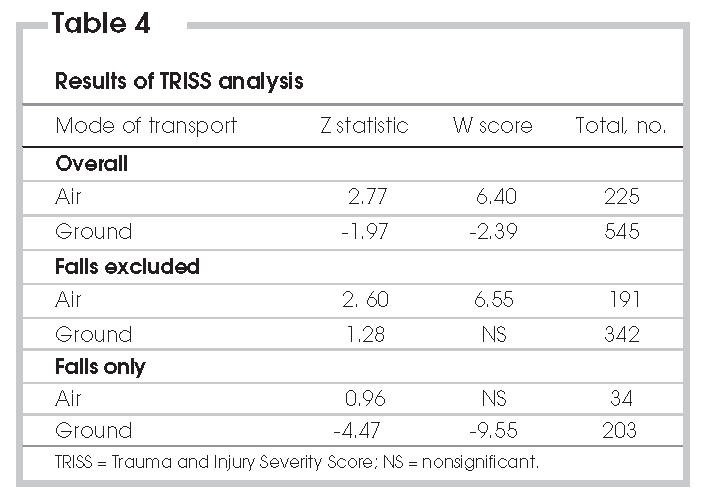
Because falls comprised a large portion of the mechanisms of injury in the GAT cohort, with a few in the AMT cohort, we performed a TRISS analysis of the data set excluding all falls, as well as an analysis of only those with fall as a mechanism of injury. The results are shown in Table 4.
Discussion
Most studies comparing HEMS with GAT show some benefit of air transport. The first major comparison of outcome in the air transport of trauma patients was published by Baxt and Moody in 1983.7 The study was a retrospective TRISS-based analysis with a cohort of patients transported by ground as a control group. The authors showed a 53% reduction in mortality with AMT. Notably, there seemed to be major limitations in the skills and interventions provided by a less-experienced ground crew. Boyd and others8 also recognized this difference between the highly trained air medical crew and their ground crew counterparts. This study focused specifically on the use of AMT for trauma in a rural setting and observed that the air medical crew provided necessary assistance for less experienced and sometimes unavailable rural physicians. They found a 25% reduction in mortality with the use of air medical services. Urdaneta and colleagues3 evaluated AMT in a rural setting and found that it played a role in 26.9% of a rural trauma patient cohort.3 Several later studies have also concluded that the major benefit of AMT is the high rate of early intervention (airway management and resuscitation) by air medical crews.9–12 More recently, Thomas and colleagues13 conducted a large registry-based multicentre retrospective analysis, comparing AMT and GAT, using a stratified analysis. They too found significant mortality benefits of AMT over GAT. These benefits were associated with several factors pertaining to the rapid response and advanced skill level of the air medical crews. Cunningham and colleagues published a study showing no significant benefit of AMT and suggested that this mode of transport was overused in patients with minor injuries.14 In their study, however, a large proportion of the patients transported had an ISS < 12 and likely did not warrant HEMS. They did, however, stratify their results and showed a significant benefit of AMT in patients with an ISS between 21 and 30.
In this study, we used TRISS analysis to explore the use of rotor wing AMT for the transport and care of major trauma patients in our predominantly rural province. Our contribution with this work is to provide an outcomes analysis on a Canadian cohort of blunt trauma patients.
The AMT cohort was younger (median age 38 yr) and more severely injured (median ISS 25) than the GAT patients. In this study, AMT transport was associated with a 25% reduction in mortality (23.8% predicted, 18% actual), whereas GAT was associated with a 10% increase in mortality. Reasons for the increased survival in the HEMS patients have been discussed elsewhere, but the prevailing opinion is that the advanced training and interventions provided by the air medical crew is the single most important factor in the improved survival from AMT.3,7–13
A large number of patients in the ground ambulance cohort were injured as a result of falls. In previous studies, it has been suggested that a high percentage of falls in an older cohort may bias the results, because this patient population likely has more comorbid illness, resulting in a worse than predicted outcome.6 TRISS analyses are unable to control for this. When we excluded falls from the analyses, the AMT group still had significantly better survival than predicted. The GAT group, however, had equivalent predicted and actual survivals. Using TRISS to evaluate only the group with fall as the mechanism of injury shows the poor outcomes in this group, with a W value of –9.6 (Table 4). It would appear that outcomes for the GAT cohort have been biased by the subgroup of patients sustaining injury from falls. This population is of an older age and likely has more comorbidities; thus it is poorly modelled with the TRISS methodology. Dividing subjects into 2 age categories (≥ 55 yr and < 55 yr) is not enough to account for the significant role of age in the prediction of outcome.
Transport modality data in this study are comparable with prior studies on rural AMT.2,3,8 In these studies, interfacility transports are much more prevalent than scene transports. The urban AMT literature is quite different, usually with up to 50% of patients being transported directly from the scene. Patients with more severe injuries, requiring longer transport times or needing more advanced interventions are more likely to need initial assessment and stabilization at a regional trauma centre. These patients will also be more likely to qualify for air transport to the tertiary centre.
Several limitations of this research must be discussed. First are the limitations of using the TRISS analysis, as noted earlier. A general discussion of the problems inherent in TRISS analyses is beyond the scope of this paper. However, despite its flaws, TRISS remains the best method of evaluating outcomes in trauma. As recently as June 2005, authors publishing trauma literature continued to claim that TRISS is the gold standard for trauma outcomes analysis.15 One of the developers of the TRISS method, Dr. Howard Champion, while lamenting the need for evolution of this statistical tool, concedes that there is presently no better alternative.16
For our analyses, we substituted normal physiological values where data were missing. This particular method has not been well-validated in the literature; however, no immediate bias is evident. Inserting normal physiological values into missing data sets would, at worst, make these patients look less critical than they truly are, resulting in a higher predicted survival rate. A higher predicted survival rate should serve to underestimate the benefit of AMT in this study and may overestimate the negative outcome in GAT.
This study is still a registry-based retrospective study, subject to all of the criticisms of a retrospective study. Prospective randomized trials, however, are simply not feasible or ethical in this realm. Future work should focus on developing a modern Canadian data set for use in evaluating trauma outcomes. There are other projects in progress to develop more robust analysis tools to replace the TRISS analysis. These new statistical tools are intended to include more data on comorbid illness, age and injury, and will hopefully result in a better model of blunt trauma patients. It would be of value to evaluate the reasons for worse outcomes than predicted in GAT of trauma patients.
We have not explored the cost of HEMS in the review of our program, although cost receives significant mention in the AMT literature. One study has evaluated the cost per life-year saved when using AMT for the prehospital care of trauma patients.17 This study showed that the cost per life-year saved was approximately $2500, on the basis of a TRISS analysis, which means 5 additional survivors per 100 patients. The authors then compared this cost with other medical interventions (hypertension treatment, mammography, liver transplant), which have costs of $11 000–$43 000 per life-year saved. Assuming the benefit of AMT is real, the cost appears reasonable. True cost-effectiveness analysis, comparing the cost per life-year saved for GAT versus AMT, would be an important addition to the current literature.
Conclusions
The transport and care of blunt major trauma patients with an ISS of ≥ 12 by a provincially dedicated rotor wing air medical service, in a predominantly rural region, was associated with statistically significant less critical outcomes than those of patients transported by standard ground ambulance. This is the first large Canadian study to specifically address ground versus air transport of trauma patients on a province-wide basis with a single emergency medical service system.
This work was presented orally at the Trauma Association of Canada/Australasian Trauma Society meeting April 2005 in Whistler, BC, where the paper won best clinical research paper.
Accepted for publication Dec. 13, 2005.
Competing interests: None declared.
Correspondence to: Dr. Alex D. Mitchell, 1-026B Victoria Building, QE II Health Sciences Centre, 1278 Tower Rd., Halifax NS B3H 2Y9; fax 902 473-5835; admitche@dal.ca
References
- 1.Mann NC, Pinkney KA, Price DD, et al. Injury mortality following the loss of air medical support for rural interhospital transport. Acad Emerg Med 2002;9:694-8. [DOI] [PubMed]
- 2.Cummings G, O'Keefe G. Scene disposition and mode of transport following rural trauma: a prospective cohort study comparing patient costs. J Emerg Med 2000;18:349-54. [DOI] [PubMed]
- 3.Urdaneta LF, Miller BK, Ringenberg BJ, et al. Role of an emergency helicopter transport service in rural trauma. Arch Surg 1987;122:992-6. [DOI] [PubMed]
- 4.Nicholl JP, Beeby NR, Brazier JE. A comparison of the costs and performance of an emergency helicopter and land ambulances in a rural area. Injury 1994;25:145-53. [DOI] [PubMed]
- 5.Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma 1987;27:370-8. [PubMed]
- 6.Petrie D, Lane P, Stewart T. An evaluation of patient outcomes comparing trauma team activated versus trauma team not activated using TRISS analysis. J Trauma 1996;41:870-5. [DOI] [PubMed]
- 7.Baxt WG, Moody P. The impact of rotorcraft aeromedical emergency care service on trauma mortality. JAMA 1983;249:3047-51. [PubMed]
- 8.Boyd CR, Corse KM, Campbell RC. Emergency interhospital transport of the major trauma patient: air versus ground. J Trauma 1989;29:789-94. [DOI] [PubMed]
- 9.Moylan JA, Fitzpatrick KT, Beyer AJ, et al. Factors improving survival in multisystem trauma patients. Ann Surg 1988;207:679-85. [DOI] [PMC free article] [PubMed]
- 10.Schwartz RJ, Jacobs LM, Juda RJ. A comparison of ground paramedics and aeromedical treatment of severe blunt trauma patients. Conn Med 1990;54:660-2. [PubMed]
- 11.Schmidt U, Frame SB, Nerlich ML, et al. On scene helicopter transport of patients with multiple injuries—comparison of a German and an American system. J Trauma 1992;33:548-55. [DOI] [PubMed]
- 12.Jacobs LM, Gabram SG, Sztajnkrycer MD, et al. Helicopter air medical transport: ten-year outcomes for trauma patients in a New England program. Conn Med 1999;63:677-82. [PubMed]
- 13.Thomas SH, Harrison TH, Buras WR, et al. Helicopter transport and blunt trauma mortality: a multicenter trial. J Trauma 2002;52:136-45. [DOI] [PubMed]
- 14.Cunningham P, Rutledge R, Baker CC, et al. A comparison of the association of helicopter and ground ambulance transport with the outcome of injury in trauma patients transported from the scene. J Trauma 1997;43:940-6. [DOI] [PubMed]
- 15.Glance LG, Osler TM, Dick AW. Evaluating trauma centre quality. J Trauma 2005;58:1265-71. [DOI] [PubMed]
- 16.Champion H. Editorial comment. J Trauma 2005;58:1277.
- 17.Gearhart PA, Wuerz R, Localio AR. Cost-effectiveness analysis of helicopter EMS for trauma patients. Ann Emerg Med 1997;30:500-6. [DOI] [PubMed]


