Abstract
Introduction
Laparoscopic repair of ventral and incisional hernias (LVIHRs) is feasible; however, many facets of this procedure remain poorly defined. The indications, essential technical features and postoperative management should be standardized to optimize outcomes and facilitate training in this promising approach to incisional hernia repair.
Methods
All patients referred to one surgeon at a tertiary care centre for LVIHR from 1999 to 2004 were analyzed. Patient records were analyzed and perioperative outcomes were documented.
Results
Of the 69 patients who were referred for management of incisional hernia, 64 underwent LVIHR. The mean age of patients selected for surgery was 61.4 years (28% of patients over age 70 years); their mean body mass index (BMI) was 32.8 kg/m2 and mean American Association of Anaesthetists (ASA) score was 2.5 (52% of patients had an ASA score equal to 3). The mean operating time was 130.7 minutes for a mean abdominal wall defect of 123.9 cm2 and a mean prosthetic mesh size of 344 cm2. Patients with recurrent incisional hernias and previous prosthetic mesh were the most challenging, with a mean BMI of 39 kg/m2, mean operating time of 191 minutes, mean defect of 224 cm2 and mean prosthetic mesh size of 508 cm2. One patient was converted to open surgery and, in 2 patients, small bowel injuries were repaired laparoscopically without adverse sequelae. The mean length of stay was 4.5 days (median 3.0 d). Postoperatively, 78% of patients developed seromas within the residual hernia sac. All seromas were managed nonoperatively; one-half resolved by 7 weeks, and larger seromas persisted for up to 24 weeks. There was an 18.7% rate of minor complications and a 3.1% rate of major complications (no deaths). After a mean follow-up of 7.7 months, 2 recurrent hernias (3.1%) were identified in patients with multiple previous open mesh repairs.
Conclusion
Although LVIHR may be challenging, it has the potential to be considered a primary approach for most ventral and incisional hernias, regardless of patient status or hernia complexity.
Abstract
Introduction
La réparation par laparoscopie de hernies ventrales et cicatricielles (RLHVC) est faisable, mais de nombreux aspects de cette intervention demeurent mal définis. Il y a lieu de normaliser les indications, les caractéristiques techniques essentielles et la prise en charge postopératoire afin d'optimiser les résultats et de faciliter la formation dans cette technique prometteuse de réparation des hernies cicatricielles.
Méthodes
On a étudié le cas de tous les patients référés à un chirurgien d'un centre de soins tertiaires pour une RLHVC de 1999 à 2004. On a analysé les dossiers des patients et documenté les résultats peropératoires.
Résultats
Des 69 patients référés pour le traitement d'une hernie cicatricielle, 64 ont subi une RLHVC. L'âge moyen des patients choisis pour subir une intervention chirurgicale s'établissait à 61,4 ans (28 % des patients avaient plus de 70 ans), leur indice de masse corporelle (IMC) moyen atteignait 32,8 kg/m2 et l'indice moyen de l'American Association of Anaesthetists (ASA) s'établissait à 2,5 (52 % des patients avaient un indice ASA égal à 3). L'intervention a duré en moyenne 130,7 minutes pour un défaut moyen de la paroi abdominale de 123,9 cm2 et une résille prothétique d'une superficie moyenne de 344 cm2. Les patients qui avaient des hernies cicatricielles à répétition et avaient déjà reçu une résille prothétique représentaient les cas les plus difficiles. Ils avaient un IMC moyen de 39 kg/m2, leur intervention a duré en moyenne 191 minutes, le défaut avait une superficie moyenne de 224 cm2 et la résille prothétique, une superficie moyenne de 508 cm2. Dans le cas d'un patient, on a converti l'intervention en chirurgie ouverte et, dans deux cas, on a réparé des traumatismes de l'intestin grêle par laparoscopie sans qu'il y ait de séquelles indésirables. La durée moyenne du séjour s'est établie à 4,5 jours (médiane de 3,0 j). Après l'intervention, un sérome a fait son apparition dans le sac herniaire résiduel chez 78 % des patients. On a traité tous les séromes de façon non chirurgicale : la moitié se sont résorbés en 7 semaines et les séromes les plus étendus ont persisté jusqu'à 24 semaines. Le taux des complications mineures a atteint 18,7 % et celui des complications majeures (sans décès), 3,1 %. Après un suivi moyen de 7,7 mois, on a repéré deux hernies répétitives (3,1 %) chez des patients ayant déjà subi de multiples réparations ouvertes avec résille.
Conclusion
Même si la RLHVC peut poser un défi, on pourrait la considérer comme une technique de premier choix pour la plupart des hernies ventrales et cicatricielles, quel que soit l'état du patient ou la complexité de la hernie.
The management of patients with incisional hernia continues to test the skill and judgment of gastrointestinal surgeons. The standard open approach to incisional hernia repair has produced unsatisfactory outcomes. The only randomized, controlled clinical trial to produce reliable data on the outcomes of open incisional hernia repair reported a recurrence rate of 43% for sutured repair and 24% for mesh repair of small abdominal wall hernias.1 These disappointing results underscore the important dilemma currently facing general surgeons. With the excessive morbidity, long hospital stay and unacceptably high recurrence rates that plague the traditional open approach to incisional hernia, an alternative solution is required.2
The feasibility of a laparoscopic approach to ventral and incisional hernia repair (LVIHR) has been demonstrated in published surgical series.3–5 However, the technique of LVIHR continues to evolve, and many technical aspects of the procedure remain controversial and have not been standardized. In addition, the true effectiveness (reproducibility) of LVIHR has not been tested.6,7
Patients who develop incisional hernias are often elderly or obese, with multiple comorbid diseases placing them at substantial risk for further surgical management. Clinical experience suggests that LVIHR may be used as a primary approach for most patients who present with ventral and incisional hernias. In this study, one surgeon's experience with LVIHR is analyzed to characterize the indications, outcomes and challenges for LVIHR.
Methods
From August 1999 to June 2004, all patients referred to a single surgeon at St Joseph's Hospital in Hamilton, Ontario (a tertiary care hospital) with ventral and incisional hernias and deemed fit for surgery were offered LVIHR with prosthetic mesh. Patients were not specifically excluded from a laparoscopic approach on the basis of their age, number of previous repairs, estimated defect size, intraperitoneal mesh, body mass index (BMI), comorbidities or abdominal wall stomas. Data were abstracted from office and hospital charts, and all details of patient progress and complications related to surgery were documented. Follow-up for each patient comprised complete clinical assessment and physical examination. The data were evaluated with summary statistics to analyze outcomes.
Surgical technique
All patients were given a mechanical bowel preparation preoperatively. Prophylaxis for wound infection and deep vein thrombosis were used routinely. The patient was catheterized and positioned supine with both arms tucked in at the sides.
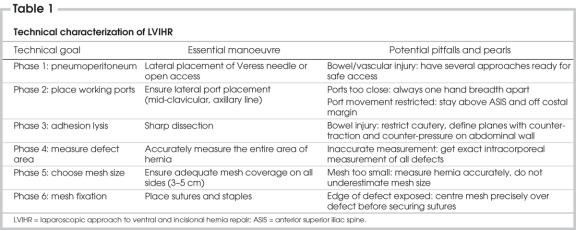
The technical approach to LVIHR is described in Table 1. A pneumoperitoneum is established with a Veress needle in the subcostal position. Trocars are placed as shown in Figure 1. A 10-mm 0º or 30º laparoscope is inserted with an Optiview 10-mm trocar (Ethicon, Cincinnati, Ohio). The camera port is inserted as laterally as possible on the side estimated to have the greatest distance from the abdominal wall defect. Two working ports are placed just above the level of the camera port and on either side (usually one 10-mm and one 5-mm trocar). All abdominal wall adhesions are divided with scissors and cautery. The falciform ligament is often mobilized from the anterior abdominal wall. Care must be taken with the use of electrocautery to avoid inadvertent bowel injury. The total area of abdominal wall defects are identified and measured internally with an umbilical tape marked at 2-cm increments. An appropriate sized mesh is chosen, allowing at least 3-cm overlap on all sides (Dual mesh, Gore Flagstaff, Ariz. or Composix EX, Bard Billerica, Mass.). Anchoring sutures (2–0 Gore, Gore Flagstaff, Ariz.) are attached to the periphery of the mesh (bites incorporating expanded polytetrafluoroethylene [ePTFE] and polypropylene layers). From 4 to 10 sutures are usually placed, depending on the mesh size (i.e., 4 sutures for 10 × 15-cm mesh, 8–10 sutures for 20 × 30-cm mesh). The mesh is then placed into the peritoneal cavity via the 10-mm working port or directly through the port site. The mesh is oriented and centred on the defect, and the transabdominal anchoring sutures are positioned with a Gore Suture Passer. The sutures are tied, and the edge of the mesh is secured with spiral tacks at 1-cm intervals. Additional tacks are placed centrally in large mesh applications. The pneumoperitoneum is reduced from 15 mm Hg to 10 mm Hg, so that the sutures are tied in a tension-free manner. All 10-mm trocar sites are closed with a Carter Thomason fascial closure device (Inlet Medical, Eden Prairie, Minn.).
Table 1
FIG. 1. Lateral port placement for laparoscopic approach to ventral and incisional hernia repair.
Results
Demographics
During the study period, 69 patients were referred for elective repair of incisional or ventral hernia. One patient requested open repair and 1 patient was advised by medical consultants not to proceed with surgical management due to unacceptable operative risk (this patient had obesity, diabetes, hypertension as well as renal failure and a massive, chronically incarcerated ventral hernia and nonhealing skin ulcer related to the hernia). Three patients with massive flank hernias after open nephrectomy were not offered surgery (muscle denervation, no identifiable fascial edge beyond costal margin or iliac crest); 1 patient with a massive, recurrent abdominal wall hernia with a broad defect extending from xiphoid to pubis did not return to clinic after initial consultation.
Sixty-four patients underwent elective repair of ventral and incisional hernias by a laparoscopic approach. One patient with a recurrence after LVIHR was repaired laparoscopically and is included in the analysis. This group included patients at advanced age with abdominal wall stomas (hernia not related to stoma site), multiple comorbidities, obesity, multiple previous recurrences and intraperitoneal mesh.
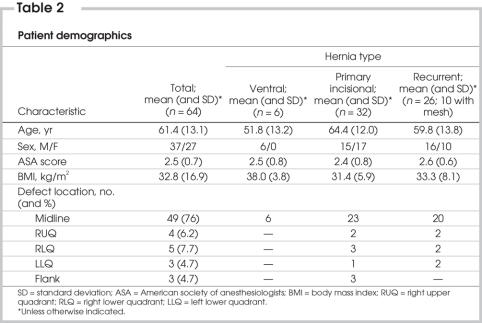
Table 2 shows the basic demographics of the group who underwent LVIHR. Ventral hernias are defined as abdominal wall defects (usually peri-umbilical) not arising on the basis of a previous abdominal incision. The age range was 27–87 years, with over 28% of patients aged 70 years or older. Classification of patient risk by American Association of Anaesthetists (ASA) score showed that 8% of patients were ASA 1, 37% ASA 2, 52% ASA 3 and 3% ASA 4. The mean BMI for all patients in this series was 32.8 kg/m2; patients with ventral hernias had a higher BMI (mean 38 kg/m2). The abdominal wall defects repaired in this series were most commonly located at the midline (76% overall).
Table 2
Outcomes
The outcomes of surgical management are shown in Table 3. The abdominal wall defects in this series were relatively large (mean size 123.9 cm2), and the overall mean operating time was 130.7 minutes. One LVIHR was converted to open surgery without complication. This patient had a large, chronically incarcerated midline incisional hernia containing a small bowel, and the small bowel could not be mobilized successfully from the hernia sac. There were 2 intra-operative complications, comprising one seromuscular tear of the small bowel on insertion of the primary visually guided trocar and one sharp injury to the small bowel during adhesion lysis. Both were repaired by intracorporeal suturing, and the LVIHR was completed as usual. There were no obvious adverse sequelae as a result.
Table 3
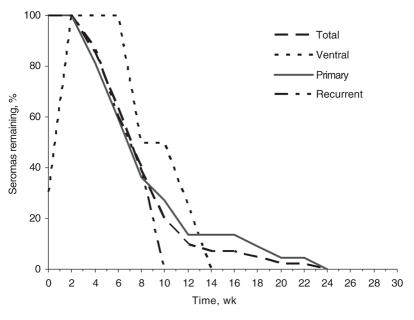
There were 50 postoperative seromas (78% of patients overall) identified on the initial follow-up visit (usually 3 weeks after surgery). All patients were observed to resolution of the seroma, and no patients required aspiration. The mean time to seroma resolution was 8.6 weeks. When analyzed by hernia type, time to resolution was 10.5 weeks for ventral hernias, 9 weeks for primary incisional hernias and 7.7 weeks for recurrent incisional hernias. Analyzing the time to resolution further indicated that approximately one-half of all seromas resolved by 7 weeks; the larger seromas required up to 24 weeks to resolve (Fig. 2). Five patients developed considerable and persistent abdominal wall pain due either to the anchoring sutures or to spiral tacks. This was managed successfully with a combination of opioid analgesics and a short course of nonsteroidal anti-inflammatory medications (NSAIDs) in all patients except one, who required referral to a pain service. There were no instances of mesh-related infections; one trocar site infection was managed with drainage and antibiotics. Two patients required readmission for persisting nausea and ileus, which resolved after conservative management. One patient required reoperation in the early postoperative period for ischemia of the splenic flexure of the colon; the patient required bowel resection with diverting stomas and removal of the mesh. This patient survived a complicated hospital stay of 75 days. Three other important complications occurred, including postoperative delirium in an 87-year-old man and postoperative weakness in an 82-year-old woman (both fully resolved). One patient with a pre-existing history of cardiac valvular disease and prosthetic valve replacement developed a dissection of the thoracic aorta on post-operative day 1 and required referral to a vascular surgeon for management. The mean overall length of stay was 4.5 days (median 3.0 d).
FIG. 2: Analysis of time to resolution for postoperative seroma after LVIHR.
There were 2 recurrences (3.1%) identified in this series after a mean follow-up of 7.7 months (range 1–32 mo, median follow-up 4 mo; 28% of patients seen at 1 year, 6% of patients seen at 2 years). Both patients had multiple previous open incisional hernia repairs with placement of prosthetic mesh. One patient was managed successfully with LVIHR; the second patient did not wish further surgery for a hernia that was considered small and was asymptomatic at the time of assessment.
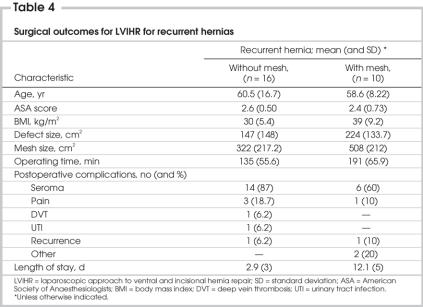
A comparison of LVIHR for recurrent hernias that have been previously repaired with and without mesh is shown in Table 4. Patients with a recurrent incisional hernia and previously placed mesh had morbid obesity (mean BMI 39 kg/m2) with a large abdominal wall defect (mean size 224 cm2) and required very large prosthetic mesh for repair (mean size 508 cm2). Operating times and hospital stay was also increased in this group of patients (median operating time 215 min, median length of stay 5 d).
Table 4
Discussion
Gastrointestinal surgeons need a successful method for managing ventral and incisional hernias. The results of open surgery have been very disappointing, with a recurrence rate near 50% after primary repair and 23% after mesh repair.1 These data are derived from the only randomized controlled trial assessing open surgical management of incisional hernia. Also reported in this study was the substantial morbidity of open surgery, including mesh-related infections (4%), wound hematomas (11%) and persisting abdominal wall pain (18%).
LVIHR is a challenging procedure, but it has the potential to improve outcomes for the management of ventral and incisional hernia. The data presented in this manuscript suggest that LVIHR may be indicated for most patients, regardless of age, status or hernia complexity. In this series, the most challenging patients were those with long-standing defects, incarcerated small bowel (only conversion in this series), morbid obesity, multiple previous repairs and placement of prosthetic mesh. Adhesions tend to be widespread and fibrotic in patients with previously placed prosthetic mesh, and the bowel can be densely adherent to the mesh. Interestingly, elderly patients and patients with elevated ASA status or more complex presentations (abdominal wall stomas, renal failure, and multiple previous surgeries) may be managed by LVIHR with satisfactory outcomes.
In this series, important distinctions have been identified between ventral, primary incisional and recurrent hernias (Table 3). Ventral hernias tend to be small (mean size 34.7 cm2); recurrent hernias tend to be quite large and often comprise multiple defects (mean size 176 cm2 v. mean primary incisional hernia size 104.2 cm2). Equally important is the size of the mesh required, which increases according to the defect size; the largest mesh is often used in the repair of recurrent incisional hernias (mean mesh size 388.9 cm2). The operating times reflect the defect size and mesh required for repair. Ventral hernias are repaired in less time than incisional hernias (mean operating time 95.8 min), whereas recurrent incisional hernias tend to require the most time (mean operating time 155.7 min). These are important criteria for the surgeon to consider when selecting cases for LVIHR early in his or her experience.
It is important to standardize new surgical procedures to facilitate the teaching and analysis of outcomes. Although there may be variations in approach, each phase of LVIHR has essential goals, technical manoeuvres and potential pitfalls (Table 1). In the initial phase of LVIHR, a pneumoperitoneum is established to create the working space. Access to the peritoneal cavity remains controversial for all laparoscopic procedures, and a standardized approach has not been established.8,9 In this series, the peritoneal cavity was accessed by Veress needle. An open approach is reserved for patients in whom a pneumoperitoneum cannot be established. Patients undergoing LVIHR are often obese; consequently, a routine lateral open approach can be challenging. In the second phase of LVIHR, the lateral working ports are placed under direct vision. It is important to position the working ports as far laterally as possible to maximize the distance from the defect. This facilitates placement of a large mesh and mesh fixation. For the third and most challenging phase of the procedure, all adhesions to the anterior abdominal wall are divided. This is done with metzenbaum scissors and careful use of electrocautery. A 30º camera is essential to provide visualization of adhesions and adherent bowel. If a bowel injury occurs during this phase of the procedure, the injury must be fully characterized and repaired. Unrecognized bowel injury is a serious complication and demands vigilance throughout such complex laparoscopic procedures.6 If the operating surgeon has any suspicion of additional injuries or is not confident of their assessment or skills in laparoscopic repair, conversion to open surgery is the recommended and prudent management strategy. Subsequent mesh placement after bowel injury is a challenging decision. A complete bowel preparation is routinely given to facilitate management of large bowel injury. I would be reluctant to place prosthetic mesh in the event of a large bowel injury during LVIHR. In this series, one patient had a full thickness small bowel injury that was primarily repaired laparoscopically. There was no evidence of local contamination, and LVIHR was completed with no subsequent infectious complications.
Once adhesion lysis is complete, the surgeon can identify all abdominal wall defects and accurately measure the defective area. This is best accomplished intracorporeally to avoid the distortion from the abdominal wall contour and the hernia sac (distended with CO2). Extracorporeal measurement of the defective area can be inaccurate, especially in patients with obesity. Accurate measurement of the defect is important, so that an appropriate sized mesh is chosen. A mesh that is too small reduces coverage of the defect; conversely, a mesh that is too large can create technical problems during placement and positioning.
The optimal type, size and method of mesh prosthesis fixation has not been established. A composite mesh provides the relative adhesion barrier of ePTFE and the rigidity, strength and incorporation of polypropylene (Composix EX, Bard, Billerica, Mass.). In follow-up of patients after LVIHR ePTFE mesh tends to display considerable laxity and can bulge in patients with large abdominal wall defects. The size of mesh chosen for LVIHR is important to achieve substantial overlap of the defect. Although initial reports recommended an overlap of 1–2 cm, a greater degree of overlap provides additional protection in the event of mesh shrinkage or migration or if the mesh is not accurately centred on the abdominal wall defect.10 In addition, greater mesh coverage may improve incorporation and fixation. In this series, 2 hernia recurrences have been identified over a relatively short follow-up period. Each of these was due to inadequate coverage of the defect and eventual prolapse of the mesh into the defect. This was clearly visualized on subsequent LVIHR for one of the recurrences. Others have documented high recurrence rates after LVIHR, suggesting the use of small mesh prostheses, poor positioning or poor fixation techniques.7 Most authors report low recurrence rates, although few studies have sufficient follow-up to give reliable data.11–13
In the final phase of LVIHR, the mesh prosthesis is fixed with a combination of sutures and spiral tacks. Sutures provide reliable full-thickness abdominal wall fixation, whereas spiral tacks may have a variable degree of penetration of the abdominal wall (standard spiral tack length is 4.8 mm).14 Poor fixation of the mesh will ultimately lead to a recurrence as the mesh migrates into the defect. Conversely, sutures cause distinct postoperative pain, limiting mobility and prolonging postoperative ileus. There may be a relation between the type of mesh, the extent of mesh overlap of the defect and the number of sutures required. In essence, using a large macroporous mesh with considerable overlap (> 3 cm) might allow the surgeon to modify the number of anchoring sutures to reduce postoperative pain.
The most appropriate management of postoperative seroma after LVIHR has not been fully described.15 Seromas often occur after LVIHR but have not been clearly classified as complications.16 In this series, postoperative seromas were identified in most patients (78%), whereas other series have documented much lower rates of postoperative seroma. Scrutiny of these studies suggests that only persistent seromas are reported.13 In this series, reassurance and ongoing follow-up was satisfactory for all patients; no patient required invasive management for a seroma. Other authors have reported routine aspiration for all seromas.3 The implications of a conservative versus an aggressive approach to seroma after LVIHR remains to be established. In this series, no patient required aspiration of a seroma, and no mesh infections were encountered.
Further effort by those experienced in LVIHR is necessary to standardize this technique to facilitate the training and assessment of clinical outcomes. Clinical trials are needed to evaluate this innovative approach to incisional and ventral hernia and to compare LVIHR to the standard open approach. This manuscript may serve as a guide to facilitate the standardization of LVIHR and the management of these complex patients.
Acknowledgments
Thanks to Dr. C.J. de Gara for his editorial guidance in the review of this manuscript.
Accepted for publication July 19, 2005
Competing interests: Dr. Birch has received speaker's fees from Bard.
Correspondence to: Dr. Daniel W Birch, Royal Alexandra Hospital, 10240 Kingsway, Edmonton AB T5H 3V9; fax 780 735-4771; dbirch@ualberta.ca
References
- 1.Luijendijk RW, Hop WC, van den Tol MP, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 2000;343:392-8. [DOI] [PubMed]
- 2.Korenkov M, Sauerland S, Arndt M, et al. Randomized clinical trial of suture repair, polypropylene mesh or autodermal hernoplasty for incisional hernia. Br J Surg 2002;89:50-6. [DOI] [PubMed]
- 3.Heniford BT, Park A, Ramshaw BJ, et al. Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg 2000;190:645-50. [DOI] [PubMed]
- 4.Goodney PP, Birkmeyer CM, Birkmeyer JD. Short-term outcomes of laparoscopic and open ventral hernia repair. Arch Surg 2002;137:1161-5. [DOI] [PubMed]
- 5.Park A, Birch DW, Lovrics P. Laparoscopic and open incisional hernia repair: a comparison study. Surgery 1998;124:816-22. [DOI] [PubMed]
- 6.Wright BE, Niskanen BD, Peterson DJ, et al. Laparoscopic ventral hernia repair: are there comparative advantages over traditional methods of repair? Am Surg 2002;68:291-5. [PubMed]
- 7.Rosen M, Brody F, Pronsky J, et al. Recurrence after laparoscopic ventral hernia repair. Surg Endosc 2003;17:123-8. [DOI] [PubMed]
- 8.Merlin TL, Hiller JE, Maddern GJ, et al. Systematic review of the safety and effectiveness of methods used to establish pneumoperitoneum in laparoscopic surgery. Br J Surg 2003;90:668-79. [DOI] [PubMed]
- 9.Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc 2002;16:1121-43. [DOI] [PubMed]
- 10.Holzman MD, Purut CM, Reintgen K, et al. Laparoscopic ventral and incisional hernioplasty. Surg Endosc 1997;11:32-5. [DOI] [PubMed]
- 11.Eid GM, Prince JM, Mattar SG, et al. Medium-term follow-up confirms the safety and durability of laparoscopic ventral hernia repair with PTFE. Surgery 2003;134:599-603. [DOI] [PubMed]
- 12.Carbajo MA, Martp del Olomo JC, Blanco JI, et al. Laparoscopic approach to incisional hernia. Surg Endosc 2003;17:118-22. [DOI] [PubMed]
- 13.Heniford BT, Park A, Ramshaw BJ, et al. Laparoscopic repair of ventral hernias: nine years' experience with 850 consecutive hernias. Ann Surg 2003;238:391-9. [DOI] [PMC free article] [PubMed]
- 14.Van't Riet M, De Vos van Steenwijk PJ, Kleinrensink GJ, et al. Tensile strength of mesh fixation methods in laparoscopic incisional hernia repair. Surg Endosc 2002;16:1713-6. [DOI] [PubMed]
- 15.Tsimoyiannis EC, Siakas P, Glantzounis G, et al. Seroma in laparoscopic ventral hernioplasty. Surg Laparosc Endosc Percutan Tech 2001;11:317-21. [DOI] [PubMed]
- 16.Susmallian S, Gewurtz G, Ezri T, et al. Seroma after laparoscopic repair of hernia with PTFE patch: is it really a complication? Hernia 2001;5:139-41. [DOI] [PubMed]