Abstract
Objective
This study was designed to address a recurring observation in our centre that, despite a satisfactory postoperative radiographic limb alignment, some patients are dissatisfied with the alignment and appearance of their operated leg. We carried out a prospective survey to determine patient perception of limb alignment after total knee arthroplasty (TKA) and whether level of satisfaction with alignment affects clinical outcome.
Methods
Patients self-rated their alignment, their satisfaction with alignment and their level of knee pain on a visual analogue scale (VAS). Additional outcome measures included pre-and postoperative Knee Society Score (KSS), Oxford Knee Score (OKS) and the Health Survey Short Form (SF-12).
Results
Twenty of 87 (23%) patients were dissatisfied with their new leg alignment and had a poorer perception of pain and range of motion after TKA. Despite this finding, KSS and OKS were no different between patients who were satisfied and those who were dissatisfied with their limb alignment. The SF-12 showed a trend toward lower scores in patients who were dissatisfied with their limb alignment.
Conclusions
Satisfaction with perceived limb alignment appears to influence outcome after TKA and is not reflected in current outcome scales. Perhaps patients should be counselled on how alignment is restored and on what to expect of their limb alignment and appearance after TKA.
Abstract
Objectif
Cette étude visait à donner suite à une observation qui revenait souvent dans notre Centre, soit qu'en dépit de l'alignement satisfaisant du membre confirmé par radiographie postopératoire, certains patients sont insatisfaits de l'alignement et de l'apparence de leur jambe opérée. Nous avons procédé à un sondage prospectif pour déterminer la perception que les patients ont de l'alignement du membre après une arthroplastie totale du genou (ATG) et si le niveau de satisfaction à l'égard de l'alignement a un effet sur le résultat clinique.
Méthodes
Les patients ont autoévalué leur alignement, leur satisfaction à l'égard de celui-ci et leur niveau de douleur au genou sur une échelle visuelle analogue (EVA). On a mesuré d'autres résultats comme le score de la Knee Society (KSS), le score d'Oxford pour le genou (OKS) et le formulaire abrégé de l'Enquête sur la santé (SF-12).
Résultats
Vingt des 87 patients (23 %) étaient insatisfaits du nouvel alignement de leur jambe et avaient une moins bonne perception de la douleur et de l'amplitude du mouvement après l'ATG. En dépit de cette constatation, les scores KSS et OKS n'étaient pas différents entre les patients satisfaits de l'alignement de leur membre et ceux qui ne l'étaient pas. Leur formulaire SF-12 a révélé une tendance à des scores plus faibles chez les patients insatisfaits de l'alignement de leur membre.
Conclusions
La satisfaction à l'égard de l'alignement perçu du membre semble avoir une influence sur le résultat après une ATG et ne se reflète pas dans les échelles courantes de résultats. Il faudrait peut-être expliquer aux patients comment on rétablit l'alignement et leur dire à quoi ils doivent s'attendre quant à l'alignement et à l'apparence de leur membre après une ATG.
The success of total knee arthroplasty (TKA) in relieving pain and improving function has been well-documented.1,2 Long-term survival of TKA has been shown to correlate with achieving appropriate coronal plane alignment.3,4 Radiographic evaluation of leg alignment is included in the objective outcome assessment of the Knee Society Score (KSS);5 however, the issue of patient satisfaction with post-TKA lower extremity alignment has, to our knowledge, not been addressed in any of the commonly reported arthroplasty outcome measures, including the KSS, the Oxford Knee Score (OKS) and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) disease-specific functional rating tools.5–7
Fitzpatrick and colleagues8 observed that patient expectations are strongly linked to clinical outcomes. Mancuso and collaborators9 developed the Hospital for Special Surgery Knee Replacement Expectations Survey to address this topic, with relevant questions largely based on pain relief, improving range of motion (ROM) and function. Further, when Bullens and colleagues10 compared subjective and objective outcomes for TKA, they found a poor correlation between physician and patient perspectives. It has been widely reported that surgeons often perceive outcomes of total hip and knee arthroplasty with more success than patients do.11–14
This study was designed to address a recurring observation in our centre that, despite a satisfactory postoperative radiographic limb alignment, some patients are dissatisfied with the alignment and appearance of their operated leg. It was occasionally observed that, when the relative width of the pelvis is large relative to limb length, specifically among women, the limb often appeared valgus clinically when radiographically it was varus gonarthrosis. Further, once alignment was corrected to neutral radiographically with a TKA, their knees appeared to be more valgus, which was unsatisfactory to some patients. Our primary objective was to determine whether patient dissatisfaction with self-perceived knee alignment contributed to an inferior clinical outcome. Given our above-noted clinical observation, we also sought to determine whether sex and body mass index (BMI) contributed to a misperception of limb alignment and greater patient dissatisfaction.
Materials and methods
After obtaining Research Ethics Board approval, 87 patients undergoing elective primary unilateral TKA for osteoarthritis between August 2003 and March 2004 at a single tertiary care arthroplasty centre consented to participate in a prospective evaluation of their perceived satisfaction with postoperative TKA alignment.
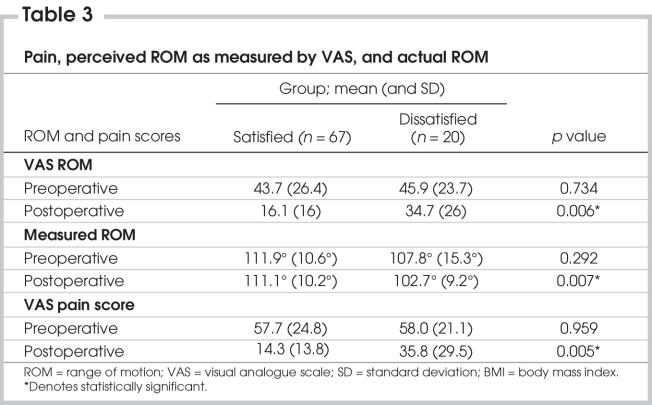
Patients were asked to complete a nonvalidated knee alignment questionnaire preoperatively (1 week before surgery) and at 6 months postoperative (Fig. 1). Patients were asked whether they were satisfied with their limb alignment. The questionnaire included a visual analogue scale (VAS) of pain and ROM as well as pictorials and descriptions illustrating varus, normal and valgus limb alignment. The questionnaire included a 5-point ordinal scale, which asked patients to self-rate the severity of their deformity (Fig. 1).
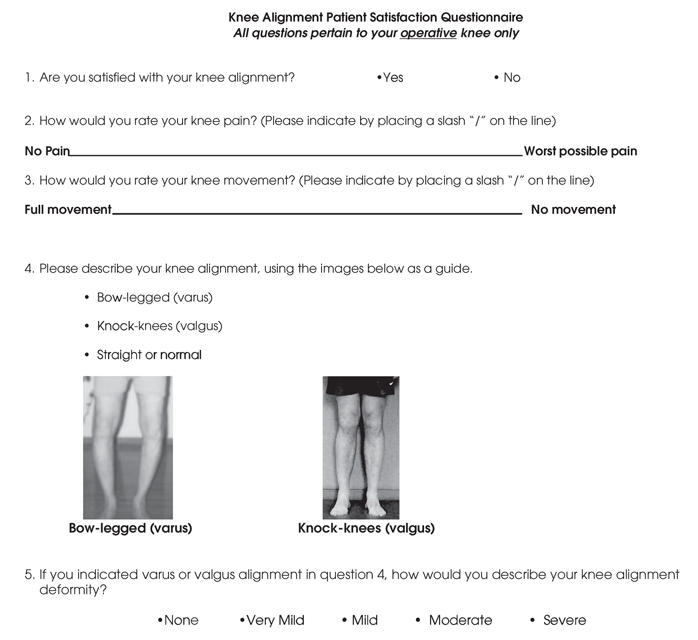
FIG. 1. Nonvalidated patient-derived questionnaire to assess patient satisfaction with alignment, perception of alignment, pain and range of motion.
All patients were examined clinically and radiographically at preoperative assessment and 6 months post-operative. Clinical outcome assessment included measured ROM and the KSS,5 as recorded by an independent observer who was not involved in direct patient care. We reported the KSS clinical score, which incorporates pain, stability and ROM and the KSS function score, which rates the patient's ability to walk and climb stairs and perform activities of daily living.
Supplementary subjective outcome tools completed by the patient preoperatively and at 6 months postoperative included the OKS6 and the Health Survey Short Form (SF-12),15 which incorporates both physical and mental component summary scores.
Standardized 3-foot anteroposterior radiographs were used to measure preoperative and postoperative anatomic knee alignment. The tibiofemoral angle is measured by intersecting the femoral anatomic axis with the tibial anatomic axis.16 As per Petersen and Engh,16 acceptable alignment was defined as an anatomic axis of 4 to 10 degrees valgus. Radiographic alignment was compared with patient perception of alignment, rated as varus, valgus or normal, as documented on the questionnaire. An independent observer performed radiographic measurement.
We analyzed all categorical data, using descriptive statistics and the chi-square test or Fisher's exact test where appropriate. We analyzed continuous data, including age, BMI, radiographic alignment measures, ROM and outcome scores, using descriptive statistics. Outcome variables among patients satisfied with postoperative alignment, compared with unsatisfied patients, were analyzed with the independent samples t test. A value of p < 0.05 was considered statistically significant.
Results
The study sample comprised 87 consecutive unilateral TKA patients undergoing surgery for osteoarthritis, including 56 (64.4%) women and 31 (35.6%) men. Patients' mean age was 69.2 (standard deviation [SD] 8.8) years and mean BMI was 33.3 (SD 6) kg/m2.
Of the study sample, 51 of 87 (58.6%) patients were correct in determining their preoperative knee alignment as varus, valgus or normal, and 56 of 87 (64.4%) were correct in determining their postoperative alignment, as confirmed by radiographic alignment measurement.
Sixty-seven of 87 patients (77%) were satisfied with their postoperative alignment, whereas 20 of 87 (23%) were dissatisfied. Sixty-seven of 48 (71.6%) satisfied patients correctly described their alignment, while only 8 of 20 (40%) patients dissatisfied with their postoperative alignment correctly determined their alignment (p = 0.01). Preoperatively, both the satisfied and the dissatisfied patients rated the severity of their deformity similarly. Postoperatively, the dissatisfied patients perceived the malalignment of their limb as moderate or severe, while the satisfied patients rated their deformity from mild to none (Table 1).
Table 1
The mean radiographic alignment was no different between patients who were satisfied with their alignment and those who were dissatisfied. Mean preoperative radiographic tibiofemoral alignment was 4.3 degrees for both the satisfied (SD 4.2°) and the dissatisfied group (SD 4.7°), and postoperative tibiofemoral radiographic alignment was 5.3 degrees (SD 2.4° and SD 2.2°, respectively) for both groups. Of all patients, 84% had normal radiographic alignment (4°–10° tibiofemoral angle). Of the 20 dissatisfied patients, only 1 was outside the neutral range (4°–10°), with a 2-degree tibiofemoral angle.
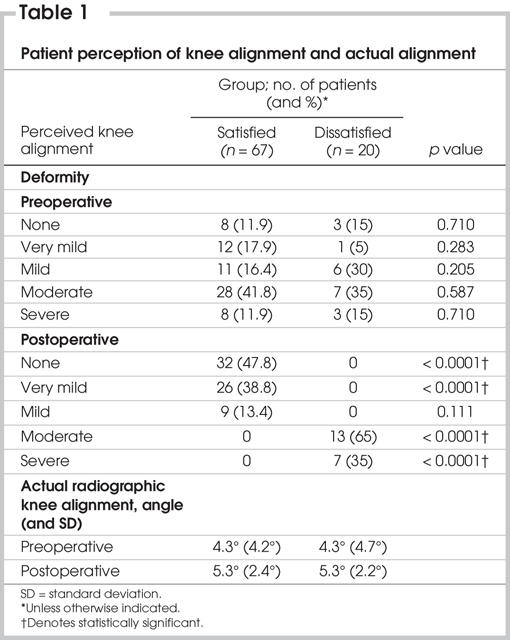
Patient demographics, including age, sex and BMI, were not statistically different between patients who were satisfied with their limb alignment and those who were dissatisfied (Table 2).
Table 2
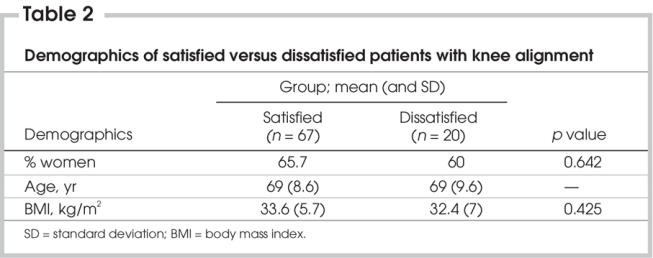
Mean preoperative VAS pain score was similar between the 2 groups, with a score of 57.7 (SD 24.8) for satisfied patients and 58 (SD 21.1) for dissatisfied patients (p = 0.959). Six-month postoperative VAS pain score was significantly different between the 2 groups, with a mean score of 14.3 (SD 13.8) for the satisfied group and 35.8 (SD 29.5) for the dissatisfied group (p = 0.005) (Table 3).
Table 3
Mean preoperative VAS knee ROM was rated as 43.7 (SD 26.4) by the satisfied group and 45.9 (SD 23.7) by the dissatisfied group (p =0.734), while postoperative VAS knee range of movement was rated as 16.1 (SD 16) by the satisfied group and 34.7 (SD 26) by the dissatisfied group (p = 0.006) (Table 3). Mean actual preoperative measured ROM was different between the 2 groups, at 111.9 (SD 10.6) for the satisfied group and 107.8 (SD 15.3) for the dissatisfied group (p = 0.292). At 6 months postoperative, we showed a significant difference in measured ROM between the 2 groups; ROM for the satisfied group was 111.1 (SD 10.2) and for the dissatisfied group was 102.7 (SD 9.2) (p = 0.007) (Table 3).
Interestingly, mean actual ROM and patient perceived ROM as measured with the VAS scale were significantly correlated both preoperatively (0.044) and postoperatively (p = 0.007) for the 2 groups.
The mean KSS and OKS scores did not differ between the patients who were satisfied with their limb alignment and those who were dissatisfied both pre-and postoperatively (Table 4).
Table 4
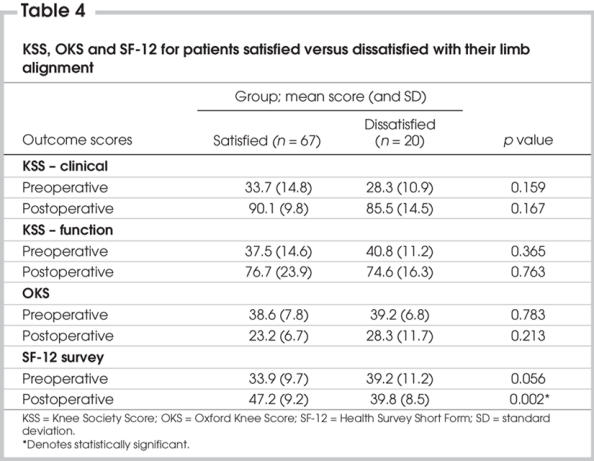
The SF-12 scores showed a trend toward a higher score preoperatively in the group of patients dissatisfied with limb alignment (33.9 v. 39.2; p = 0.056) and less improved scores at 6 months postoperative in those who were dissatisfied with limb alignment (39.8 v. 47.2; p < 0.002) (Table 4).
Discussion
The current study confirmed our impression that patient perception of knee alignment correlates poorly with true radiographic alignment. Despite generally normal radiographic alignment, almost one-quarter of patients were dissatisfied with their limb alignment. Patients who were dissatisfied were more likely to incorrectly perceive their alignment and rate the deformity as more severe. We tried to implicate overlying soft tissues or limb shape as the cause for this misperception of limb alignment. Large BMI and female sex were thought to reflect this misleading limb shape; however, these factors were not shown to correlate with a poor perception of limb alignment.
Patients dissatisfied with their limb alignment had poorer self-perceived pain and ROM postoperatively than did patients who were satisfied with their alignment. Objectively, there was a difference in measured ROM between the 2 groups but no difference in knee alignment. It is difficult to ascertain whether the perceived increased pain and poorer ROM reflects dissatisfaction with limb alignment or whether all 3 factors reflect a global feeling of dissatisfaction not captured in the KSS and OKS. When comparing the SF-12 scores pre-operatively between our 2 groups, the difference did not reach statistical significance (p = 0.056). It did, however, show a trend toward the dissatisfied group functioning better preoperatively with little improvement postoperatively. With a larger sample size, this might have reached significance, making it valuable in future studies predicting patients with poorer subjective outcomes after TKA. Perhaps patients dissatisfied with their limb alignment generally had a higher expectation from their TKA, compared with those who were satisfied with their limb alignment.
Patient misperception of knee alignment is likely multifactorial. It may be that patients simply did not understand the meaning of alignment, despite pictorials and descriptions. The issue of patient satisfaction or, more specifically, dissatisfaction, with knee alignment is far more complex. It may be that the dissatisfaction noted in our study reveals other variables in addition to alignment, such as a perception of more pain and poorer ROM. Although the group of patients dissatisfied with their knee alignment reported greater VAS pain scores, it might have been helpful to corroborate this finding to objective measures, such as narcotic use postsurgery. Regardless, limb alignment appears to be an issue that is important to patients, and it is not addressed in the outcome measures evaluated in this study.
Although we used a nonvalidated questionnaire to gather data for this study, there is, to our knowledge, no subjective outcome tool that evaluates patient perception of knee alignment. Several studies have demonstrated that simple questionnaires on patient satisfaction have high correlation with more elaborate disease-specific questionnaires and are very reliable.17,18 A study should be undertaken to validate a questionnaire that incorporates the issue of patient satisfaction with their perceived knee alignment.
Restoring a neutral mechanical axis is a key technical consideration in TKA and has been shown to correlate with improved implant survival.3,4 Achieving this balance can be challenging. Petersen and Engh16 restored neutral alignment in 74% of their cases. Mahaluxmivala and colleagues19 achieved a neutral mechanical alignment in 75% of cases in a series of 673 patients. In the current study, neutral alignment was achieved in 84% of cases, which likely reflects improved instrumentation. While we don't recommend altering alignment to try to match what a patient perceives as satisfactory, we do acknowledge that a discussion should take place to determine patient expectations preoperatively. Patients can then be counselled on what limb alignment and appearance will be achieved after correction within a neutral range.
In conclusion, perceived knee alignment seems to be a factor that influences patient perceived outcomes after TKA and is not reflected in commonly used subjective outcome tools. We could not identify patients at risk for dissatisfaction with knee alignment based on sex or BMI. This study supports the need to place greater emphasis on matching patient expectations to outcomes. Specifically, patients should be educated on what to expect of the appearance of their limb after TKA. This may be accomplished by explaining preoperatively that they have a radiographic deformity that needs to be corrected, even though they may not appreciate that deformity clinically in their own limb. Patient satisfaction with regard to limb alignment should be considered for inclusion in subjective TKA outcome tools.
Accepted for publication Jan. 9, 2006
Manuscript presented, in its entirety, in a podium presentation at the 2005 Canadian Orthopaedic Association Annual Meeting, Montréal, Québec, June 2005.
Competing interests: None declared.
Correspondence to: Danielle Petruccelli, Hamilton Arthroplasty Group, Hamilton Health Sciences Henderson Hospital, 711 Concession St., Hamilton ON L8V 1C3; fax 905 389-5617; petrucce@hhsc.ca
References
- 1.Schai PA, Thornhill TS, Scott RD. Total knee arthroplasty with the PFC system. Results at a minimum of ten years and survivorship analysis. J Bone Joint Surg Br 1998;80:850-8. [DOI] [PubMed]
- 2.Gill GS, Joshi AB, Mills DM. Total condylar knee arthroplasty: 16 to 21 year results. Clin Orthop Relat Res 1999;367:210-5. [PubMed]
- 3.Bargren JH, Blaha JD, Freeman MAR. Alignment in total knee arthroplasty: correlated biomechanical and clinical observations. Clin Orthop Relat Res 1983;173:178-83. [PubMed]
- 4.Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br 1991;73:709-14. [DOI] [PubMed]
- 5.Insall JN, Dorr LD, Scott RD, et al. Rationale of the knee society clinical rating system. Clin Orthop Relat Res 1989;248:13-4. [PubMed]
- 6.Dawson J, Fitzpatrick R, Murray D, et al. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 1998;80:63-9. [DOI] [PubMed]
- 7.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC, a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-40. [PubMed]
- 8.Fitzpatrick R, Fletcher A, Gore S. Quality of life measures in health care. I: applications and issues in assessment. BMJ 1992;305:1074-7. [DOI] [PMC free article] [PubMed]
- 9.Mancuso CA, Sculco TP, Wickiewica TL, et al. Patients' expectations of knee surgery. J Bone Joint Surg Am 2001;83-A:1005-12. [DOI] [PubMed]
- 10.Bullens PH, van Loon CM, de Waal Malefijt MC, et al. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty 2001;16:740-7. [DOI] [PubMed]
- 11.Moran M, Khan A, Sochart DH, et al. Expect the best, prepare for the worst: surgeon and patient expectation of the outcome of primary total hip and knee replacement. Ann R Coll Surg Engl 2003;85:204-6. [DOI] [PMC free article] [PubMed]
- 12.Lieberman JR, Dorey F, Shekelle P. Differences between patients' and physicians' evaluations of outcome after total hip arthroplasty. J Bone Joint Surg Am 1996;78:835-8. [DOI] [PubMed]
- 13.McGrory BJ, Morrey BF, Rand JA, et al. Correlation of patient questionnaire responses and physician history in grading clinical outcome following hip and knee arthroplasty. A prospective study of 201 joint arthroplasties. J Arthroplasty 1996;11:47-57. [DOI] [PubMed]
- 14.Brokelman RB, van Loon CJ, Rijnberg WJ. Patient versus surgeon satisfaction after total hip arthroplasty. J Bone Joint Surg Br 2003;85:495-8. [PubMed]
- 15.Ware J Jr, Kosinski M, Keller SD. A 12-item short form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. [DOI] [PubMed]
- 16.Petersen TL, Engh GA. Radiographic assessment of knee alignment after total knee arthroplasty. J Arthroplasty 1988;3:67-72. [DOI] [PubMed]
- 17.Robertsson O, Dunbar M. Patient satisfaction compared with general health and disease-specific questionnaires in knee arthroplasty patients. J Arthroplasty 2001;16:476-82. [DOI] [PubMed]
- 18.Anderson JG, Wixson RL, Tsai D. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 1996;11:831-40. [DOI] [PubMed]
- 19.Mahaluxmivala J, Bankes MJK, Nicolai P, et al. The effect of surgeon experience in component positioning in 673 press fit condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty 2001;16:635-40. [DOI] [PubMed]