Patients presenting to surgical clinics with rectal strictures are uncommon. Diagnostic evaluation is carried out with the purpose of differentiating them from the common causes of rectal stricture (including inflammatory bowel disease and malignant disease). There are few reports describing rectal stricture as a late complication of chronic proctitis associated with lymphogranuloma venereum (LGV) infection. We present a case of a patient with a rectal stricture caused by LGV to illustrate the diagnostic approach and treatment of this rare condition.
Case report
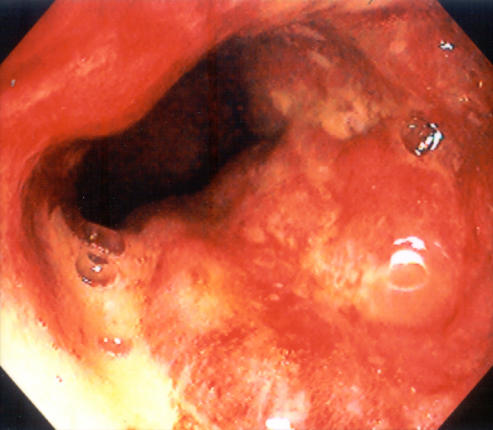
A 45-year-old man was referred to our surgical clinic for investigation of rectal bleeding and anal discomfort. His medical history indicated he was HIV positive. His CD4 count was 360 × 106/L and his viral load was undetectable. No abnormalities were found on perianal inspection. Digital rectal examination revealed a mass-like lesion with some irregularity producing a circumferential stricture. Rigid sigmoidoscopy showed a mass in the distal rectum. Colonoscopy showed a rectal stricture extending from 11 cm to 8 cm from the anal verge (Fig. 1). The scope could pass through the stricture. Although this was not a fibrotic stricture, the circumferential nature of the lesion created a strictured appearance. The remaining colon and ileum were endoscopically normal. Biopsy specimens of the stricture showed ulceration superimposed on an atypical lymphoid infiltrate. There was mild to moderate acute and chronic inflammation in the lamina propria with no evidence of dysplasia or malignancy and no indication of cytomegaloviral infection on immunohistochemical stain. Blood measurements were noncontributory. Pelvic MRI showed diffuse, up to 3 cm, thickening of the rectum for a distance of 10 cm from the anal verge. The MRI scan favoured an inflammatory process over a malignant lesion in view of the long segment of involvement and inflammatory changes. The infectious disease service was consulted, and because LGV was suspected clinically he was started on doxycycline. Serologic examination confirmed LGV. A follow-up colonoscopy was performed at 5 weeks, which showed near resolution of the stricture, and another colonoscopy at 6 months showed complete resolution (Fig. 2).
FIG. 1. Colonoscopy showed an irregular, circumferential rectal stricture. The stricture started 11 cm from the anal verge and extended distally for a distance of 3 cm.

FIG. 2. Colonoscopy 6 months after treatment with doxycycline shows complete resolution of the rectal stricture.
Discussion
LGV is an emerging and significant public health concern in western Europe and recently in Canada.1,2 It is a sexually transmitted infection caused by Chlamydia trachomatis. LGV proctitis is often mild, but chronic cases can be associated with serious complications. If LGV is misdiagnosed or partially treated, the natural history of chronic long-lasting inflammation of the rectum may include the development of fissures, perianal abscess and strictures of the rectum.3,4 Some patients have undergone anterior resection for a presumed malignant lesion only to have the diagnosis of LGV established after histologic examination of the specimen.3,5 Ideally, diagnosis should be made before initiating specific treatment. However, in certain circumstances, the initiation of antibiotic treatment based on clinical suspicion may be appropriate. This case demonstrates that appropriate treatment with doxycycline1 in suspected cases of LGV can result in remarkable improvement and even resolution of rectal strictures.
Although this disease is rare, LGV should not be forgotten in the differential diagnosis of rectal problems including rectal strictures. In view of the increasing incidence of LGV in the West, it is important for physicians to be acutely aware of LGV proctitis in high-risk patients.
Competing interests: None declared.
Accepted for publication July 21, 2006
Correspondence to: Dr. Martin Friedlich, Ottawa Hospital — General Campus, Rm. 2003 Eye Institute, Ottawa ON K1H 8L6; fax 613 739-6646; mfriedlich@ottawahospital.on.ca
References
- 1.Kropp RY, Wong T. Emergence of lymphogranuloma venereum in Canada. CMAJ 2005;172:1674-6. [DOI] [PMC free article] [PubMed]
- 2.Nieuwenhuis RF, Ossewaarde JM, Gotz HM, et al. Resurgence of lymphogranuloma venereum in western Europe. Clin Infect Dis 2004;39:996-1003. [DOI] [PubMed]
- 3.Papagrigoriadis S, Rennie JA. Lymphogranuloma venereum as a cause of rectal strictures. Postgrad Med J 1998;74:168-9. [DOI] [PMC free article] [PubMed]
- 4.Ruther U, Rupp W, Muller HA, et al. Rectal pseudotumor due to Chlamydia trachomatis in a male homosexual. Endoscopy 1990;22:237-8. [DOI] [PubMed]
- 5.Parkash S, Radhakrishna K. Problematic ulcerative lesions in sexually transmitted diseases: surgical management. Sex Transm Dis 1986;13:127-33. [DOI] [PubMed]