Abstract
Objective
Lumbar microsurgical discectomy was traditionally done as an inpatient procedure, but over the last decade, there has been an ever-expanding shift toward outpatient lumbar microdiscectomy (OLM). We have been performing OLM since 1997 (MB) and 2002 (EMM), but no study of patient satisfaction has been carried out to date. the objective of our study was to investigate patient satisfaction with the experience
Methods
Between September 2004 and March 2005, we carried out a qualitative case study at Toronto Western Hospital, involving interviews with 28 patients who had recently undergone OLM. The protocol was approved by the institutional Research Ethics Board, and informed consent was obtained from each participant. Interviews were transcribed and stored anonymously and subjected to modified thematic analysis by 5 reviewers.
Results
Analysis of the interviews yielded several overarching themes: 1) patients are surprised that back surgery can be done on an outpatient basis; 2) the amount and quality of information they receive is satisfactory; 3) the overall experience is positive; 4) trust in one's surgeon is important; and 5) some patients have significant back pain in the early postoperative period.
Conclusions
Most patients appreciate the need for the health care system to save money where possible so that it can be spent in other, more resource-intensive areas. Outpatient lumbar microdiscectomy satisfies this goal while retaining high patient satisfaction rates. Qualitative research can yield substantial insight, which will improve the experience for future patients. Qualitative research is rare in the surgical literature and can answer questions quantitative research methods cannot.
Abstract
Objectif
La discectomie microchirurgicale lombaire est habituellement pratiquée en service interne, mais on constate depuis dix ans un virage de plus en plus important vers la microdiscectomie lombaire en service externe (MLE). Nous pratiquons des MLE depuis 1997 (MB) et 2002 (EMM), mais il ne s'est fait jusqu'à maintenant aucune étude sur la satisfaction des patients. Notre étude visait à déterminer la satisfaction des patients à l'égard de l'expérience.
Méthodes
Entre septembre 2004 et mars 2005, nous avons procédé, à l'Hôpital Toronto Western, à une étude de cas qualitative à partir d'entrevues auprès de 28 patients ayant subi récemment une MLE. Le conseil d'éthique de la recherche de l'établissement a approuvé le protocole et on a obtenu le consentement éclairé de chaque participant. Les entrevues ont été transcrites et mémorisées anonymement et soumises à une analyse thématique modifiée par cinq examinateurs.
Résultats
L'analyse des entrevues a dégagé plusieurs thèmes dominants : 1) les patients sont étonnés que l'on puisse pratiquer une intervention chirurgicale au dos en service externe; 2) le volume et la qualité de l'information qu'ils reçoivent sont satisfaisants; 3) l'expérience globale est positive; 4) il est important d'avoir confiance dans le chirurgien; 5) certains patients ont une douleur importante au dos au début de la période postopératoire.
Conclusions
La plupart des patients comprennent que le système de santé doit épargner de l'argent dans la mesure du possible afin de pouvoir le consacrer à d'autres domaines qui consomment davantage de ressources. La microdiscectomie lombaire en service externe atteint ce but tout en maintenant des taux élevés de satisfaction chez les patients. La recherche qualitative peut produire des aperçus importants qui amélioreront les expériences des patients à venir. La recherche qualitative est rare dans les publications chirurgicales et peut éclairer des questions auxquelles les méthodes de recherche quantitatives ne peuvent répondre.
Qualitative research has value for investigating complex and sensitive issues because it allows the exploration of previously unforeseen lines of inquiry.1–3 It can help examine patients' experience and can address questions that quantitative methods cannot. Specifically, interviews contain narrative information that is simply not available when other methods of inquiry are used. Qualitative research has not traditionally been an integral part of the surgeon's research armamentarium, and most surgeons are relatively unfamiliar with its methods and uses.
Although information on outcomes after outpatient lumbar microdiscectomy (OLM) is available from questionnaires,4,5 the literature is virtually devoid of reports on patients' perspectives, acceptance of the procedure and satisfaction in the peri-and early postoperative periods. The present investigation aimed to determine patient satisfaction with OLM and attempted to assess potentially hidden human costs arising from discharge the same day as surgery, which are not addressed by other research methods. This study is unique in its objective of analyzing a previously undocumented domain of the human experience in ambulatory neurosurgery.
Over the past few decades nearly every branch of surgery has been drifting toward less invasive, shorter procedures that maximize safety and cost-effectiveness. Some of the well-established outpatient procedures include cardiac angioplasty, carpal tunnel release and other peripheral nerve surgery and surgery for bladder disorders.6 With the advent of improved drugs and techniques for general anesthesia and less invasive approaches (such as the microsurgical approach to discectomy, developed almost 3 decades ago, and newer innovations such as the tubular retractor method that results in less dissection through the muscles)7 neurosurgery has become more heavily invested in outpatient surgery.6,8 However, neurosurgeons have not yet universally adapted such procedures as lumbar microscurgical discectomy to ambulatory outpatients.9 It therefore remains an ongoing challenge to identify and analyze any implicit consequences, both beneficial and harmful, to patients receiving innovative and cost-effective procedures such as OLM.6,8,10–17
Methods
Design
The present study was a qualitative case study using interviews with patients who had recently undergone OLM.
Setting and participants
Patients were sought from the practices of 2 neurosurgeons (MB, EMM). Care was relatively uniform except for the details of surgery. One surgeon (MB) used the “traditional” microsurgical discectomy method, whereas the other (EMM) used the muscle-splitting technique with tubular retraction. All participants were invited to participate in the interviews 5–8 weeks postsurgery, after their first follow-up visit to the surgeon. Informed consent was obtained. Those who remained in the hospital overnight and those who could not communicate freely in English were excluded. Neither surgeon routinely offers overnight admission to ambulatory lumbar microdiscectomy patients, and no conversions to inpatient status occurred during the study period. Consecutive patients in both surgeons' practices were invited to participate in this study.
Sample size
We sought 28 interviews with eligible patients. This sample size was selected because previous qualitative studies suggest that thematic saturation levels are reached approximately at or before this number of interviews.1–3,18–20 Saturation in qualitative research refers to the concept that, at some point, successive interviews will not yield any new concepts beyond the ones that have already emerged.
Data collection
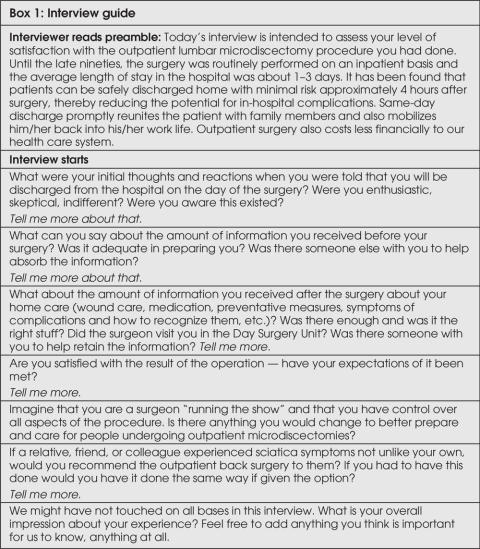
Open-ended, face-to-face interviews with postoperative patients about their levels of satisfaction were conducted over the course of 6 months. An interview guide was followed, but the interviews remained fluid enough for emerging themes to be captured as they arose (Box 1). Interviews were carried out by a third party (MH) who was at the time an undergraduate neuroscience student and not a health care provider in the patients' treatment process. All interviews were audiotaped and transcribed. Demographic parameters were obtained for each patient.
Box 1.
Data analysis
The data were examined through modified thematic analysis consisting of open and axial coding. In the former, the data were read and fragmented into groups of related concepts that alluded to the same main idea. In the latter, the dominant ideas that emerged were organized into overarching themes.2,3 The transcriptions were reviewed by the 3 principal investigators and 2 observers, who all contributed to developing the coding framework. Finally, as a “member check,” a draft of the results was sent to a small subset of study participants (specifically, 2 patients: the fifth and fifth-last patients interviewed) to verify the reasonableness of the findings.
Research ethics
Participation was entirely voluntary, and informed consent was obtained. Confidentiality and the freedom to withdraw from the study were ensured, and all audiotapes and transcriptions were rendered anonymous and kept in a secure location. The investigation was approved by the Research Ethics Board of the University Health Network.
Results
Patient information
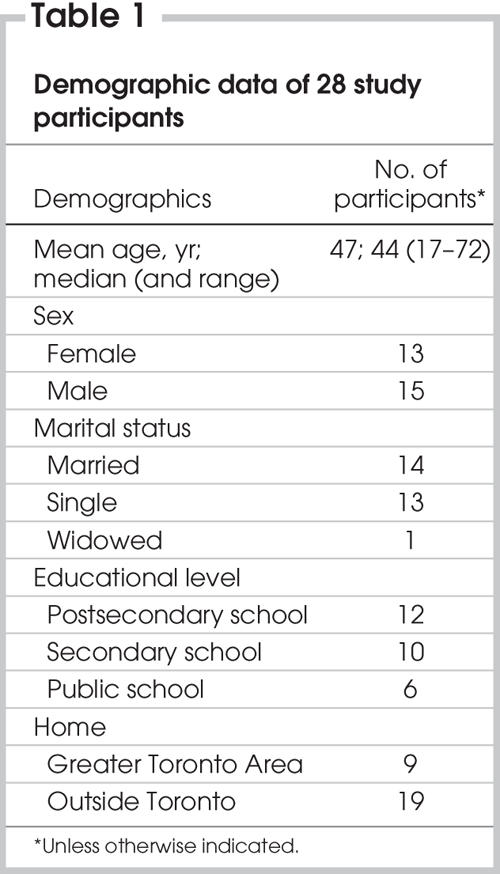
Twenty-eight consecutive eligible patients were interviewed over a 6-month interval between September 2004 and March 2005. No patient approached declined to participate. The demographic data for 28 patients who completed the study are displayed in Table 1.
Table 1
Thematic analysis
The predominant sentiments that emerged from the 28 interviews were positive in that most patients reported they would change very little about the process. Certain narrative remarks indicated minor unsatisfactory experiences, but these were overshadowed by the positive feelings about the benefits of outpatient surgery. The interviews yielded a rich assortment of material, which we condensed into 5 overarching themes. The main themes are presented in order of descending importance to the patients. The themes are based on their narratives and illustrated by verbatim quotes from participant interviews.
The overall experience was satisfactory
The predominant theme that emerged was satisfaction with the overall experience. Patients expressed eagerness to leave the hospital and recuperate at home under the care of family members. Most were very pleased with the coordination of all aspects of their care on the day of the surgery. A major facet of patient satisfaction was that each department ran in a timely and efficient manner. The vast majority of patients felt that outpatient surgery optimized the experience for everyone involved, including patients, relatives and hospital staff. Over 90% would undertake the same course of action and would again willingly choose to be discharged the same day. The comfort of one's own home and familiar faces and surroundings were preferred to the fast-paced, impersonal hospital environment. (“I'm home, then I'm in my own bed, I'm in my own environment. … I just know that, for me, I would heal faster.” “Considering the way hospitals are run now, with lack of staff … I wouldn't be given the attention that I got at home.”) The few patients who expressed a preference for an overnight stay recollected significant postoperative pain and nausea as grounds for their desire to stay longer.
The quality and amount of patient education was adequate
Patients reported that the information provided to them before and after surgery was all-encompassing. The combination of written information and verbal instructions from the surgeon and nurses was considered thorough. Most patients appreciated the written reference material (i.e., a booklet) after discharge. (“The information … was on a printout and it was very explicit. It didn't leave any questions.” “Printed information is excellent, provided it goes along with some verbal explanation.”)
The presence of an accompanying relative on the day of the surgery provided another opportunity for information retention. In some instances, patients rely on their spouses or children to comprehend all that is said as they themselves take a less involved, passive approach. Some patients did state that it was difficult to retain all the information presented to them and noted specific examples of gaps in information provided. (“I don't recall hearing much detail, you know, that it might be a kind of tough ride home.”)
Patients were surprised at the possibility of outpatient back surgery
Most patients were not aware of OLM, although they had heard about other types of surgery being preformed as ambulatory procedures. Many described their immediate reaction as a mixture of shock, skepticism and, eventually, relief.
Same-day discharge precipitated 1 of 2 common responses: for most, it alleviated anxiety and lessened their fears; for some, it caused apprehension. Most began to perceive the procedure as less fearsome than an inpatient procedure might be. (“I was very excited about the fact that it was day surgery … how could you possibly have major or invasive surgery if you are not being kept in the hospital?”) Many felt reassured that swift discharge indicated a reliably positive prognosis for their postoperative condition. (“I think a lot of people equate time in the hospital as to the severity of what is now to transpire with the operation.”) In some instances, the news caused mild alarm based on the widespread belief that one is always safer in the care of hospital staff (i.e., being admitted to the hospital ensures that an unexpected detrimental outcome can be taken care of promptly). In some cases, this perception was apparently perpetuated by the patients' next of kin and acquaintances, some of whom had had spinal surgery as inpatients in the past. (“It's major surgery so you don't know how you're going to recover and how do they know within 4 hours that you're going to be fine? … It was really scary to … start walking around and really not knowing what to expect.” “For surgery of that nature I didn't think that it was possible that the hospital would allow a discharge on the same day and I was just afraid of the complications.”)
Trust in one's surgeon was important
Most patients stated that they believed their surgeon was competent and trustworthy. It appears that the surgeon's endorsement of the safe nature of the outpatient procedure played a key role in dissipating patient fears and misgivings. For example, most patients reported that they would undergo the same surgery if it were needed and if it were preformed by the same surgeon. (“We were comfortable with that based on the doctor's approval … it's going to be okay, it's a one day thing ... .”) The nurses' roles in the day-surgery unit are also vital in diminishing patient stress before the operation. A patient-friendly environment in which questions are met in a receptive and reassuring atmosphere contributes to overall trust in the system. (“I was really nervous before the operation, but coming in and everybody explaining stuff to me the day of the surgery … as they were wheeling me in, I was totally comfortable.”)
Postoperative pain was an issue
In the vast majority of patients, a pronounced improvement in or elimination of sciatica pain was reported. Most patients complained of nausea and immediate postoperative discomfort ranging from mild to severe pain at the incision site. Patients undergoing general anesthesia for the first time were more distraught by the emetic side effects of anesthetic drugs (“the pain went out of my leg that same day … all I had to do was concentrate on the healing process of the wound”). The physical strain of commuting from the hospital to the patient's home caused significant discomfort in some, especially among out-of-town patients. (“There is an element of pain walking to the car and getting into the car and being comfortable driving back, and I had a two-hour drive … but still I would rather do that than stay overnight.”)
Discussion
The role of elective OLM for the treatment of severe sciatica refractory to medical management is to relieve suffering and to lead to a significant positive effect on patients' quality of life. Outcome studies and standard quantitative analysis demonstrate that OLM is not only resource-friendly but also effective. Standard outcome instruments such as the Medical Outcomes Study 36-item Short Form and the Prolo Scale demonstrate positive patient health outcome in most patients after microsdiscectomy.9 Our study examined the patient's perspective and experience with OLM, using qualitative research methodology. Our focus was to provide better insight into the experience from the patient's perspective and to examine issues that are not amenable to ex-ploration by quantitative research methodology.
Qualitative research is subjective and does have inherent weaknesses. It may seem awkward and weak to most quantitatively oriented surgeons. The framework for analyzing patient satisfaction in a qualitative study may be too narrow. Themes are generated from previous patient encounters and observations and provide the basis for appropriate questions to be asked in the interviews. However, this approach, which is coloured by biases and preconceptions on the part of the researchers, (neurosurgeons in this case) may provide too narrow a scope for patients to express views on a wide range of topics and issues. Generally speaking, a combination of structured questions and an open-ended format allows maximal retrieval of relevant information.
Another weakness of qualitative research is the subjectivity of the thematic analysis. This can be mitigated but not totally removed by ensuring that there are multiple reviewers from different backgrounds and by obtaining a member check, that is, a review of the findings by a subset of study participants.
The findings in this study revealed high patient satisfaction with OLM. They also revealed that patients do not absorb all information given to them by the surgeon and nurses and that information retention is highly variable among individuals of different backgrounds (which include social, ethnic, cultural, educational and other nonclassifiable factors). Gaps in understanding regarding any aspect of a patient's care can cause significant but easily avoidable distress for some.
As a result of our findings, we recommend 3 possible useful strategies that could be advantageous in engaging and educating patients who may be reluctant or anxious to participate in outpatient neurosurgery. First, provide a list of former patient volunteers who are willing to freely and voluntarily share their experience; second, offer an optional, nurse-escorted tour of the day-surgery facilities; and third, create a patient-centred DVD guide repeating all verbal instructions and illustrating the procedure by means of an animated film.
A survey of the last one-third of study participants revealed that all patients supported the creation of a directory of former patients' contact numbers. Further, all patients agreed that they would not oppose having their name included in this prospective external support system scheme. Because the concept is vulnerable to individual subjective recollections and idiosyncratic experience bias, discretion is needed in the inclusion criteria for such a support system.
The present study revealed that, compared with lengthier in-hospital stays, outpatient microdiscectomy is subjectively favoured by the vast majority of patients and that, by and large, patient satisfaction was high. Perhaps the most important lesson arising from this study is that improved information is needed for future patients during the preoperative decision-making process, on the day of surgery and in the postoperative course.
In our present environment of reduced resources, understanding the full impact of interventions such as OLM, including impacts on efficiency and patient satisfaction, will not only help inform future research but possibly redirect resources to areas in need of improvement, such as patient education.
Acknowledgments
We thank Diane Cartwright and Mary Heenan for their help analyzing the interviews, the day surgery nurses for all their help caring for the patients and all the patients who graciously participated.
Competing interests: None declared.
Accepted for publication Mar. 13, 2006
Correspondence to: Dr. Mark Bernstein, Toronto Western Hospital, 399 Bathurst St., 4W451, Toronto ON M5T 2S8; fax 416 603-5298; Mark.Bernstein@uhn.on.ca
References
- 1.Sheldon L. Grounded theory: issues for research in nursing. Nurs Stand 1998;12:47-50. [DOI] [PubMed]
- 2.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks (CA): Sage Publications; 1998. p. 55-242.
- 3.Yin RK. Case study research: design and methods. 2nd ed. Thousand Oaks (CA): Sage Publications; 1994.
- 4.Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75-80% success rate be the norm? J Neurosurg Spine 2002;96:34-44. [DOI] [PubMed]
- 5.Ljubicic Bistrovic I, Ljubicic D, Ekl D, et al. Influence of depression on patients satisfaction with the outcome of microsurgical “key-hole” vs classical discectomy: prospective matched-cohort study. Croat Med J 2002;43:702-6. [PubMed]
- 6.Bhattacharyya AK, Bernstein M. Outpatient neurosurgery: state of the art, feasibility, and relevance. Advances in Clinical Neurosciences 2003;13:15-26.
- 7.Obenchain TG. Speculum lumbar extraforaminal microdiscectomy. Spine J 2001;1:415-20. [DOI] [PubMed]
- 8.Singhal A, Bernstein M. Outpatient lumbar microdiscectomy: a prospective study in 122 patients. Can J Neurol Sci 2002;29:249-52. [DOI] [PubMed]
- 9.Thome C, Barth M, Scharf J, et al. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. J Neurosurg Spine 2005;2:271-8. [DOI] [PubMed]
- 10.An HS, Simpson JM, Stein R. Outpatient laminotomy and discectomy. J Spinal Disord 1999;12:192-6. [PubMed]
- 11.Bednar DA. Analysis of factors affecting successful discharge in patients undergoing lumbar discectomy for sciatica performed on a day-surgical basis: a prospective study of sequential cohorts. J Spinal Disord 1999;12:359-62. [PubMed]
- 12.Bookwalter JW, Busch MD, Nicely D. Ambulatory surgery is safe and effective in radicular disc disease. Spine 1994;19:526-30. [DOI] [PubMed]
- 13.Lorish TR, Tanabe CT, Waller FT, et al. Correlation between health outcome and length of hospital stay in lumbar microdiscectomy. Spine 1998;23:2195-200. [DOI] [PubMed]
- 14.McLain RF, Kalfas I, Bell GR, et al. Comparison of spinal and general anesthesia in the lumbar laminectomy surgery: a case controlled analysis of 400 patients. J Neurosurg Spine 2005;2:17-22. [DOI] [PubMed]
- 15.Scanlon J, Richards B. Development of a same day laminectomy program. J Perianesth Nurs 2004;19:84-8. [DOI] [PubMed]
- 16.Shaikh S, Chung F, Imarengiaye C, et al. Pain, nausea, vomiting and ocular complications delay discharge following ambulatory microdiscectomy. Can J Anaesth 2003;50:514-8. [DOI] [PubMed]
- 17.Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine 1978;3:175-82. [PubMed]
- 18.Bernstein M, Potvin D, Martin DK. A qualitative study of attitudes toward error in patients facing brain tumour surgery. Can J Neurol Sci 2004;31:208-12. [DOI] [PubMed]
- 19.Martin DK, Singer PA, Bernstein M. Access to intensive care unit beds for neurosurgery patients: a qualitative case study. J Neurol Neurosurg Psychiatry 2003;74:1299-303. [DOI] [PMC free article] [PubMed]
- 20.McKneally MF, Martin DK. An entrustment model of consent for surgical treatment of life-threatening illness: perspective of patients requiring esophagectomy. J Thorac Cardiovasc Surg 2000;120:264-9. [DOI] [PubMed]