Abstract
Objective
To characterize the common injuries incurred by elderly trauma victims and to identify the most frequent complications and outcomes.
Methods
We undertook a retrospective descriptive chart review of 125 consecutive patients who were over age 65 years and who were admitted to an academic hospital in Kingston, Ontario, over a 3-year period with an injury severity score (ISS) > 12. Complete data about the mechanism of injury (MOI), age, date, sex, specific injury, principal and secondary diagnoses, comorbid conditions, intensive care unit (ICU) and hospital length of stay and discharge disposition were recorded for 99 of these patients.
Results
Elderly trauma cases accounted for 125 of the total 460 trauma admissions over 3 years. For that same period, more than 50% of trauma deaths occurred among elderly patients, of whom 65 were men and 34 were women. Their mean age was 77 (standard deviation [SD] 6) years, with an age range of 66–95 years. The average ISS score was 23 (SD 13), with a range of 12–75. MOI included falls (64%), motor vehicle collision (27%), injury from machinery (3%), injury from natural and environmental causes (2%), suicide or self-inflicted injury (3%) and burns (1%). The mean length of stay was 14.6 days, but this ranged from 1 to 111 days. Of the 99 patients, 14 were admitted to the ICU for a total of 37 days, and 9 of these died. Of the total of 67 (67%) patients who were discharged from hospital, 46% were discharged home and 32% died. Falls accounted for the most frequent MOI, followed by motor vehicle collisions. The most common injury in the falls group was subdural hematoma, whereas fractures were the most common injuries in the motor vehicle collision group. The most frequent complications included urinary tract infections and aspiration pneumonias. Neither age nor MOI was correlated with injury severity. Increasing age and injury severity were predictors for complications and mortality while in hospital.
Conclusions
Despite severe injuries, most elderly patients can survive traumatic injuries. The data suggest that, although elderly patients are prone to incur complications and have greater risk of dying as a result of their injuries, most of these patients will survive their traumatic accidents. The data also show that nosocomial complications play a significant role in the risk of mortality in elderly trauma victims.
Abstract
Objectif
Caractériser les traumatismes souvent subis par les personnes âgées et déterminer leurs complications et leur issue les plus fréquentes.
Méthodes
Étude descriptive rétrospective des dossiers de 125 patients consécutifs de 65 ans ou plus admis dans un hôpital universitaire à Kingston (Ont.), au cours d'une période de trois ans, et dont l'indice de gravité de la blessure (IGB) dépassait 12. On a consigné pour 99 de ces patients des données complètes sur le facteur mécanique traumatisant (FMT), l'âge, la date, le sexe, le traumatisme précis, les diagnostics principal et secondaire, les affections comorbides, la durée du séjour aux soins intensifs (SI) et à l'hôpital et l'issue au moment du congé.
Résultats
Parmi les 460 traumatisés admis en trois ans, il y avait 125 personnes âgées. Au cours de la même période, plus de 50 % des décès de traumatisés sont survenus chez les patients âgés, qui comptaient 65 hommes et 34 femmes. Les patients avaient en moyenne 77 (écart-type [ET] 6) ans, pour une plage de 66 à 95 ans. L'IGB moyen s'établissait à 23 (ET 13), pour une plage de 12 à 75. Les facteurs mécaniques traumatisants comprenaient les chutes (64 %), les accidents de la circulation (27 %), les traumatismes causés par des machines (3 %), les traumatismes attribuables à des causes naturelles et environnementales (2 %), les suicides ou traumatismes auto-infligés (3 %) et les brûlures (1 %). La durée moyenne du séjour s'établissait à 14,6 jours mais elle a varié de 1 à 111 jours. Des 99 patients, 14 ont été admis aux SI, pour un total de 37 jours, et 9 sont décédés. Des 67 (67 %) patients qui ont quitté l'hôpital, 46 % sont retournés à la maison et 32 % sont décédés. Les chutes ont constitué le facteur mécanique traumatisant le plus fréquent, suivies des accidents de la circulation. L'hématome sous-dural a constitué le traumatisme le plus fréquent chez les victimes de chutes, tandis que les victimes d'accidents de la circulation ont subi surtout des fractures. Les infections urinaires et les pneumonies d'aspiration constituaient les complications les plus fréquentes. On n'a pas établi de lien entre l'âge ou le facteur mécanique traumatisant et la gravité du traumatisme. L'âge croissant et la gravité du traumatisme étaient des prédicteurs de complications et de mortalité pendant le séjour à l'hôpital.
Conclusions
En dépit de blessures graves, la plupart des patients âgés peuvent survivre à des traumatismes. Les données indiquent que même si les patients âgés sont fragiles aux complications et risquent davantage de mourir des suites de leurs blessures, la plupart survivront au traumatisme. Les données montrent aussi que les complications nosocomiales jouent un rôle important dans le risque de mortalité chez les personnes âgées victimes d'un traumatisme.
The resources required for the management of patients admitted to hospital is a constant concern for many levels of hospital staff and administration. Although the medical demands of patients admitted for elective procedures can be accommodated ahead of time, patients who require admission in an emergent setting and patients who are the victims of trauma can place unpredictable demands on hospital personnel and medical resources. Elderly trauma victims further complicate these medical demands by frequently arriving with a larger number of comorbid conditions than individuals in other age groups; they also have a decreased ability to tolerate severe injury for long periods of time.1,2 Previous studies have shown that, although this subgroup represents a smaller proportion of traumas, these patients require a disproportionate amount of hospital resources.3 However it has also been shown that elderly victims who survive the initial traumatic event can regain much of their previous level of functioning.4
As the number of people over the age of 65 years begins to increase in the population, the proportion of injuries that occur among these individuals, who are then cared for as hospital inpatients, will also be expected to increase.5 In the future therefore, resource managers and caregivers will benefit from an understanding of the medical resources commonly required by these individuals. Although studies to compare injury types and severity, complications and morbidity have been conducted in larger US centres, few Canadian studies have been published to date that describe the causes of traumatic injury to elderly individuals and the medical consequences of these injuries.6 Further, no studies have been done to profile similar accidents in a Canadian city the size of Kingston, Ontario.
Through this retrospective study, we aimed to determine the most common mechanisms of injury in elderly trauma patients in this setting and to identify the most common injuries for a particular mechanism of injury. By describing this group of patients, our objective was to profile the common age, sex, comorbidities, complications and range of injury severity incurred by this population of trauma patients for comparison with other age groups. Inferences can be also drawn from these data to develop prevention strategies for specific types of injuries as well as to increase understanding of the necessity for rehabilitation in this age group. Our findings will also be useful to health care practitioners and health care planners preparing for an aging population in which these interventions will become more frequent.
This study asks the following 3 questions: What are the most common mechanisms and patterns of injury experienced by elderly trauma victims? What are the complications that result from these injuries? How do increasing age, injury severity and complications influence outcomes experienced by elderly trauma victims?
Methods
This retrospective descriptive study took place at Kingston General Hospital, a tertiary care hospital in southeastern Ontario with a catchment area of about 400 000. Located in the town of Kingston (population 115 000), it is a teaching hospital of Queen's University. A search of the trauma database identified 125 subjects who were over age 65 years and who met the criteria of a trauma patient (injury severity score [ISS] > 12) on admission. Patients were selected for a 3-year period from Mar. 31, 2000, to Apr. 1, 2003. Data were collected from 3 sources: the trauma database, the computerized patient records and the patient charts. The mechanism of injury (MOI), injury type, age and ISS scores were available for all 125 admissions over this 3-year period.
Detailed computerized records were available for 99 of these trauma patients. These data included age, sex, admission date, diagnoses, complications, discharge disposition and mortality. The definitions of the principal diagnosis, complications and comorbidities are based on the International Classification of Diseases, 9th revision (ICD-9) classification system.7 We used descriptive statistics to analyze the data. When applicable, means were tested according to Student's t test. Approval for this research was obtained from the hospital's ethics committee.
Results
Trauma demographics
In the 3 years between Mar. 31, 2000, and Apr. 1, 2003, there were 125 trauma victims over age 65 years with ISS scores of > 12, out of a total of 460 trauma victims (27%).
The injuries sustained by these individuals were classified into 6 categories: falls, motor vehicle collision (MVC), suicide or self-inflicted injury, burns, machinery or naturally caused injuries. Falls were the most frequent injuries and accounted for 64% of all trauma admissions in this age group. MVCs were the next most common and accounted for 27% of admissions. Machine injuries, natural accidents and suicides made up 3%, 2% and 3%, respectively. Burns were the least frequent cause at 1%. These injury mechanisms remained in the same proportions over the 3-year period. The average injury score on admission was 23 (standard deviation [SD] 13), with a range of 12–75 and a 95% confidence interval (CI) of 23–27.
Age independently had a very poor correlation with the severity score of these elderly patients (p = 0.819). There was also a poor association with each MOI and the severity score. MVC showed the highest correlation, but the association was not statistically significant. If the variables of age, falls and MVCs are combined, they only account for 1.8% of the variation in injury severity (r2), according to multivariate analysis.
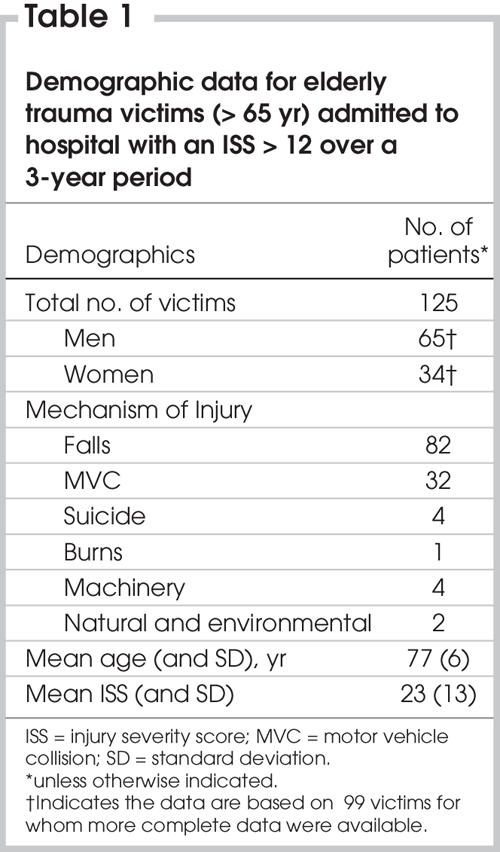
Hospital data
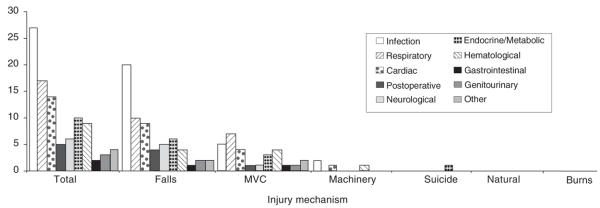
Complete computerized patient records were available for 99 of the 125 patients admitted through the trauma service. The average age of these individuals was 77 (SD 6) years, with a range of 66–95 years. In this age group, traumatic injuries were more frequently incurred by men (65%) than by women (34%) (Table 1).
Table 1
Principal admitting diagnosis
Within each MOI, there was a range of possible specific injuries incurred. If these injuries are grouped by system overall, head injuries accounted for the greatest proportion of principal diagnoses (64%). Thoracic and orthopedic injuries made up 14% and 12%, respectively, of principal diagnoses at the time of admission. Subdural hemorrhages were the most common specific principal diagnosis. Of victims suffering falls (n = 69), subdural hemorrhage (30/69) and hemorrhage without intracranial wound (8/69) were the most frequent principal diagnoses. Other injuries included basal skull fractures (4/69) and cerebral laceration and contusion without intracranial wound (4/69). There were also several principal admitting diagnoses that were not related to the trauma but could be interpreted as the cause of the fall. These included respiratory failure, convulsions, heart failure and heart block. The principal diagnoses as a result of MVCs (n = 20) were mostly related to high-velocity blunt trauma to the torso and extremities and included fractured ribs (2/20) and nonspecific intracranial bleeds (2/20). In total, 9/20 patients had fractures, making orthopedic injuries the most common injuries suffered by elderly patients in an MVC (Fig. 1).
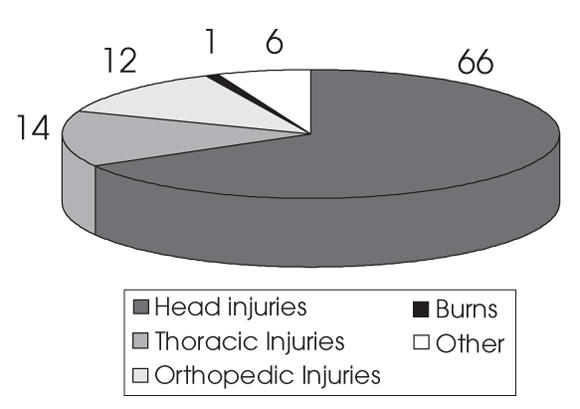
FIG. 1. Distribution of injuries by system in elderly trauma victims (n = 99).
The other MOIs were more specific in regard to principal admitting diagnosis. Machinery injuries involved almost exclusively fractures, self-inflicted injuries most frequently involved penetrating injuries, and burns were most common among those injured by fire and flames.
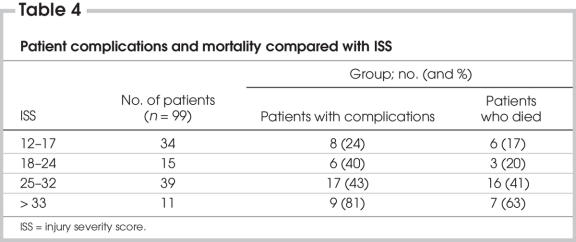
Complications
Of the patients, 41 experienced a total of 97 recorded complications while in hospital as a result of their injuries (Fig. 2); 23 patients suffered from multiple complications. The most common complications were infections and included urinary tract infections (8/97) and pneumonias due to aspiration (6/97). Respiratory failure (4/97) and cardiac complications (4/97) were also common. These complications were mostly limited to patients who had suffered falls or been victims of MVCs. Those patients who suffered injury by machinery, burns, natural accidents or suicide attempts experienced relatively few complications. There were very few of these patients, and the mortality associated with burns and suicide was also quite high, which may account for the low number of complications in these patients. Of patients who suffered complications, 41% died. The mean age of patients who suffered complications was 79.35 years, which is statistically significant when compared with trauma victims who did not encounter complications (76.64 yr) (p = 0.036). The MOI, however, is not a statically significant predictor of complication. The odds ratio (OR) of experiencing a complication in this population increases 1.08 at a 1-year interval; thus, for every 10 years of age, the risk of complications is 10.75 times higher. Further, patients who experienced complications were more likely to die (OR 2.63, 95% CI 1.11–6.24, p = 0.031).
FIG. 2. Complications associated with injury mechanisms. MVC = motor vehicle collision.
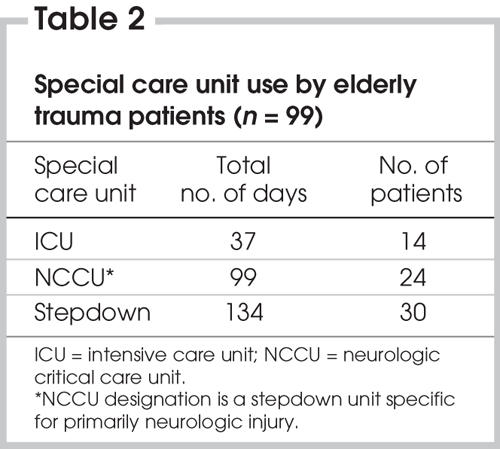
Hospital and intensive care unit length of stay
The mean length of stay in hospital was 14.6 days, but it ranged from 1 to an extreme of 111 days (95% CI 11–17 d). There were 14 patients admitted to the intensive care unit (ICU) for a total of 37 days, 9 of whom died. The total number of ICU days occupied by elderly trauma patients may thus be abbreviated. These patients also used other special care units, such as the neurologic critical care unit (NCCU) and step-down units (Table 2). No patients were admitted to multiple units during their recovery.
Table 2
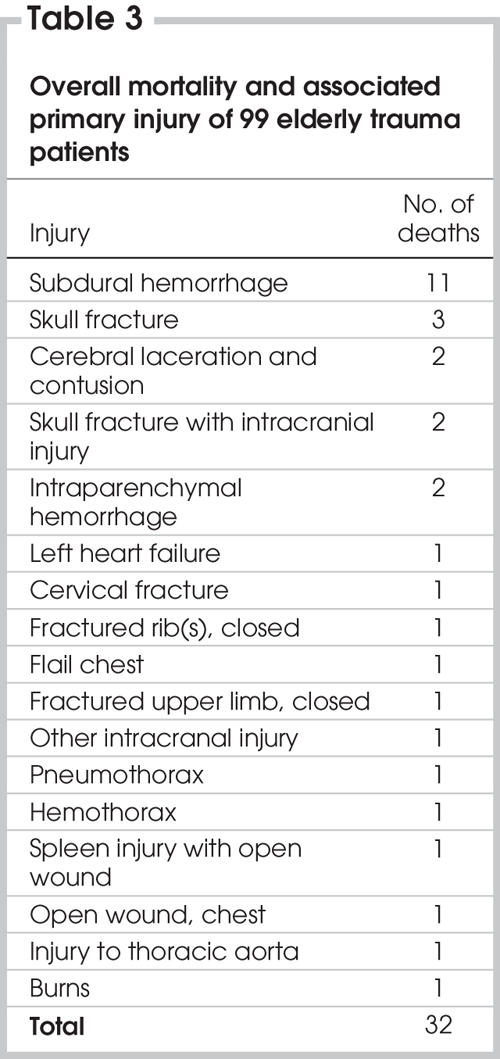
Patient outcomes
Of the 99 elderly trauma patients admitted to hospital, 32 died while in hospital. In total, 61 deaths were due to trauma over the 3-year period, making elderly trauma a disproportionate contributor to trauma deaths. Falls constituted the MOI with the most frequent deaths; however, falls also made up the highest proportion of injuries overall. In actuality, 35% (7/20) of MVC victims died, compared with 33% who suffered falls (23/69), 100% who suffered burns (1/1) and 25% who attempted suicide (1/4). Therefore, although MVCs and falls proved to be almost equally lethal, falls were about 3 times more common. The principal admitting diagnosis with the highest mortality was subdural hemorrhage (Table 3).
Table 3
The ISS scores of patients who died, compared with patients who survived, were statistically significant (means were 30.1 and 23.3, respectively, p = 0.007). There were no significant differences in the means of their ages. If patients are subdivided according to injury severity (Table 4), patients with higher ISS scores had more associated complications and higher mortality (p < 0.001). There is also a definite association between (higher ISS × complications) and mortality (p = 0.004).
Table 4
Sixty-seven patients (67%) were discharged from hospital to another care facility. Destinations included home (31%) or home care (4%), an acute care facility with (5%) or without (11%) psychiatric services, a general rehabilitation hospital (9%), a nursing home (3%) and an ambulatory or chronic care hospital (2%).
Discussion
Elderly patients account for more than 50% of the deaths that result from trauma, even though they make up only 30% of total admissions. Although the elderly suffer from comorbid conditions and limited physiological reserves that may predispose them to die with a less severe injury, a high percentage of elderly patients return to their home. This fact encourages careful analysis of these patients to identify trends in injury patterns and complications that could be avoided, thereby allowing more of these patients to survive their initial injuries.
Elderly trauma demographics
The results of this study demonstrate quite convincingly that the most frequent mechanism of traumatic injury experienced by this patient population is falls, followed by MVCs. Similar data were published by Ferrera and colleagues in a 1-year study of trauma in the elderly carried out at an urban university in the United States.8 Gomberg and colleagues9 also found that compared with younger patients who were more likely to be injured by MVC, older patients were more likely to be injured in a fall. Similar studies in Australia and Japan indicated that elderly trauma victims in these regions were less likely to be injured in collisions involving motor vehicles.10,11 In the United States, Valley and colleagues12 showed that the leading MOIs were in decreasing order, MVCs, falls, and auto–pedestrian injuries. A profile of trauma in Florida also demonstrated the same findings.13 When compared with different age groups, younger and older individuals are also more likely to be involved in MVCs (occupant and pedestrian), suicide and residential fire.14
The reasons that have been suggested for this trend toward injury by falls are based on the physiological changes of aging and the decreases in bone mass, balance and reaction time in elderly patients, which predisposes them to falls.15 The principal admitting diagnoses of seizures respiratory failure and cardiac failure in the elderly patients in this study also indicates that elderly comorbidities can predispose them to trauma. Recently, Bell and colleagues16 studied older patients presenting to the emergency department after a fall. In terms of hospital resource use, 57.2% were admitted to hospital, 48% with a fracture and 52% for investigation of the medical cause of the fall.16 A review by Baker and Harvey17 states that injuries were the sixth leading cause of death in the population aged 75 years and over at the time, with falls being the leading cause of injury-related deaths. This study states that the proportion of fatal falls among patients in nursing homes shows an increase that corresponds to increasing age.
The overwhelming incidence of falls in this population suggests that it should be the primary focus of preventive strategies for the reductions of traumatic injuries in this population. Simple changes to the home environment and safety measures such as assistive walking devices may be underused resources in this population. The implementation of these and other safety measures may have a significant impact in reducing this mechanism as the largest cause of elderly trauma.
Injury patterns
An understanding of the injuries typical of an elderly trauma case can expedite diagnosis, treatment and management. The data on MOI for both falls and MVCs demonstrate that fall victims should be checked for intracranial hemorrhages and other head injuries and that those injured in MVCs should be carefully examined for fractures. A large proportion of fall victims presented with subdural hemorrhages, making them the most prevalent injuries as well as the injuries with the highest mortality. The diagnosis of subdural hematoma is often more problematic in the elderly, compared with younger patients, owing in part to cerebral atrophy and other medical conditions common in the elderly.18 Data from elderly patients who presented with brain injury compared with data from nonelderly patients, demonstrated that elderly patients had increased mortality and worse functional outcome than nonelderly patients who presented with head injury, even though their head injury and overall injuries were seemingly less severe.19
Blunt trauma in the elderly is also associated with high morbidity (23.8%) and mortality (16.8%) rates.20 Elderly patients who sustain blunt chest trauma with rib fractures have twice the mortality and morbidity of younger patients with similar injuries.21 For each additional rib fracture in the elderly mortality increases by 19%, and the risk of pneumonia increases by 27%.21
Complications
In this study, about one-half of the admitted elderly patients had complications. Aspiration pneumonias and urinary tract infections can be considered preventable events during the course of hospital care of the elderly trauma patient. This is in agreement with Rothschild and colleagues,22 who also found that the most common complications were preventable among elderly trauma victims. The high proportion of deaths that occurred among patients who suffered complications emphasizes the point that these patients are physiologically challenged to meet the demands of their injuries. The ages of patients who experienced complications were also statistically higher than the ages of those who did not, which can be interpreted as further evidence of loss of physiological reserve among these individuals.
These facts accentuate the need for close monitoring for these preventable events. The increased risk of mortality among elderly patients who experience complications further strengthens this point. A similar study23 of elderly trauma patients reviewed a large number of data on admission and preadmission as well as on successive complications. Regression analysis revealed that ISS predicted adult respiratory distress syndrome pneumonia, sepsis and gastrointestinal complications; fluid transfusion, transfusion requirements and need for surgery predicted sepsis. These complications, in turn, were significant risk factors for mortality.23 Subgroup analysis in our study also shows that increasing proportions of patients experience complications as ISS increases. Therefore, both age and injury severities play a role in the development of complications among these trauma victims.
Predictive mortality
To reduce mortality associated with elderly trauma and to increase the predictability of patient outcomes, it has been suggested that age should be considered in contemporary scoring systems and treatment algorithms, in addition to the standard severity scores. In this study, the difference in ISS scores of patients who died, compared with patients who survived, was statistically significant, whereas the means of their ages did not differ significantly . This finding is supported by a published study that analyzed the ability to predict death of such diverse variables as age, sex, MOI, admission blood pressure, Glasgow Coma Scale score, respiratory status, Trauma Score, Revised Trauma Score and ISS. It was found that the ISS was the variable that correlated most significantly with mortality.24 Sugimoto and colleagues25 suggest that criteria should be developed specifically for geriatric victims with trauma-induced injuries, given their positive outcomes with aggressive initial management.
Contrary to Knudson and colleagues,24 van der Sluis and colleagues26 state that long-term survival is mainly determined by host factors and not by injury severity in patients with femoral neck fractures. One of the largest comparisons of trauma victims based on age, has revealed several aspects of trauma outcome that vary with a person's age. Elderly (≥ 65 yr) patients had significantly higher mortality rates than younger (< 65 yr) trauma patients after stratification by ISS, Revised Trauma Score and other preexisting comorbidities. A patient age over 65 years was associated with a 2- to 3-fold increased mortality risk in mild (ISS < 15), moderate (ISS 15–29) and severe traumatic injury (ISS ≥ 30), compared with a patient age under 65 years. This study argued that age was an independent predictor of mortality in elderly trauma.5 Thus it is apparent that many contrasting views are presented in the literature.
The data from our study support the view that ISS is a better predictor of mortality than age. In the interpretation of this study's data, it must be emphasized that 11% of the patients suffered severe injury (ISS > 33). Therefore, these data and predictors of complications apply best to injuries of low-to-moderate severity. There are also several other predictive factors related to hospital stay that indicate higher mortality risk. They include admission for an MVC or fall, occurrence of complications and ICU use. However, these hospital factors are also individually influenced by higher injury severity scores; therefore, the higher mortality associated with them may be a result of the severity of the original injury.
Outcomes
It has been shown repeatedly in other studies that the elderly account for a disproportionate number of deaths, compared with the number of admitted trauma victims from other age groups. However, as in this study, growing evidence indicates that, despite having severe injuries, a large proportion of patients who survive their injuries can return home after recovery.6
Once the oldest are stratified by physiological response, such as injury magnitude and psysiologic severity of illness, their outcome parallels that of their younger trauma cohorts.27,28 Day and colleagues29 determined that although age is an important factor in survival after major trauma those who do survive generally return to full activity and independence. Another study concluded that despite tremendous resource use, most trauma patients with prolonged ICU stays can eventually return to varying degrees of functional daily living and independence, although not to preinjury levels.30 Older patients arriving alive and admitted to the hospital following penetrating trauma are as likely to survive as younger patients with injuries of similar severity, but they have longer ICU and hospital stays.1
This longer length of stay may be accounted for by their increased chances of having comorbid conditions.2 These long-term illnesses can severely compromise an elderly trauma victim's ability to compensate for and recover from severe injury. Several studies have concluded that there is a significant association between severe preexisting medical disease as indicated by ASA classification (ASA III-V) and death during admission for trauma.31 Conflicting data suggest that despite higher injury severity and lower survival probability the length of hospital and ICU stays for elderly trauma victims and the percentage of admissions to the ICU were similar, although admittedly, this may be due to higher mortality in elderly patients.32–34 However if they are managed aggressively, patients aged 75 years and older have a favourable long-term outcome that is significantly greater.4
The counter-argument to a high proportion of positive outcomes for the elderly is provided by 2 studies reporting that elderly trauma patients have high mortality and morbidity even with fairly minor or moderately severe injuries and even though they may not require activation of the trauma team on initial assessment.35,36 Bergeron and colleagues37 found that, despite lower indices of injury severity even after comorbidities were taken into account, mortality was still significantly increased in elderly patients admitted to a trauma centre with rib fractures.
Even though the exact proportion of successful outcomes from elderly trauma is a subject of debate, the demand for rehabilitation of this population is of great importance. Although a large proportion of these patients are sent home, they frequently require assistive services such as rehabilitation or home care for the management of their recovery.6 The duration of hospital stay after these injuries is also often influenced by the speed of rehabilitation. Further, adequate rehabilitation in hospital and before discharge decreases the chances of further complications. As this need becomes more apparent, administrative and governmental agencies should be made aware that, with our aging population, further support of these programs will be even more important in the future.
Future studies and prevention
The increased resources required to manage elderly trauma patients in hospital and the significant effect on their life afterwards have made preventive research an important topic in elderly trauma. A 1990 paper38 estimated that total medical care expenditures for unintentional injuries in the elderly population in 1977 might have been over US$2 billion; making some simple estimations the authors suggest that in 1984 the cost might have been as high as US$5 billion. With the elderly injured population constituting an even greater proportion of the trauma population, these figures can only be expected to increase. Although the elderly make up about 12% of the US population, they account for nearly 33% of health care resources expended on traumatic injuries.15 A second population study39 reports that about 39 000 adults aged 65 years and older die from injuries each year in the United States; worldwide, this annual toll is about 946 000 people.
Future studies into this area should therefore concentrate on establishing effective practices for the prevention of these injuries. This study relies on the strength of several tests of statistical significance, based on a sample size of 99 patients. Many of its conclusions, therefore, must be based on inferred trends seen in this data. For a more comprehensive understanding of this patient population, further studies using a larger range of patients should be conducted in multiple geographic locations. Long-term follow-up of these same patients would also be beneficial to assess their long-term mortality and functional status in addition to their immediate discharge disposition. Continuing research to establish a causative mechanism for the high incidence of mortality in this population is also paramount.
Summary
As the number of people over the age of 65 years begins to increase, the proportion of individuals who suffer injuries and who are cared for as hospital inpatients in medical facilities may also be expected to increase. Age alone predicts only the chances of complications, not injury severity or mortality. However, the severity of the injury in an elderly trauma victim is predictive of both complications and mortality. The most common complications may be preventable infectious events that are associated with mortality when they occur. The high incidence of head injuries in this population makes a thorough neurologic investigation paramount for most. In our study, a large proportion of these patients were discharged from hospital, and about one-third were discharged to their homes.
Competing interests: None declared.
Accepted for publication Jan. 9, 2006
Correspondence to: Dr. R. Gowing, Department of Surgery, McMaster University Medical Centre, 1280 Main St. W., Hamilton ON L8S 4L8; robgowing@gmail.com
References
- 1.Roth BJ, Velmahos GC, Oder DB, et al. Penetrating trauma in patients older than 55 years: a case-control study. Injury 2001;32:551-4. [DOI] [PubMed]
- 2.Nagy KK, Smith RF, Roberts RR, et al. Prognosis of penetrating trauma in elderly patients: a comparison with younger patients. J Trauma 2000;49:190-3; discussion 193-4. [DOI] [PubMed]
- 3.Perdue PW, Watts DD, Kaufmann CR, et al. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma 1998;45:805-10. [DOI] [PubMed]
- 4.Battistella FD, Din AM, Perez L. Trauma patients 75 years and older: long-term follow-up results justify aggressive management. J Trauma 1998;44:618-23; discussion 623. [DOI] [PubMed]
- 5.Clark DE, Chu MK. Increasing importance of the elderly in a trauma system. Am J Emerg Med 2002;20:108-11. [DOI] [PubMed]
- 6.Inaba K, Goecke M, Sharkey P, et al. Long term outcomes after injury in the elderly. J Trauma 2003;54:486-91. [DOI] [PubMed]
- 7.National Center for Health Statistics (U.S.) United States. International classification of diseases, 9th revision. Hyattsville (MD): The Center.
- 8.Ferrera PC. Bartfield JM. D'Andrea CC. Outcomes of admitted geriatric trauma victims. Am J Emerg Med 2000;18:575-80. [DOI] [PubMed]
- 9.Gomberg BF, Gruen GS, Smith WR, et al. Outcomes in acute orthopaedic trauma: a review of 130,506 patients by age. Injury 1999;30:431-7. [DOI] [PubMed]
- 10.Gillies D. Elderly trauma: they are different. Aust Crit Care 1999;12:24-30. [DOI] [PubMed]
- 11.Ng W, Fujishima S, Suzuki M, et al. Characteristics of elderly patients presenting to the emergency department with injury. Keio J Med 2002;51:11-6. [DOI] [PubMed]
- 12.Valley VT, Hepp H, DeBehnke DJ, et al. A profile of geriatric trauma in southeastern Wisconsin. Wis Med J 1994;93:165-8. [PubMed]
- 13.Tepas JJ 3rd, Veldenz HC, Lottenberg L, et al. Elderly injury: a profile of trauma experience in the Sunshine (Retirement) State. J Trauma 2000;48:581-4; discussion 584-6. [DOI] [PubMed]
- 14.Wolf ME, Rivara FP. Nonfall injuries in older adults. Annu Rev Public Health 1992;13:509-28. [DOI] [PubMed]
- 15.Wright AS, Schurr MJ. Geriatric trauma: review and recommendations. WMJ 2001;100:57-9. [PubMed]
- 16.Bell AJ, Talbot-Stern JK., Hennessy A. Characteristics and outcomes of older patients presenting to the emergency department after a fall: a retrospective analysis. Med J Aust 2000;173:179-82. [DOI] [PubMed]
- 17.Baker SP, Harvey AH. Fall injuries in the elderly. Clin Geriatr Med 1985;1:501-12. [PubMed]
- 18.Ellis GL. Subdural hematoma in the elderly. Emerg Med Clin North Am 1990;8:281-94. [PubMed]
- 19.Susman M, DiRusso SM, Sullivan T, et al. Traumatic brain injury in the elderly: increased mortality and worse functional outcome at discharge despite lower injury severity. J Trauma 2002;53:219-23; discussion 223-4. [DOI] [PubMed]
- 20.Inci I, Ozcelik C, Nizam O, et al. Thoracic trauma in the elderly. Eur J Emerg Med 1998;5:445-50. [PubMed]
- 21.Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040-6; discussion 1046-7. [DOI] [PubMed]
- 22.Rothschild JM, Bates DW, Leape LL. Preventable medical injuries in older patients. Arch Intern Med 2000;160:2717-28. [DOI] [PubMed]
- 23.Tornetta p III, Mostafavi H, Riina J, et al. Morbidity and mortality in elderly trauma patients. J Trauma 1999;46:702-6. [DOI] [PubMed]
- 24.Knudson MM, Lieberman J, Morris JA, et al. Mortality factors in geriatric blunt trauma patients. Arch Surg 1994;129:448-53. [DOI] [PubMed]
- 25.Sugimoto K, Aruga T, Hirata M, et al. Geriatric trauma patients at a suburban level-I trauma center in Japan. Prehospital Disaster Med 1999;14:186-90. [PubMed]
- 26.van der Sluis CK, Timmer HW, Eisma WH, et al. Outcome in elderly injured patients: injury severity versus host factors. Injury 1997;28:588-92. [DOI] [PubMed]
- 27.Shabot MM, Johnson CL. Outcome from critical care in the “oldest old” trauma patients. J Trauma 1995;39:254-9; discussion 259-60. [DOI] [PubMed]
- 28.Johnson CL, Margulies DR, Kearney TJ, et al. Trauma in the elderly: an analysis of outcomes based on age. Am Surg 1994;60:899-902. [PubMed]
- 29.Day RJ, Vinen J, Hewitt-Falls E. Major trauma outcomes in the elderly. Med J Aust 1994;160:675-8. [PubMed]
- 30.Miller RS, Patton M, Graham RM, et al. Outcomes of trauma patients who survive prolonged lengths of stay in the intensive care unit. J Trauma 2000;48:229-34. [DOI] [PubMed]
- 31.Pickering SA, Esberger D, Moran CG. The outcome following major trauma in the elderly. Predictors of survival. Injury 1999;30:703-6. [DOI] [PubMed]
- 32.Young JS, Cephas GA, Blow O. Outcome and cost of trauma among the elderly: a real-life model of a single-payer reimbursement system. J Trauma 1998;45:800-4. [DOI] [PubMed]
- 33.Taylor MD, Tracy JK, Meyer W, et al. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma 2002;53:407-14. [DOI] [PubMed]
- 34.Smith DP, Enderson BL, Maull KI. Trauma in the elderly: determinants of outcome. South Med J 1990;83:171-7. [DOI] [PubMed]
- 35.Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg 2002;89:1319-22. [DOI] [PubMed]
- 36.Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma 2001;51:754-6; discussion 756-7. [DOI] [PubMed]
- 37.Bergeron E, Lavoie A, Clas D, et al. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J Trauma 2003;54:478-85. [DOI] [PubMed]
- 38.Bernstein AB, Schur CL. Expenditures for unintentional injuries among the elderly. J Aging Health 1990;2:157-78. [DOI] [PubMed]
- 39.Binder S. Injuries among older adults: the challenge of optimizing safety and minimizing unintended consequences. Inj Prev 2002;8(Suppl 4):IV2-4. [DOI] [PMC free article] [PubMed]