Abstract
Objective
To retrospectively review the outcomes of percutaneous flexor tenotomies of diabetic claw toes with ulcers or pending ulcers.
Methods
We undertook a retrospective chart review between January 1999 and June 2005 to identify those patients who had undergone a percutaneous flexor tenotomy for diabetic claw toe deformities. We identified 34 toes in 14 patients. Of these, 24 toes had ulcerations at the terminal aspect and 3 had radiographic evidence of osteomyelitis of the terminal phalange. All patients had palpable pulses and good capillary refill. A percutaneous flexor tenotomy was performed on all toes in an outpatient clinic; patients with a rigid flexor contracture at the proximal interphalangeal joint underwent an osteoclaysis to correct a portion of the deformity.
Results
The average follow-up was 13 months. All patients with ulcers healed and there were no significant complications. Those without osteomyelitis healed within an average of 3 weeks and those with osteomyelitis healed within an average of 8 weeks.
Conclusion
A percutaneous flexor tenotomy with osteoclasis of the proximal interphalangeal joint performed in an outpatient clinic is a safe and effective method to off-load the tip of the toe so that that ulcer healing can occur. The presence of osteomyelitis is not a contraindication for this technique; however, an increased healing time can be expected.
Abstract
Objectif
Étudier rétrospectivement les résultats de ténotomies percutanées du fléchisseur de l'orteil en griffe de diabétique avec ulcères ou ulcères imminents.
Méthodes
Nous avons entrepris une étude rétrospective de dossiers datant de janvier 1999 à juin 2005 afin d'identifier les patients qui avaient subi une ténotomie percutanée du fléchisseur à cause de difformités de l'orteil en griffe de diabétique. Nous avons trouvé 34 orteils chez 14 patients. Sur ce total, 24 orteils avaient des ulcères à la face terminale et dans trois cas, la radiographie indiquait une ostéomyélite de la phalange terminale. Tous les patients avaient un pouls palpable et un bon remplissage capillaire. On a procédé en service externe à une ténotomie percutanée du fléchisseur sur tous les orteils. Les patients qui avaient une contraction rigide du fléchisseur à l'articulation interphalangienne proximale ont subi une ostéoclasie visant à corriger une partie de la difformité.
Résultats
Le suivi moyen a été de 13 mois. Tous les patients qui avaient des ulcères ont guéri et il n'y avait plus aucune complication importante. Ceux qui n'avaient pas d'ostéomyélite ont guéri en trois semaines en moyenne et ceux qui en avaient une, en huit semaines en moyenne.
Conclusion
La ténotomie percutanée du fléchisseur avec ostéoclasie de l'articulation interphalangienne proximale pratiquée en service externe constitue une façon sûre et efficace d'éliminer la charge au bout de l'orteil afin que l'ulcère puisse guérir. La présence d'une ostéomyélite ne constitue pas une contre-indication pour cette technique, mais on peut s'attendre à ce que la guérison prenne plus de temps.
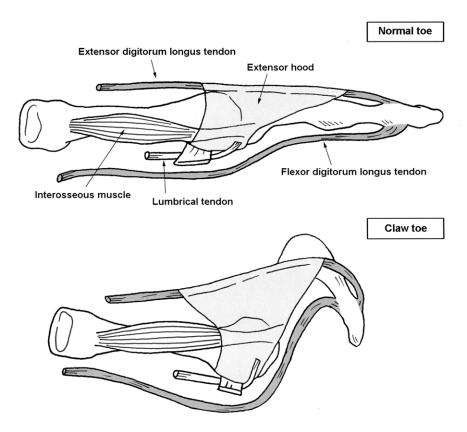
Claw toe deformities are common among people who have had diabetes for more than 10 years.1–4 The diabetic motor neuropathy causes dysfunction of the interossei and lumbricals. The unopposed action of long extensors and flexors results in a hyperextension deformity of the metatarsophalangeal joint and flexor contractures of the distal or proximal inter-phalangeal joints, or both (Fig. 1).
FIG. 1. Toe anatomy and changes with a claw toe deformity.
The intrinsic-minus (claw) deformity of the toes can lead to increased pressure, precipitating ulceration beneath the metatarsal head, over the dorsum of the proximal interphalangeal joint and at the tip of the affected toe. Conservative options such as supportive shoe wear and orthotics can help off-load the dorsal and plantar aspects of the toes. The shoe should have a rigid shank with forefoot rocker, a high toe-box and a soft upper with no internal seams. The orthotic should be supportive, with a soft covering layer and a metatarsal pad. However, despite appropriate nonoperative measures, the ulcers caused by claw toe deformity can still occur and be difficult to heal. Persistent ulceration can lead to osteomyelitis of the phalanges and metatarsal heads (Fig. 2A and 2B). Correction of the claw toe deformity is essential for ulcer healing. A percutaneous tenotomy of the long flexors with osteoclasis of the proximal interphalangeal joint can be performed on an outpatient basis and will aid in the rapid healing of digital ulcers.5–9
FIG. 2. Left: Patient with a 15-year history of diabetes. Patient has a high arched foot with equinus contracture and clawing of the lesser toes. These subtle deformities have been precipitated by the motor neuropathy. Right: Ulceration at tip of a toe caused by a claw toe deformity.
The current study is a retrospective review of percutaneous flexor tenotomies performed in an outpatient clinic in patients with diabetes, claw toe deformities and digital ulceration.
Methods
We retrospectively reviewed the charts of patients with diabetes treated at the High Risk Foot Clinic of St. Michael's Hospital in Toronto, Ontario, between January 1999 and June 2005. All the patients had a claw toe deformity and ulcer at the tip of the distal phalanx of 1 or more toes and underwent flexor tenotomy.
The indication for flexor tenotomy was a flexible or mild-to-moderate rigid claw toe with an ulcer at the tip of the distal phalanx. Contraindications for the procedure were absence of palpable dorsalis pedis and posterior tibial pulses and significant soft tissue infection presenting as cellulitis. Osteomyelitis of the distal phalanx was considered present when there was bone resorption or fragmentation on radiograph and the ulcer probed to bone.
All tenotomies were performed by the senior author (T.D.), who used the technique described.
Technique for percutaneous flexor tenotomy
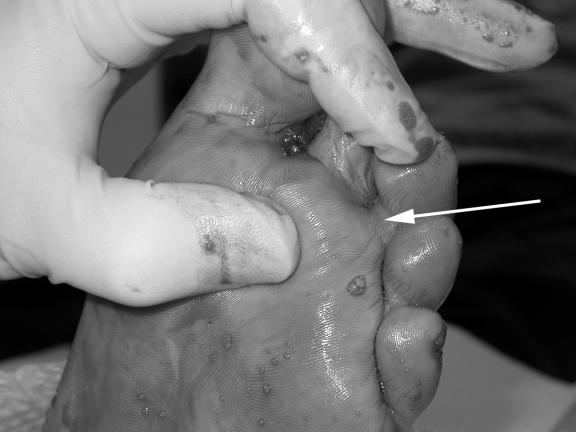
The patient lies supine on the examination table with his or her feet at the lower edge of the bed. Precautions to ensure sterility are always followed. For a digital block, 5 mL of lidocaine may be used; however, in diabetic patients with sensory neuropathy, this is often not necessary. The long flexor of the toe is placed under tension by dorsiflexing the ankle as well as applying pressure over the plantar aspect of the metatarsal head with the thumb and passively extending the metatarsal. The toe is maintained in a flexed position to cause bow stringing of the flexor tendon (Fig. 3). A beaver blade is inserted at the midline of the base of the middle phalanx through a tiny puncture wound. The tendon can be felt with the tip of the blade and must be gently cut by careful side-to-side micromovents of the blade tip without straying medially or laterally to avoid injury to the neurovascular bundles. If the deformity is rigid, the toe is hyperextended at the proximal interphalangeal joint (osteoclasis). Pressure is applied with dressing gauze for several minutes and a sterile dressing applied over the stab wound. The patient is allowed to bear weight in his or her normal shoes, and daily dressings of the ulcer are maintained.
FIG. 3. Foot prepped and draped in the clinic. The ankle is dorsiflexed to neutral, the toe is held in extension at the metatarsophalangeal joint and flexion at the proximal interphalangeal joint to create bowstringing of the flexor tendon. This improves the surgeon's ability to isolate the tendon while performing the percutaneous flexor tenotomy.
The patient is examined within 1 week to ensure that the stab wound is healing satisfactorily and then at regular intervals until the toe ulcers have healed.
Results
Flexor tenotomy was performed on 34 toes in 14 patients with type 2 diabetes mellitus, of whom 8 were men and 6 were women. The average age of the patients was 58 years (range 37–79 y). Of the claw toes, 24 had ulceration at the tip of the distal phalanx, and of these, 3 demonstrated radiological evidence of underlying osteomyelitis. As a prophylactic measure, flexor tenotomy was also performed on 10 claw toes that did not have ulcers but that were at risk of ulceration. Six procedures were done on the first toe (4 with ulceration and 2 without), 11 on the second toe (8 with ulceration and 3 without), 11 on the third toe (7 with ulceration and 4 without), 6 on the fourth toe (5 with ulceration and 1 without) and none on the fifth toe.
The 24 ulcers without osteomyelitis healed within 3 weeks of flexor tenotomy. The 3 ulcers with associated osteomyelitis healed within 8 weeks. These ulcers had been present for an average of 11 months (range 3–24 mo) before tenotomy. There were no serious complications following the procedure. One patient had minor serous oozing from the stab wound postoperatively, but the wound healed within 2 weeks. Average follow-up was 13 months (range 3–27 mo, standard deviation 7 mo). After the procedure, none of the 14 patients had a recurrence of the ulcer, nor did any patient develop a hyperextension deformity of the proximal interphalangeal joint or ulceration beneath the corresponding metatarsal head.
Discussion
In the toe, interossei and lumbricals normally flex the metatarsophalangeal joint and extend the proximal and distal interphalangeal joints. The action of the intrinsic muscles is opposed by the action of the long extensor and flexor tendons; hence, the toe remains balanced. In patients with diabetes, motor neuropathy can cause dysfunction of the interossei and lumbricals muscles.10–12 The unopposed action of the extensor digitorum longus extends the metatarsophalangeal joint and the flexor digitorum longus flexes the interphalangeal joints (Fig. 1) causing a claw toe deformity.13–15
When the toe is clawed, increased pressure and shear forces occur between the skin at the tip of the toe and the inner sole of the shoe.10 In the presence of diabetic sensory neuropathy, protective sensation is lost. Therefore, the patient continues to allow the toe to be subjected to abnormal forces even when an ulcer develops. For this reason the ulcers on the tips of the claw toes become recalcitrant. Tendon sheath infections, cellulitis and osteomyelitis can further complicate the situation, and toe amputations may even be required.
Tenotomy of the long flexor does not always completely correct the claw toe deformity, but it off-loads the pressure over the terminal aspect of the toe sufficiently to allow ulcers to heal and to prevent recurrence.
In our cohort of patients, 100% of the ulcers, including the recalcitrant ones, rapidly healed after flexor tenotomy; in the 10 toes that had prophylactic tenotomies, no ulcer occurred.
Flexor tenotomy can be performed in a clinical setting, often without a digital nerve block in patients with diabetes and sensory neuropathy. The patients are particularly pleased about the fact that they can continue to ambulate in their regular footwear.
We found this procedure to be effective and safe, with no significant complications. Careful screening to ensure adequate blood flow is an essential component in the evaluation of the patient.
Radiographic evidence of osteomyelitis of the distal aspect of the distal phalanx is not a contraindication for flexor tenotomy. In this series, the 3 ulcers associated with osteomyelitis resolved with flexor tenotomy and antibiotic treatment; however, the average healing time was longer than for ulcers without osteomyelitis (3 wk v. 8 wk).
This is a preliminary retrospective study with chart review; therefore, the intermediate or long-term outcomes of a flexor tenotomy cannot be determined. Currently, a prospective trial with force plate analysis has been initiated.
Conclusion
Percutaneous flexor tenotomy is a safe and effective procedure that can be performed in a clinical setting. It aids in rapid healing of recalcitrant ulcers on the tips of the claw toe deformities in diabetic patients.
Contributors: All authors designed the study. All authors acquired and analyzed the data. Drs. Tamir, Daniels and Ms. McLaren wrote the article, and all authors revised it. All authors gave final approval for the article to be published.
Competing interests: None declared.
Accepted for publication May 23, 2006
Correspondence to: Dr. Timothy R. Daniels, University of Toronto, Ste. 800, 55 Queen St. E, Toronto ON M5C 1R6; fax 416 359-1601; danielst@smh.toronto.on.ca
References
- 1.Reiber G, Boyko E, Smith D. Lower extremity foot ulcers and amputations in diabetes. In: Harris M, editor. Diabetes in America. Bethesda (MD): National Institutes of Health; 1995. p. 409-28.
- 2.Singh N, Armstrong D, Lipsky B. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217-28. [DOI] [PubMed]
- 3.Young MJ, Breddy JL, Veves A, et al. The prediction of diabetic neuropathic foot ulceration using vibration perception thresholds. a prospective study. Diabetes Care 1994;17:557-60. [DOI] [PubMed]
- 4.Boyko EJ, Ahroni JH, Stensel V, et al. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care 1999;22: 1036-42. [DOI] [PubMed]
- 5.Sayner LR, Rosenblum BI, Giurini GM. Elective surgery of the diabetic foot. Clin Podiatr Med Surg 2003;20:783-92. [DOI] [PubMed]
- 6.Parrish TF. Dynamic correction of claw toes. Orthop Clin North Am 1973;4: 97-102. [PubMed]
- 7.Pollard JP, Morrison PJ. Flexor tenotomy in the treatment of curly toes. Proc R Soc Med 1975;68:480-1. [PMC free article] [PubMed]
- 8.Feeney MS, Williams RL, Stephen MM. Selective lengthening of the proximal flexor tendon in the management of acquired claw toes. J Bone Joint Surg Br 2001;83:335-8. [DOI] [PubMed]
- 9.Harmonson JK, Harkless LB. Operative procedures for the correction of hammertoe, claw toe, and mallet toe. A literature review. Clin Podiatr Med Surg 1996;13: 211-20. [PubMed]
- 10.Cavanagh P, Ulbrecht J. Biomechanics of the foot in diabetes mellitus. In: Bowker J, Levin ME, O'Neal LW, editors. The diabetic foot. St. Louis: Mosby; 1993. p. 207-26.
- 11.Fernando DJ, Masson EA, Veves A, et al. Relationship of limited joint mobility to abnormal foot pressures and diabetic foot ulceration. Diabetes Care 1991;14:8-11. [DOI] [PubMed]
- 12.Mueller MJ, Hastings M, Commean PK, et al. Forefoot structural predictors of plantar pressures during walking in people with diabetes and peripheral neuropathy. J Biomech 2003;36:1009-17. [DOI] [PubMed]
- 13.Myerson MS, Shereff MJ. The pathological anatomy of claw and hammer toes. J Bone Joint Surg Am 1989;71:45-9. [PubMed]
- 14.Green DR, Brekke M. Anatomy, biomechanics, and pathomechanics of lesser digital deformities. Clin Podiatr Med Surg 1996;13:179-200. [PubMed]
- 15.Mann R, Inman B. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am 1964;46:469-81. [PubMed]