Inflammatory pseudotumour, or inflammatory myofibroblastic tumour (IMT), occurs in various organs, with the lung being the commonest anatomic site.1 IMT is currently regarded as a neoplasm with a wide spectrum of biological behaviour.1 We present a case of pancreatic IMT in a patient with rectal bleeding.
Case report
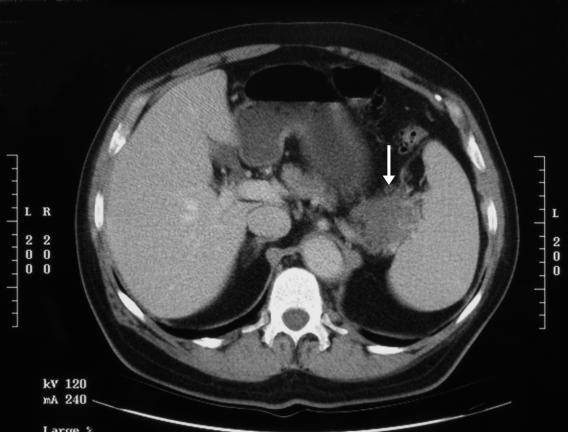
A 56-year-old man with an unremarkable medical history was investigated for intermittent rectal bleeding. Physical examination and routine blood work revealed no abnormality. On endoscopy there were pancolonic diverticulae that were assumed to cause his rectal bleeding. An abdominal CT scan showed a vascular mass measuring 5 cm × 7 cm in the tail of the pancreas, consistent with pancreatic carcinoma (Fig. 1). At laparotomy the mass, which was associated with multiple fibrous adhesions to the surrounding tissue, was excised by distal pancreatectomy with splenectomy. Macroscopically, the lesion measured 7 cm in greatest dimension and was white and rubbery with extensions into the surrounding tissue (Fig. 2).
FIG. 1. CT of the abdomen reveals a solid mass (arrow) in the tail of the pancreas with an irregular border, suggesting a pancreatic cancer.
FIG. 2. Solid pancreatic mass with minimal extension and invasion into peripancreatic fat and multiple fibrous adhesions.
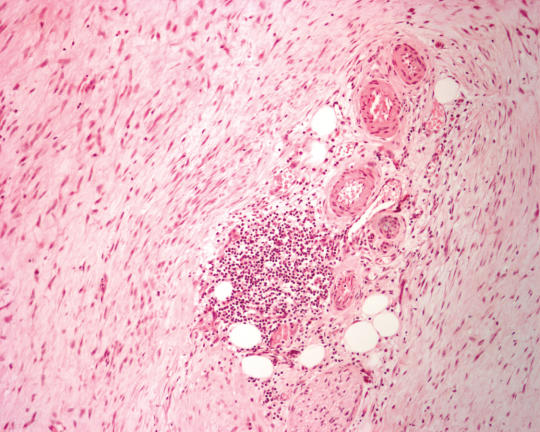
Histologically, the lesion consisted of spindle cells in a vague storiform pattern. Focal edema, myomatous change, hyalinized fibrosis and patchy lymphocytic infiltration were present. The cells contained elongated nuclei, inconspicuous nucleoli and an ill-defined eosinophilic cytoplasm. Neither nuclear atypia nor mitotic activity were present (Fig. 3). Immunohistochemical staining was negative for desmin, myosin and CD34; focally positive for smooth-muscle actin and p53. Electron microscopy demonstrated fusiform cells with abundant rough endoplasmic reticulum and occasional thin filaments with focal myosin densities. All findings were in keeping with an inflammatory myofibroblastic tumour of the pancreas.2 The patient was well and showed no evidence of tumour recurrence or metastasis 18 months after the operation.
FIG. 3. Histologic appearance of the pancreatic lesion showing a proliferation of spindle-shaped cells and an aggregate of lymphoid cells (hematoxylin–eosin; original magnification 250×).
Discussion
Pancreatic IMT is rare, with only 25 cases having been reported in the English-language literature.2 It may occur at any age (range 2.5–70 y, average 36 y), is more common in women and measures 1.5–13 cm (average 6 cm). Sixty percent of pancreatic IMTs are located in the head and 40% in the body and tail of the organ.2 Common presenting clinical symptoms are abdominal pain or discomfort, weight loss, a palpable abdominal mass and anemia. Obstructive jaundice was present in 66.7% of IMTs located in the head of the pancreas.2 In almost all cases, a correct diagnosis was not made pre-or intraoperatively, even with intraoperative frozen-section examination of the tumour. IMT was most commonly mistaken for a pancreatic cancer clinically and radiologically, and its definitive diagnosis was made only by extensive histologic examination with ancillary testing.2 Histologically, the lesion is characterized by a myofibroblastic proliferation in a vague storiform pattern and a varying degree of inflammatory infiltrates consisting mainly of lymphocytes, plasma cells and histiocytes, as seen in our case.2 Features present in some cases of pancreatic IMT with aggressive behaviour were ganglion-like cells, nuclear atypia, aneuploidy and p53 expression2; in our case, only p53 expression was present. The only known effective treatment for pancreatic IMT is complete surgical resection, which has a favourable prognosis.2
Competing interests: None declared.
Accepted for publication July 19, 2006
Correspondence to: Dr. Adrian Sim, Division of Anatomical Pathology, University of Alberta Hospital, 8440–112th St., Edmonton AB T6G 2B7; absim@ualberta.ca
References
- 1.Coffin CM, Dehner LP, Meis-Kindblom JM. Inflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and related lesions: an historical review with differential diagnostic considerations. Semin Diagn Pathol 1998;15:102-10. [PubMed]
- 2.Pungpapong S, Geiger XJ, Raimondo M. Inflammatory myofibroblastic tumor presenting as a pancreatic mass: a case report and review of the literature. JOP 2004;5:360-7. [PubMed]