Abstract
Objective
To develop a core curriculum for orthopedic surgery and to conduct a national survey to assess the importance of 281 curriculum items. Attention was focused on 55 topics pertaining to hip and knee reconstruction.
Methods
A 281-item curriculum was developed. We completed a content review and cross-sectional survey of a random selection of orthopedic surgeons whose primary affiliation was nonuniversity. We analyzed the data descriptively and quantitatively, using histograms, a modified Hotelling's T2 statistic with the p value determined by a permutation test, and the Benjamini-Hochberg/Yekutieli procedure. Our analyses assumed that each respondent answered questions independently of the answers of any other respondent but that the answers to different questions by the same respondent might be dependent.
Results
Of 156 orthopedic surgeons, 131 (84%) participated in this study. Of 55 items ranked by all respondents, 42 received an average mean score greater than 3.5/4.0, and 51 received an average mean score equal to or greater than 3.0/40 (the standard deviation for each item ranged from 0.00 to 0.08), suggesting that 92.7% of the items are important or probably important to know by the end of residency.
Conclusion
This study demonstrates agreement that it is important to include 92.7% of the items that pertain to hip and knee reconstruction in a core curriculum for orthopedic surgery. Residency training programs may need to ensure that appropriate educational opportunities focusing on complex primary and revision surgery are available to meet the future needs of orthopedic surgeons whose primary affiliation is nonuniversity.
Abstract
Objectif
Créer un tronc commun pour le programme d'études en chirurgie orthopédique et effectuer un sondage national pour évaluer l'importance de 281 éléments du programme. On a concentré l'attention sur 55 sujets reliés à l'arthroplastie de la hanche et du genou.
Méthodes
Nous avons créé un programme d'études comportant 281 éléments. Nous avons effectué une étude de contenu et une enquête transversale auprès d'un échantillon aléatoire de chirurgiens orthopédistes dont la principale affiliation était non universitaire. Nous avons analysé les données de façon descriptive et quantitative en utilisant des histogrammes, une statistique T-carré de Hotelling modifiée dont la valeur p est déterminée par un test de permutation et nous avons suivi la procédure Benjamini-Hochberg–Yekutieli. Dans nos analyses, nous avons supposé que chaque répondant avait répondu aux questions indépendamment des autres, mais que les réponses du même répondant à des questions différentes pourraient être dépendantes.
Résultats
Sur 156 chirurgiens orthopédistes, 131 (84 %) ont participé à l'étude. Sur 55 éléments classés par tous les répondants, 42 ont reçu en moyenne un résultat moyen de plus de 3,5/4,0 et 51 ont reçu un résultat moyen de 3,0/4,0 ou plus (l'écart-type de chaque élément a varié de 0,00 à 0,08), ce qui indique qu'il est important ou probablement important de connaître 92,7 % des éléments à la fin de la résidence.
Conclusion
Cette étude démontre qu'il importe d'inclure 92,7 % des éléments ayant trait à l'arthroplastie de la hanche et du genou dans le tronc commun du programme d'études en chirurgie orthopédique. Les programmes de formation en résidence pourraient devoir s'assurer que des possibilités suffisantes de formation en chirurgie primaire complexe et en chirurgie de révision sont offertes pour répondre aux besoins futurs des chirurgiens orthopédistes dont l'affiliation principale est non universitaire.
This paper is part of a larger study of the development and validation of a core curriculum for orthopedic surgery. One entire core curriculum was validated, and then 10 individual analyses were completed to clarify the content that residents should learn during residency in orthopedic surgery. This paper pertains specifically to core curriculum items relating to adult hip and knee reconstruction.
The World Health Organization (WHO) projects that by the year 2020 osteoarthritis will be the fourth leading cause of disability worldwide. Not surprisingly, the economic burden of illness generated from conditions as such arthritis will be enormous.1–11
The cost of illness resulting from musculoskeletal conditions was a main reason the WHO declared the years 2000–2010 to be the decade for bone and joint health, with a major aim being to increase education of health care providers at all levels. In Canada, the Bone and Joint Decade Undergraduate Curriculum Groups (BJDUCG) core curriculum recommendations for musculoskeletal conditions12 were validated in postgraduate education by 6 disciplines that manage patients with musculoskeletal conditions. These disciplines include family medicine, sports medicine, emergency medicine, physical medicine and rehabilitation, rheumatology and orthopedic surgery.13
The need to educate people with surgical skills to manage patients with hip and knee arthritis and related conditions will continue to be extremely important. Currently there are no guidelines on what orthopedic residents should be learning about musculoskeletal conditions involving the hip and knee. It is assumed that residents in all orthopedic training programs will become competent in performing primary total knee and hip reconstruction. However, no core curriculum content has been validated in the educational domain of adult hip and knee reconstruction.
An educational initiative to develop and validate an orthopedic curriculum designed to meet the needs of resident education in Canada was undertaken. This educational initiative was given full support by the Canadian Orthopaedic Association and Bone and Joint Decade Canada. In addition, the Specialty Committee for Orthopaedic Surgery of the Royal College of Physicians and Surgeons of Canada (RCPSC) and the Examination Committee for Orthopaedic Surgery in Canada specifically requested that this national survey to assess the importance of orthopedic curriculum items be determined by orthopedic surgeons whose primary affiliation is nonuniversity.
This study's objective was to determine the importance of core content to be included in a core curriculum for orthopedic surgery, with a specific focus on content pertaining to adult hip and knee reconstruction.
The null hypothesis tested was that, on completion of his or her residency training, it is important for a resident to demonstrate equal knowledge of all items in the core curriculum for orthopedic surgery pertaining to adult hip and knee reconstruction or to perform all related procedures with equal proficiency.
Methods
Development of the outcome measure
A 281-item, 3-section questionnaire was developed. The previously validated international core curriculum for musculoskeletal health makes up the first section.13 Specialty objectives of the RCPSC specifically pertaining to orthopedic surgery make up the second cluster of items. The third section includes a complete procedure list based on codebooks from across Canada. Once this outcome measure was created, we compared it with the curricula of the various institutions to ensure that what the university programs thought to be important was also included.
The outcome was fully reviewed for content by 10 orthopedic surgeons (with FRCSC designation) of both sexes, representing adult and pediatric orthopedic surgery, education and research from within Canada and the United States. A modified outcome was then developed on the basis of feedback from this review, and the final questionnaire had 281 items. The questionnaire was translated into French to facilitate data collection from francophone orthopedists. This questionnaire is available on request from the corresponding author.
Randomization and cross-sectional survey
From the 2004 RCPSC list of actively practising orthopedic surgeons in Canada, 156 orthopedic surgeons whose primary affiliation was nonuniversity were randomized to this study via a random number table. The randomization was done in 3 separate processes to ensure appropriate representation from the Atlantic provinces and Quebec, central Canada (Ontario) and western Canada (Manitoba, Saskatchewan, Alberta, British Columbia and the 3 territories). These distributions were based on the numbers of orthopedic surgeons within regions.
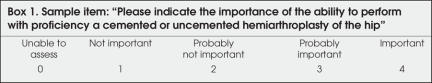
A schedule for direct one-on-one interviews was arranged, and interviews were conducted in both official languages according to the functional language of each respondent. A cross-sectional survey was completed. The anglophone interviews were completed either over the telephone or in person, and the francophone interviews were completed via direct one-on-one interviews during a research tour through Quebec. Possible responses to each of the 281 questions were as follows: 0 = unable to assess; 1 = not important; 2 = probably not important; 3 = probably important and; 4 = important. A sample question is outlined in Box 1.
Box 1.
Statistical analysis
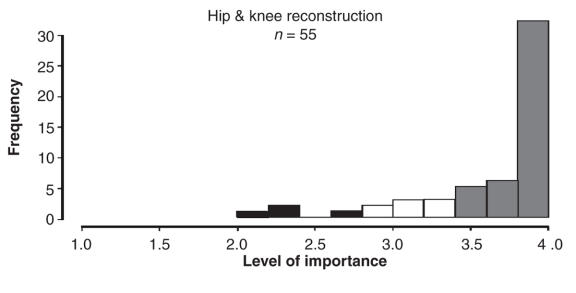
We analyzed the data descriptively and quantitatively, using histograms, a modified Hotelling's T2 statistic14 with p value determined by a permutation test, and the Benjamini-Hochberg/Yekutieli procedure.15–18 Our analyses assumed that each respondent answered questions independently of the answers of any other respondent but that the answers to different questions by the same respondent might be dependent. We used a histogram to summarize the average mean scores of items pertaining specifically to adult hip and knee reconstruction.
Each of the 131 identified orthopedic surgeons answered each of the 281 questions during the same sitting. Answers given to different questions by the same respondent must be considered related (“dependent”) to each other. Dealing with these dependencies entailed our using the modified Hotelling's T2 statistic with a p value determined by a permutation test.
We then used the Benjamini-Hochberg/Yekutieli procedure to help us manage the large number of tests we did for differences between pairs of questions. This procedure showed definitively that questions are not all the same, in that the distribution of the ratings given to one question appeared to be different from that of another question for many pairs of questions.
The analysis first addressed all 281 items. Average ranked mean scores were obtained and listed in ascending order of importance for the entire core curriculum. This study highlighted content pertaining to adult reconstruction of the hip and knee.
Results
Demographics
Of 156 orthopedic surgeons whose primary affiliation is nonuniversity, a sample of 131 participated in this study, for an overall response rate of 84%. There was a 90% response rate from the Atlantic provinces and Quebec and an 80% response rate from Ontario, the 3 territories and the western provinces of Manitoba, Saskatchewan, Alberta and British Columbia.
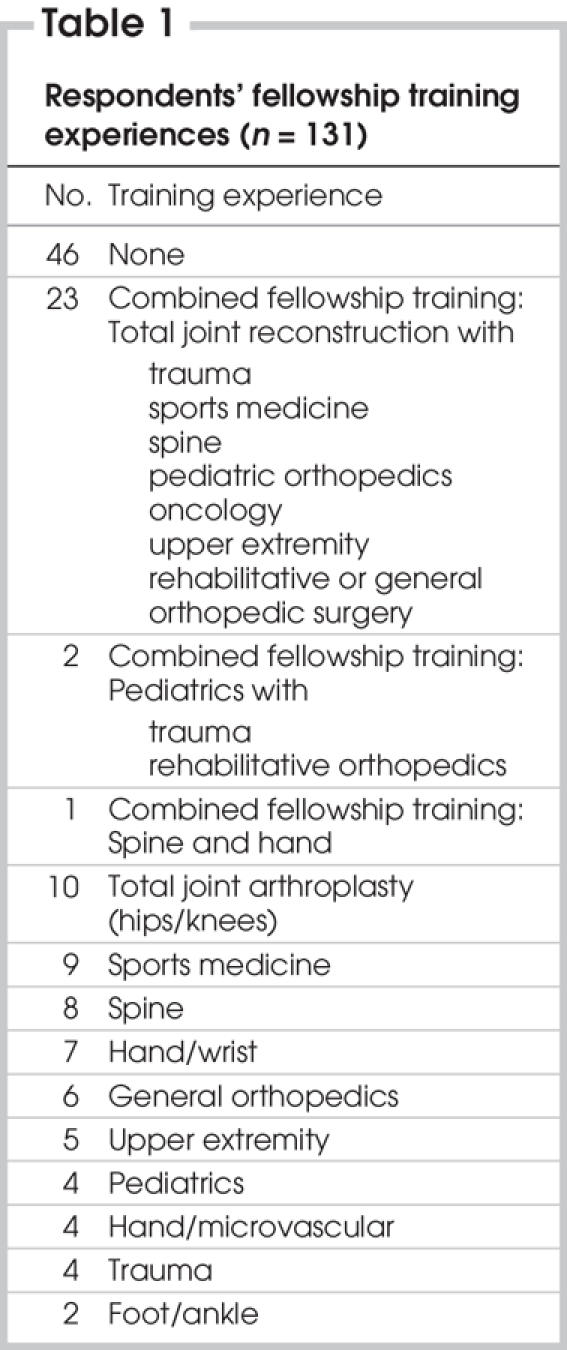
Of the respondents, 85% classified themselves as generalists and 15% as specialists. The average age of each respondent was 48.7 years. Each respondent had been in practice for an average of 16.8 years. Men made up 90% of the respondents and women 10%. The demographics of fellowship training experiences are outlined in Table 1.
Table 1
Orthopedic curriculum content for adult hip and knee reconstruction
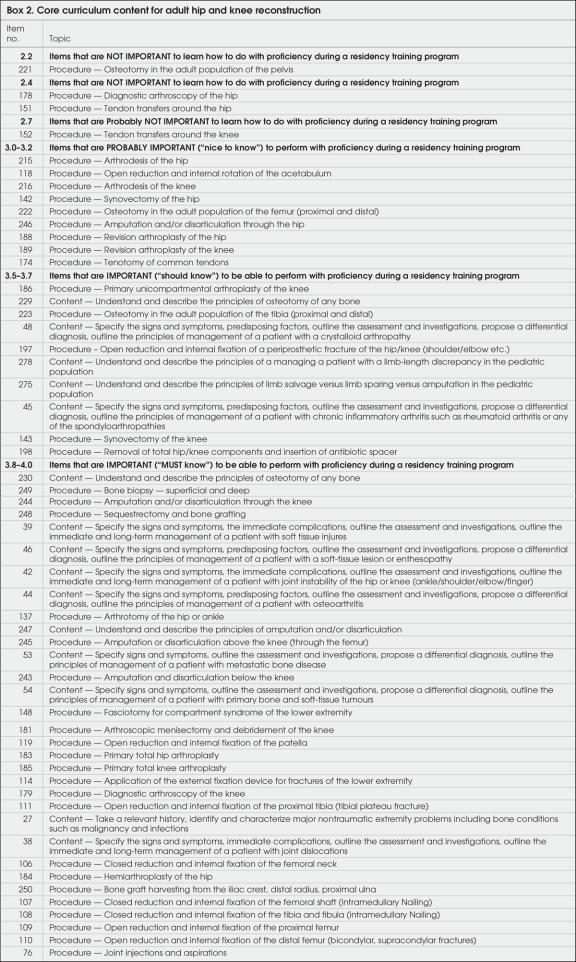
The histogram (Fig. 1) demonstrates in graphical format the distribution of curriculum items pertaining to hip and knee reconstruction in ascending order of importance. Content pertaining to adult hip and knee reconstruction for the resident level of education is outlined in Box 2.
FIG. 1: Histogram showing distribution of items for hip and knee reconstruction core curriculum content, based on level of importance according to respondents.
Box 2.
Of 55 adult hip and knee reconstruction items, 51 were given an average mean score of equal to or greater than 3.0/4.0 by all 131 respondents (Fig. 1), suggesting that 92.7% of the items (Box 2) are either probably important or important to know by the end of residency. The standard deviation (SD) for each item ranged from 0.00 to 0.08. In addition, the Benjamini-Hocherg/Yekutieli procedure demonstrates that, for 70% of the 1485 pairs of questions (55 × 54 / 2) pertaining to adult hip and knee reconstruction, the distributions of the ratings given to one question are different from that of another question for many pairs of questions. There is a false-discovery rate of less than 0.05 (Fig. 1).
Discussion
Currently, the expectation of the Specialty Committee for the RCPSC is that residents are graduating from their respective training programs with the ability to perform primary hip and knee reconstruction with competence. However, some questions arise: Are programs graduating residents competent to perform complex primary and revision procedures? Should residents be competent in their ability to perform such procedures around the hip and knee? Is the exposure to surgical hip and knee arthritic conditions and the ability to operate comfortably on such conditions specific to the fellowship level, or should this exposure also be given more serious attention at the residency level?
Our study suggests that orthopedic residents should be competent in their ability to know of and understand cognitive content pertaining to the ability to specify signs and symptoms and immediate complications. They should be able to outline the assessment, investigations and management plans for various musculoskeletal conditions such as arthritis, soft-tissue conditions, joint dislocations, joint instability, infections, malignancy and tumours, amputations and joint disarticulations, limb-length discrepancy and limb sparing versus limb salvage. Finally, they should understand the principles of managing patients with chronic inflammatory arthritis, such as rheumatoid arthritis or any of the spondyloarthropathies.
A specific focus on lower-extremity reconstruction procedures as they relate to arthritis, such as primary hip and knee reconstruction, unicompartment knee arthroplasty, osteotomy and removal of components and insertion of cement spacer in the presence of infection, were also identified as areas in which residents should have knowledge and competency on completion of residency.
In addition, lower extremity reconstruction procedures as they pertain to trauma, such as the ability to perform with proficiency a hemiarthroplasty, stabilization of lower extremity fractures and periprosthetic fracture fixation, will need to be emphasized.
Items considered to be less important include competency in more complex hip and knee procedures, including arthrodeses, joint disarticulations and some soft tissue procedures, along with competency in revision total joint procedures and stabilizing fractures of the acetabulum.
Items considered probably not at all important to be learned with proficiency during residency include tendon transfers around the hip, hip arthroscopy and osteotomies about the pelvis and femur. These procedures may reflect content that would be more suitable at the fellowship level of education.
The projected burden of illness for musculoskeletal conditions will be tremendous as our “front-end baby-boomers” enter their retirement years. By the year 2020, the WHO projects that, worldwide, 40% of a population that is living longer will be afflicted with osteoarthritis. These trends will specifically affect the number of joint reconstruction procedures performed by orthopedic surgeons. Epidemiologic data suggest that patient demographics of people receiving total joint procedures are changing19 and that many primary total joint replacements being performed will likely need to be revised at an exponential rate in the future.20 If these projections are true, then orthopedists whose primary affiliation is nonuniversity will need to be competent in these procedures. Will there be enough competent surgeons in Canada to meet these projected demands?
Previous studies indicate that educating orthopedic residents is expensive.3,21–23 How residents are educated12,13,21–29 is not the focus of this particular study. However, educational planning will need to focus somewhat on cost-effective and efficient ways of educating future orthopedic surgeons to meet the projected health care demands. Residency training programs are uniquely positioned to implement suggestions and to provide solutions to ensure adequate surgical education in the area of hip and knee reconstruction. It will be important for programs to ensure that adequate learning opportunities are available for residents to learn the cognitive and technical skill sets essential to lower extremity reconstruction.30
In addition, education tends to be driven by evaluation.31 Therefore, fellowship examination questions should reflect the areas being emphasized during training to ensure that what is being taught is also being evaluated. If examination questions reflect the areas of competence required for an orthopedic surgeon in the community, then residency training programs will tend to expose their residents to suitable learning experiences that will prepare them for success on the fellowship examination.
The strengths of the study included:
• A previously validated international core curriculum for musculoskeletal health.
• Randomization of orthopedic surgeons in 3 different regions of Canada and use of a translated outcome with direct one-on-one interviews, which may explain the 84% response rate.
• A full content review before the study was conducted.
• A translated outcome measure and direct interviewing of the francophone orthopedists, which may explain the 90% response rate from Quebec and the Atlantic provinces.
• Full endorsement by the RCPSC Specialty Committee for Orthopaedic Surgery.
• Unprecedented collaboration between the Canadian Orthopaedic Association and Bone and Joint Decade Canada for the sole purpose of improving education of orthopedic surgeons across Canada.
Study limitations include a positive response bias within the questionnaire and a limited scale grading the level of importance. As well, the wording of the questions asked each respondent to indicate the importance of either content or procedures. This implies that we are asking for opinions rather than asking about what respondents are actually doing.
Conclusions
Terminal and enabling objectives for orthopedic curricula pertaining to adult hip and knee reconstruction should focus on common problems of various musculoskeletal conditions, complex primary and revision procedures and the ability to manage complications.
The necessity to educate orthopedic surgeons in the area of adult hip and knee reconstruction within Canada will continue to be important. However, it is also our professional responsibility to ensure that surgeons entering into our health care system can in fact safely and competently deliver these services. Programs may need to consider strategies to balance the time that residents spend in the various disciplines of orthopedic surgery to ensure that specific content is learned and competence is evaluated. If these goals are not attainable, then other options, such as the development of regional referral centres, may need to be considered32 to meet current and projected health care demands for all Canadians.
Presented at the 2006 Annual Meeting of the American Academy of Orthopaedic Surgeons, March 22–26, 2006, Chicago, Ill., USA.
Contributors: Drs. Wadey, Maloney and Walker designed the study. Dr. Wadey acquired the data, and Drs. Wadey, Maloney, Dev and Walker analyzed it. Dr. Wadey wrote the article, which Drs. Maloney, Dev and Walker reviewed. All authors gave final approval for publication of the article.
Competing interests: Dr. Wadey received funding support as the 2003 and 2004 Medical Education Travelling Fellow for the Royal College of Physicians and Surgeons of Canada. None declared for Drs. Maloney, Dev and Walker.
Accepted for publication Nov. 16, 2006
Correspondence to: Dr. V.M.R. Wadey, Lower Extremity Reconstruction, Division of Orthopaedic Surgery, Department of Surgery, University of Toronto, Holland Orthopaedic & Arthritic Centre, 43 Wellesley St. E, Suite 621, Toronto ON M4Y 1H1; fax 416 239-4971; veronica.wadey@sunnybrook.ca
References
- 1.Brouwer WB, van Exel NJ, van de Berg B, et al. Burden of caregiving: evidence of objective burden, subjective burden, and quality of life impacts on informal caregivers of patients with rheumatoid arthritis. Arthritis Rheum 2004;51:570-7. [DOI] [PubMed]
- 2.Cooper NJ. Economic burden of rheumatoid arthritis: a systematic review. Rheumatology (Oxford) 2000;39:28-33. [DOI] [PubMed]
- 3.Coyte PC, Asche CV, Croxford R, et al. The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res 1998;11:315-25. [DOI] [PubMed]
- 4.Guillemin F, Durieux S, Daurès JP, et al. Costs of rheumatoid arthritis in France: a multicenter study of 1109 patients managed by hospital-based rheumatologists. J Rheumatol 2004;31:1297-304. [PubMed]
- 5.Gupta S, Hawker GA, Laporte A, et al. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology (Oxford) 2005;44:1531-7. [DOI] [PubMed]
- 6.Kvien TK. Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics 2004;22(Suppl):1-12. [DOI] [PubMed]
- 7.Leardini G, Salaffi F, Caporali R, et al. Direct and indirect costs of osteoarthritis of the knee. Clin Exp Rheumatol 2004;22:699-706. [PubMed]
- 8.Söderlin MK, Kautiainen H, Skogh T, et al. Quality of life and economic burden of illness in very early arthritis. A population based study in southern Sweden. J Rheumatol 2004;31:1717-22. [PubMed]
- 9.Verstappen SM, Verkleij H, Bijlsma JW, et al. Determinants of direct costs in Dutch rheumatoid arthritis patients. Ann Rheum Dis 2004;63:817-24. [DOI] [PMC free article] [PubMed]
- 10.Westhovens R, Boonen A, Verbruggen L, et al. Healthcare consumption and direct costs of rheumatoid arthritis in Belgium. Clin Rheumatol 2005;24:615-9. [DOI] [PubMed]
- 11.Yelin E, Cisternas MG, Pasta DJ, et al. Medical care expenditures and earnings losses of persons with arthritis and other rheumatic conditions in the United States in 1997: total and incremental estimates. Arthritis Rheum 2004;50:2317-26. [DOI] [PubMed]
- 12.Woolf AD, Walsh NE, Akesson K. Global core recommendations for musculoskeletal undergraduate curriculum. Ann Rheum Dis 2004;63:517-24. [DOI] [PMC free article] [PubMed]
- 13.Wadey VMR, Tang ET, Abelseth G, et al. Canadian multidisciplinary core curriculum for musculoskeletal health. J Rheumatol 2007;34:455-7. [PubMed]
- 14.Behseta S, Kass RE. Testing equality of two functions using BARS. Stat Med 2005;24:3523-34. [DOI] [PubMed]
- 15.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Statist Soc Ser 1995;B57:289-300.
- 16.Benjamini Y, Hochberg Y. Multiple hypotheses testing with weights. Scand J Stat 1997;24:407-18.
- 17.Benjamini Y, Hochberg Y. The adaptive control of the false discovery rate in multiple hypotheses testing. J Behav Educ Statist 2000;25:60-83.
- 18.Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat 2001;29:1165-88.
- 19.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res 2006;443:266-72. [DOI] [PubMed]
- 20.Williams MH, Newton JN, Frankel SJ, et al. Prevalence of total hip replacement: how much demand has been met? J Epidemiol Community Health 1994;48:188-91. [DOI] [PMC free article] [PubMed]
- 21.Gunther SB, Soto GE, Colman WW. Interactive computer simulations of knee-replacement surgery. Acad Med 2002;77:753-4. [DOI] [PubMed]
- 22.Lavernia CJ, Sierra RJ, Hernandez RA. The cost of teaching total knee arthroplasty surgery to orthopaedic surgery residents. Clin Orthop Relat Res 2000;380: 99-107. [DOI] [PubMed]
- 23.Roye WW Jr, Dunn EL, Watermeyer DS, et al. Postgraduate trauma education; the surgeon; the cost. J Trauma 1989;29:1471-5. [DOI] [PubMed]
- 24.Chapman MW. Education in orthopaedic trauma. Clin Orthop Relat Res 1997;339:7-19. [DOI] [PubMed]
- 25.Graham CA, Sinclair MT. A survey of advanced trauma life-support training for trainees in acute surgical specialties. Injury 1996;27:631-4. [DOI] [PubMed]
- 26.Rogers F, Shackford S, Daniel S, et al. Workload redistribution: a new approach to the 80 hour workweek. J Trauma 2006;60:911-4. Comment in: J Trauma 2006;60:246-7; author reply 247. [DOI] [PubMed]
- 27.Rozental TD, Lonner JH, Parekh SG. The Internet as a communication tool for academic orthopaedic surgery departments in the United States. J Bone Joint Surg Am 2001;83:987-91. [DOI] [PubMed]
- 28.Rymaszewski LA, Sharma S, McGill PE, et al. A team approach to musculo-skeletal disorders. Ann R Coll Surg Engl 2005;87:174-80. [DOI] [PMC free article] [PubMed]
- 29.Toms AD, McClelland D, Maffulli N. Trauma and orthopaedic training in the United Kingdom. J Bone Joint Surg Am 2002;84:501-3. [DOI] [PubMed]
- 30.Dailey SW, Brinker MR, Elliott MN. Orthopaedic residents' perceptions of the content and adequacy of their residency training. Am J Orthop 1998;27:563-70. [PubMed]
- 31.Kragh JF Jr, Bagg MR, Ward JA, et al. Measuring medical education and curriculum during orthopaedic residency. J Surg Res 2005;123:268-74. [DOI] [PubMed]
- 32.Katz JN, Barrett J, Mahomed NN, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am 2004;86:1909-16. [DOI] [PubMed]