Abstract
Objective
Pathophysiological processes in the first days after trauma seem to be important for the development and final outcome in cases of multiple organ failure (MOF). Our objective in this study was to assess the kinetics of C-reactive protein (CRP), interleukin-6 (IL-6), interleukin-10 (IL-10) and phospholipase A2 group II (PLA2-II) as predictors of more severe forms of MOF. As well, we sought to assess the criteria for systemic inflammatory response syndrome (SIRS) and Simplified Acute Physiology Score (SAPS II) values and to create predictive models of MOF development.
Methods
This prospective study recruited a sample from 75 patients treated for severe injuries at surgical intensive care units at the Clinical Center of Serbia. Of these patients, a total of 65 met the entry criteria, which included an Injury Severity Score ≥ 18 (severe injury), age range 16–65 years, admission to the hospital within the first 24 hours after injury and survival longer then 48 hours. We excluded patients with primary injury to the central nervous system.
Results
When patients with and without MOF were compared, a statistically significant difference was noted in the average CRP and PLA2II levels on all days. IL-6 and IL-10 concentrations were significantly different on all days of hospitalization.
Conclusion
According to the results of our study, it is possible to create predictive models with a high level of accuracy for the development of organ failure in traumatized patients. The most important parameters of MOF development are serum IL-6 concentration on the first day of hospitalization and the number of positive SIRS criteria on the fourth day of hospitalization.
Abstract
Objectif
Les phénomènes physiopathologiques qui surviennent au cours des premiers jours suivant un traumatisme semblent importants pour l'évolution et l'issue finale dans les cas de défaillance d'organes multiples (DOM). Cette étude visait à évaluer la cinétique de la protéine C-réactive (PCR), de l'interleukine-6 (IL-6), de l'interleukine-10 (IL-10) et de la phospholipase A2 du groupe II (PLA2-II) comme prédicteurs de formes plus sévères de DOM. Nous avons cherché aussi à évaluer les critères du syndrome de réponse inflammatoire systémique (SIRS) et les valeurs du score simplifié de la physiologie aigüe (SAPS II), ainsi que des modèles prédicteurs d'apparition de DOM.
Méthodes
Pour cette étude prospective, nous avons recruté un échantillon parmi 75 patients traités pour des traumatismes sévères aux unités chirurgicales des soins intensifs du Centre clinique de la Serbie. Parmi ces patients, 65 au total satisfaisaient aux critères d'admission, qui incluaient un score de gravité de la blessure de ≥ 18 (traumatisme grave), une plage d'âge de 16 à 65 ans, l'hospitalisation dans les 24 heures suivant le traumatisme et une survie de plus de 48 heures. Nous avons exclu les patients qui avaient un traumatisme primaire au système nerveux central.
Résultats
Lorsqu'on a comparé les patients avec et sans DOM, on a constaté une différence statistiquement significative au niveau des concentrations moyennes de PCR et de PLA2-II tous les jours. Les concentrations d'IL-6 et d'IL-10 étaient significativement différentes tous les jours de l'hospitalisation.
Conclusion
Les résultats de notre étude indiquent qu'il est possible de créer des modèles prédicteurs très précis de l'apparition de la défaillance d'organes chez les patients traumatisés. Les paramètres les plus importants de l'apparition de DOM sont la concentration sérique d'IL-6 le premier jour de l'hospitalisation et le nombre de critères positifs de SIRS le quatrième jour de l'hospitalisation.
Multiple organ failure (MOF) is the leading cause of late death after trauma. The term defines an “all-or-nothing” event and represents the extreme point of a continuous dynamic process of organ function deterioration. There is no gold standard for quantification of the degree of organ damage. Several scores are used, the most well-known of which are the Multiple Organ Dysfunction (MOD) score from 1995 and the Denver postinjury MOF score.1,2 Most studies have combined 2 or more scores to achieve higher objectivity.2 The outcome of MOF after an injury has not improved in the last decade.3 Injury severity, late or inadequate resuscitation, inadequate surgical intervention, persistent inflammatory focus, previous organ damage, chronic disease and age over 65 years may affect the presentation and outcome of MOF. Its frequency is directly related to advances in technology and supportive treatment in intensive care units.
Mediators play an important role in the development of MOF and may therefore be used as predictors of posttraumatic development and mortality.4 A dysfunctional systemic inflammatory response syndrome (SIRS) is the central event in MOF pathogenesis.5 The Society of Critical Care Medicine and the American College of Chest Physicans defined the following criteria for SIRS6,7: body temperature > 38°C or < 36°C, heart rate > 90 beats/min, tachypnea (a respiratory rate > 20 breaths/min at room temperature or PaCO2 < 4.3 kPa), white blood cell count > 12 000/mm3 or < 4000/mm5 or > 10% bands.
It is still not possible to identify the risk group in time to undertake efficient intervention. There is a tight correlation between cytokine plasma level, development of MOF and mortality rate. Thus the development of immunomonitoring would help in the selection of patients at risk for posttraumatic complications and also in the choice of the most appropriate treatment protocols for severely injured patients.8
The aim of this study was to assess the kinetics of C-reactive protein (CRP), interleukin-6 (IL-6), interleukin-10 (IL-10) and phospholipase A2 group II (PLA2-II) as predictors of MOF. As well, we sought to assess criteria for SIRS and Simplified Acute Physiology Score (SAPS II) values and to create predictive models of MOF development.
Methods
At its beginning, this prospective study included 75 patients treated for severe injuries at surgical intensive care units in the Clinical Center of Serbia. All subjects fulfilled the following criteria: Injury Severity Score (ISS) ≥ 18 (severe injury), age range 16–65 years and admission to the hospital within the first 24 hours after the injury. Patients with primary injury to the central nervous system were excluded.9 An additional 10 patients were excluded owing to development of MOF in the first 24 hours after the injury and to lethal outcome in the first 48 hours. The remaining 65 patients were followed for the next 10 days. They were separated into 2 groups: the first comprised 29 patients with severe trauma without organ insufficiency, and the second comprised 36 patients with severe trauma and organ insufficiency. Markers and mediators of inflammation were determined in all patients within the first 24 hours and then on the second, third, seventh and tenth day of hospitalization. The reference range for PLA2-II was 0–6 ng/mL, as determined from 120 healthy people with by means of enzyme-linked immunoadsorbent assay (ELISA) (Boehringer Mannheim GmbH, Germany). Inter-and intra-assay coefficients of variation for normal, elevated (19 ng/mL) and markedly high (60 ng/mL) PLA2-II concentrations of pooled patients' sera were less than 11% and 6%, respectively.10 Concentration of CRP was determined by immunonephelometry on the “Behring” laser nephelometer, with a normal value being < 9 mg/mL. Interleukin concentration was measured with an Immunotech test (Immunotech, Marseille, France) based on “sandwich” enzyme immunodetermination. The reference range for IL-6 was 0–8 pg/mL, and for IL-10, it was 0–10 pg/mL.
The SAPS II has 17 variables, 12 of which assess physiology, age and type of treatment and 3 of which identify the presence of chronic diseases such as AIDS, metastatic cancer or hematologic malignancy. For the 12 physiologic variables, the poorest values in the first 24 hours upon admission (those with the highest number of points) are taken into account.
We determined the Injury Severity Score (ISS) from the formula (ISS = Abbreviated Injury Score [AIS]2 + AIS2 + AIS2) where AIS2 represents squared single highest scores from 3 regions of the body in the first 24 hours. We also applied the combined MOF/MODS score that defines organ damage according to the presence of 1 or more variables.1,11,12 Respiratory failure was deemed present when mechanical ventilation was necessary for at least 72 hours, when PaO2/FiO2 < 37.3 kPa positive end-expiratory pressure (PEEP) was over 8 cm H2O and when there was radiographically confirmed acute respiratory distress syndrome or a respiratory rate ≤ 5/min or ≥ 49/min. Hepatic failure was defined as bilirubinemia over 51 μmol/L for at least 48 hours. Renal insufficiency was defined as serum creatinine over 177 μmol/L for at least 48 hours. Heart failure was defined as cardiac index < 3.0 × min–1 × m–2, obligatory application of inotropic therapy, heart rate ≤ 54/min, present ventricular tachicardy and/or fibrillation and mean arterial pressure ≤ 49 mm Hg or pH ≤ 7.24. Hematologic insufficiency was defined as a platelet count < 20000 or a white blood cell count < 1 × 10–9/L. We analyzed these parameters in all patients included in our study, and the worst results in the first 24 hours were taken into account when we qualified for the existence of organ insufficiency. The presence of at least 1 of the mentioned criteria during hospitalisation defined existing organ damage. MOF duration was not significant because it represents an “all-or-nothing” event.
We used χ2, Student's t test and the Mann–Whitney U test for intergroup comparisons. A logistic regression coefficient was used to investigate the correlation between the number of SIRS criteria per hospital days and the development of MOF. Values of p < 0.05 or p < 0.01 were considered significant. Each variable was assessed individually with univariate analysis as a resulting variable for MOF. Parameters that were found to be statistically significant predictors with univariate analysis were then included in a multivariate model.
Results
The MOF patients' average age was 47 (standard deviation [SD] 15) years. Most patients had blunt injuries (51 patients, 78.1%), whereas 14 (21.9%) had open wounds. Most patients had triple (41.7%), double (33.3%) or single (16.7%) organ insufficiency. Only 8.3% of patients had 4 or more insufficient organs. The male:female ratio was 52:13, which is common for traumatic injuries. The average ISS score was 30.48 (SD 0.73), and the average SAPS II score was 39.62 (SD 13.05).
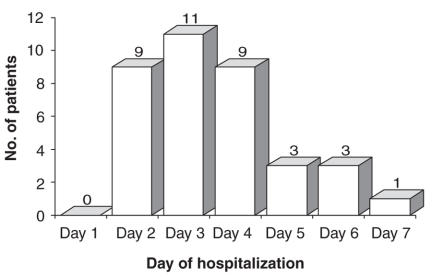
Early MOF appearing in the first 72 hours after the injury, was present in 20 patients (56%), whereas 16 patients (44%) had late MOF appearing 72 hours after the injury (Fig. 1).
FIG. 1. Time of multiple organ failure onset in patients with severe trauma.
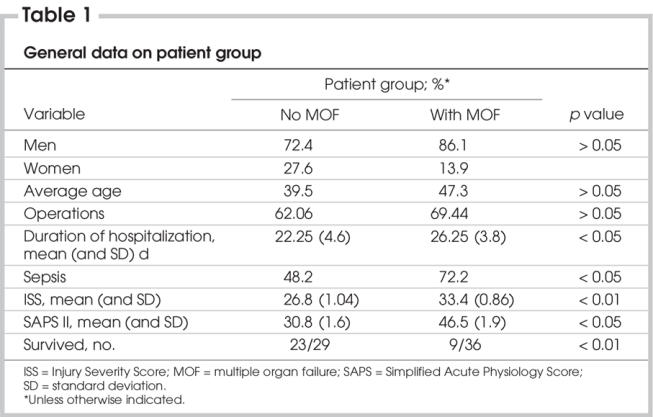
Table 1 shows the patients' distribution according to MOF presence in relation to sex, surgical treatment, duration of hospitalization, frequency of sepsis, ISS and SAPS II scores and survival. A highly statistically significant difference was noted in survival between groups with and without MOF.
Table 1
The number of SIRS variables was significantly different between the patient groups with and without MOF on day 5 of hospitalization, as shown in Figure 2. Further, a significant correlation was found between SIRS determinants and the appearance and progression of MOF in the first 5 of 7 observed days.
FIG. 2. Number of positive SIRS variables per hospital days in patients with and without MOF. MOF = multiple organ failure; SIRS = systemic inflammatory response syndrome; white star = p < 0.05; black star = p < 0.01.
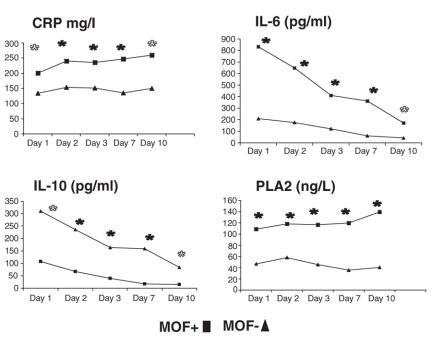
Average CRP (mg/L), IL-6 (pg/mL), IL-10 (pg/mL) and PLA2-II (ng/L) on the first, second, third, seventh and tenth day after the injury are shown in Figure 3. During the entire follow-up period, a statistically significant difference in average CRP and PLA2-II levels was noted between patients with and without MOF. Concentrations of IL-6 and IL-10 were significantly different on all days of hospitalization.
FIG. 3. Average CRP (mg/L), IL-6 (pg/mL), IL-10 (pg/mL) and PLA2-II (ng/L) in patients with and without MOF following severe trauma (Mann–Whitney U test). CRP = C-reactive protein; IL = interleukin; MOF = multiple organ failure; PLA2-II = phospholipase A2..
We used a multivariate logistic regression model to further investigate interactions between all statistically significant factors contributing to MOF, as perceived with univariate analysis. This approach led to the conclusion that the most significant predictors of MOF are the combined results of SIRS on the fourth day and IL-6 on the first day of hospitalization (SIRS 4 and IL-6.1). This model has predictive value of 89.66%.
Table 2 shows the average CRP (mg/L), IL-6 (pg/mL), IL-10 (pg/mL) and PLA2-II (ng/L) levels on the first, second, third, seventh and tenth day following the injury, depending on the number of damaged organs.
Table 2

Discussion
The high average ISS score in our group of patients reflects the organization of our health system, in which our hospital is responsible for the most severely injured patients. A significant number of these patients develop MOF. Experience suggests that MOF appears in 2 forms: early and late. Most studies consider the period within 72 hours of admission to be the upper limit for diagnosis of early MOF. MOF appearing after 72 hours is diagnosed as late. In our study, out of 36 patients with MOF, 55.6% had the early form. These data only refer to presentation of signs of failure of the first damaged organ or system, since a certain number of organ failures were identified even after the tenth day of hospitalization.
Respiratory insufficiency is almost always the first to appear, followed by cardiovascular decompensation. Formerly, renal insufficiency was the second most frequent failure. Hepatic failure is usually a late manifestation of MOF. The mortality rate follows the increase in the number of affected organs. It varies from 11% in patients with single organ system failure to 62% in patients with failure of 2 systems, as reported by some authors.13,14 Insufficiency of 3 or more organs almost always results in a lethal outcome, even with the best conditions for treatment.15 Apart from the order in which failures appear, their combination is also important. In a study of 1171 patients, lethal outcome after combined cardiac-respiratory failure occurred in 66.7% patients, after respiratory-hepatic failure, it occurred in 53.9%, and after hepatic-respiratory insufficiency, it occurred in 33.3%.1 In our study, 89% of patients with MOF had signs of respiratory failure, 28% had signs of renal failure and 32% had signs of cardiovascular decompensation, which is accompanied by an especially high mortality rate. Hepatic failure was also present in a significant number (34%), but it usually appeared later and resolved more quickly. In 83% of patients in our study, respiratory insufficiency appeared first, which is consistent with the findings of other authors.16 A smaller number of patients had renal failure (9%), cardiovascular insufficiency (5%) and cerebrovascular insufficiency (3%) as the first manifestation of MOF. Most of our patients had failure of 3 (41.7%), 2 (33.3%) or 1 (16.7%) organ system, and only 8.3% had 4 or more insufficient organs. The most frequent combination of organ failure in our patients was respiratory-renal failure and respiratory-hepatic failure. In patients with 3 or more affected organs, the most frequent combination was respiratory-renal-cardiovascular insufficiency, followed by respiratory-renal-hepatic failure.
The mortality rate in patients with MOF was high (75%). The average ISS value in our study was higher than reported by other authors in studies with similar mortality rates. In patients with failure of 2 organs, several studies reported a mortality rate of 42%,10 while another study reported a mortality rate of 35%.17 The mortality rate in patients with 2 insufficient organs was higher in our study (83%) than that reported by other authors. However, all patients with single organ failure survived.
In critically ill patients, serial measurements of CRP concentrations may help to identify those who require more aggressive interventions to avoid complications.18 All our patients with MOF had significantly higher CRP levels, compared with patients without MOF, indicating that CRP levels are a good early marker of morbidity in intensive care unit patients.
Lipolytic enzyme PLA2-II plays a significant role in the synthesis of lipid mediators, which, together with cytokines, are most important in the host response to infection or other insult such as trauma.19 It is important for a clinician to identify the patients with increased levels of PLA2-II and to observe whether these values are predictive of complications and outcome.20,21 Studies on the role of PLA2-II in different settings (multiple injury, acute pancreatitis, sepsis) indicated that phospholipase levels correlate well with disease severity and survival,10,22 Increased secretory PLA2-II activity is associated with the development of postinjury MOF.23 Most studies report that in the first 24 hours after trauma there is no significant increase of this enzyme.21 This is somewhat different from our findings, although in our study average levels of PLA2 for the first day of hospitalization were lower than for the following days. It should be emphasized, however, that most patients from remote regions of our country were admitted to the hospital after more time had elapsed, although always within 24 hours of the injury.
The plasma IL-6 level may be a marker of cytokine cascade and may reflect a complex inflammatory host response and the severity of disease (or injury).24 The ratio of IL-6 to IL-10 may be a predictive factor in SIRS.25
Some authors always include cytokine status when distributing injured patients according to severity of the injury and expected outcome.26–28 According to these models, cytokine concentrations are classified in 4 groups with adequate prognostic significance (number of points).29 Almost one-half of the patients in our study (45%) belonged to the third (IL-6 > 250 pg/L) and fourth (IL-6 > 500 pg/L) group, suggesting a bad prognosis. There are reports that IL-6 level on days 2 and 4 were significantly higher in MOF patients than in those without MOF.30 Some authors describe significant IL-6 increase on the first or even second day; however, most state that the window closes after 3 days, indicating that IL-6 levels have no prognostic value after that point.7
In vitro experiments show that human monocytes produce IL-10 after lipopolysaccharide stimulation but later than IL-6. The presence of anti–IL-10 antibodies in cell culture results in its increased production, thus implying the regulatory role of IL-10.31 Our study confirms dissapointing findings on its protective role. Its concentration has similar kinetics to IL-6 concentration kinetics, and average IL-6 and IL-10 serum concentrations were significantly different between groups on all days of hospitalization (Fig. 3).
Conclusions
IL-6 kinetics in the first days of hospitalization may suggest the development of MOF, even before clear clinical symptoms develop.
Average levels of IL-10 after the injury, even in the first 24 hours, indicate the development of MOF.
Average daily concentrations of PLA2-II can determine with significant confidence which patients will aquire MOF.
The kinetics of CRP concentration differ significantly between groups, depending on MOF development, especially from the second to the seventh day of hospitalization.
On the basis of our study results, it is possible to design predictive models for the development of organ failure. The most important parameters are serum IL-6 concentration on the first day of hospitalization and the number of positive SIRS criteria on the fourth day of hospitalization.
Contributors: Drs. Z. Lausevic and Stojimirovic designed the study. Drs. Z. and M. Lausevic and Krstic acquired data, which Drs. M. Lausevic, Trbojevic-Stankovic and Stojimirovic analyzed. Drs. M. Lausevic and Stojimirovic wrote the article, which Drs. Z. and M. Lausevic, Trbojevic-Stankovic and Krstic reviewed. All authors gave final consent for publication.
Competing interests: None declared.
Accepted for publication Apr. 23, 2007
Correspondence to: Dr. Z. Lausevic, Center for Emergency Surgery, Clinical Center of Serbia, 2 Paster St. Belgrade 11000, Serbia and Montenegro; fax +381-11-2437623; zlaus@eunet.yu
References
- 1.Regel G, Grotz M, Weltner T, et al. Pattern of organ failure following severe trauma. World J Surg 1996;20:422-9. [DOI] [PubMed]
- 2.Bernard GR. Quantification of organ dysfunction: seeking stardandization. CritCare Med 1998;26:1767-8. [DOI] [PubMed]
- 3.Ciesla DJ, Moore EE, Johnson JL, et al. A 12-year prospective study of postinjury multiple organ failure: has anything changed. Arch Surg 2005;140:432-8. [DOI] [PubMed]
- 4.Hildebrand F, Pape HC, Krettek C. The importance of cytokines in the posttraumatic inflammatory reaction. Unfallchirurg 2005;108:793-803. [DOI] [PubMed]
- 5.Keel M, Trentz O. Pathophysiology of polytrauma. Injury 2005;36:691-709. [DOI] [PubMed]
- 6.American College of Chest Physicians/ Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992;20:864-74. [PubMed]
- 7.American College of Chest Physicians. National Institute of Allergy and Infectious Disease, and National Heart, Lung, and Blood Institute Workshop. From the bench to the bedside: the future of sepsis research, a workshop executive summary. Chest 1997;111:744-53. [PubMed]
- 8.Keel M, Trentz O. Pathophysiology of polytrauma. Injury 2005;36:691-709. [DOI] [PubMed]
- 9.Ciesla DJ, Moore EE, Johnson JL, et al. Decreased progression of postinjury lung dysfunction to the acute respiratory distress syndrome and multiple organ failure. Surgery 2006;140:640-7. [DOI] [PubMed]
- 10.Dajak M, Ignjatovic S, Majkic-Singh N, et al. Prognostic value of Phospholipase Al group II, C-reactive protein and Symplified Acute Physiological Score II in intensive care patients. Clin Lab (Zaragoza) 2006;52:387-92. [PubMed]
- 11.Sauaia A, Moore FA, Moore EE, et al. Multiple organ failure can be predicted as early as 12 hours after injury. J Trauma 1998;45:291-303. [DOI] [PubMed]
- 12.Waydhas C, Nast-Kolb D, Trupka A, et al. Posttraumatic inflammatory response, secondary operations, and late multiple organ failure. J Trauma 1996;40:624-31. [DOI] [PubMed]
- 13.Moore FA, Sauaia A, Moore EE, et al. Postinjury multiple organ failure: a bimodal phenomenon. J Trauma 1996;40:501-12. [DOI] [PubMed]
- 14.Sauaia A, Moore FA, Moore EE, et al. Early risk factors for postinjury multiple organ failure. World J Surg 1996;20:392-400. [DOI] [PubMed]
- 15.Rixen D, Siegel JH, Friedman HP. “Sepsis/SIRS,'' physiologis slassification, severity stratification, relation to cytokine elaboration and outcome prediction in posttrauma critical illness. J Trauma 1996;41:581-98. [DOI] [PubMed]
- 16.Ciesla DJ, Moore EE, Johnson JL, et al. The role of the lung in postinjury multiple organ failure. Surgery 2005;138:749-57. [DOI] [PubMed]
- 17.Zimmerman JE, Knaus WA, Sun X, et al. Severity stratification and outcome prediction for multisystem organ failure and dysfunction. World J Surg 1996;20:401-5. [DOI] [PubMed]
- 18.Lobo SMA, Lobo FRM, Peres Bota D. C-reactive protein levels correlate with mortality and organ failure in critically ill patients. Chest 2003;123:2043-9. [DOI] [PubMed]
- 19.Kellermann W, Frentzel-Beyme R, Welte M, et al. Phospholipase A in acute lung injury after trauma and sepsis: its relation to the inflammatory mediators PMN-elastase, C3a, and neopterin. Klin Wochenschr 1989;67:190-5. [DOI] [PubMed]
- 20.Nevalainen TJ. Serum phospholipases A2 in inflammatory diseases. Clin Chem 1993;39:2453-9. [PubMed]
- 21.Waydhas C, Nast-Kolb D, Duswald KH, et al. Prognostic value of serum phospholipase A2 in the multitraumatized patient. Klin Wochenschr 1989;67:203-6. [DOI] [PubMed]
- 22.Buchler M, Deller A, Malfertheiner P, et al. Serum phospholipase A2 in intensive care patients with peritonitis, multiple injury, and necrotizing pancreatitis. Klin Wochenschr 1989;67:217-21. [DOI] [PubMed]
- 23.Partrick DA, Moore EE, Silliman CC, et al. Secretory phospholipase A2 activity correlates with postinjury multiple organ failure. Crit Care Med 2001;29:989-93. [DOI] [PubMed]
- 24.Patrick DA, Moore FA, Moore EE, et al. The inflammatory profile of interleukin-6, interleukin-8 and soluble cell adhesion molecule-1 in post-injury multiple organ failure. Am J Surg 1997;172:425-31. [DOI] [PubMed]
- 25.Miyaoka K, Iwase M, Suzuki R, et al. Clinical evaluation of circulating interleukin-6 and interleukin-10 levels after surgery-induced inflammation. J Surg Res 2005;125:144-50. [DOI] [PubMed]
- 26.Suffredini AF. Current procpets for the treatment of clinical sepsis. Crit Care Med 1994;22:12-8. [PubMed]
- 27.Bernard GR. Sepsis trials: intersection of investigation, regulation, funding, and practice. Am J Respir Crit Care Med 1995;152:4-10. [DOI] [PubMed]
- 28.Borden EC, Chin P. Interleukin-6: a cytokine with potential diagnostic and therapeutic roles. J Lab Clin Med 1994;123:824-9. [PubMed]
- 29.Bone RC. Toward a theory regarding the pathogenesis of the systemic inflammatory response syndrome: what we know and do not know about cytokine regulation. Crit Care Med 1996;24:163-72. [DOI] [PubMed]
- 30.Spindler-Vesel A, Wraber B, Vovk I, et al. Intestinal permeability and cytokine inflammatory response in multiply injured patients. J Interferon Cytokine Res 2006;26:771-6. [DOI] [PubMed]
- 31.Marchant A, Deviere J, Byl B, et al. Interleukin-10 production during septicaemia. Lancet 1994;343:707-8. [DOI] [PubMed]