Abstract
Objective:
To answer the following clinical questions: (1) Is poor postural control associated with increased risk of a lateral ankle sprain? (2) Is postural control adversely affected after acute lateral ankle sprain? (3) Is postural control adversely affected in those with chronic ankle instability?
Data Sources:
PubMed and CINAHL entries from 1966 through October 2006 were searched using the terms ankle sprain, ankle instability, balance, chronic ankle instability, functional ankle instability, postural control, and postural sway.
Study Selection:
Only studies assessing postural control measures in participants on a stable force plate performing the modified Romberg test were included. To be included, a study had to address at least 1 of the 3 clinical questions stated above and provide adequate results for calculation of effect sizes or odds ratios where applicable.
Data Extraction:
We calculated odds ratios with 95% confidence intervals for studies assessing postural control as a risk factor for lateral ankle sprains. Effect sizes were estimated with the Cohen d and associated 95% confidence intervals for comparisons of postural control performance between healthy and injured groups, or healthy and injured limbs, respectively.
Data Synthesis:
Poor postural control is most likely associated with an increased risk of sustaining an acute ankle sprain. Postural control is impaired after acute lateral ankle sprain, with deficits identified in both the injured and uninjured sides compared with controls. Although chronic ankle instability has been purported to be associated with altered postural control, these impairments have not been detected consistently with the use of traditional instrumented measures.
Conclusions:
Instrumented postural control testing on stable force plates is better at identifying deficits that are associated with an increased risk of ankle sprain and that occur after acute ankle sprains than at detecting deficits related to chronic ankle instability.
Keywords: ankle sprains, balance, chronic ankle instability, stabilometry
Lateral ankle sprains are extremely common among physically active individuals. Sprains to the lateral ankle ligaments frequently result in pathologic laxity and sensorimotor deficits about the ankle. Poor postural control performance, one facet of sensorimotor function, has been associated with lateral ankle instability since Freeman's landmark works in the mid-1960s.1,2 It has been suggested that lateral ankle instability is often associated with poor postural control, which can be defined as the inability to maintain stability above a narrow base of support in single-limb stance2–4; however, no uniform consensus exists in the published literature. Numerous noninstrumented and instrumented measures of postural control in single-limb stance have been reported in the ankle instability literature over the past 4 decades, with instrumented force plate measures becoming the gold standard of assessment.
Instrumented measures of postural control have been used in an attempt to predict ankle sprain risk and to assess sensorimotor deficits after acute ankle sprains and in those with chronic ankle instability (CAI). Yet the disparate methods and measures reported in the literature can make the interpretation of this body of literature difficult.5 Inconsistent findings in the ankle instability and postural control literature make it difficult for health care providers to render informed clinical decisions when evaluating and treating patients with ankle instability. To date, no systematic reviews have thoroughly summarized the research literature as it relates to instrumented postural control testing, lateral ankle sprains, and CAI. A comprehensive summary of research findings in this area will allow health care providers to make clinical decisions relating to ankle instability and postural control that are informed by the best available evidence. Therefore, the purposes of this systematic review are to answer the following clinical questions: (1) Is poor postural control associated with increased risk of a lateral ankle sprain? (2) Is postural control adversely affected after acute lateral ankle sprain? (3) Is postural control adversely affected in those with CAI?
Methods
Search Strategy
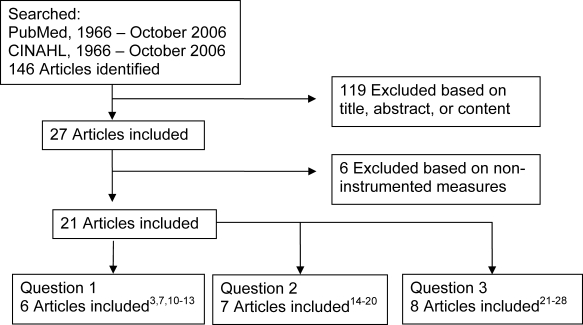
We searched PubMed and CINAHL entries from 1966 through October 2006 using the terms ankle sprain, ankle instability, balance, chronic ankle instability, functional ankle instability, postural control, and postural sway. Relevant articles were also identified by cross-referencing the citation lists of articles identified in the electronic search. A total of 144 articles were identified (Figure 1).
Figure 1. Flow chart for selecting articles to be included in the systematic review to answer our 3 questions. Article reference numbers are superscripted.
Criteria for Selecting Studies
Only studies assessing postural control measures in participants on a stable force plate performing the modified Romberg test were included. We chose to only investigate studies that used the Romberg test on a stable surface because we were most interested in assessing the relationships between ankle instability and “static” postural control; studies assessing static postural control are most commonly reported in the ankle instability literature. To be included, a study had to address at least 1 of the 3 clinical questions stated above and provide adequate results for calculation of effect size or odds ratio where applicable.
Assessment of Methodologic Quality
Included studies were evaluated using the PEDro scale.6 Consensus regarding the PEDro score for each article was agreed upon by both authors.
Data Extraction and Statistical Analysis
For the assessment of predictive ability of postural control scores, 2 types of effect measures were calculated based on the data reported in the original articles. Where possible, we calculated odds ratios for sustaining an ankle sprain between those in different categories based on their postural control measures (ie, group with lowest third of performance scores versus highest third of performance scores7). In addition, we calculated effect sizes (Cohen d) for postural control measures between those who went on to sustain acute ankle sprains and those who did not. The strength of effect sizes was interpreted using the guidelines described by Cohen,8 with values less than 0.4 interpreted as weak, from 0.41 to 0.7 as moderate, and more than 0.7 as strong. For both odds ratio and effect size estimates, 95% confidence intervals (CIs) were calculated around the point estimates.
For the comparisons of postural control performance deficits related to acute ankle sprains and CAI, estimates of effect size (Cohen d) and 95% CIs were made (1) within involved and uninvolved limbs in those with unilateral ankle injuries, and (2) between the pathologic group and the healthy control group. It was not possible to compare both factors from all included studies.
Lastly, the quality of evidence used to answer each of the 3 questions was assessed with the Strength of Recommendation Taxonomy (SORT).9 The SORT level of recommendations range from 1 to 3, with 1 indicating good-quality, patient-oriented evidence; 2 indicating limited-quality, patient-oriented evidence; and 3 indicating non–patient-oriented evidence. The SORT strength of recommendations range from A through C, with A indicating that the recommendation was based on consistent and good-quality, patient-oriented evidence; B that it was based on inconsistent or limited-quality, patient-oriented evidence; and C that it was based on evidence other than patient-oriented evidence.9
Results
Was Poor Postural Control Associated With Increased Risk of Lateral Ankle Sprain?
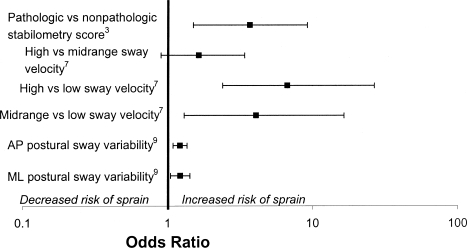
Six articles3,7,10–13 met the inclusion criteria to answer this question (Table 1). The mean PEDro score for these articles was 5.6. Three articles3,7,11 provided sufficient data to allow calculation of odds ratios (Figure 2), and 5 articles7,10–13 allowed calculation of effect sizes (Figure 3). The point measures of the odds ratios ranged from 1.22 to 6.70, indicating that athletes with poorer postural control measures were at increased risk of ankle sprain. Only 1 of the 6 comparisons had a 95% CI that crossed 1.0 for the odds ratio, and this comparison was between groups representing the best and middle tertiles of postural control performance in the study by McGuine et al.7 Thus, the risk of ankle sprain did not increase for the group with poorer postural control. In contrast, when the lower boundary of the odds ratio CI was greater than 1.0, the risk of ankle sprain increased for the group with poorest postural control.
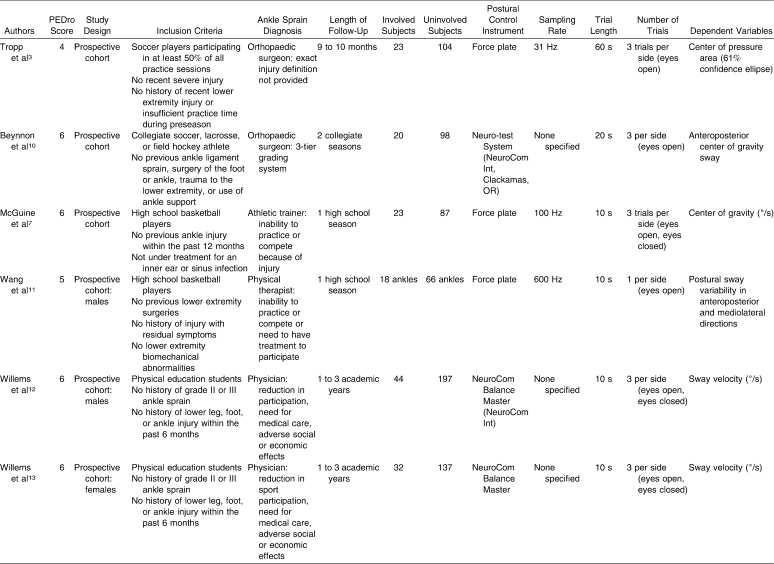
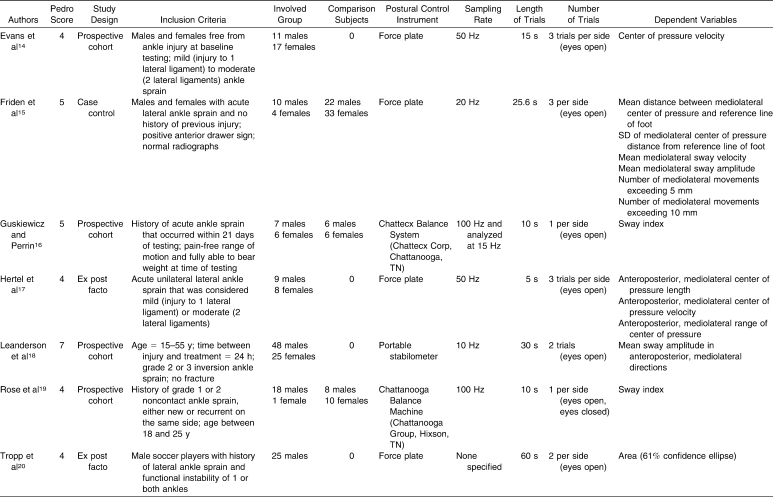
Table 1.
Articles Included to Answer the Question, “Was Poorer Postural Control Associated With Increased Risk of Ankle Sprain?”
Figure 2. Was poor postural control associated with increased risk of ankle sprain? Odds ratios and 95% confidence intervals are shown for postural control as a risk factor for lateral ankle sprains. Individuals who sustained a first-time ankle sprain had worse postural control measures than those who did not go on to sustain sprains. ML indicates mediolateral; AP, anteroposterior. Article reference numbers are superscripted.
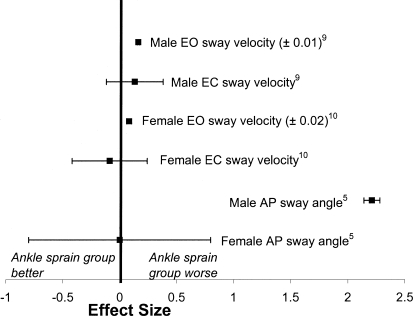
Figure 3. Was poor postural control associated with increased risk of ankle sprain? Effect sizes and 95% confidence intervals compare those who went on to sprain their ankles and those who did not. Findings are inconsistent as to whether those who sustained an ankle sprain had poorer postural control than those who did not. EO indicates eyes open; EC, eyes closed. Article reference numbers are superscripted.
The results of the effect size analyses are less consistent, with point estimates ranging from −0.09 to 2.21 and positive effect sizes indicating worse postural control in athletes who went on to sprain their ankles. In this subset of studies, 3 of the 6 comparisons had CIs that crossed zero. When the lower boundary of the effect size CI crossed zero, whether or not those who went on to sprain their ankles had worse instrumented postural control performance scores than those who did not suffer sprains was unclear. Based on this evidence, it appears that a consensus (albeit not unanimous) of evidence indicates that poor postural control was associated with increased risk of ankle sprain. The SORT level of evidence was 2 because the methodologic quality of included articles was not consistently high, with a grade of recommendation of B because of some inconsistent findings.
Was Postural Control Adversely Affected After Acute Lateral Ankle Sprain?
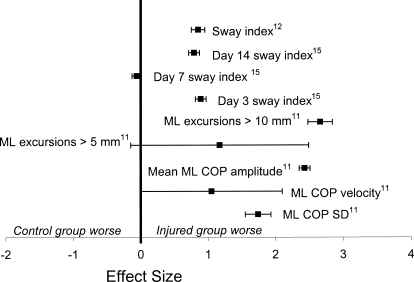
Seven articles14–20 met the inclusion criteria to answer this question (Table 2). The mean PEDro score for these articles was 4.7. Authors of 3 articles15,16,19 examined group differences between an acute lateral ankle sprain group and a healthy control group (Figure 4). The point measures of effect size for group comparisons on the injured side ranged from −0.25 to 2.66, with a positive value indicating poorer postural control in the injured group than the uninjured group. Most of the effect size values were moderate to strong, with CIs that did not cross zero. Comparisons between the uninjured limbs of the injured group and the matched limbs in the control group revealed effect size point estimates ranging from 0.28 to 1.21, with the majority having CIs that did not cross zero. Thus, deficits in postural control were seen in both the injured and uninjured limbs of participants sustaining unilateral ankle sprains compared with the control group.
Table 2.
Articles Included to Answer the Question, “Is Postural Control Adversely Affected by Acute Lateral Ankle Sprain?”
Figure 4. Was postural control adversely affected by acute lateral ankle sprain? Effect sizes and 95% confidence intervals compare postural control measures for injured groups (acute lateral ankle sprain) with healthy groups. Postural control was adversely affected by acute lateral ankle sprain compared with healthy controls. ML indicates mediolateral; COP, center of pressure. Article reference numbers are superscripted.
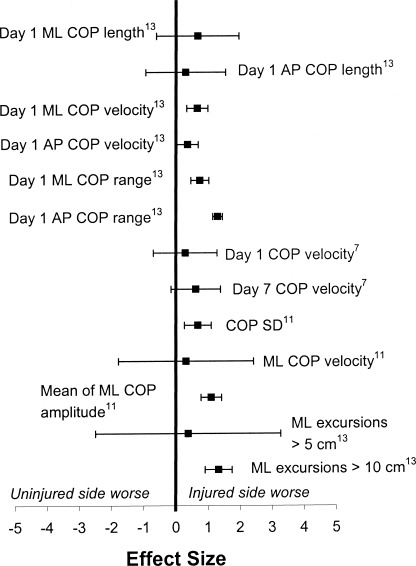
Authors of 6 articles14,15,17–20 examined side differences between the acutely injured limb and the contralateral healthy limb in participants with unilateral ankle sprains (Figure 5). The effect size point measures for side comparisons ranged from −0.41 to 2.13, with a positive value indicating poorer postural control in the injured limb. Most effect sizes were moderately to strongly positive, but several had CIs that crossed zero. Based on this evidence, it appears that postural control was adversely affected in both the injured and uninjured sides in individuals with unilateral acute ankle sprains. The SORT level of evidence was 1, with a grade of recommendation of A. However, there is inconclusive evidence as to whether side-to-side differences in postural control exist between the injured and uninjured limbs after acute ankle sprains. For the intralimb comparison of patients with unilateral ankle sprains, the SORT level of evidence was 2, with a grade of recommendation of B.
Figure 5. Was postural control adversely affected by acute lateral ankle sprain? Effect sizes and 95% confidence limits compare postural control performance between injured and uninjured limbs in those with acute lateral ankle sprains. Whether actual deficits in postural control exist when comparing the injured with the uninjured side in those who suffered acute lateral ankle sprain is inconclusive. The results of Tropp et al20 are not shown here due to the large confidence intervals associated with the point measure of effect size (effect size for COP area = 0.23, 95% confidence interval = −51.22, 51.48). ML indicates mediolateral; COP, center of pressure; AP, anteroposterior. Article reference numbers are superscripted.
Was Postural Control Adversely Affected in Those With Chronic Ankle Instability?
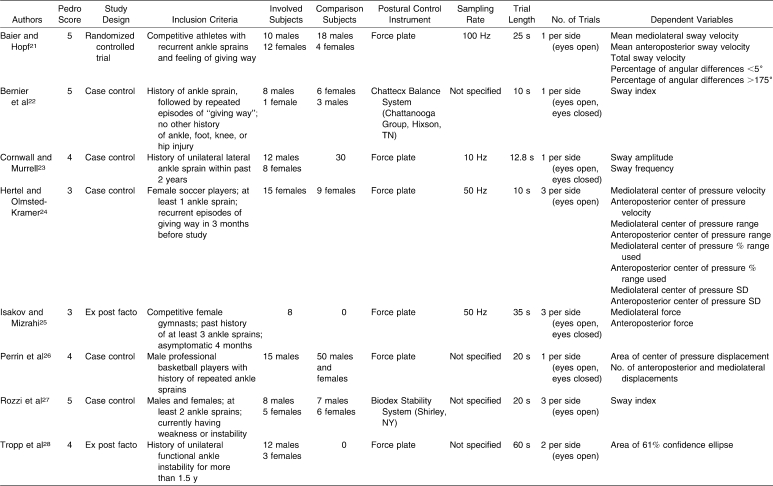
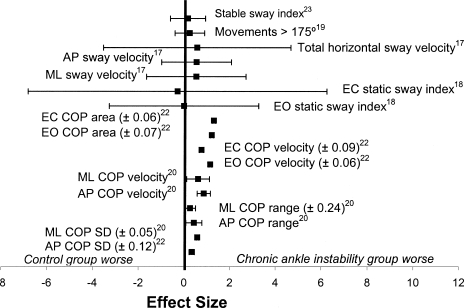
Authors of 8 articles21–28 met the inclusion criteria to answer this question (Table 3). The mean PEDro score for these articles was 4.3. Investigators in 7 studies21–24,26–28 examined differences between a CAI group and a group of healthy controls (Figure 6). The point estimates of the group comparison effect sizes ranged from −0.29 to 1.31, with a positive effect size indicating worse postural control in the CAI group and a negative effect size indicating poorer postural control in the control group. Most of the effect sizes for group comparisons were positive, ranging from weak to strong effects; however, several of the CIs around these point measures crossed zero.
Table 3.
Included Articles to Answer the Question: “Is Postural Control Adversely Affected by Chronic Ankle Instability?”
Figure 6. Was postural control adversely affected by chronic ankle instability? Effect sizes and 95% confidence intervals compare healthy and chronic ankle instability groups. Whether postural control deficits existed in those with CAI compared with healthy controls is unclear. Effect sizes for Tropp28 (COP area = 0.96, 95% confidence interval [CI] = −24.91, 26.83) and Cornwall and Murrell23 (anteroposterior COP length = .29, 95% CI = −17.60, 18.18; mediolateral COP length = .46, 95% CI = −17.43, 18.35) are not shown due to wide CIs. AP indicates anteroposterior; ML, mediolateral; EC, eyes closed; EO, eyes open; COP, center of pressure. Article reference numbers are superscripted.
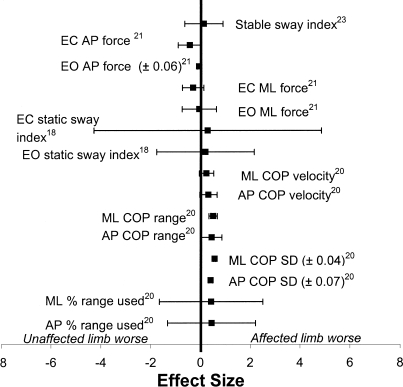
Authors of 5 articles22,24,25,27,28 studied differences between limbs of a group reporting unilateral CAI (Figure 7). The point measures of these effect sizes ranged from −0.47 to 0.57, with a positive effect size indicating poorer postural control in the involved limb than the uninvolved limb. Most of the CIs around these point measures crossed zero. Therefore, postural control appeared to be adversely affected in the presence of CAI when compared with a healthy sample, but the extent of the effect was uncertain because of inconsistent results with small effect sizes and large CIs. In contrast to acute ankle sprains, evidence was not conclusive that unilateral CAI affected the postural control of the uninvolved limb. The SORT level of evidence was a 2, with a grade of recommendation of B.
Figure 7. Was postural control adversely affected by chronic ankle instability? Effect sizes and 95% confidence intervals compare affected and unaffected limbs in those with unilateral chronic ankle instability. Whether postural control deficits exist in the affected limb versus the unaffected limb in those with unilateral CAI is unclear. Results of Tropp28 are not displayed due to wide confidence intervals around the effect size (COP area = .26, 95% confidence interval = −32.54, 33.06). EC indicates eyes closed; EO, eyes open; AP, anteroposterior; ML, mediolateral. Article reference numbers are superscripted.
Discussion
Was Poor Postural Control Associated With Increased Risk of Lateral Ankle Sprain?
Six groups3,7,10–13 who answered this question provided good representation of a heterogeneous population of males and females of various ages in various sports. An important consideration in injury predictor studies is whether participants were equal at baseline on the most important measures of interest. Within the included studies, the participants were free from ankle injury for at least 12 months. No differences were noted in instrumented postural control measures between athletes who had never suffered an ankle sprain and athletes who had sustained their most recent ankle sprain more than 12 months ago.29 Of the included studies, only Tropp et al3 found that players with a history of ankle sprains had no difference in the incidence of ankle injuries in the following season. This is important because several investigators29–31 have reported that the primary risk factor in suffering an ankle sprain is a previous history of sprain.
When postural control performance in single-limb stance was used as the sole predictor of ankle sprain risk, consistent predictive results were found.3,7 However, when multiple predictors of ankle sprain risk were used, this was not the case.9,12,13 For example, in a study of numerous other potential predictors, including lower extremity alignment, muscle strength and reaction time, and ankle laxity, Beynnon et al10 noted that postural control performance did not predict ankle sprain risk in male and female collegiate athletes. In males, increased talar tilt predicted ankle sprain risk, and in females, increased tibial varum and calcaneal eversion range of motion were predictors. Conversely, in a study examining the roles of postural control, ankle strength, and flexibility in predicting risk of ankle sprain, Wang et al11 found that poor postural control performance was the best predictor of ankle sprain. Yet postural control performance only accounted for approximately 20% of the variance in increased injury risk and, curiously, the authors did not recommend it as an effective injury predictor. The interaction between single-limb postural control and other potential risk factors is not clearly understood, as indicated by the conflicting results of these multifactorial studies.
Measures of postural control varied within these studies. Willems et al12,13 and Beynnon et al10 used center of gravity (COG) excursion measures in single-limb stance. These measures did not detect postural control differences between participants who went on to sprain their ankles and those who did not. Tropp et al3 and Wang et al11 used center of pressure (COP) excursion measures and did identify an increased risk of ankle sprain in those with poorer scores. The COG excursion measured the movement of the vertical ground reaction force in relation to the force plate during single-limb stance. The COP excursion measured the 3-dimensional interaction between the foot and the force plate as the body attempted to maintain itself over a fixed base of support. The COP measures appeared to be more sensitive in detecting postural control impairments in those at increased risk of ankle sprain. It is also important to note that Willems et al12,13 identified different components of postural control in double-limb stance that were more strongly related to increased risk of ankle sprain. Males with decreased directional control and females with decreased endpoint excursion in double-limb stance, as measured by the NeuroCom Balance Master (NeuroCom Int, Clackamas, OR), were at greater risk of sprain.12 These tests indicate diminished volitional postural control and represent more challenging tasks to the sensorimotor system in keeping the center of gravity within the base of support.
The inconsistent findings of the included studies may also be due to different definitions of lateral ankle sprain and variations in the length of time participants were followed after baseline testing. The definition of ankle sprain varied across studies, from not being fully described3 to using descriptions in previously published grading systems.10,12,13 Some injury definitions required the ankle injury to prevent a player from participating in a practice or game,7 whereas others allowed players to continue sport participation if they required treatment.11 In all these studies, ankle sprains were diagnosed by an athletic trainer,9 physiotherapist,10 or physician.3,7,8,11 The time participants were followed for ankle sprain after baseline testing varied from the length of a single high school sports season9,10 to up to 3 academic years.7,11 Those studies with follow-up times of less than 1 year3,7,11 showed more consistent findings of poor postural control performance as an injury risk factor than those studies with longer follow-up periods.7,8,11
Although agreement within the literature suggests that poor postural control was associated with an increased risk of ankle sprain, some findings were inconsistent with the traditional measures of postural control in single-limb stance. The choice of measurement technique and predictive model may significantly confound the relationship between postural control and ankle sprain risk. The task of static single-limb stance on a force plate may not be challenging enough to elucidate differences in postural control among individuals who are at greater risk of ankle sprain. More large-scale, high-quality prospective studies are needed to test this possibility. Clinically, postural control can be easily assessed in an effort to identify people who may be at greater risk for sustaining an ankle sprain. A better understanding of these deficits may allow us to more effectively target these people for a prevention program that lessens the ankle sprain risk.
Was Postural Control Adversely Affected After Acute Lateral Ankle Sprain?
The included studies provided a good representation of sex and severity of ankle sprain.14–20 Evidence is strong that postural control deficits were present in individuals after acute lateral ankle sprain. These deficits were detected regardless of the differences in instrumented postural control measurement and were most apparent when acutely injured subjects were compared with a healthy control group.
In a true prospective study, Evans et al14 identified postural control deficits present in both the injured and uninjured limbs of individuals after unilateral ankle sprains. Comparisons to baseline preinjury measures revealed that postural control deficits resolved at the second follow-up (7 days) for the uninjured limbs but remained for at least 4 weeks after injury in the injured limbs. The impairments seen in the injured limbs were greater than those seen in the uninjured limbs. Friden et al15 found diminished postural control in the injured and uninjured limbs of athletes after acute ankle sprains compared with a reference group. Diminished postural control in both limbs of individuals after acute ankle sprain helps to explain the inconsistencies in side-to-side deficits. Tropp et al20 first proposed a central change in postural control due to unilateral ankle sprain. It is likely that side-to-side differences within acutely injured participants were not consistently present in the studies we reviewed because central impairments led to bilateral postural control deficits after acute lateral ankle sprain.
Baseline preinjury measures of postural control are essential for confirming these deficits. Based on these findings, we recommend that the uninjured limb not be used as a control limb when making side-to-side comparisons for impaired postural control after acute ankle sprains. Instead, we recommend making comparisons with baseline measures from the injured limb or comparisons with a healthy reference group. Further research is necessary to identify the potential mechanisms related to the central changes associated with impaired postural control in single-limb stance bilaterally after acute ankle sprain.
Freeman1 and Freeman et al2 initially proposed that the postural control deficits after acute ankle sprains were due to damaged ligamentous and articular mechanoreceptors in the injured ligaments. However, the deficits may indicate a larger motor control deficit.32 Postural control deficits have been detected in both injured and uninjured limbs after acute unilateral ankle sprain.14 Alterations in muscles proximal to the ankle have also been identified in those with a history of ankle sprain.32–34 Bullock-Saxton et al33 and Bullock-Saxton34 found alterations in hip extensor activity in both injured and uninjured limbs after severe unilateral ankle sprains. These proximal alterations may be related to kinetic and kinematic changes noted in single-limb drop landings35 and the Star Excursion Balance Test performance of those with repetitive ankle sprains.36 If central and proximal deficits occur after ankle sprains, local rehabilitation strategies that focus only on restoring range of motion and strength of the muscles surrounding the injured ankle may not be adequate to reduce the risk of injury recurrence. Strategies that instead focus on restoring global coordination, such as dynamic balance training, may produce improvement in treatment outcomes related to lateral ankle sprain.27,30 Several investigators have found improvements in both trained and untrained limbs after a unilateral balance training intervention.27,37,38 Based on this evidence, we recommend implementation of balance training for the uninjured limb and training the proximal musculature during the period of restricted weight-bearing and function for the injured ankle, as well as closed chain exercises to challenge the entire injured limb once full weight-bearing is possible in an effort to prevent recurrent ankle sprains.
Was Postural Control Adversely Affected in Those With Chronic Ankle Instability?
Based on our systematic review, it is unclear whether postural control deficits were present in individuals with CAI when compared with a control group. Moderate to strong effect sizes showed such differences, but the CIs around these point measures were very wide and tended to cross zero. The relatively small sample sizes in the included studies and discrepancies in the definition of CAI across studies may have been factors. It was also unclear whether side-to-side deficits were present in individuals with unilateral CAI.
The contributing factors to CAI are not well understood.39 Most commonly, CAI has been defined as a history of an ankle sprain followed by several episodes of recurrent sprains or the feeling of the ankle “giving way.”39 However, inconsistencies in the reported inclusion and exclusion criteria for establishing CAI status across the included studies are troubling. Clearly, more uniform inclusion and exclusion criteria for CAI across studies are needed. There were relatively small sample sizes (8 to 22 participants) consisting of relatively young, healthy adults who were physically active at the time of the study.21–28 The subtle deficits in postural control that may contribute to CAI have not been consistently detected by instrumented measures of static postural control in single-limb stance. The lack of consistent criteria for CAI, along with the various sampling rates, trial time lengths, and dependent measures used for instrumented postural control testing, make comparisons across these studies difficult and comprehensive conclusions hard to draw.
All the participants in these studies were able to successfully complete the task of standing on one limb during the trials that were analyzed. However, none of the authors reported or compared the number of failed trials between healthy and CAI groups. The subtle deficit in postural control may not be detected in the successful trials but in the number of times an individual had to repeat trials after failed attempts. Freeman1 and Freeman et al2 noted balance deficits based on the participant and examiner reports of impaired postural control in single-limb stance in those with CAI. Objective reports of postural impairments associated with CAI through the Balance Error Scoring System have also shown promise in detecting differences between those with and without CAI.40 The Balance Error Scoring System is used to evaluate how many postural errors a person commits in attempting to maintain postural control over a period of time on stable and unstable surfaces in single-leg and tandem-leg stance. Examining postural control that leads to failure in CAI may be more beneficial than examining when individuals succeed.
As stated above, the traditional measures and techniques of instrumented postural control assessment may not be sensitive enough to detect these deficits associated with CAI. A recent development in postural control assessment in those with CAI is examining the spatiotemporal characteristics of the COP during single-limb stance.24,41 Time to boundary (TTB), a novel instrumented force plate measure derived from the dynamic systems theory of motor control, examines the intrinsic components of COP associated with changes in direction relative to the boundaries of the base of support. The TTB estimates the amount of time the sensorimotor system has to make a postural correction in order to maintain the body over its base of support.24,40–44 Less TTB indicates diminished postural control. This measurement technique detects different components of postural control than the traditional measures such as COP velocity and range.41 Hertel and Olmsted-Kramer24 established TTB deficits in individuals with unilateral CAI compared with healthy individuals. Thus, those with CAI had less time to make postural corrections in single-limb stance. These TTB deficits were also detected in the unaffected limbs of those with unilateral CAI when compared with healthy controls. These findings may point toward similar bilateral motor control deficits previously identified in those with acute ankle sprains.
As discussed previously, after an acute sprain, clear deficits in postural control in both the injured and uninjured limbs have been measured with traditional measures of COP. However, these measures were not different from baseline values by approximately 4 weeks.14 The deficits in postural control associated with CAI appear to be more subtle than with acute sprains, and more complex functional tasks may allow for better identification of these deficits. Postural control deficits have been reported with more challenging postural control tasks, such as time to stabilization after a jump-landing task45 and the Star Excursion Balance Test (a test of dynamic balance).36,46,47 In these techniques, participants were asked to perform more demanding tasks that emphasize maintaining postural control during dynamic activities. These measures have shown promise in detecting postural control impairments associated with CAI.
Postural control deficits in those with CAI have not been consistently detected with traditional measures of postural control in single-limb stance. Therefore, the clinical diagnosis of CAI should not be based solely on static postural control testing with traditional force plate measures. More challenging tasks, such as the Star Excursion Balance Test, and functional tasks, such as jump landings, may demonstrate more clinically relevant detection of postural control impairments related to CAI.
Conclusions
Poor postural control is most likely associated with an increased risk of sustaining an acute ankle sprain. Postural control is clearly impaired after acute lateral ankle sprains, with deficits identified in both the injured and uninjured limbs compared with controls. Although CAI has been purported to be associated with altered postural control, these impairments have not been detected consistently with the use of traditional instrumented measures.
Footnotes
Patrick O. McKeon, PhD, ATC, CSCS, and Jay Hertel, PhD, ATC, FACSM, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
References
- 1.Freeman M.A. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47(4):669–677. [PubMed] [Google Scholar]
- 2.Freeman M.A, Dean M.R, Hanham I.W. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–685. [PubMed] [Google Scholar]
- 3.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16(1):64–66. [PubMed] [Google Scholar]
- 4.Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6(6):833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- 5.Riemann B.L. Is there a link between chronic ankle instability and postural instability. J Athl Train. 2002;37(4):386–393. [PMC free article] [PubMed] [Google Scholar]
- 6.Maher C.G, Sherrington C, Herbert R.D, Moseley A.M, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 7.McGuine T.A, Greene J.J, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10(4):239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; p. 1988. [Google Scholar]
- 9.Ebell M.H, Siwek J, Weiss B.D, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 10.Beynnon B.D, Renstrom P.A, Alosa D.M, Baumhauer J.F, Vacek P.M. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19(2):213–220. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 11.Wang H.K, Chen C.H, Shiang T.Y, Jan M.H, Lin K.H. Risk-factor analysis of high school basketball-player ankle injuries: a prospective controlled cohort study evaluating postural sway, ankle strength, and flexibility. Arch Phys Med Rehabil. 2006;87(6):821–825. doi: 10.1016/j.apmr.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 12.Willems T.M, Witvrouw E, Delbaere K, Mahieu N, De Bourdeaudhuij I, De Clercq D. Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med. 2005;33(3):415–423. doi: 10.1177/0363546504268137. [DOI] [PubMed] [Google Scholar]
- 13.Willems T.M, Witvrouw E, Delbaere K, Philippaerts R, De Bourdeaudhuij I, De Clercq D. Intrinsic risk factors for inversion ankle sprains in females: a prospective study. Scand J Med Sci Sports. 2005;15(5):336–345. doi: 10.1111/j.1600-0838.2004.00428.x. [DOI] [PubMed] [Google Scholar]
- 14.Evans T, Hertel J, Sebastianelli W. Bilateral deficits in postural control following lateral ankle sprain. Foot Ankle Int. 2004;25(11):833–839. doi: 10.1177/107110070402501114. [DOI] [PubMed] [Google Scholar]
- 15.Friden T, Zatterstrom R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17(1):118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- 16.Guskiewicz K.M, Perrin D.H. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23(5):326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- 17.Hertel J, Buckley W.E, Denegar C.R. Serial testing of postural control after acute lateral ankle sprain. J Athl Train. 2001;36(4):363–368. [PMC free article] [PubMed] [Google Scholar]
- 18.Leanderson J, Bergqvist M, Rolf C, Westblad P, Wigelius-Roovers S, Wredmark T. Early influence of an ankle sprain on objective measures of ankle joint function: a prospective randomised study of ankle brace treatment. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):51–58. doi: 10.1007/s001670050120. [DOI] [PubMed] [Google Scholar]
- 19.Rose A, Lee R.J, Williams R.M, Thomson L.C, Forsyth A. Functional instability in non-contact ankle ligament injuries. Br J Sports Med. 2000;34(5):352–358. doi: 10.1136/bjsm.34.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12(3):185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- 21.Baier M, Hopf T. Ankle orthoses effect on single-limb standing balance in athletes with functional ankle instability. Arch Phys Med Rehabil. 1998;79(8):939–944. doi: 10.1016/s0003-9993(98)90091-0. [DOI] [PubMed] [Google Scholar]
- 22.Bernier J.N, Perrin D, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32(3):226–232. [PMC free article] [PubMed] [Google Scholar]
- 23.Cornwall M.W, Murrell P. Postural sway following inversion sprain of the ankle. J Am Podiatr Med Assoc. 1991;81(5):243–247. doi: 10.7547/87507315-81-5-243. [DOI] [PubMed] [Google Scholar]
- 24.Hertel J, Olmsted-Kramer L.C. Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture. 2007;25(1):33–39. doi: 10.1016/j.gaitpost.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle. Br J Sports Med. 1997;31(1):65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perrin P.P, Bene M.C, Perrin C.A, Durupt D. Ankle trauma significantly impairs posture control: a study in basketball players and controls. Int J Sports Med. 1997;18(5):387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- 27.Rozzi S.L, Lephart S.M, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29(8):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 28.Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7(5):291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- 29.Bahr R, Bahr I.A. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7(3):166–171. doi: 10.1111/j.1600-0838.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 30.Bahr R, Lian O, Bahr I.A. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7(3):172–177. doi: 10.1111/j.1600-0838.1997.tb00135.x. [DOI] [PubMed] [Google Scholar]
- 31.Beynnon B.D, Murphy D.F, Alosa D.M. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 32.Beckman S.M, Buchanan T.S. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch Phys Med Rehabil. 1995;76(12):1138–1143. doi: 10.1016/s0003-9993(95)80123-5. [DOI] [PubMed] [Google Scholar]
- 33.Bullock-Saxton J.E, Janda V, Bullock M.I. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med. 1994;15(6):330–334. doi: 10.1055/s-2007-1021069. [DOI] [PubMed] [Google Scholar]
- 34.Bullock-Saxton J.E. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74(1):17–31. doi: 10.1093/ptj/74.1.17. [DOI] [PubMed] [Google Scholar]
- 35.Caulfield B, Garrett M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin Biomech (Bristol, Avon) 2004;19(6):617–621. doi: 10.1016/j.clinbiomech.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 36.Gribble P.A, Hertel J, Denegar C.R, Buckley W.E. The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train. 2004;39(4):321–329. [PMC free article] [PubMed] [Google Scholar]
- 37.Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9(2):141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- 38.Rothermel S, Hale S.A, Hertel J, Denegar C.R. Effect of active foot positioning on the outcome of a balance training program. Phys Ther Sport. 2004;5(2):98–103. [Google Scholar]
- 39.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 40.Docherty C.L, Valovich McLeod T.C, Shultz S.J. Postural control deficits in participants with functional ankle instability as measured by the Balance Error Scoring System. Clin J Sport Med. 2006;16(3):203–208. doi: 10.1097/00042752-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Hertel J, Olmsted-Kramer L, Challis J. Time-to-boundary measures of postural control during quiet single leg standing. J Appl Biomech. 2006;22(1):67–73. doi: 10.1123/jab.22.1.67. [DOI] [PubMed] [Google Scholar]
- 42.van Emmerik R, van Wegen E. On the functional aspects of variability in postural control. Exerc Sport Sci Rev. 2002;30(4):177–183. doi: 10.1097/00003677-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 43.van Wegen E.E, van Emmerik R.E, Riccio G.E. Postural orientation: age-related changes in variability and time-to-boundary. Hum Mov Sci. 2002;21(1):61–84. doi: 10.1016/s0167-9457(02)00077-5. [DOI] [PubMed] [Google Scholar]
- 44.van Wegen E.E, van Emmerik R.E, Wagenaar R.C, Ellis T. Stability boundaries and lateral postural control in Parkinson's disease. Motor Control. 2001;5(3):254–269. doi: 10.1123/mcj.5.3.254. [DOI] [PubMed] [Google Scholar]
- 45.Ross S.E, Guskiewicz K.M, Yu B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J Athl Train. 2005;40(4):298–304. [PMC free article] [PubMed] [Google Scholar]
- 46.Hertel J, Braham R, Hale S, Olmsted-Kramer L. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sport Phys Ther. 2006;36(3):131–137. doi: 10.2519/jospt.2006.36.3.131. [DOI] [PubMed] [Google Scholar]
- 47.Olmsted L.C, Carcia C.R, Hertel J, Shultz S.J. Efficacy of the Star Excursion Balance Tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train. 2002;37(4):501–506. [PMC free article] [PubMed] [Google Scholar]