About 10%-15% of pheochromocytomas eventually develop metastases (1). Few patients with metastatic pheochromocytoma are suitable candidates for surgical resection of the tumor.
This correspondence introduces radiofrequency ablation (RFA) as an alternate treatment modality in pheochromocytoma. RFA is a safe, predictable, and effective method for local tumor destruction in primary and metastatic carcinomas (2-7). We report on a patient with metastatic pheochromocytoma with a rapidly growing bone metastasis who was treated with RFA.
The patient, a 42-year-old man, first presented with episodes of hematuria, hypertension, and palpitations. A 24-hour urine collection demonstrated elevated levels of catecholamines and metanephrines. Computed tomography (CT) scan revealed a 5.5 × 7.5 × 8.0-cm pheochromocytoma invading the posterior urinary bladder wall. His tumor was considered unresectable. The patient was treated with radiotherapy and six cycles of chemotherapy, with 80% tumor shrinkage followed by cystectomy. CT scans 5 years later showed lung metastases and a 0.5-cm third lesion on the right rib. The lesion grew gradually, then rapidly to 3 cm in diameter, with marked elevations in the levels of plasma norepinephrine (6974 pg/mL), free normetanephrine (3516 pg/mL), urinary norepinephrine (707 μg/24 hours), total metanephrines (6090 μg/24 hours), and vanillylmandelic acid (18.2 μg/24 hours). 6-[18F]Fluorodopamine positron emission tomography (Fig. 1) and [131I]metaiodobenzylguanidine scintigraphy confirmed that the rib lesion was metastatic pheochromocytoma. To treat the rib lesion, we chose RFA after we considered the limitations, side effects, and time commitments of radiotherapy, chemotherapy, and surgical resection. Because RFA disrupts cells by heat, marked catecholamine release was anticipated. Therefore, beginning 2 weeks before the procedure, the patient received phenoxybenzamine, atenolol, and α-methyl-para-tyrosine (Demser™; Merck Sharp & Dohme, West Point, PA). The adequacy of the adrenergic blockade was assessed by a provocative glucagon test 2 days before the RFA. Glucagon increased the patient’s blood pressure, and phenoxybenzamine was increased to 80 mg and Demser™ to 1.5 g once a day.
Fig. 1.
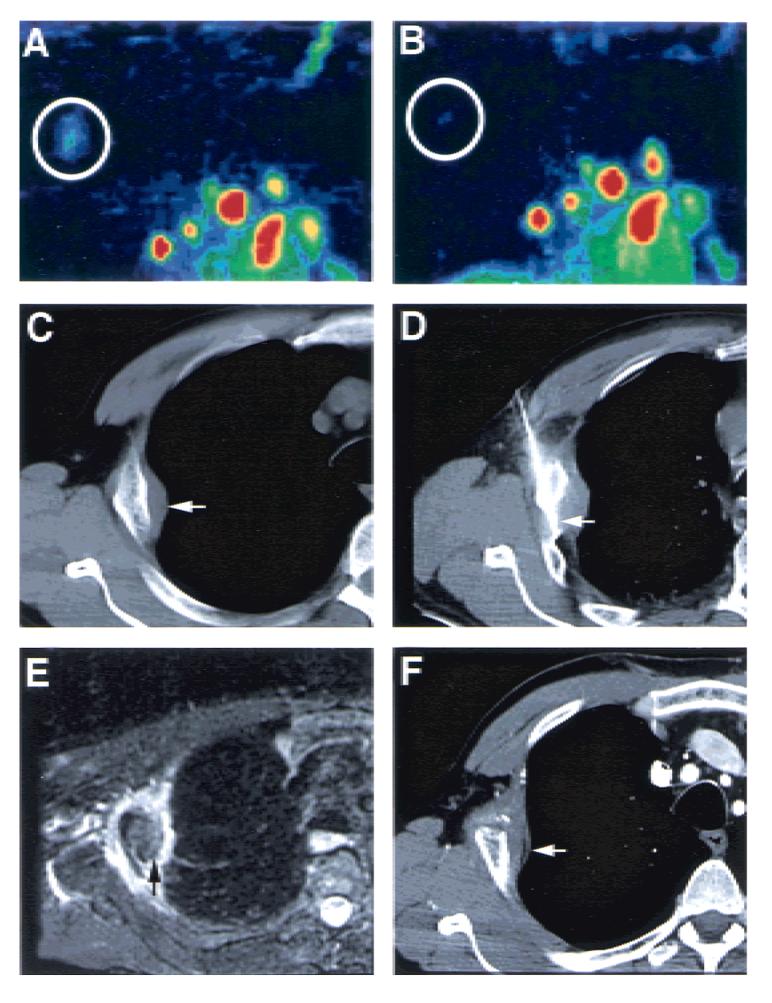
A) 6-[18F]Fluorodopamine positron emission tomography scan shows metastatic lesions in the right third rib (circle). Other masses in red color correspond with metastatic pheochromocytoma in both lungs. B) Markedly diminished uptake of 6-[18F]fluorodopamine in the right third rib indicates successful radiofrequency ablation of the metastatic lesion in this area. Circle is around the “remaining” tumor or area where the tumor was originally located. C) Computed tomography (CT) scan of the right chest without intravenous contrast shows rib metastasis with bony reaction and surrounding pleural mass (arrow). D) CT scan of the chest during treatment shows the uninsulated tip (arrow) of the radiofrequency needle electrode in the mass, after being placed with CT and ultrasound guidance. E) T-2 weighted magnetic resonance image 6 weeks after treatment shows low signal in region of mass, with uniform and regular, high signal in the periphery, consistent with inflammatory granulation tissue. Consistent with the absence of blood flow, the tumor did not enhance following contrast administration after treatment (not shown). F) Contrast-enhanced CT scan of the chest 6 weeks after treatment shows lack of enhancement in the region of the tumor, suggesting successful ablation on early follow-up. Arrow points to the area where the tumor was originally found.
RFA was performed in the interventional CT scan suite after an intercostal nerve block. Probe temperature was gradually increased to 86 °C, with treatment duration progressively increasing from 10 seconds to 10 minutes. RFA resulted in marked norepinephrine release (0.24-2.78 pmol/mL) and hypertension, managed with intravenous labetelol and a nitroprusside infusion. After RFA, phenoxybenzamine and Demser™ were tapered over a 2-week period. Successful ablation was documented by loss of signal intensity on CT and lack of tumor enhancement on magnetic resonance imaging, 1 day and 6 weeks after RFA (Fig. 1), and by 6-[18F]fluorodopamine positron emission tomography scan 2 weeks after RFA (Fig. 1).
This case illustrates that RFA can be used safely to ablate rapidly growing pheochromocytoma. In pheochromocytoma, where cells release contents in response to stimuli, it was unclear whether RFA would be safe. However, oral phenoxybenzamine, atenolol, and Demser™ with intravenous labetelol and nitroprusside provided adequate control of acute hypertension. On the basis of this experience, we propose that RFA be evaluated further in patients with primary or metastatic pheochromocytoma as an alternative to surgery, chemotherapy, or radiotherapy. 6-[18F]Fluorodopamine positron emission tomography scan provides a valuable tool to evaluate the effects of the ablation; it can be used as an alternative to CT and magnetic resonance imaging, in conjunction with measurements of levels of plasma catecholamines and metanephrines.
Contributor Information
KAREL PACAK, Pediatric and Reproductive Endocrinology Branch, National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD.
TITO FOJO, Medicine Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD.
DAVID S. GOLDSTEIN, Clinical Neurocardiology Section, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD
GRAEME EISENHOFER, Clinical Neurocardiology Section, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, MD.
McCLELLAN M. WALTHER, Urologic Oncology Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD
W. MARSTON LINEHAN, Urologic Oncology Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD.
LISA BACHENHEIMER, Department of Anesthesiology, Clinical Center, National Institutes of Health, Bethesda, MD.
JAME ABRAHAM, Medicine Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD.
BRADFORD J. WOOD, Department of Radiology, Clinical Center), National Institutes of Health, Bethesda, MD
REFERENCES
- (1).Manger W, Gifford R. Clinical and experimental pheochromocytoma. Blackwell Science; Cambridge (MA): 1996. [Google Scholar]
- (2).Seki T, Tamai T, Nakagawa T, Inoue K. Percutaneous radiofrequency (RF) ablation therapy for hepatocellular carcinoma: difficulty in removing the expandable RF needle electrode. AJR Am J Roentgenol. 2000;174:264–5. doi: 10.2214/ajr.174.1.1740264a. [DOI] [PubMed] [Google Scholar]
- (3).Dupuy DE, Zagoria RJ, Akerley W, Mayo-Smith WW, Kavanagh PV, Safran H. Percutaneous radiofrequency ablation of malignancies in the lung. AJR Am J Roentgenol. 2000;174:57–9. doi: 10.2214/ajr.174.1.1740057. [DOI] [PubMed] [Google Scholar]
- (4).Zlotta AR, Djavan B, Matos C, Noel JC, Peny MO, Silverman DE, et al. Percutaneous transperineal radiofrequency ablation of prostate tumour: safety, feasibility and pathological effects on human prostate cancer. Br J Urol. 1998;81:265–75. doi: 10.1046/j.1464-410x.1998.00504.x. [DOI] [PubMed] [Google Scholar]
- (5).Jeffrey SS, Birdwell RL, Ikeda DM, Daniel BL, Nowels KW, Dirbas FM, et al. Radiofrequency ablation of breast cancer: first report of an emerging technology. Arch Surg. 1999;134:1064–8. doi: 10.1001/archsurg.134.10.1064. [DOI] [PubMed] [Google Scholar]
- (6).Wood BJ, Fojo A, Gomez-Jorge J, Chang R, Spies J. Radiofrequency ablation of adrenocortical carcinoma: early experience. Scientific paper at Society for Cardiovascular and Interventional Radiology 25thAnnual Scientific Meeting. J Vasc Interv Radiol. 2000;11S:224–5. [Google Scholar]
- (7).Wood BJ, Levy EB, Gomez-Jorge J, Chang R, Spies J. Radiofrequency ablation of renal tumors. Scientific paper at Society for Cardiovascular and Interventional Radiology 25thAnnual Scientific Meeting. J Vasc Interv Radiol. 2000;11S:225. [Google Scholar]


