Abstract
Objective
To describe the Interdisciplinary Council on Developmental and Learning Disorders Diagnostic Manual for Infants and Young Children (ICDL-DMIC) created by representatives of the Interdisciplinary Council on Developmental and Learning Disorders.
Method
A description of the rationale of the different sections of the ICDL-DMIC dealing with infants and young children, focusing on a classification system which integrates all components of development and functioning which have been traditionally addressed by different disciplines.
Results
A description of an in-depth approach to mental health diagnosis for infants and young children that goes beyond simply a description of symptoms and captures the qualities of the individual.
Conclusion
The ICDL-DMIC presents an innovative approach to the assessment and diagnosis of infants and young children and their families, featuring a multi-dimensional classification system which uniquely considers the emerging functional emotional developmental capacities of the infant and young child and the developmental pathway to symptom patterns.
Keywords: functional emotional developmental capacities, infants, multi-axial, interdisciplinary, young children
Résumé
Objectifs
Présenter l’Interdisciplinary Council on Developmental and Learning Disorders- Diagnostic Manual for Infants and Young Children (ICDL-DMIC) créé par les représentants de l’Interdisciplinary Council on Developmental and Learning Disorders.
Méthodologie
Cet article présente et analyse les différentes sections du ICDL-DMIC qui traitent des nourrissons et des jeunes enfants. Il se concentre sur un système de classification intégrant toutes les composantes du développement et du fonctionnement, domaines qui étaient encore récemment du ressort de disciplines différentes.
Résultats
L’article décrit une approche approfondie du diagnostic de santé mentale du nourrisson et du jeune enfant qui va au-delà de la simple description des symptômes et prend en compte les qualités du sujet.
Conclusion
L’ICDL-DMIC propose une approche nova-trice de l’évaluation et du diagnostic du nourrisson, du jeune enfant et de sa famille. Il présente un système de classement multidimensionnel qui est unique car il considère les capacités développementales, émotionnelles et fonctionnelles du nourrisson et du jeune enfant, ainsi que le cheminement développemental qui conduit aux symptômes.
Keywords: capacités développementales, émotionnelles et fonctionnelles, nourrissons, multi-axial, interdisciplinaire, jeune enfant
Introduction
Infancy and early childhood is characterized by dynamic relationships between the different dimensions of human development, including emotional, social, language, cognitive, regulatory-sensory processing, and motor capacities. No classification system currently exists that describes challenges in each of these areas of functioning and the relationships between them. A dynamic, developmental, multi-axial approach that includes all the relevant dimensions of human development is especially vital during these formative years when not only is the brain and mind growing more rapidly than it ever will again, but it is literally forming the relationships between its different components. Attending to these interconnected components is essential in classifying disorders as the basis for meaningful intervention planning and research.
The new Interdisciplinary Council on Developmental and Learning Disorders Diagnostic Manual for Infants and young Children (ICDL-DMIC) utilizes a comprehensive approach which includes interactive, neurodevelopmental, regulatory-sensory processing, language, and learning disorders (Interdisciplinary Council on Developmental and Learning Disorders, 2005). It emphasizes the multiple relationships between different areas of development and can identify those infants and young children who present with a specific type of problem but often have challenges in other areas of functioning. For example, a pre-schooler with an impulse control problem will often have challenges in terms of caregiver/ child interaction patterns and different aspects of sensory processing, language, and cognition. Similarly, children with language problems may often also evidence contributions from challenges in motor planning and sequencing and other aspects of sensory processing. Challenges in any area can derail healthy emotional development and relationships.
The ICDL-DMIC introduces the concept of the developmental pathways which guides understanding of why particular symptoms develop related to the way the child reacts to and comprehends different sensations and plans actions (an expression of his or her biological patterns), the ways in which the caregiving environment interacts with these individual differences (within the normative range of individual differences, but not at the level of a disorder), and the levels or stages of emotional and intellectual organization that are negotiated through these interactions. These inter-related elements constitute the Developmental, Individual Difference, Relationship-based (DIR) model (Greenspan & Wieder, 1997). The DMIC was conceptualized over a thirty year period, beginning with the research conducted at the Clinical Infant Development program (NIMH) directed by Greenspan. Important foundations for this effort stem from an ongoing task force of leading infant researchers who met regularly to formulate the critical factors essential for infant metal health. These pioneers included Reginald Lourie, Selma Fraiberg, T. Berry Brazelton, Julius Richmond, Ed Ziegler, Katherine Barnard, as well as Stanley Greenspan and Serena Wieder and a number of others. This led to the Task Force at Zero to Three: The National Center for Infants, Toddlers, and Families which developed the first Diagnostic Classification (DC 0–3), chaired by Greenspan and Wieder (1994) and then to the Interdisciplinary Council on Developmental and Learning Disorders (ICDL) Task Force which formulated the ICDL-DMIC in 2005.
The ICDL Task Force expanded the classification system to include language and learning disorders, and a new developmentally-based framework for regulatory-sensory processing disorders and neurodevelopmental disorders of relating and communicating (autism spectrum disorders, multisystem developmental disorders, etc.) to provide a comprehensive and systematic method for presenting a rich, detailed clinical picture of each infant or young child and his or her family along with a framework for systematically organizing these rich descriptions into clinically meaningful categories. Thus, the goal of the ICDL-DMIC is to formulate a truly clinically useful approach that will facilitate research into etiological factors and inform effective intervention approaches that are tailored to the unique developmental profiles of each child and family.
An Interdisciplinary Approach to Classification
This classification system integrates all components of development and functioning which have been traditionally addressed by different disciplines. It is designed for professionals credentialed to do diagnoses. It can also be used by all disciplines as a roadmap to understanding the interactions between the different components of the child’s development, their family and environment in order to guide assessments and interventions. It augments other existing diagnostic systems such as ICD-10, DSM IV-R, and DC: 0–3R. Because the ICDL-DMIC is an interdisciplinary tool that supports the integration of knowledge from different disciplines, it will, for example, guide the mental health professional to integrate what has been learned about development, regulatory-sensory processing, language, visuospatial, and learning capacities into their mental health expertise. Similarly, pediatricians, occupational, physical, and speech and language therapists, educators, and professionals from other disciplines will integrate understanding of emotional development, interactive disorders, and family and environmental factors on adequate, constricted or disordered functioning.
The Need for a Comprehensive Multidimensional Developmental Approach
Earlier diagnostic approaches relied on lists of categorical symptoms that are readily observable are used in the belief that they facilitate reliable judgments. The symptom-based approach, however, has not demonstrated the clinical validity, including predicting clinical course or informing clinical practice, to the degree hoped for. For many diagnoses, the reliability among practicing clinicians making the diagnosis has also been disappointing (Spiegel, 2005).
Multidimensional Classification Based on the DIR Model
Dimensional approaches tend to be based on an implicit understanding that most mental health and developmental disorders are based on complex dynamic, developmental processes. We have formulated a developmental, biopsy-chosocial model to describe the processes that contribute to mental health, development, regulatory-sensory processing, language, and learning disorders in infancy and early childhood—the Developmental, Individual-Difference, Relationship-Based (DIR) approach. The DIR approach focuses on (D) Developmental capacities - the level of emotional, social, and intellectual functioning (technically called functional emotional developmental capacities). It also focuses on biologically-based (I) Individual processing differences in the way an infant or young child reacts to and comprehends different sensations, such as auditory, visuospatial, or tactile, as well as the way in which the child plans, sequences, and executes actions. It also focuses on the (R) Relationships, including child/caregiver/family and other relationship patterns).
Unique Features of the ICDL-DMIC Multiaxial System
Comprehensiveness and systematization guided the ICDL work groups in creating this manual. Only a diagnostic system that describes the full complexity of disordered functioning and characterizes different subtypes can provide a basis for basic research on underlying etiologies and developmental pathways. A number of unique features operationalize this perspective. For example, in Axis I each of the primary disorders classified under the heading “Interactive Disorders” is described in terms of its clinical phenomena, presenting symptoms, developmental pathways, and therapeutic implications. In addition, each disorder is described along a number of axes, which attempts to capture and emphasize an important component of, and/or contributor to, the disorder. These include the infant’s or young child’s level of emotional and social functioning, child-caregiver and family interaction patterns, motor planning and processing differences (regulatory sensory processing profile), language functioning, visuospatial capacities, and unique stressors that may be affecting the child and his or her family. In addition, a new feature of the ICDL-DMIC is the inclusion of Language Disorders and Learning Challenges.
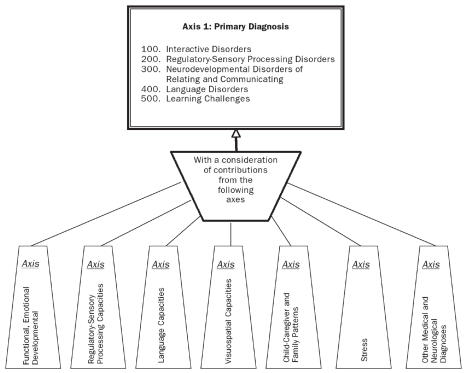
The goal of the ICDL-DMIC is to present both a rich, detailed clinical picture of each infant or young child and his or her family and, at the same time, provide a framework for systematically organizing these rich descriptions into clinically meaningful categories. Each Axis is briefly described in this article and summarized in Figure 1.
Axis I–Primary Diagnosis
The broad diagnostic category—Interactive Disorder, Regulatory-Sensory Processing Disorder, Neurodevelop-mental Disorder of Relating and Communicating, Language Disorder, and/or Learning Challenges—and the specific type of disorder within the category.
Axis II–Functional Emotional Developmental Capacities
The relative mastery of each of the functional emotional developmental capacities, including shared attention and regulation, engagement and relating, two-way intentional, affective signaling and communication, long chains of co-regulated emotional signaling and shared social problem solving, creating symbols or ideas, building bridges between ideas- logical thinking.
Axis III–Regulatory-Sensory Processing Capacities
The regulatory-sensory processing capacities, in terms of self-regulation, sensory modulation, sensory discrimination, and sensory-based motor abilities, including postural control and motor planning.
Axis IV–Language Capacities
Includes gestural and verbal communication (comprehension and production) at each developmental level.
Axis V–Visuospatial Capacities
The progressive development of visuospatial aspects of body awareness and sense thinking, location of the body in space, relation of objects to the self and other objects and people, conservation of space, visual logical thinking, and representational thought.
Axis VI–Child-Caregiver and Family Patterns
Characteristics of infant or child-caregiver interaction patterns and family or environmental patterns.
Axis VII–Stress
Stressors related to situations, conditions or events in the family’s or child’s life which can impact the child’s emotional functioning and development when appropriate protective factors or adequate resiliency isn’t evident.
Axis VIII–Other Medical and Neurological Diagnoses
Selecting a Primary Diagnosis
Most infant and early childhood disorders are characterized by multiple elements or dimensions, for example, interactive and family patterns, and regulatory-sensory processing patterns. These disorders include anxiety and mood disorders, disruptive behavior, elective mutism, as well as sleep, eating, and elimination disorders. A multi-axial approach will allow a systematic description of each of the contributing elements. Before concluding on a primary diagnosis, all the axes must be fully evaluated in order to determine the various dimensions contributing to the presenting problems. Once all this information is considered, clinical reasoning will guide the experienced clinician in selecting the predominant pattern and identifying how the developmental pathway contributes to the symptom choice.
The decision process would first consider the most comprehensive disorder where multiple elements of development are derailed. For example, Neurodevelopmental Disorders of Relating and Communicating includes Regulatory-Sensory Processing Disorders, Language Disorder, and emotional constrictions. When relating and communicating are not significantly derailed then the Regulatory-Sensory Processing Disorders are considered next to see if the presenting behavioral patterns are coupled with motor and/or regulatory-sensory processing challenges. When a regulatory-sensory processing contribution is significant, it will take precedence over the interactive elements in the designation of the primary diagnosis. If interactive challenges dominate, it becomes the primary disorder.
With Interactive Disorders there is so much overlap in symptoms, the clinician must consider when the symptom is part of a broader disorder such as anxiety, mood or disruptive behavior, and when it is itself the primary disorder. For example, if a child with Anxiety Disorder also has sleep problems, but the sleep problem is intermittent or a temporary disruption of a developmental capacity already mastered, along with possible other disruptions in eating or toileting, then an additional diagnosis would not be necessary. However, if the sleep problem is very intense or of longer duration, and also meets the description of the primary disorder, then it could be considered a second primary diagnosis. Similarly, if a child manifests disruptive or oppositional behavior, Anxiety Disorder or Disruptive Behavior Problem could be considered and the differentiating consideration would be whether the child has a pattern of impulse control problems in various situations or emotional states. If not, then Anxiety Disorder may be the only primary diagnosis selected. More than one diagnosis is permitted under this system. In addition, as indicated earlier, we emphasize a Language Disorder or Learning Challenge can be used as a second primary diagnosis when a child evidences a significant difficulty in either of these areas of functioning. In other words, clinical reasoning must determine if the multiple symptoms are significant enough to constitute an additional diagnosis or are part of the primary problem.
Clinical Thresholds for Diagnosis
Deciding when a behavioral or emotional pattern constitutes a disorder rather than a disruption or variation within the normal range presents the clinician with a challenge. This can be especially difficult during the first five years when development is proceeding rapidly and has so much variation influenced by individual differences. It is also a challenge when so many of the same symptoms can relate to different disorders given the limited number of symptoms in the infant’s and young child’s repertoire.
As indicated above, the attempts to define specific criteria for disorders in order to reach reliability do not always have solid evidence. In addition, many of the current classification approaches go beyond the available research in their specificity by requiring a specific number of criteria for a diagnosis, yet there are insufficient studies documenting what it means if the patient meets only two out of five (i.e., there is no data supporting a clear line between two versus three of the criteria), or are some criteria more important than others.
Similarly, there’s insufficient data on how long a symptom should be evidenced, as if two days less than the indicated two weeks is scientifically based. Criteria that are easy to agree upon are not necessarily the criteria that are meaningful for clinical planning or research on etiological factors and developmental pathways. We do not yet have a scientifically-based diagnostic system for mental health, developmental, and learning challenges, but we do have emerging data and a great deal of clinical experience.
Since we are currently operating on expert consensus with supportive, but incomplete, data, this classification system utilizes functional or operational considerations to make the clinical judgment of whether the presenting problems cross the clinical threshold to be considered a disorder. The following hierarchy should be considered:
Is the child functioning within his or her age-expected functional developmental capacities? What is the range of the child’s comprehension and expression of emotions with gestures and/or words or play, in comparison to age expectations? See Axis II– Functional Emotional Developmental Capacities, as well as other clinical assessments.
How well is the child functioning within the family structure on a daily basis including routines of sleep, meals, play, relating to family, caregivers and sibling interactions? Is the environment stable? Is the child stable?
Is the child adapting to daycare or pre-school adequately and able to enjoy these environments and learning experiences?
Is the child participating in expected social interactions, developing friendships, and able to play with peers?
What are the child’s emerging attitudes and feelings towards him or herself and others (e.g., angry, depressed, suspicious, etc.) in comparison to what’s expected for his or her age (e.g., some degree of negativism is expected during the preschool years)?
The child may present significant challenges in any one of these areas which may be sufficient to warrant a diagnosis as with, difficulties in relating and communicating. In some cases, more than one area may be involved but the problem may not be spilling over significantly to preschool or peer play, such as a disorder of emotional range and stability where constrictions are significant and family interactions cannot support healthier emotional development. Sometimes the threshold is not crossed until the preschool brings the problem to the attention of the family—the problem may not be perceived or evidenced at home, yet is significantly impeding the child’s adaptation at school. The greater the number of areas of functioning that are involved, the more likely a diagnosis is indicated.
Furthermore, in addition to the detailed descriptions of the primary diagnosis to guide clinical judgment, Axes II through VII require a clinical formulation indicating the degree to which impairment is evident. The more severe the impairment or delay of the expected developmental capacities, the greater the evidence for the disorder(s). Clinical judgment relies on evaluating the functional or operating areas and each of the dimensions in this multi-axial system to determine if the clinical threshold for a diagnosis has been crossed.
Even when the clinical threshold is not crossed, the diagnostic process and evaluation provides the parent with a better understanding of their child’s profile of strengths and vulnerabilities and allow anticipatory guidance to better support the development of the child and family in the future.
Axis I–Primary Diagnosis
[Note: Due to space limitations, only the overarching diagnostic code is included for each primary disorder. Please see ICDL-DMIC (Interdisciplinary Council on Developmental and Learning Disorders, 2005) for more detail.]
100. Interactive Disorders1
Interactive disorders are characterized by the way a child perceives and experiences his emotional world and/or by a particular mal-adaptive child-caregiver interaction pattern (Greenspan, 1992). The caregiver’s personality, fantasies and intentions; the child’s emerging organization of experience; and the way these come together through child-caregiver interactions are important components of the basis for understanding the nature of the difficulty and for devising an effective intervention plan. As with all infant and early childhood disorders, it is also important to consider the child’s constitutional-maturational variations, and family and environmental factors (Axes VI and VII) .Although each child has a unique regulatory-sensory processing profile, constitutional-maturational variations are not a major contributing factor in interactive disorders, as they are in the category of Regulatory-Sensory Processing Disorder.
The evaluating clinician must also consider the interaction patterns characteristic of each of the six developmental levels and determine which patterns have been negotiated successfully and which are absent or constricted. These are captured in Axis II. Regardless of the symptom, the goal of treatment is not only to alleviate it, but also to facilitate the child’s progress toward an age-appropriate developmental level and toward an age-appropriate degree of stability and range of thematic experience.
Symptoms that can reflect an interactive disorder include anxiety, fears, behavior control problems, and sleeping and eating problems. The same symptoms can be reflective of any number of diagnoses. This is understandable in light of the limited number of behaviors or limited expression of feelings infants and young children are capable of. This category also includes transient situational adjustment reactions, such as a child’s response to his mother’s return to work. It also includes certain reactions to trauma in which the response does not involve multiple aspects of development. Because of space limitations, just a few abbreviated primary disorders (101. Anxiety Disorder and 105. Depression) have been selected to illustrate the ICDL-DMIC approach to Axis I. See ICDL-DMIC (ICDL, 2005) for more detail.
101. Anxiety Disorder
Presenting Pattern
Infants and young children may evidence persistent levels of anxiety and fear which impede age-expected range of emotions and functioning. In infants and very young preverbal children anxiety is more generalized nature, in which symptoms such as excessive fearfulness, tantrums, agitation, avoidance, panic reactions, and worries are in evidence on a persistent basis even when the child is not threatened by separation from a primary caregiver. In the older child anxiety can take the form of specific fears or verbalized worries, obsessions or preoccupations, excessive tantrums, distress and agitation, and avoidance or counterphobic behaviors. The child may talk about their fears but not respond to reassurances, or may have a freeze, fight or flight reaction and is clearly distressed and fearful and cannot carry on usual routines and activities without significant disruptions during the day or night. Hypervigilant behavior can be observed at all ages, even in very young infants (3 to 4 months of age). The child appears frightened, overly reactive, and overly focused, as though there were imminent danger. Infants who are abused may show this reaction quite early in their development, although it can manifest itself at any time.
For any form of anxiety, first consider is the anxiety primarily related to a Regulatory-Sensory Processing Disorder (see 200. Regulatory-Sensory Processing Disorders). Second, is the anxiety primarily related to expected developmental transitions or tasks the child is having difficulty mastering? Or third, is the anxiety primary related to infant-caregiver interactions? The primary source of the anxiety may not always be clear.
Interactive elements are evident in situations where the primary caregiver is not providing ongoing personal security and may be unable to alleviate the anxiety through such strategies as helping the child anticipate what might be anxiety, problem solving conversations, practice in pretend play, preparing the child for what will occur; soothe, negotiate and reassure the child sufficiently if the anxiety increases. Caregiver may also be anxious and distressed and anticipating the child’s anxiety and feels ill equipped to help, or feeling annoyed, or overly worried. He or she may also be bringing her own anxieties to the situation at hand, such as social inhibition, or a specific phobia such as fearing dogs, or over- identifying with the child who reminds her of similar experiences in her childhood. In either case, the interaction between the child and caregiver increases the anxiety and distress and makes it difficult to support the child.
The Developmental Pathway
Tend to be over reactive to sensations like sound and touch and to experience and express affect intensely. Caregiver overreacts to the child’s emotional communications. As a consequence, the child feels overwhelmed and deregulated (contrast with depression where caregiver shuts down). Instead of experiencing a loss or rupture in the relationship (as the depressed child might), the anxious child constantly feels overwhelmed and experiences dysphoric or unpleasant affects associated with being overwhelmed.
Therapeutic Implications
Requires long chains of especially soothing, reciprocal emotional interactions. Therapy needs to focus on use of affects as a symbolic signal to cope and not escalate or panic and on the child’s expectations that relationships will intrude on or overwhelm him. Along with verbal awareness of the child’s affective and interactive patterns, the anxious child needs to experience new ways of engaging in interactive, affective exchanges and signaling.
105. Depression
In healthy development, infants and young children gradually expand their capacities for emotional expression and experiencing a wide range of feelings. This gradually expanding capacity is part of the infant-caregiver relationship pattern. Adaptive interactive patterns enable the infant to successfully negotiate each of the functional emotional developmental capacities, and thereby experience, by the time they are toddlers, a large range of emotions from joy, pleasure, and enthusiasm to transient sadness and fear. They are also able to enjoy assertiveness and exploration, as well as a growing curiosity.
Presenting Pattern
Infants and young children can begin showing a consistent mood pattern, rather than the range of emotional states expected for their age and developmental stage. For example, some toddlers and preschoolers display a persistently sad or depressed affect. They may indicate they are sad or well up with tears when asked about feelings or even seeing someone else feeling sad or crying. They appear to show little pleasure or interest in their usually enjoyable activities and do not initiate “fun” activities. Sometimes they may have difficulty showing or verbalizing expectable feelings of sadness in situations that would ordinarily elicit sad feelings, or insist they are “happy” even as they cry or look very sad. As they become symbolic, they may play out and talk about depressive themes. Preschoolers may, for example, enact in play and/or verbalize persistent feelings of being “bad,” and slightly older children may even talk about wishing they were not alive or present themes of dying in their play (which is not part of a bereavement or trauma situation).
Infants and young children may also evidence persistent agitation and irritability, with nothing pleasing them, or in contrast, may move very little, show little energy, and turn down activities they may have once enjoyed. Other children have sleep or eating difficulties (with weight loss or gains), which are common symptoms related to various sources of stress.
The severity of the mood disorder may be reflected in the intensity of just a few of the behaviors described above, or the increasing number of challenges, the longer the child feels depressed. Infant-caregiver interaction patterns often play a major role in the child’s difficulties in regulating mood. The child may experience the loss of love or support when the parent cannot accept their full range of behavior and feelings. For example, the parent may be very loving in response to compliance and being good, but pull away when the child is angry or aggressive. The parent may not be able to respond to the child when his own conflicts are triggered and he is ambivalent or unpredictable to the child.
The depression becomes apparent over time when the child experiences some loss or conflict with others and is unable to rely on an internalized, nurturing image to soothe and comfort. Such difficulties can, if left unaddressed, persist into adulthood. See the case example below.
Developmental Pathway
Sensory over-responsiveness, stronger verbal processing capacities, and weaker visuospatial processing capacities characterize the pattern we have observed in many individuals prone to depression. In a child at risk for depressive patterns, the caregiver tends to shut down when the child’s affect is becoming intense (i.e., the caregiver finds it hard to maintain a pattern of co-regulated affective interaction at these moments of heightened affect). The child experiences a loss or rupture in the relationship, sometimes only for a few seconds. This very brief sense of loss becomes associated with strong affect. As expectations are formed, due to better “pattern construction,” the child expects loss and/or emptiness when he has strong feelings. As he becomes more symbolic, this pattern can be experienced in terms of images of loss and, later on, “I must have caused the loss by being bad or angry or demanding.” Instead of an internal security blanket of warm, soothing, comforting images and expectations, the child experiences loss and sadness.
Therapeutic Implications
One aspect of therapeutic work with the child (or adult) with depressive tendencies is working on the flow of interaction, helping the caregiver maintain co-regulated, affective interactions, pulling the child in with extra enthusiasm, as needed, rather than temporarily withdrawing or “freezing” and, at the same time, helping the caregiver understand what might have happened to bring on these tendencies. The goal is to help the child become able to experience, express, and explore a broad range of affects, including feelings of anger, entitlement, and fear of loss. Helping the child learn to visualize the nurturing parent can help alleviate the sense of loss and encourage self-soothing and adaptive responses.
To illustrate how infant-caregiver interaction patterns, as well as the child’s regulatory-sensory processing profile and the caregiver’s personality, can contribute to this type of challenge, consider the example of a bright, talented, and precociously verbal 4-year-old who became depressed when she experienced competitive situations at preschool.
When a child became competitive with her during playtime, she felt the other child was unfair and had a feeling of loss; she then got depressed and didn’t play with or talk to the other children for the rest of the morning. This sequence occurred routinely when she experienced competition. She could describe a feeling of “being all alone” during these moments. Her therapist asked her if she could bring to mind an image of her mother and picture her nurturing her at these times. She said, “I can’t picture my Mommy.” She was unable to create a nurturing internal image. Her therapist later learned that she had a mother who had consistently responded to her strong feelings not by nurturing her but instead by “shutting down” and “becoming stone-faced.”
A clue to this pattern was the patient’s reaction to her therapist’s periodic temporary loss of empathy and relatedness. If, for example, the therapist looked out the window for a second, she would immediately look quite sad. Instead of trying to pull the therapist back in, she would look down and her voice would go into more of a monotone, as though she were giving up.
It wasn’t sufficient, however, just to verbally point out this pattern. It was also necessary to create a different type of affective interaction and rhythm. The therapist needed to pull her back in with animated affective gestures and literally challenge her with his affective gestures to take the initiative. He did this with very distinct “expectant” looks, which communicated, “Can you keep the affective rhythm going, or are you going to intensify my momentary lapse with an even bigger one?” Eventually, therapist and patient were able to explore this pattern in play and with words.
Initially, this patient didn’t have the basis for recreating a multi-sensory, affective experience of nurturing in her own imagination. She didn’t have the internal affective image or feelings to get her through a tough time. Instead, she would get depressed because she had no internal, representational “security blanket” to fall back on. The “security blanket” was absent at the level of two-way, presymbolic affective communication and at the level of symbolization. As she learned to initiate affective interactions at times of loss, she also gradually became able to imagine and symbolize an internal “security blanket” made up of images. She could feel and picture her mother or friends in nurturing interactions.
This patient was also much stronger in her verbal processing capacities than her visu-ospatial processing, a pattern we have observed in many individuals prone to depression. Because of these processing patterns, she took a long time to progress to the level of feeling and picturing nurturing interactions. She began by describing them and gradually progressed to picturing and feeling them.
As her explorations broadened, she was able to deal with many additional conflicts. For example, she was very competitive with her “stone-faced” mother and had sought out her father as an “ally” in the family triangle. Only after she was able to construct internal, nurturing images, however, was she able to explore her own competitiveness, triangular relationship, and other conflicts.
200. Regulatory-Sensory Processing Disorders2
[Note: Due to space limitations, only the overarching diagnostic code is included for each primary disorder.]
Regulatory-Sensory Processing Disorders (RSPD), involve symptom patterns such as inattention, overreactivity, sensory seeking, and refer to those challenges where differences in the child’s constitutional and maturational variations, in terms of sensory over- or underreactivity, visuospatial, auditory and language processing, or motor planning and sequencing difficulties are a primary contributor to the child’s challenges. While all children evidence their own unique regulatory-sensory processing patterns, an RSPD should be considered when the child’s motor and sensory differences are contributing to challenges that interfere with age-expected emotional, social, language, cognitive (including attention), motor, or sensory functioning. RSPD gives rise to some of the same symptoms and behaviors as interactive disorders, including nightmares, withdrawal, aggressiveness, fearfulness and anxiety, sleeping and eating disturbances, and difficulty in peer relationships. However, RSPD involves clearly identifiable constitutional-maturational factors in the child.
The diagnosis of RSPD involves a distinct behavioral pattern and a sensory modulation, sensory-motor, sensory discrimination or attentional processing difficulty. When both a behavioral and a sensory pattern are not present, other diagnoses may be more appropriate. For example, an infant who is irritable and withdrawn after being abandoned may be evidencing an expectable type of relationship or attachment difficulty. An infant who is irritable and overly responsive to routine interpersonal experiences, in the absence of a clearly identified sensory, sensory-motor or processing difficulty, may have an anxiety or mood disorder. Sleep and eating difficulties, in the absence of identifiable sensory responsivity or sensory processing differences, are classified as disorders in their own right. Further evaluation is then needed to determine whether the cause is an interactive disorder or some other underlying problem that does not fall within our three broad categories. See ICDL-DMIC (ICDL, 2005) for more detail.
Type I: Sensory Modulation Challenges
(such as over-responsivity, under-responsivity, and sensory-seeking) are characterized by an inability to grade the degree, intensity, and nature of responses to sensory input. Often the child’s responses do not fit the demands of the situation and the child, therefore, demonstrates difficulty achieving and maintaining an optimal range of performance and adapting to challenges in daily life. In addition, sensory discrimination challenges and to sensory-based motor challenges (postural control problems and dyspraxia).
Type II: Sensory Discrimination Challenges
represent problems discerning the characteristics of sensory stimuli. The result is a lessened capability to interpret or give meaning to the specific qualities of stimuli, to detect similarities and differences among stimuli, and to differentiate the temporal and/or spatial qualities of stimuli. Children can perceive that stimuli are present and can modulate their responses to the stimuli, but cannot tell precisely what or where the stimulus is. Children with this challenge have difficulty interpreting the spatial and temporal qualities of sensory input and, as such, cannot use time and space information or other specific characteristics of the sensory experience to guide performance.
Type III: Sensory-Based Motor Challenges (Postural Regulation Difficulties and Dyspraxia)
Postural challenges refer to difficulty stabilizing the body during movement or at rest in order to meet the demands of the environment or of a given motor task. Postural problems are characterized by inappropriate muscle tension, hypo- or hypertonic muscle tone, inadequate control of movement, and/or inadequate muscle contraction to achieve movement against resistance. Postural difficulties frequently occur in the presence of vestibular, proprioceptive, and visual-motor problems, and include poor stability in the trunk, poor righting and equilibrium reactions, poor trunk rotation and/or poor ocular control.
Postural challenges can occur with or without a motor planning disorder, although it is often observed with dyspraxia, particularly in difficulty with bilateral integration activities (e.g., doing activities that require use of both sides of the body together such as riding a bike, pumping a swing, etc.) and with rhythmical activities (e.g., bouncing a ball, clapping on the beat). Dyspraxia is an impairment in the ability to plan, sequence and execute novel or unfamiliar actions. It is characterized by awkward and poorly coordinated motor performance, which can be observed in gross motor, fine motor and/or oral motor abilities. To be diagnosed with sensory-based dyspraxia, deficits must manifest in processing of sensory information in one or more of the following sensory domains: tactile, kinesthetic, proprioceptive, or vestibular. Visual-motor and visual spatial deficits usually accompany this difficulty also.
These children learn by trial and error, with decreased ability to generalize skills to other similar motor tasks. Execution of discrete motor skills (e.g., standing, walking, pincer grasp) may be adequate. However, the performance of complex tasks may be compromised, including tasks that require one or more of the following: significant sequencing, important timing aspects, rhythm of motor action, or subtle adaptation in the “moment of action.” All three patterns involve inattentive, disorganized behavioral patterns and school and academic challenges.
300. Neurodevelopmental Disorders of Relating and Communicating3
Neurodevelopmental disorders of relating and communicating (NDRC) involve problems in multiple aspects of a child’s development, including social relationships, language, cognitive functioning, and sensory and motor processing. This category includes earlier conceptualizations of multisystem developmental disorders (MSDD), as characterized in Infancy and Early Childhood (Greenspan, 1992) and Diagnostic Classification: 0–3 (DC 0–3) (Diagnostic Classification Task Force, 1994). Additionally, it includes the DSM-IV-R category of pervasive developmental disorders (PDD), also referred to as ASD. Since the description of MSDD in DC 0–3 and PDD in DSM-IV-R, the framework has been broadened to allow consideration of the full range of disorders of relating, communicating, and thinking. Thus, the large degree of individual variation in infants and young children who ultimately evidence common features of difficulties in forming relationships, communicating at preverbal and verbal levels, and engaging in creative and abstract reflective thinking can be captured. This helps differentiate the profiles that children commonly considered on the autism spectrum present and helps define the variations seen among the children with the same diagnosis. This differentiation is important for both intervention planning and research purposes.
NDRC may be viewed as part of the broad neurological category of a non-progressive disorder of the central nervous system. The technical term in ICD-10 (the International Diagnostic System) is “static” (non-progressive) “encephalopathy” (disorder of the central nervous system). It is also important to understand how regulatory-sensory processing disorders differ from NDRC. Although RSPDs involve deficits in processing capacities, unlike NDRC, they do not derail a child’s overall relating and communicating. Disorders of relating and communicating combine regulatory-sensory processing problems with significant developmental delays and dysfunctions. The child’s biologically-based processing difficulties contribute to, but are not decisive in determining, relationship and communication difficulties. A complete evaluation of the regulatory-sensory processing capacities is necessary to understand their contribution to NDRC.
In contrast, an important pattern to recognize involves developmental impairments resulting from severe environmental stress and trauma. For example, in failure-to-thrive syndrome, an infant’s motor, cognitive, language, affective, and physical growth may slow down or cease altogether. Persistent abuse or neglect can produce a similar global disruption in development and functioning. A tentative diagnosis of neurodevelopmental disorder could be given, but in these cases it would be important to see what changes occur once a comprehensive intervention program is put in place. In some cases, intervention can reverse the developmental impairments and the child may get back on track with only residual problems or may recover completely. In severe cases, only partial recovery may be evidenced.
NDRC can be more fully understood from the perspective of a developmental biopsy-chosocial model. Applying the DIR model to NDRC has enabled the development of a classification system that attempts to capture individual subtypes based on a more complete understanding of the developmental pathways that lead to significant challenges in relating, communicating, and thinking.
Table 1 is a very brief overview of the four types of NDRC which cluster the major profiles we have observed in children with significant challenges in relating, communicating, and thinking. Each type highlights the varied features of the subgroup, but it is important to remember that these types and their associated features are on a continuum. This table is provided as a summary to facilitate the use of this framework in a variety of clinical and research settings. Please see ICDL-DMIC (ICDL, 2005) for more detail.
Table 1.
Overview of Clinical Subtypes of NDRC and Related Motor and Sensory-Processing Profile
|
301. Type I - Early Symbolic, with Constrictions: Intermittent capacities for attending and relating; reciprocal interaction; and, with support, shared social problem-solving and the beginning use of meaningful ideas (i.e., with help, the child can relate and interact and even use a few words, but not in a continuous and stable age-expected manner).
Children with this pattern tend to show rapid progress in a comprehensive program that tailors meaningful emotional interactions to their unique motor and sensory processing profile. |
|
302. Type II - Purposeful Problem Solving, with Constrictions: Intermittent capacities for attention, relating, and a few back- and-forth reciprocal interactions, with only fleeting capacities for shared social problem-solving and repeating some words.
Children with this pattern tend to make steady, methodical progress. |
|
303. Type III - Intermittently Engaged and Purposeful: Only fleeting capacities for attention and engagement. With lots of support, occasionally a few back-and-forth reciprocal interactions. Often no capacity for repeating words or using ideas, although may be able to repeat a few words in a memory-based (rather than meaningful) manner.
Children with this pattern often make slow but steady progress, especially in the basics of relating with warmth and learning to engage in longer sequences of reciprocal interaction. Over long periods of time, often gradually master some words and phrases. |
|
304. Type IV - Aimless and Unpurposeful. Similar to Type III above, but with a pattern of multiple regressions (loss of capacities). May also evidence a greater number of associated neurological challenges, such as seizures, marked hypotonia, etc.
Children with this pattern often make very, very slow progress. The progress can be enhanced if the sources of the regressive tendencies can be identified. |
| Other Neurodevelopmental Disorders (Including Genetic and Metabolic Syndromes) |
| Children Who Are Difficult to Classify |
400. Language Disorders4
[Note: Due to space limitations, only the over-arching diagnostic code is included for each primary disorder.]
Language Disorders include challenges in communication in the context of a developmental framework that considers all components of language (e.g., gestures, motor, sensory, social, etc.). These can constitute a primary disorder when not part of another major disorder, such as NDRC. Language capacities also have their own profile (see Axis IV) because of the significance of language in development, as well as its impact on overall development. See ICDL-DMIC (ICDL, 2005) for more detail.
500. Learning Challenges5
[Note: Due to space limitations, only the overarching diagnostic code is included for each primary disorder.]
Learning challenges are included in this classification in order to identify the early pathways associated with later learning differences and challenges at school age. The goal is to optimize early interventions which may head off or ameliorate these challenges later. These include learning difficulties in reading and reading comprehension, math, and written expression, as well as organizational capacities (i.e., executive functioning). See ICDL-DMIC (ICDL, 2005) for more detail.
Axes II to VIII
In addition to the detailed descriptions of the primary diagnosis, evaluation of the functional or operating areas and Axes II–VII determines if the clinical threshold for a diagnosis has been crossed. The more severe the impairment or delay of the expected developmental capacities, the greater the evidence for the disorder(s).
Below is a brief description outlining the axes. See the manual for the full description.
Axis II – Functional Emotional Developmental Capacities
Axis II identifies six basic functional emotional developmental capacities, which depend on critical affective interactions (see Table 2). These capacities initially emerge in a developmental progression at the ages indicated. In optimal development, as a child grows, he or she continues to develop each capacity to a higher level. Yet, each child may first evidence these processes at ages that are later than expected and/or to different degrees. See ICDL-DMIC (ICDL, 2005) for more detail.
Table 2.
Basic Functional Emotional Developmental Capacities Which Depend on Critical Affective Interactions
| Level/Expected Emotional Function | Developmental Level |
|---|---|
| Level 1: Shared Attention and Regulation | Between birth to 3 months |
| Level 2: Engagement and Relating | Between 2 and 6 months |
| Level 3: Two-Way Purposeful Interaction | Between 4 and 9 months |
| Level 4: Shared Social Problem Solving | Between 9 and 18 months |
| Level 5: Creating Symbols and Ideas | Between 18 and 30 months |
| Level 6: Building Logical Bridges Between Ideas: Logical Thinking | Between 30 and 48 months |
Axis III – Regulatory-Sensory Processing Capacities
This axis reviews the same regulatory sensory processing capacities described in Axis I and is used when the individual differences do not interfere with age-expected emotional, social, cognitive, or learning capacities. The purpose is to capture to which pattern or developmental pathway may be contributing to the child’s challenges, but is not a primary diagnosis.
Axis IV–Language Capacities
Differences in language functioning, just as differences in regulatory-sensory function and family patterns, contribute to the primary symptom patterns of the child. It is also parallel to the functional emotional developmental stages because both are describing the presymbolic as well as the symbolic levels of the child’s overall functioning and communication. The language capacities, including gestural and verbal communication, however, focus on communication, particularly from the toddler through the preschool years.
Axis V–Visuospatial Capacities
This Axis addresses six visuospatial capacities which develop during infancy and early childhood (pre-school) years which interact simultaneously with the other sensory processing capacities and support or impede emotional and cognitive development. It is important to remember that all the capacities overlap and that the clinician should keep the developmental continuum in mind, as opposed to just focusing on a chronology of milestones. These six capacities are shown in Table 3 below. See ICDL-DMIC (ICDL, 2005) for more detail
Table 3.
Visuospatial Capacities Which Interact Simultaneously With Other Sensory Processing Capacities and Support or Impede Emotional and Cognitive Development
| Visuospatial Capacities |
|---|
| 1. Body Awareness |
| 2. Location of the Body in Space (involves location of own body parts in relatin to each other, location of the body as a whole in its immediate surroundings; and location of the body in terms of the broader environment) |
| 3. Relation of Objects to Self and Other Objects and People |
| 4. Conservation of Space |
| 5. Visual Logical Reasoning |
| 6. Representational Thought (drawing, thinking, visualizing) |
Axis VI–Child-Caregiver and Family Patterns
Axis VI describes the overall functioning of the caregiver and the degree to which the caregiver is able to support the child’s negotiation of each developmental level. Since caregiver and family patterns affect children in every group of disorders, and not just the interactive disorders, it is included as a separate axis. Table 4 outlines the guidelines to observe each care-giver’s interaction with the child (see ICDL-DMIC [2005] for more detail).
Table 4.
Guidelines for Observing Caregiver Interaction with Child
| 1. Caregiver tends to comfort the infant or child |
| 2. Caregiver tends to find appropriate levels of stimulation to interest the infant or child |
| 3. Caregiver tends to pleasurably engage the infant or child |
| 4. Caregiver tends to read and respond to the infant’s or child’s emotional signals and needs in most emotional areas |
| 5. Caregiver tends to encourage the infant or child to move forward in development |
Axis VII–Stress
The purpose of this axis is to identify and consider the possible contribution stress may be having on the presenting symptom patterns. Stressors related to situations, conditions or events in the family’s or child’s life can impact the child’s emotional functioning and development depending on the resources of the child and the family’s ability to mobilize adequate protective factors and suport at the time of the stress. The following sequence can be used to assess the impact of the stress (see ICDL-DMIC [2005] for more detail).
Identify and list the possible sources of stress
Determine the onset, severity and duration of the stressors identified
Assess the changes in the child’s functioning and mental health possibly influenced by the stressors.
Axis VIII–Other Medical and Neurological Diagnoses
Careful listing of medical disorders facilitates the clinician’s thorough investigation and the exploration of possible relationships with the child’s mental health, developmental, and learning challenges.
Conclusion
The ICDL-DMIC presents an innovative approach to the assessment and diagnosis of infants and young children and their families. It features a multi-dimensional classification system which uniquely considers the emerging functional emotional developmental capacities of the infant and young child and the developmental pathway to symptom patterns. By also assessing the regulatory, language, and visu-ospatial capacities of the infant, in addition to stress and medical conditions, the ICDL-DMIC integrates all the interactive aspects of developmental capacities, individual differences, and the impact of relationships.
Acknowledgements/Conflict of Interest
The authors have no financial relationships to disclose.
Footnotes
The Work Group on Interactive Disorders includes: Serena Wieder, Ph.D., Lois Black, Ph.D., Griffin Doyle, Ph.D., Barbara Dunbar, Ph.D., Barbara Kalmanson, Ph.D., Lori Jeanne Peloquin, Ph.D., Ricki Robinson, M.D., MPH., Ruby Salazar, LCSW, Rick Solomon, M.D., Rosemary White, OTR, Molly Romer Witten, Ph.D.
Work Group members include: Lucy J. Miller, Ph.D., OTR, Marie Anzalone, Sc.D., OTR, Sharon A. Cermak, Ed.D., OTR/L, Shelly J. Lane, Ph.D., OTR, Beth Osten, M.S., OTR/L, Serena Wieder, Ph.D., Stanley I. Greenspan, M.D.
Since the description of multisystem developmental disorders in DC:0–3, a work group of the Interdisciplinary Council on Developmental and Learning Disorders (ICDL) has developed the current classification of NDRC. The Work Group members include: Serena Wieder, Ph.D., Lois Black, Ph.D., Griffin Doyle, Ph.D., Barbara Dunbar, Ph.D., Barbara Kalmanson, Ph.D., Lori-Jean Peloquin, Ph.D., Ricki Robinson, M.D., M.P.H., Ruby Salazar, LCSW, Rick Solomon, M.D., Rosemary White, OTR, Molly Romer Witten, Ph.D., and Stanley I. Greenspan, M.D.
Work Group members included: Sherri Cawn, M.A., CCC-SLP; Sima Gerber, Ph.D., CCC; Cindy Harrision, M.S.c., SLP; Diane Lewis, M.A., CCC-SLP; Jane R. Madell, Ph.D., CCC A/SLP; Stuart G. Shanker, D.Phil.; Amy M. Wetherby, Ph.D., CCC-SLP; Stanley I. Greenspan, M.D.
The ICDL Work Group on Learning Challenges included: Pat Lindamood, M.S., CCC-SLP, Robert L. Hendren, D.O., Joan Mele-McCarthy, D.A., Kytja Voeller, M.D., Harry Wachs, O.D., Serena Wieder, Ph.D., and Stanley I. Greenspan, M.D.
References
- Greenspan SI. Infancy and Early Childhood: The Practice of Clinical Assessment and Intervention with Emotional and Developmental Challenges. International Universities Press; Madison, CT: 1992. [Google Scholar]
- Greenspan SI, Wieder S. Developmental patterns and outcomes in infants and children with disorders in relating and communicating: A chart review of 200 cases of children with autistic spectrum diagnoses. Journal of Developmental Learning Disabilities. 1997;1:87–141. [Google Scholar]
- Interdisciplinary Council on Developmental and Learning Disorders (ICDL) Diagnostic manual for infancy and early childhood: Mental health, developmental, regulatory-sensory processing, language and learning disorders – ICDL-DMIC. Bethesda, MD: Interdisciplinary Council on Developmental and Learning Disorders; 2005. [Google Scholar]
- Spiegel A. How One Man Revolutionized Psychiatry. [[accessed 5/1/08]];The New Yorker [online] 2005 Available at: http://www.newyorker.com/archive/2005/01/03/050103fa_fact.
- ZERO TO THREE Diagnostic Classification Task Force, Greenspan, S. I. (chair), Weider, S. (co-chair and clinical director) (1994) Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood. ZERO TO THREE/National Center for Clinical Infant Programs, Arlington, VA.