Abstract
Introduction
Interprofessional health and social service partnerships (IHSSP) are internationally acknowledged as integral for comprehensive chronic illness care. However, the evidence-base for partnership effectiveness is lacking. This paper aims to clarify partnership measurement issues, conceptualize IHSSP at the front-line staff level, and identify tools valid for group process measurement.
Theory and methods
A systematic literature review utilizing three interrelated searches was conducted. Thematic analysis techniques were supported by NVivo 7 software. Complexity theory was used to guide the analysis, ground the new conceptualization and validate the selected measures. Other properties of the measures were critiqued using established criteria.
Results
There is a need for a convergent view of what constitutes a partnership and its measurement. The salient attributes of IHSSP and their interorganizational context were described and grounded within complexity theory. Two measures were selected and validated for measurement of proximal group outcomes.
Conclusion
This paper depicts a novel complexity theory-based conceptual model for IHSSP of front-line staff who provide chronic illness care. The conceptualization provides the underpinnings for a comprehensive evaluative framework for partnerships. Two partnership process measurement tools, the PSAT and TCI are valid for IHSSP process measurement with consideration of their strengths and limitations.
Keywords: partnership, chronic disease, interprofessional complexity theory
Introduction
Partnerships are increasingly used to enhance health service delivery in response to an explosion in chronic disease prevalence. Although partnerships will ultimately redefine how health services are configured and delivered, little is known about how these partnerships function and their impact on outcomes [1, 2]. This paper focuses on the conceptualization and measurement of interprofessional health and social service partnerships (IHSSP) at the front-line, service provider group level. In the literature, the terms partnership, collaboration, and teamwork are used interchangeably to “reflect the idea of individuals coming together for a mutually accepted goal or mission” [3]. However, in this paper, interprofessional is the term used to describe the process of multiple disciplines working together. Partnership is used to indicate the collaborative nature of the process. Health and social services are named to bring attention to an expanded view of health beyond the traditions of cure and care associated with these disciplines.
Background
The multiple and often complex needs of populations affected by the epidemic of chronic illnesses require approaches that include both health and social services, and extend beyond traditional acute episodic health care and the services of any single organization [4–9]. In response, healthcare policies in Canada, as in other Western countries, require services to be integrated, often through partnerships to meet increased demands [9–13]. Support for IHSSP is so strong in the UK that the National Health Service has legislation requiring mandatory health and social service partnerships to break down traditional disciplinary barriers to collaboration [14, 15]. The span of health and social service partnerships can include anything from the coordination of individual clinical care by front-line staff to the management of medical and social support services for specific populations through the creation of large health care organizations [16]. Goals common to all approaches are to provide the best quality, most appropriate and effective services, and reduce overlap, duplication and gaps in care [17, 18].
Research on coordination of individual care demonstrates that proactive and comprehensive care that includes health and social services improves health outcomes [19, 20]. The quantity, type and source of comprehensive care will vary according to the needs and resources of the client at particular points in time [19, 21]. For example, clients with chronic hepatitis C, a chronic infectious illness spread by blood-to-blood contact, present with multiple and changing needs associated with the disease and compounded by social, economic and psychological factors [22, 23]. Responses to these needs increase partnership linkages, through social services, to other human services representing the broad determinants of health such as welfare, employment, and wage replacement [24].
IHSSP history and function
Interprofessional partnerships in health care have a long history [25, 26], as both public and not-for-profit agencies have worked together to coordinate services, pool resources and achieve shared goals [27, 28]. The public health literature contains many descriptions of interprofessional partnerships and guidelines for formation [29, 30]. IHSSP are initiated through formal and/or informal relationships in and across organizations and based on a common value, a holistic person-centred approach to care [31]. Nurses, as core providers in the provision of chronic illness care, frequently coordinate IHSSP [32]. Communication can occur in-person or through a variety of means such as phone, fax, e-mail and internet portals. IHSSP function in ways that transcend organizational boundaries [33] resulting in the emergence of virtual interorganizational structures [34]. IHSSP are defined in this paper as virtual interorganizational structures formed around client needs through formal and/or informal relationships of front-line health and social service providers from various organizations who collaborate to provide comprehensive and integrated care and support services to those with chronic conditions.
Although partnerships are widely embraced, research on the factors that influence their collaborative processes and outcomes is not well established [1, 2] and evidence of effectiveness is lacking [35–37]. There is evidence that partnerships frequently fail [38], they are complex to administer, time consuming to establish, require investment of scarce resources and have a potential for loss of decision-making control [27, 39, 40]. Separate funding streams for health and social services can complicate cooperative service planning and delivery requiring creativity and innovation to create service linkages. The increased emphasis on health system performance improvement through partnerships and the concomitant need to demonstrate that partnerships are functioning efficiently led to the aim of this paper to review partnership measurement issues, develop an IHSSP conceptual model and identify measurement tool/s for its evaluation [41].
Methods and theory
A literature review was performed on articles retrieved through three interrelated searches outlined in Table 1. The literature was searched to find: 1) issues associated with the measurement of partnerships, 2) the salient attributes of IHSSP processes at the front-line staff level and the interrelated contextual factors of importance for measurement, and 3) tools to measure IHSSP functioning at the front-line service provider group level. It is important to note that the aim of search two did not include identification of literature for development of a predictive model with weighted criteria.
Table 1.
Search strategies.
| Timeframe | 1990–2007 |
| Key words and terms combined for Search 1: | ‘Partnership’ and ‘interprofessional’ and ‘measurement’ |
| Partnership measurement and Search 2: Partnership characteristics | Search 2 dropped measurement term. Synonyms and variations of keywords were employed in the first 2 searches to expand and refine the search scope. Synonyms included: ‘patient care team’, ‘collaboration’, ‘interdisciplinary’, ‘multidisciplinary’, ‘delivery of health care’ and ‘evaluation’ |
| Search 3: Partnership measurement tools | ‘Partnership’ or ‘teamwork’ or ‘patient care team’, and ‘scales’, ‘tools’ and ‘questionnaires’. |
| Restrictions | English language, peer reviewed systematic reviews, primary research, conceptual articles, government research reports and books |
| Databases searched | Cochrane Database of Systematic Reviews, Clinical Evidence, MEDLINE, CINAHL, EMBASE, PsychINFO, and Health and Psychosocial Instruments, Google, Google Scholar |
| Hierarchy of evidence | In ascending order systematic review articles (e.g. syntheses of research, concept analysis) single studies, articles and books |
| Types of literature | Nursing, medicine, social sciences and psychology (including selected references from organizational development) |
| Other documents added to the literature review | Seminal works added as required to complete writers' understanding of the concepts. Reference sections were hand searched to ensure completeness |
The search method was iterative starting with broad searches of online databases and the authors' personal libraries, selecting relevant articles, identifying the articles' main Mesh Headings, and repeating the electronic search using refined terms and, for selected articles, using the online ‘find similar’ reference feature. Hand searching reference sections of selected articles and electronic searches of leading authors were also conducted.
The thematic analysis [42] was guided by complexity theory, a contemporary form of systems theory. For example, complexity theory was used to guide the selection of attributes to be measured, cluster the attributes into themes and conceptualize the pattern of interrelationships within the context of an IHSSP as a complex adaptive system [43].
The literature obtained from search one was analyzed to identify the issues and gaps of partnership measurement. The literature from search two was analyzed to identify the salient attributes of IHSSP processes at the front-line staff level and the interrelated contextual components of the conceptual framework. Salient attributes were defined as the recurrent characteristics of the concept of IHSSP found within systematic reviews and concept analysis [44]. All articles were read several times by the principal investigator (GB) to identify and code the themes. Qualitative analysis software, NVivo 7, was used to facilitate interrogation, refine the coding structure and organize the thematic relationships. The process was repeated by a trained research assistant to ensure that consensus was achieved.
Tools to measure partnership functioning identified in search three were required to meet all of the following criteria to be considered for full review: a) the purpose of the instrument is to assess partnership processes at the level of the group, b) the tool has good theoretical concordance with our conceptualization i.e. the salient attributes and theory base, c) there is at least one published reliability and validity assessment, d) the instrument is suitable for self-report and, e) is currently available for use. The criteria were applied in ascending order and tools were rejected at the first failed criteria point. This process was necessary to ensure that the most robust and well-developed tools would be located and evaluated [45] and would fit with the chosen theoretical framework of complexity theory.
Review of the selected instruments, guided by criteria identified by Streiner and Norman [45], included a description of the tool, the history of development, theoretical relevance, ease of use, reliability, and validity. Reliability included appraisal of test-retest and internal consistency and sensitivity. Assessments of validity included a review of face, content, construct, predictive, criterion, and discriminant validity.
Results
The papers retrieved were from Canada, USA, UK, Europe and Australia.
Issues associated with the measurement of IHSSP
IHSSP measurement is complicated by the fact that there is no standard interpretation of the concept of partnerships [46]. Other challenges involve variations in form, content and change over time. Partnerships occur in numerous forms, vary in depth of involvement, number and diversity of members (including diverse views and agendas), and are established through a process of negotiation [41]. Even if the members remain constant their relationships can change over time [47]. Comparing the findings from partnership research is problematic due to the conceptual variation, the variety of research methods used and the tendency of disciplines to work within their respective research paradigms and theoretical perspectives with little crossover or mutual recognition (evidenced through lack of cross-discipline citations) [46, 48–50]. Additionally, different stakeholders may attach different weights to success criteria [51–53]. The diverse views associated with partnerships and their measurement has added breadth to the field but a consensus view of partnerships has not yet emerged.
There is an abundance of support for partnerships and rhetoric on their advantages in the literature but the evidence-base is lacking [35–37]. Partnerships have been evaluated in a few studies that measured outcomes in client or population health and the quality of the group's collaborative process but the results are inconclusive [54–56]. Aside from methodological deficiencies, an explanation for the lack of positive clinical outcomes is that these outcomes may take years to realize and would fall outside most study timeframes [33]. Partnership process outcomes, on the other hand, occur earlier and can be measured at different time points. However, the literature on front-line staff collaborative processes focuses on relationships with clients largely ignoring relationships with colleagues [57]. The research on healthcare teams has focused on single elements that have been studied individually within the context of formal meetings [58]. Collaboration that occurs outside meetings is unstudied.
In this paper the assumption is made that collaborative processes may not be sufficient to improve health outcomes, but that quality interprofessional collaborative processes are necessary precursors to improved services and outcomes for individuals and populations with chronic conditions. Thus, the measurement of interprofessional collaborative processes is a necessary step in understanding whether quality processes contribute to better health outcomes.
Theoretical implications of complexity theory to IHSSP functions
IHSSP are complex adaptive systems as conceptualized through complexity theory [59]. As such, IHSSP were considered as self-organizing interorganizational systems that experience change within the group and are influenced, but not controlled by factors external to the group. For example, as nursing and other providers self-organize in response to the needs of those with chronic illness, IHSSP are created through increases in connectivity (number of partners), diversity (type of partners) and interactions (frequency of interactions). The increase in information flow and feedback loops precipitate mutual adjustment of, for example, behaviours, beliefs, or plans in response to changing demands. Mutual adjustment occurs through learning that allows for creativity, reflection and evaluation. Mutual adjustment is a type of change process in which the outcomes are unpredictable and small changes can have large effects by changing the context for others in the partnership [60]. The culmination of change through mutual adjustment is termed ‘adaptation’ otherwise referred to as emergence, innovation and synergy [61, 62]. Thus, the complexity of chronic illness management requires that IHSSP be responsive to unpredictable changes in clients' chronic condition/problems [63]. Adapting plans and practices to changing conditions requires responsive and flexible partnership processes in order to produce the desired outcomes and impact [64, 65].
Identification of salient attributes and conceptualization of IHSSP
The analysis began with review papers in accordance with the hierarchy of evidence in Table 1. The papers from which the salient attributes of IHSSP were primarily selected were reviews of empirical studies of the determinants of interprofessional collaboration [66–68], a review of theory and research on interagency collaboration in the public sector [69], and concept analyses of health care partnerships [70–72].
The attributes of IHSSP to be measured that were selected from the data are itemized in Table 2 within four thematic areas; 1) agreement of the need to partner, which was the most frequently recurring theme in the literature, 2) collegial relationships, a theme which contains items related to interprofessional communication, 3) interdependency, a theme that is stressed in the literature as central to group functioning, and 4) a final cluster, entitled power and leadership, which represents attributes consistent with shared power and leadership through influence.
Table 2.
Salient attributes, moderators, and outcomes of Interprofessional Health and Social Service Partnerships (IHSSP).
| IHSSP feature | Theme | Description or sub-themes |
|---|---|---|
| I. Salient attributes | 1. Agreement | Recognize and accept the need for partnership |
| 2. Collegial relationships | a. Reciprocity – mutually beneficial, mutual support, encouragement and feedback | |
| b. Communication – transparent, open, and honest, understanding of how discipline's work contributes to goals and able to communicate that contribution to others, constructive negotiation of goals, plans, and boundaries, compromise, active listening, face-to-face or virtual | ||
| c. Mutual trust – trust depends on skills, knowledge and experience and confidence in one's professional role, confidence in each other | ||
| d. Respect – aware of and values the contributions and perspectives of others | ||
| e. Equal status | ||
| f. Conflict management | ||
| 3. Interdependency – between two or more professionals | a. Sharing – goals, philosophy, values, advocacy, accountability, knowledge (professional, community resources), responsibility, planning and intervention | |
| b. Willingness to cooperate rather than compete, enthusiasm | ||
| c. Voluntary – sharing time, resources, energy | ||
| d. Permeable boundaries – recognize areas of interdependence and respect areas of independence, flexibility | ||
| e. Presence of synergy | ||
| 4. Power and leadership – through influence | a. Shared within the group | |
| b. Based on knowledge and experience | ||
| c. Consensual and egalitarian decision-making | ||
| II. Moderating factors-organizational | 1. Structure | a. Hierarchical emphasis on power and control |
| b. Horizontal or decentralized emphasis on flexible structures and teamwork | ||
| c. Community vs. hospital setting | ||
| 2. Philosophy and culture | Values participation and interdependence vs. dominance | |
| 3. Administrative support | Rules and procedures for collaboration | |
| 4. Resources | Funding mechanisms, human resource sharing, diverse and competing commitments | |
| 5. Coordination and communication mechanisms | ||
| 6. Sustainability | Conflicts with organizational self-interests, domain, autonomy | |
| 7. Clinical guidelines | ||
| II. Moderating factors – systemic | 1. Social, professional, culture, educational and resources | a. Socialization – hierarchies i.e. power differences between professions, gender stereotypes, differences in social status |
| b. Professional – jurisdictional, regulatory and medico-legal factors (individual vs. collective accountability), values and ideologies, job security, terminology | ||
| c. Cultural – individualism, autonomy, territoriality, specialization, control | ||
| d. Educational – limited knowledge, understanding and valuing of the roles of other disciplines, | ||
| e. Financial resources – professional compensation mechanisms (collective agreements, fee-for-service, organization bound vs. individual), institutional and intersectoral funding | ||
| III. Outcomes | 1. Partnership functioning | |
| 2. System capacity | ||
| 3. Individual and population health outcomes |
The attributes selected are congruent with complexity theory, i.e. attributes which contribute to self-organization, connectivity, diversity and interactions. Agreement of the need to partner is a necessary, if not sufficient, requirement for self-organization. It affects the number and diversity of partners and the frequency of their interactions. Collegial relationships impact the information flow of a system, affecting the level of mutual adjustment and resulting interdependency. Attributes of leadership and power are characteristic of a self-organizing system as they emphasize a shared process that occurs through influence rather than a position of power and control.
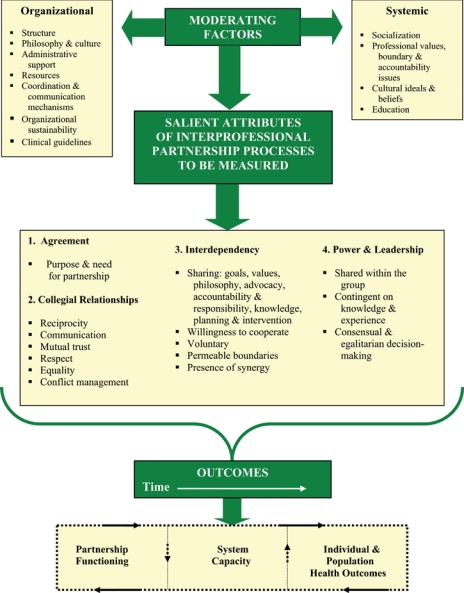
Figure 1 displays our conceptualization of the attributes of interprofessional collaborative processes to be measured situated within the interorganizational system that contains external influences or moderating factors and outcomes. The processes within and between the components of the system are dynamic but displayed as linear for the purposes of heuristic simplicity. The external factors that influence IHSSP member's participation found in the literature are termed ‘organizational’ and ‘systemic’ factors, detailed in Table 2 and displayed in Figure 1. Organizational and systemic influences are conceptualized as moderating or influencing factors as they can act as both barriers as well as enhancing factors [73]. Finally, outcomes of interprofessional processes complete the conceptual model in Figure 1 and are presented under the categories of Partnership Functioning, System Capacity and Individual/Population Health Outcomes. These outcomes are interrelated and assumed to be time dependent with quality partnership processes leading initially to beneficial outcomes for the partnership. Feedback loops within the system could result in changes in the moderating factors such as benefits to the partner's parent organization or changes in wait time policies. Outcomes related to moderating factors are termed ‘system capacity’ in Figure 1.
Figure 1.
Conceptual model showing the salient attributes of IHSSP within the interorganizational system.
The final category, Individual and Population Health Outcomes, includes partnership outcomes such as client satisfaction, improved health and quality of life, and reduced incidence of disease.
Selection and evaluation of measurement tools
A total of 171 instruments were screened for review, of which, 168 were rejected because they did not have an explicit theory base from which to determine concordance with the conceptual model as required by the second inclusion criteria. Of the remaining three instruments, one instrument—the Task Force Member survey—was grounded in theory but rejected as we were unable to obtain the instrument or a history of its development and testing [74]. Thus, only two instruments met our stringent selection criteria, the Partnership Self-Assessment Tool (PSAT) [75], and the Team Climate Inventory (TCI) [76].
The Partnership Self-Assessment Tool (PSAT), was developed by public health specialists for practical use by groups working to promote health and well-being in their communities [2]. It measures partnership synergy and other related dimensions of the partnership process [77]. This self-administered tool, takes 20 minutes to complete, contains 11 domains, and 67 clearly written and easily understood items. Seventeen items employ a dicotomous yes/no scale and 50 use a 5-point Likert scale. The originators caution that the PSAT is not intended for use by external evaluators to avoid the social desireability bias inherent when evaluations are perceived to be tied to funding decisions.
The Team Climate Inventory (TCI), a self-administered measure of team innovativeness was rigorously developed by organizational psychologists Neil Anderson and Michael West [78].
It was developed for research and practical use to evaluate team functioning at the level of the group [78].
The TCI has three versions, with 61, 38 or 14 clearly written and easily understood items that are scored on 5 to 7-point Likert scales [76]. The 38-item scale which contains an additional six items inserted to measure social desirability bias [79] is referred to in this paper as a 38-item scale. It is the most frequently reported version, is available for purchase (starter kit $495 USD, group norms and scoring software provided), and requires only 15 minutes to complete. The level of analysis is the group (permanent or semi-permanent) within an organization.
The items in both the PSAT and TCI exhibit concordance with the salient attributes of IHSSP as illustrated in Table 3. The TCI does not have an item match in theme 1, Agreement (agreement to participate is a basic assumption of their theory), while the PSAT had items matches in all themes. Item matching of the TCI with the PSAT, shown in Table 4 reveals that the TCI matches are mainly related to group synergy which is in accordance with the stated purpose of the tool.
Table 3.
Concordance of the Partnership Self-Assessment Tool (PSAT) and the Team Climate Inventory (TCI) with the identified attributes of IHSSP.
| Conceptual model | PSAT item # | TCI item # |
|---|---|---|
| Salient attributes | ||
| 1. Agreement | 53 | |
| 2. Collegial relationships | 14, 15, 16, 17, 24, 32, 59, 60, 62, 63 | 12, 15, 16, 17, 18, 19, 20, 21, 22, 23, 26 |
| 3. Interdependency | 1, 2, 3, 4, 5, 6, 7, 8, 9, 11, 13, 18, 19, 22, 23, 25, 26, 28, 31, 49, 63, 65, 66, 67 | 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 24, 25, 27, 28, 29, 30, 31, 33, 34, 35, 36, 37, 38 |
| 4. Power and leadership through influence | 10, 12, 42, 43, 44, 57, 64 | 13, 14 |
| Moderating factors | 21, 33–41, 56, 58, 61 | |
| Outcomes | 20, 27, 45–48, 50–52, 54–55 | 32 |
Table 4.
Team Climate Inventory (TCI) item matched with Partnership Self-Assessment Tool (PSAT) items.
| PSAT items (n=67) | TCI items (n=38) |
|---|---|
| Synergy | |
| Items 1–9 (9 items) | Items 1–5, 7–11, 24, 27–31, 36 (17 items) |
| Leadership | |
| Items 10–20 (11 items) | Items 12–13, 16–17, 25–26 (6 items) |
| Efficiency | |
| Items 21–23 (3 items) | No matches |
| Administration and management | |
| Items 24–32 (9 items) | Items 15, 18, 20–22, 33–35, 37–38 (10 items) |
| Non-financial resources | |
| Items 33–38 (6 items) | No matches |
| Financial and other capital resources | |
| Items 39–41 (3 items) | No matches |
| Decision making | |
| Items 42–44 (3 items) | Item 14 (1 item) |
| Benefits of participation | |
| Items 45–55 (11 items) | Item 32 (1 item) |
| Drawbacks of participation | |
| Items 56–62 (7 items) | No matches |
| Satisfaction with participation | |
| Items 63–67 (5 items) | Items 6, 19, 23 (3 items) |
Both measures have well-described theoretical frameworks that are consistent with complexity theory as both take a complex adaptive systems perspective toward group process. The PSAT is based on partnership synergy theory [2, 62]. Synergy is defined as “the breakthroughs in thinking and action that are produced when a collaborative process successfully combines the complementary knowledge, skills and resources of a group of participants” [80]. Attributes of improved thinking include creativity, invention, challenging the status quo and innnovative problem-solving [81, 82]. The theory considers synergy a proximal outcome of good quality partnership processes [62].
The concept of synergy, as used in the PSAT, is a surrogate for the concept of adaptation in complexity theory. Both concepts are assumed to represent the ultimate proximal outcome of successful partnership processes. Additionally, successful processes require the ability of partners to interact effectively in order to understand and address complex problems and sustain interventions. Success is related to who is involved (number and diversity of members) and how they are involved which includes fluent and frequent interactions and shared leadership (a bottom up, self-organized approach to problem-solving).
The TCI is based on the four-factor theory of climate for innovation [83], a well-studied model of team innovation [79]. This theory assumes teams are the principal means in which a climate of sharing grows, through active social construction, and becomes embedded within the organization [84, 85]. Three criteria determine a team: 1) work interactions occur at least infrequently, 2) a common goal or outcome serves as the impetuous for collective action, and 3) interdependent tasks require the group members to develop a shared understanding and expected patterns of response [85]. Climate for innovation is defined as, “the manner of working together that the team has evolved” [78]. Innovation is defined as “ the intentional introduction and application within a role, group or organization of ideas, processes, products or procedures, new to the relevant unit of adoption, designed to specifically benefit role performance, the group, the organization or the wider society” [86]. Creativity is considered to be part of the innovation process [87].
Innovation, as described in the four-factor theory, is synonymous with the concept of adaptation within complexity theory i.e. the introduction and application of new ideas or processes that benefit the group, organization or society. Climate is presented as a collective level phenomena requiring self-organization, connectivity and feedback loops as precursors to innovation. For example, task interdependence leads to shared understandings and expected levels of behaviour. Interactions are participatory and new ideas are encouraged in congruence with a bottom up approach. A common goal or attainable outcome (agreement of the need to collaborate, an assumption in their model) unites individuals to collective action (feedback loops).
Both the PSAT and TCI have reported measures of reliability and validity which are summarized in Table 5. The PSAT is in the early stages of testing with the data confined to the originators [2] and one mention of criterion validity by Browne [88]. Establishment of face and content validity during development of the PSAT items was rigorous. It included data from qualitative interviews with members of community health promotion partnerships, an extensive review of relevant literature and measures, as well as input from a panel of experts [2]. Items were constructed at the group level and pretested in 2 series (n=11×2) of cognitive (think-aloud) interviews to be sure the items were relevant, clear and consistently interpreted, reduce the likelihood of measurement error, improve content validity and minimize the burden on participants [45, 89].
Table 5.
Comparison of Partnership Self-Assessment Tool (PSAT) and Team Climate Inventory (TCI) reliability and validity.
| Dimensions | Criterion | PSAT | TCI |
|---|---|---|---|
| Background | History since | 2002 | 1994 |
| # Items | 67 | 38 | |
| Purpose | Practical use and self-evaluation by groups | Research and practical use | |
| Target group | Generic community-based health partnerships | Generic organization-based professional teams | |
| Reliability | Measures of stability of instrument | ||
| • Test-retest | Ability to produce the same results on short-term repeated measures – uo to 6 weeks | No data | No data |
| • Internal consistency | Tests for internal consistency should indicate items are moderately correlated with each other (α-coefficients between 0.20 and 0.80) and well-correlated with the total score (α-coefficients between 0.70 and 0.90) [90, 91] | 1 study, items within each factor are highly-correlated, α-coefficients between 0.83–97 [2] | Three studies, consistently yield results within advised ranges [76, 92, 93] |
| • Sensitivity | Ability of instrument to measure change on repeated measures e.g. before and after an intervention | No data | 1 study – did not show change [93] |
| Validity | Degree to which tool items measure concept | ||
| • Face and content | Literature review, interviews and expert review determine items appear to measure all the important components of the concept | Rigorously established [2] | Rigorously established [78] |
| • Construct | Tests to determine the relationship between multiple variables i.e. exploratory and confirmatory factor analysis | 1 study of exploratory factor analysis with positive results [2] | Three studies reporting positive results of exploratory and confirmatory factor analysis [76, 94, 95] |
| • Predictive | Degree to which the test scores are predictive of a desired criterion | No data | Demonstrated in three studies [92, 96, 97] |
| • Criterion | Scores on the tool are compared to results of external evaluators or other related tools | 2 studies: 1 compared to tools with more and less relatedness, results confirmed hypothesized relationship [2, 88] | Five studies compared TCI scores to external evaluators, results positively correlated [79, 92, 96, 98, 99] |
| • Discriminant validity | Extent to which tools can distinguish between different types of groups | Demonstrated in 1 study [2] | Demonstrated in two studies [100, 101] |
The PSAT was tested in 63 health-related partnerships in operation at least 18 months in urban, suburban or rural areas in the US [2]. Reliability testing of internal consistency of the scales with the total score as measured by Cronbach's α (0.82–0.97) was good. Construct validity through factor analysis of the nine items on the synergy scale (0.742–0.893) indicated good internal construct validity. Between group discriminant validity evaluated by one-way analysis of variance tests indicated that the PSAT adequately discriminates between groups as results of within group variation were significantly (p≤0.01) less than the between group variations. Criterion validity demonstrated through comparison of the PSAT with two more and less related measures evidenced that the PSAT measures different but related constructs. The closely related measure showed a moderate correlation of 0.71 (p<0.01). Exploratory factor analysis of the items in each tool revealed each had a major and distinct factor, synergy for the PSAT and collaborative group performance for the comparator [2]. The PSAT had a low correlation (r=0.13–0.36) with the less related measure of partnership structure [88].
The TCI has performed well on reliability and validity testing in several countries and organizational cultural contexts including community-based health and social services settings. Face and content validity was established through a rigorous process of initial scale development [78]. For example, items were selected from the literature and other published measures of climate only if they were relevant to the four-factor theory and occurred at the group level.
Reliability tests of internal consistency have consistently been within recommended ranges. The items are moderately correlated with each other (α-coefficient 0.35–0.62) [76]. Internal consistency of tool scores are consistent across countries e.g. α-coefficient of 0.84–0.94 in the UK [76], 0.86–0.91 in Sweden [92] and an α-coefficient of 0.84–0.90 in Canada [93]. Only one study has reported on the TCI's ability to measure change (sensitivity) [93]. Measures taken 9 weeks apart on both the 38-item and 14-item TCI showed high positive correlations between the scores on the scales at both administrations (α 0.61–0.87). However, it was predicted that a sensitive measure would show a change as the teams were given training to increase team work at the beginning of the project. It is possible that change occurred but the TCI was not sensitive or the study timeframe was too short for significant change to occur within the newly formed teams.
Criterion validity tested through comparison with the Team Production Questionnaire showed a positive correlation of 0.14–0.51 but the power of the sample (n=16 teams) was small and not all correlations were statistically significant, indicating that the TCI may be measuring similar as well as different constructs [92]. However, several studies have compared external evaluations of the amount of innovativeness of the teams with the TCI scores and found good concordance evidencing criterion validity [79, 92, 96, 98, 99].
Construct validity of the 61 and 38-item versions of the TCI tested through exploratory and confirmatory factor analysis by several researchers has produced mixed results on whether the TCI contains four or five factors. Exploratory factor analysis on the longer version in the UK indicated there are five interrelated factors [76]. Confirmatory factor analysis completed in the UK on the 38-item version of the TCI was equivocal for the four- and five-factor model [76]. The authors chose the five factor version to maximize the predictive utility. Ragazzoni et al. [95] confirmed five factors in the 38-item Italian version. Testing by Kivimäki, et al. [94] on a Finnish sample of 2,265 local government employees indicated that the five-factor version performed better than the four-factor version in work groups with high job complexity while the four-factor version was adequate for those with low job complexity. The findings indicate that the five-factor scale is the most relevant for IHSSP due to the complexity of their work.
Between-group discriminant validity is adequate. Williams and Laungani [101] demonstrated the TCI distinguished primary health care teams from three other types of health care teams and Bain, Mann and Pirola-Merlo [100] showed the TCI discriminated between research and development teams (n=38).
Several studies have shown the TCI is predictive of team innovation [92, 96, 97]. For example, Anderson and West [96] found that the factor, support for innovation, predicts overall innovation (accounting for 46% of the variance) and innovative novelty. The factor, participative safety, best predicts the number of innovations and team self-reports of innovativeness while task orientation predicts administrative effectiveness.
Summary of the PSAT and TCI evaluation
The PSAT and TCI theoretical frameworks were compatible with the underpinnings of our conceptual model. The PSAT items demonstrated a better fit with the entire model while the TCI items exhibited a fit specifically with the salient attributes. Both tools have rigorously demonstrated face and content validity. The PSAT is relatively new and has had minimal reliability and validity testing. The TCI is a mature tool that has performed well on a diverse array of tests, in many cultures and contexts. Both measures are appropriate for health and social services groups. Neither measure has demonstrated utility as a longitudinal measure of change. Both could be used for IHSSP measurement research.
Discussion
This paper reviewed a broad and diverse literature that highlighted the issues relevant to the measurement of IHSSP of front-line staff within an interorganizational context. IHSSP were presented as necessary for the delivery of services to individuals and populations with chronic conditions in order to meet changing client needs. A new conceptual model was presented that assumes interrelatedness between the salient attributes of group process, the external factors that influence group process and outcomes. The conceptual model contains both a theoretical perspective and the partnership context as necessary elements [102]. This model addresses limitations pointed out by Allen and Hecht [103] in their review of the effectiveness of organizational teams “the organizational context in which teams operate is rarely considered even though context is quite likely to influence team success”. (p.452)
The complexity theory-bound conceptual model may be useful for IHSSP that go beyond the front-line staff level as reviews of empirical research in the UK suggest that health and social care partnership have common principles regardless of the organizational level [41]. Refinement and testing of the model from multiple perspectives would improve the theoretical formulation and could lead to a mid-range theory to ground research and clinical practice.
Although IHSSP constitute virtual interorganizational structures formed in response to client needs, measurement in this paper was limited to proximal outcomes of IHSSP processes. Measurement of partnerships should include assessment of structural features as well as the processes [104]. Since the measurement of partnership structure was beyond the scope of this paper readers are referred to the seminal works of Milward and Provan [105], Provan and Milward [56], and Provan, Milward and Isett [106] on measurement of partnership networks and that of Browne and colleagues [88] who developed and tested a detailed tool to identify, describe and evaluate the structural elements of partnerships.
The evaluation of two tools, the PSAT and TCI, provided evidence of their validity for IHSSP process measurement. While both tools have a good theoretical fit with the model and the salient attributes of IHSSP only the PSAT included measurement of contextual influences. The TCI would require supplementation with qualitative research to uncover effects of contextual influences. The evaluation also included consideration of the instruments' psychometric properties. There was ample evidence that the TCI has strong psychometric properties while knowledge of the PSAT's performance is limited. Research using the PSAT would require consideration of inclusion of psychometric testing. However, the best tool is one that matches the partnership model, the community context, needs and goals of the partnership members and other stakeholders and the goals of the researcher [102]. In consideration of the above, we chose to trial the PSAT for practical use and research with four IHSSP comprised of members from several agencies dedicated to providing care to those with chronic hepatitis C in small urban environments.
Conclusion
The new theory-based conceptualization of IHSSP of front-line staff who provide chronic illness care provides the underpinnings for a comprehensive evaluative framework for partnerships. Two partnership process measurement tools, the PSAT and TCI are valid for IHSSP measurement research with consideration of their strengths and limitations. Future research is required to test and refine the conceptual model and to develop a comprehensive evaluative framework for IHSSP.
Contributor Information
Gail Butt, School of Nursing, University of British Columbia, Associate Director, BC Hepatitis Services, BC Centre for Disease Control, 655 West 12th Avenue, Vancouver, BC, V5Z 4R9 Canada.
Maureen Markle-Reid, Ontario Ministry of Health and Long-Term Care, Health Research Personnel Development Fund, Associate Professor, School of Nursing, McMaster University, 1200 Main Street West, HSC 3N28A, Hamilton, Ontario L8N 3Z5 Canada.
Gina Browne, System-Linked Research Unit, Director, CLEAR Unit, Professor, Nursing; Clinical Epidemiology and Biostatistics and Ontario Training Centre in Health Services and Policy Research (OTC), McMaster University, Faculty of Health Sciences at Frid, Building T30, 75 Frid Street, Hamilton, Ontario, L8P 4M3 Canada.
Reviewers
Mark Harris, Professor, Executive Director, Centre for Primary Health Care and Equity, University of New South Wales, NSW, Australia
Terrence Montague, MD, Professor of Medicine, Director-General, Health Management Research Group University of Montreal, Quebec, Canada and Sara Ahmed, PhD, Faculty of Medicine, Occupational and Physical Therapy, McGill University, Montreal, Quebec, Canada
One anonymous reviewer
References
- 1.Polivka BJ, Dresbach SH, Heimlich JE, Elliott M. Interagency relationships among rural early intervention collaboratives. Public Health Nursing. 2001;18(5):340–9. doi: 10.1046/j.1525-1446.2001.00340.x. [DOI] [PubMed] [Google Scholar]
- 2.Weiss E, Anderson R, Lasker R. Making the most of collaboration: exploring the relationship between partnership synergy and partnership functioning. Health Education & Behavior. 2002;29(6):683–98. doi: 10.1177/109019802237938. [DOI] [PubMed] [Google Scholar]
- 3.Boswell C, Cannon S. New horizons for collaborative partnerships. [cited 2007 Sep 15];Online Journal of Issues in Nursing [serial online] 2005 10(1) Available from: http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Volume102005/No1January31/tpc26_216009.aspx. [PubMed] [Google Scholar]
- 4.Conrad DA. Coordinating patient care services in regional health systems: the challenge of clinical integration. Hospital & Health Services Administration. 1993;38(4):491–508. [PubMed] [Google Scholar]
- 5.Fleury M-J, Mercier C. Integrated local networks as a model for organizing mental health services. Administration and Policy in Mental Health. 2002;30(1):55–73. doi: 10.1023/a:1021227600823. [DOI] [PubMed] [Google Scholar]
- 6.Nasmith L, Cote B, Cox J, Inkell D, Rubenstein H, Jimenez V, et al. The challenge of promoting integration: conceptualization, implementation, and assessment of a pilot care delivery model for patients with type 2 diabetes. Family Medicine. 2004 Jan;36(1):40–5. [PubMed] [Google Scholar]
- 7.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded chronic care model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hospital Quarterly. 2003;7(1):73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 8.Wagner EH, Austin BT, von Korff M. Organizing care for patients with chronic illness. The Milbank Quarterly. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 9.World Health Organization. Preparing a health care workforce for the 21st century: the challenge of chronic conditions. Geneva: World Health Organization; 2005. [cited 2007 Mar 18]. Available from: http://whqlibdoc.who.int/publications/2005/9241562803.pdf. [Google Scholar]
- 10.Department of Health. Partnership in action: new opportunities for joint working between health and social services. London: NHS; 1998. [Google Scholar]
- 11.Department of Health. Modernising health and social services: national priorities guidance. London: NHS; 1998. [Google Scholar]
- 12.Glouberman S, Zimmerman B. Complicated and complex systems: what would successful reform of medicare look like? Ottawa: Commission on the Future of Health Care in Canada; 2002. [Google Scholar]
- 13.Romanow RJ. Building on values: the future of health care in Canada – final report. Ottawa: Commission on the Future of Health Care in Canada; 2002. [Google Scholar]
- 14.Department of Health. The new NHS: Modern, dependable. London: The Stationary Office; 1997. [Google Scholar]
- 15.Glendinning C. Breaking down barriers: integrating health and care services for older people in England. Health Policy. 2003;65(2):139–51. doi: 10.1016/s0168-8510(02)00205-1. [DOI] [PubMed] [Google Scholar]
- 16.Leutz WN. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. The Milbank Quarterly. 1999;77(1):77–110. doi: 10.1111/1468-0009.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leatt P, Pink GH, Guerriere M. Towards a Canadian model of integrated healthcare. Healthcare Papers. 2000 Spring;1(2):13–35. doi: 10.12927/hcpap..17216. [DOI] [PubMed] [Google Scholar]
- 18.van Eyk H, Baum F. Learning about interagency collaboration: trialing collaborative projects between hospitals and community health services. Health and Social Care in the Community. 2002;10(4):262–9. doi: 10.1046/j.1365-2524.2002.00369.x. [DOI] [PubMed] [Google Scholar]
- 19.Browne G, Roberts J, Byrne C, Gafni A, Weir R, Majumdar B. The costs and effects of addressing the needs of vulnerable populations: results of 10 years of research. Canadian Journal of Nursing Research. 2001;33(1):65–76. [PubMed] [Google Scholar]
- 20.Hay WI, van Ineveld C, Browne GB, Roberts J, Bell B, Mills MJ, et al. Prospective care of elderly patients in family practice: is screening effective? Canadian Family Physician. 1999;44:2677–87. [PMC free article] [PubMed] [Google Scholar]
- 21.Browne G, Roberts J, Gafni A, Byrne C, Weir R, Majumdar B, et al. Economic evaluations of community-based care: lessons from twelve studies in Ontario. Journal of Evaluation in Clinical Practice. 1999;5(3):1–19. doi: 10.1046/j.1365-2753.1999.00191.x. [DOI] [PubMed] [Google Scholar]
- 22.Butt G, Paterson BL, McGuinness L. Living with the stigma of hepatitis C. Western Journal of Nursing Research. 2008;30(2):204–21. doi: 10.1177/0193945907302771. [DOI] [PubMed] [Google Scholar]
- 23.Paterson BL, Butt G, McGuinness L, Moffat B. The construction of hepatitis C as a chronic illness. Clinical Nursing Research 2006 August 1. 2006;15(3):209–24. doi: 10.1177/1054773806288569. [DOI] [PubMed] [Google Scholar]
- 24.Leatt P. Integrated service delivery. Ottawa: Health Canada; 2002. [cited 2007 Mar 15]. Available from: http://www.hc-sc.gc.ca [Sharing the Learning: Health Transition Fund: Synthesis Series] [Google Scholar]
- 25.Mackay L, Soothill K, Webb C. Troubled times: the context for interprofessional collaboration. In: Soothill K, Mackay L, Webb C, editors. Interprofessional relations in health care. London: Edward Arnold; 1995. pp. 5–10. [Google Scholar]
- 26.Rawson D. Models of interprofessional work: likely theories and possibilities. In: Leathard A, editor. Going interprofessional: working together for health and welfare. London: Routledge; 1994. pp. 38–63. [Google Scholar]
- 27.Alter C, Hage J. Organizations working together. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 28.Herman KA, Wolfson M, Forster JL. The evolution, operation and future of Minnesota SAFPLAN: a coalition for family planning. Health Education Research: Theory and Practice. 1993;8(3):331–44. doi: 10.1093/her/8.3.331. [DOI] [PubMed] [Google Scholar]
- 29.Bolton LB, Georges CA, Hunter V, Long O, Wray R. Community health collaboration models for the 21st century. Nursing Administration Quarterly. 1998;22:6–17. doi: 10.1097/00006216-199802230-00005. [DOI] [PubMed] [Google Scholar]
- 30.Lezau D, Kingsbury L, Lenz B, Nelson C, Voehl S. Building coalitions: a community wide approach for promoting farming health and safety. American Association of Occupational Health Nurses Journal. 1993;41:440–9. [PubMed] [Google Scholar]
- 31.Pirkis J, Herrman H, Schweitzer I, Yung A, Grigg M, Burgess P. Evaluating complex, collaborative programmes: the partnership project as a case study. Australian & New Zealand Journal of Psychiatry. 2001;35(5):639–46. doi: 10.1080/0004867010060513. [DOI] [PubMed] [Google Scholar]
- 32.Sibbald B, Laurant M, Reeves D. Advanced nurse roles in UK primary care. The Medical Journal of Australia. 2006;185(1):10–2. doi: 10.5694/j.1326-5377.2006.tb00440.x. [DOI] [PubMed] [Google Scholar]
- 33.Provan KG, Nakama L, Veazie MA, Teufel-Shone NI, Huddleston C. Building community capacity around chronic disease services through a collaborative interorganizational network. Health Education and Behavior 2003 Dec 1. 2003;30(6):646–62. doi: 10.1177/1090198103255366. [DOI] [PubMed] [Google Scholar]
- 34.Durbin J, Rogers J, Macfarlane P, Baranek P, Goering P. Strategies for mental health system integration: a review. Final report. Toronto: Ontario Mental Health Foundation; 2001. Available from: http://www.camh.net/hsrcu/v2/publications/reports/consulting/practices.htm. [Google Scholar]
- 35.Butterfoss FD, Goodman RM, Wandersman A. Community coalitions for prevention and health promotion. Health Education Research: Theory and Practice. 1993;8(3):315–30. doi: 10.1093/her/8.3.315. [DOI] [PubMed] [Google Scholar]
- 36.Morris J. Encounters with strangers Feminism and disability. London: Women's Press; 1996. [Google Scholar]
- 37.Zwarenstein M, Reeves S. What's so great about collaboration? We need more evidence. British Medical Journal. 2000;320(15):1022–3. doi: 10.1136/bmj.320.7241.1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kreuter MW, Lezin NA, Young LA. Evaluating community-based collaborative mechanisms: implications for practitioners. Health Promotion Practice. 2000;1:49–63. [Google Scholar]
- 39.Cheadle A, Beery W, Wagner E, Fawcett S, Green L, Moss D, et al. Conference report: community-based health promotion – state of the art and recommendations for the future. American Journal of Preventive Medicine. 1997;13(4):240–3. [PubMed] [Google Scholar]
- 40.Wandersman A, Goodman RM, Butterfoss FD. Understanding coalitions and how they operate. In: Minkler M, editor. Community organizing and community building for health. New Brunswick, NJ: Rutgers University Press; 1997. pp. 261–77. [Google Scholar]
- 41.Halliday J, Asthana SNM, Richardson S. Evaluating partnership: the role of formal assessment tools. Evaluation 2004 Jul 1. 2004;10(3):285–303. [Google Scholar]
- 42.Charmaz K. Qualitative interviewing and grounded theory analysis. In: Gubrium JF, Holstein JA, editors. Handbook of interview research. Thousand Oaks: Sage; 2002. pp. 675–94. [Google Scholar]
- 43.Anderson RA, McDaniel Jr RR. Managing health care organizations: where professionalism meets complexity science. Health Care Management Review. 2000;25(1):83–92. doi: 10.1097/00004010-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 44.Rodgers BL. Concept analysis: an evolutionary view. In: Rodgers BL, Knafl KA, editors. Concept development in nursing. 2nd. Philadelphia: Saunders; 2000. pp. 77–102. [Google Scholar]
- 45.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 3rd. Oxford: Oxford University Press; 2003. [Google Scholar]
- 46.Ahgren B, Axelsson R. Evaluating integrated health care: a model for measurement. [cited 2007 Sep 15];International Journal of Integrated Care [serial online] 2005 Aug 31;5 doi: 10.5334/ijic.134. Available from: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldberg D, Comins M. Struggling with partners: the use of the term ‘partnership’ in practice. Anthropology & Medicine. 2001;8(2–3):255–64. [Google Scholar]
- 48.Alexander JA, Vaughn T, Burns LR, Zuckerman HS, Andersen RM, Torrens P. Organizational approaches to integrated health care delivery: a taxonomic analysis of physician-organization arrangements. Medical Care Research and Review. 1996;53(1):71–93. doi: 10.1177/107755879605300104. [DOI] [PubMed] [Google Scholar]
- 49.Bolland JM, Wilson JV. Three faces of integrative coordination: a model of interorganizational relations in community-based health and human services. Health Services Research. 1994;29(3):341. [PMC free article] [PubMed] [Google Scholar]
- 50.Lasker RD, Weiss ES. Broadening participation in community problem solving: a multidisciplinary model to support collaborative practice and research. Journal of Urban Health. 2003;80(1):14–47. doi: 10.1093/jurban/jtg014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boyne G, Farrell C, Law J, Powell M, Walker R. Evaluating public management reforms: Principles and practice. Buckingham: Open University Press; 2003. [Google Scholar]
- 52.Glendinning C. Partnerships between health and social services: developing a framework for evaluation. Policy and Politics. 2002;30:115–27. [Google Scholar]
- 53.Sullivan H, Skelcher C. Working across boundaries. Basingstoke: Palgrave; 2002. [Google Scholar]
- 54.Bickman L. Implications of a children's mental health managed care demonstration evaluation. Journal of Mental Health Administration. 1996;23:107–17. doi: 10.1007/BF02518647. [DOI] [PubMed] [Google Scholar]
- 55.Lehman AF, Postrado LT, Roth D, McNary SW, Goldman HH. Continuity of care and client outcomes in the Robert Wood Johnson foundation program on chronic mental illness. The Milbank Quarterly. 1994;72:105–22. [PubMed] [Google Scholar]
- 56.Provan KG, Milward HB. A preliminary theory of interorganizational network effectiveness: a comparative study of four community mental health systems. Administrative Science Quarterly. 1995;40(1) [Google Scholar]
- 57.Robinson LM. Promoting multidisciplinary relationships: a pragmatic framework for helping service providers to work collaboratively. Canadian Journal of Community Mental Health. 2005 Spring;24(1):115–27. doi: 10.7870/cjcmh-2005-0008. [DOI] [PubMed] [Google Scholar]
- 58.Cott C. “We decide you carry it out”: a social network analysis of multidisciplinary long-term care teams. Social Science & Medicine. 1997;45(9):1411–21. doi: 10.1016/s0277-9536(97)00066-x. [DOI] [PubMed] [Google Scholar]
- 59.Anderson RA, Crabtree B, Steele D, McDaniel R. Case study research: the view from complexity science. Qualitative Health Research. 2005;15(5):669–85. doi: 10.1177/1049732305275208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Plsek PE, Greenhalgh T. The challenge of complexity in health care. British Medical Journal. 2001;323:625–8. doi: 10.1136/bmj.323.7313.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Holden LM. Complex adaptive systems: concept analysis. Journal of Advanced Nursing. 2005;52(6):651–7. doi: 10.1111/j.1365-2648.2005.03638.x. [DOI] [PubMed] [Google Scholar]
- 62.Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Quarterly. 2001;79(2):179. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rowe W, Jacobs NF, Grant H. Facilitating development of organizational productive capacity: a role for empowerment evaluation. The Canadian Journal of Program Evaluation 1999 (Special Issue) :69–92. [Google Scholar]
- 64.Capra F. The hidden connections: integrating the biological, cognitive, and social dimensions of life into a science of sustainability. New York: Doubleday; 2002. [Google Scholar]
- 65.Wheatley MJ. Leadership and the new science: discovering order in a chaotic world. San Francisco: Jossey-Bass; 1999. [Google Scholar]
- 66.Curran V. Ottawa: Health Canada; 2004. Interprofessional education for collaborative patient-centered practice: research synthesis paper. Available from: http://www.hc-sc.gc.ca/hcs-sss/hhr-rhs/strateg/interprof/synth_e.html. [Google Scholar]
- 67.San Martin-Rodriguez LS, Beaulieu M-D, D'Amour D, Ferrada-Videla M. The determinants of successful collaboration: a review of theoretical and empirical studies. Journal of Interprofessional Care. 2005 May;19(Suppl 1):132–47. doi: 10.1080/13561820500082677. [DOI] [PubMed] [Google Scholar]
- 68.Canadian Health Services Research Foundation. Teamwork in healthcare: promoting effective teamwork in healthcare in Canada. Ottawa: 2006. [cited 2007 Sep 1]. Available from: http://www.chsrf.ca/research_themes/pdf/teamwork-synthesis-report_e.pdf. [Google Scholar]
- 69.Hudson B, Hardy B, Henwood M, Wistow G. In pursuit of inter-agency collaboration in the public sector: what is the contribution of theory and research? Public Management. 1999;1(2):235–60. [Google Scholar]
- 70.Bidmead C, Cowley S. A concept analysis of partnership with clients. Community Practitioner. 2005;78(6):203–8. [PubMed] [Google Scholar]
- 71.Hook ML. Partnering with patients – a concept ready for action. Journal of Advanced Nursing. 2006;56(2):133–43. doi: 10.1111/j.1365-2648.2006.03993.x. [DOI] [PubMed] [Google Scholar]
- 72.D'Amour D, Ferrada-Videla M, San Martin Rodriguez L, Beaulieu M-D. The conceptual basis for interprofessional collaboration: core concepts and theoretical frameworks. Journal of Interprofessional Care. 2005;19:116–31. doi: 10.1080/13561820500082529. [DOI] [PubMed] [Google Scholar]
- 73.El Ansari W, Phillips CJ, Hammick M. Collaboration and partnerships: developing the evidence base. Health and Social Care in the Community. 2001;9(4):215–27. doi: 10.1046/j.0966-0410.2001.00299.x. [DOI] [PubMed] [Google Scholar]
- 74.McMillan B, Florin P, Stevenson J, Kerman B, Mitchell RE. Empowerment praxis in community coalitions. American Journal of Community Psychology. 1995;23(5):699–727. doi: 10.1007/BF02506988. [DOI] [PubMed] [Google Scholar]
- 75.Center for the Advancement of Collaborative Strategies in Health. [cited 2007 Sep 1];Partnership Self-Assessment Tool 2006. Available from: http://www.cacsh.org/psat.html. [Google Scholar]
- 76.Anderson NR, West MA. Measuring climate for work group innovation: development and validation of the team climate inventory. Journal of Organizational Behavior. 1998;19:235–58. [Google Scholar]
- 77.Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. The Milbank Quarterly. 2001;79(2):179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Anderson NR, West MA. The team climate inventory. Manual and users' guide, Assessment Services for Employment. Windsor, UK: NFER-Nelson; 1994. [Google Scholar]
- 79.Mathisen GE, Einarsen S, Jørstad K, Brønnick KS. Climate for work group creativity and innovation: Norwegian validation of the team climate inventory (TCI) Scandinavian Journal of Psychology. 2004;45:383–92. doi: 10.1111/j.1467-9450.2004.00420.x. [DOI] [PubMed] [Google Scholar]
- 80.Lasker RD, Weiss ES. Creating partnership synergy: the critical role of community stakeholders. Journal of Health & Human Services Administration. 2003;26(1):119–39. [PubMed] [Google Scholar]
- 81.Gray B. Collaborating: finding common ground for multiparty problems. 1st. San Francisco: Jossey-Bass; 1989. [Google Scholar]
- 82.Richardson WC, Allegrante JP. Shaping the future of health through global partnerships. In: Koop CE, Pearson CE, Schwarz MR, editors. Critical issues in global health. San Francisco: Jossey-Bass; 2000. pp. 375–83. [Google Scholar]
- 83.West MA. The social psychology of innovation in groups. In: West M, Farr J, editors. Innovation and creativity at work: Psychological and organizational strategies. New York: Wiley; 1990. pp. 4–36. [Google Scholar]
- 84.Hosking DM, Anderson NR. Organizational change and innovation: Psychological perspectives and practices in Europe. London: Routledge; 1992. [Google Scholar]
- 85.West MA. Effective teamwork. Leicester: British Psychological Society; 1995. [Google Scholar]
- 86.West MA, Farr JL. Innovation at work: Psychological perspectives. Social Behaviour. 1989;4:15–30. [Google Scholar]
- 87.Amabile TM. Creativity in context. Boulder, CO: Westview Press; 1996. [Google Scholar]
- 88.Browne G, Roberts J, Gafni A, Byrne C, Kertyzia J, Loney P. Conceptualizing and validating the Human Services Integration Measure. [cited 2007 Sep 1];International Journal of Integrated Care [serial online] 2004 May 19;4:1–12. doi: 10.5334/ijic.98. Available from: http://www.ijic.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Forsyth B, Hubbard M. A method for identifying cognitive properties of survey items. In/reprint from: Proceedings of the Survey Research Methods Section ASA (1992) Alexandria, VA: American Statistical Association; 1992. pp. 470–5. [Google Scholar]
- 90.Henson RK. Understanding internal consistency reliability estimates: a conceptual primer on coefficient alpha. Measurement and Evaluation in Counseling and Development. 2001;34(3):177–89. [Google Scholar]
- 91.Streiner DL, Norman GR. A practical guide to their development and use. Oxford: Oxford University Press; 1991. Health measurement scales. [Google Scholar]
- 92.Agrell A, Gustafson R. The Team Climate Inventory (TCI) and group innovation: a psychometric test on a Swedish sample of work groups. Journal of Occupational and Organizational Psychology. 1994;67:413–151. [Google Scholar]
- 93.Loo R, Loewen P. A confirmatory factor- analytic and psychometric examination of the team climate inventory: full and short versions. Small Group Research. 2002;33(2):254–65. [Google Scholar]
- 94.Kivimäki M, Kuk G, Elovainio M, Thomson L, Kalliomäki-Levanto T, Heikkilä A. The Team Climate Inventory (TCI)–four or five factors? Testing the structure of TCI in samples of low and high complexity jobs. Journal of Occupational and Organizational Psychology. 1997;70:375–89. [Google Scholar]
- 95.Ragazzoni P, Baiardi P, Zotti AM, Anderson N, West M. Italian validation of the team climate inventory: a measure of team climate for innovation. Journal of Managerial Psychology. 2002;17(4):325–36. [Google Scholar]
- 96.Anderson NR, West MA. The Team Climate Inventory: the development of the TCI and its applications in teambuilding for innovativeness. European Journal of Work and Organizational Psychology. 1996;5:53–66. [Google Scholar]
- 97.Forrester RH. Team climate and innovation: an empirical study. Paper presented at the Fourth European Congress of Psychology, Athens, July 1995 [Google Scholar]
- 98.Burningham C, West MA. Individual, climate, and group interaction processes as predictors of work team innovation. Small Group Research. 1995;36:106–17. [Google Scholar]
- 99.West MA, Smith H, Feng WL, Lawthom R. Research excellence and departmental climate in British universities. Journal of Occupational and Organizational Psychology. 1998;71:261–81. [Google Scholar]
- 100.Bain PG, Mann L, Pirola-Merlo A. The innovation imperative: the relationships between team climate, innovation, and performance in research and development teams. Small Group Research. 2001;32:55–73. [Google Scholar]
- 101.Williams G, Laungani P. Analysis of teamwork in an NHS community trust: an empirical study. Journal of Interprofessional Care. 1999;13:19–28. [Google Scholar]
- 102.Granner ML, Sharpe PA. Evaluating community coalition characteristics and functioning: a summary of measurement tools. Health Education Research. 2004;19(5):514–32. doi: 10.1093/her/cyg056. [DOI] [PubMed] [Google Scholar]
- 103.Allen N, Hecht TD. The ‘romance of teams’: toward an understanding of its psychological underpinnings and implications. Journal of Occupational and Organizational Psychology. 2004;77:439–61. [Google Scholar]
- 104.Donabedian A. Explorations in quality assessment and monitoring, Volume 1: the definition of quality and approaches to its assessment. Ann Arbor: Health Administration Press; 1980. [Google Scholar]
- 105.Milward HB, Provan KG. Measuring network structure. Public Administration. 1998 Summer;76:387–407. [Google Scholar]
- 106.Provan KG, Milward HB, Isett KR. Collaboration and integration of community-based health and human services in a non-profit managed care system. Health Care Management Review. 2002;27(1):21–32. doi: 10.1097/00004010-200201000-00003. [DOI] [PubMed] [Google Scholar]