Abstract
Background
Vitamin D is important for gastrointestinal absorption of calcium and phosphorus, for bone mineralization, and is one useful therapeutic component in the prevention and treatment of osteoporosis and osteoporotic fractures. Low levels of 25 hydroxyvitamin D have been implicated as a risk factor for falls, for all fractures in general and for hip fractures in particular. At present there is a gap in the diagnosis and treatment of vitamin D deficiency in older adults with hip fractures.
Purpose
To explore the distribution of and correlates to levels of vitamin D in a population of patients with a recent hip fracture.
Sample
25 hydroxyvitamin D levels were measured in 526 screened subjects and 385 ultimately randomized patients who were part of the HORIZON RFT multinational trial, a randomized, placebo-controlled, double-blind trial testing the efficacy of a yearly intravenous bisphosphonate, zoledronic acid, in the prevention of new clinical fractures in patients with recent hip fracture repair.
Results
In screened patients, levels of 25 hydroxyvitamin D were low (median=14.7 ng/mL, IQR=7.80,22.5,), and 51% were at or below the clinically meaningful threshold of 15 ng/mL. In randomized patients, in bivariate analyses, level of 25 hydroxyvitamin D was significantly (p<0.05) related to male gender (r=0.12), calcium (r=0.16), and bone mineral density at the femoral neck (r=0.22). Low serum 25 hydroxyvitamin D (<15ng/mL) was related only to low calcium (odds=0.15 95%CI= 0.03, 0.63) in multivariate logistic models controlling for gender, age, race, BMI, living at home, alkaline phosphatase, and creatinine clearance. However, low serum calcium is an insensitive and poorly specific means of identifying patients with vitamin D deficiency, with an area under the ROC of 0.6.
Conclusions
We conclude that vitamin D insufficiency is a common problem in this population of subjects who have recently suffered a hip fracture. This insufficiency is related only to calcium in multivariable controlled models, but cannot be reliably identified or excluded by measuring serum calcium alone. Physicians should be encouraged to check and monitor serum levels of 25 hydroxyvitamin D, or to universally treat for vitamin D deficiency in patients experiencing a low trauma hip fracture.
Introduction
Vitamin D is important for gastrointestinal absorption of calcium and phosphorus, in bone mineralization and is a component of good dietary regimen 1, 2 particularly among those with osteoporosis 3. Vitamin D deficiency is common in older populations, particularly during the winter months, and in nursing home residents. However, the reported rates of vitamin D deficiencies are highly variable, ranging from 6% in healthy community-dwelling women 4 to 60% in nursing home residents 5 to 57% to 85% in a series of patients admitted 47 to the hospital 6. In a smaller sample of fracture patients than utilized here, Simonelli et al 1, found that over 50% had low vitamin D levels.
Low levels of vitamin D as assessed by serum 25 hydroxyvitamin D levels have been implicated as a risk factor for falls 4, 7 for fractures 8, 9 in general, and for hip fractures 10 in particular. A sequence in aging linking vitamin D deficiency, low serum calcium, and secondary hyperparathyroidism with increased bone resorption has been proposed 11.
Vitamin D supplementation has been shown to be a useful 4, 8 and cost-effective12 treatment for the prevention of fractures, maintaining or increasing BMD 13, and treatment post-hip fracture 9, 14, but, to date, is underutilized in the treatment after hip fractures15, 16. For example, Harrington et al. 16 reported that across several health systems in the U.S. only 14% of hip fracture patients were prescribed vitamin D. A challenge in the diagnosis and management of vitamin D deficiency in this population is the expense and lack of local availability of high-quality vitamin D assays, many of which do not accurately measure levels of 25 hydroxyergocalciferol (25(OH)D2), or vitamin D2 received from dietary sources and supplements.
Thus, at present, there is a gap in the knowledge about the prevalence, diagnosis and treatment of vitamin D deficiency in adults with hip fractures17. The aim of this study is to assess the distribution and correlates to level of vitamin D in a sample of women and men with recent hip fractures who were part of a large clinical trial. A secondary aim is to determine whether other readily available serum markers of bone metabolism such as serum calcium or alkaline phosphatase are sensitive or specific for identifying vitamin D deficiency in this population, given the cost and difficulties with current vitamin D assays.
Subjects and Methods
Subjects were part of a multinational study, “A randomized placebo-controlled double-blind trial testing the efficacy of a yearly intravenous bisphosphonate, zoledronic acid, in the prevention of new clinical fractures in patients with recent hip fracture repair” 18. Subjects were drawn from 115 clinical centers worldwide in 20 countries. The design and conduct of the study have been described elsewhere [17]. Briefly, at screening or randomization, demographic data, bone mineral density (BMD), Body Mass Index (BMI), and laboratory values for calcium, phosphorous, and creatinine were determined. At randomization, all subjects given loading dose of 100,000 units of vitamin D2 or D3, plus daily dietary supplements of vitamin D and calcium precluding examination of the natural history of the vitamin D, post hip-fracture.
Initially, 25 hydroxyvitamin D levels were measured by a central laboratory in all subjects prior to the receipt of study drug. However, early on in the trial, when the extent of vitamin D deficiency the population became apparent, the protocol was amended such that all subjects were given a loading dose of 100,000 IU vitamin D obviating the need to measure initial vitamin D level. This report includes 1174 screened (526 with vitamin D measured) and 655 randomized (385 with vitamin D measured) subjects randomized before the protocol amendment.
Male and female subject were eligible for inclusion in the study if they were greater than 50 years old, had undergone surgical repair of a hip fracture in the preceding 90 days, were ambulatory (with or without assistive devices), and had intact lower appendages. Subjects were excluded if they (1) preferred use of oral bisphosphonate, (2) had been treated with investigational drug with 30 days, (3) had a history of allergic reaction or hypersensitivity to bisphosphonates, (4) had a history of uvetitis or irititis (except secondary to trauma), (5) had a calculated creatinine clearance ≤ 30 m/min, (6) had a Serum Calcium > 2.75 mmol/L L or < 2.0 mmol/L, (7) had a serum alkaline phosphatase > 2.5 xULN, (8) had primary hyperparathyroidism, hypoparathyroidism, osteogenesis imperfecta, Paget’s disease of bone, or other metabolic bone disease (except osteoporosis), (8) had a diagnosis of cancer within 12 months, (9) had a previous organ transplant, (9) had any Intravenous bisphosphanate within the last 2 years, (10) had prior use of oral bisphosphonate within 2 years (based on length of use), (11) reported use of PTH or sodium fluoride for osteoporosis, or (12) reported prior use of Strontium.
Measures
Blood was obtained on subjects at the time of screening, and sent at ambient temperature to Covance Central Laboratory, Indianapolis, Indiana. Serum 25 hydroxyvitamin D was measured by the Nichols Advantage Assay (Nichols Research Diagnostics). From these same serum samples, calcium, creatinine, alkaline phosphatase, and albumin were measured by autoanalyzer.
At randomization, the following demographic variables were collected on the Clinical Research Form (CRF): gender, age in years, race (white, black, oriental, Hispanic, other), living at home vs. in nursing home. In addition, the following lab values were available: calcium, alkaline phosphatase, calculated creatinine clearance (by the Cockroft-Gault equation), albumin, total hip bone mineral density (BMD), and femoral neck BMD. Albumin was measured on only a subset of subjects (n=62) and therefore was not available for use in all final multivariable models.
The outcome measures were level of serum 25 hydroxyvitamin D level prior to administration of study drug, vitamin D, and calcium supplements. Since we were particularly interested in the rates and correlates of low 25 hydroxyvitamin D, using the definition of Thomas. et al., 6 for moderate and severe hypovitaminosis D, the continuous measure of vitamin D above was dicotomized at <15ng/ml vs ≥ 15ng/ml.
Analysis
Level of 25 hydroxyvitamin D – The bivariate relationship between clinical and demographic variables with 25 hydroxyvitamin D was assessed by Spearman correlation, allowing for the floor value of the assay (7ng/ml) for 25 hydroxyvitamin D. Multivariable parametric procedures were not employed, since many subjects had levels below lower detection threshold of the assay (<7ng/ml), and were coded to the floor value (7ng/ml).
Low 25 hydroxyvitamin D (15ng/ml ) - The bivariate and multivariable relationship between clinical and demographic variables with low vitamin D (<15ng/ml) was assessed by logistic regression in randomized patients.
Results
Across all screened subjects, levels of 25 hydroxyvitamin D were low (median=14.7 ng/mL, IQR=21.65,7.60). Fifty one percent of the subjects were at or below the pre-defined clinically important threshold of 15 ng/mL. The level of 25 hydroxyvitamin D was slightly lower in those who were screen failures (n=100) than in those who were ultimately randomized (n=385) (median 12.95 ng/mL vs. 15.2 ng/mL, p=0.06, by Wilcoxon rank-sum test). Males, on average, had slightly higher levels of 25 hydroxyvitamin D in 385 subjects who were enrolled and randomized, (see figure 1). The median value for males was 16.9 ng/ml and 14.4 ng/ml in females (p=0.013, by Wilcoxon rank-sum test).
Figure 1.
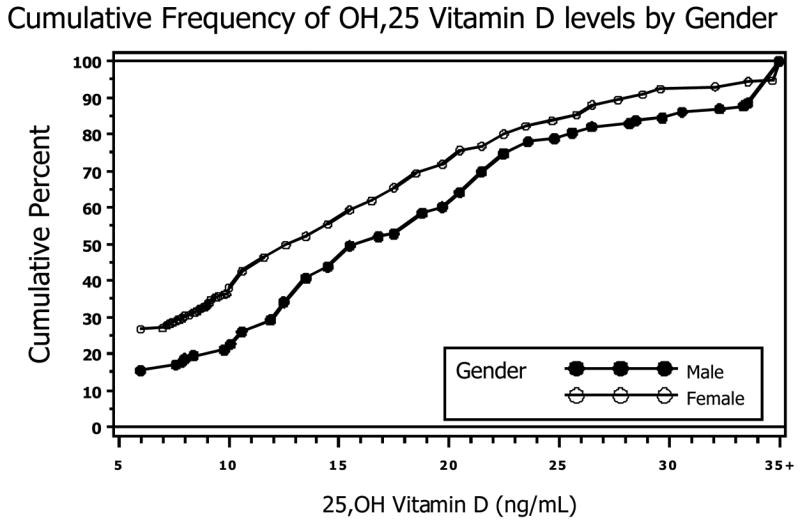
Cumulative Frequency of OH, 25 Vitamin D levels by Gender
Low calcium related to lower levels of vitamin D (spearman rho=0.13, p<0.05), albumin (rho=0.26, p>0.05), and total hip BMD (rho=0.22, p<0.05) ) in bivariate analyses (Table 1). Surprisingly, alkaline phosphatase elevations did not predict vitamin D levels.
Table 1.
Sample descriptive statistics and bivariate correlations with 25, OH vitamin D Level (N=385)
| Variable | Mean | Std Dev | Median (IQR) | Minimum | Maximum | Correlation with Vitamin D Level+ |
|---|---|---|---|---|---|---|
| Male (percent) | 26.2% | 0.13* | ||||
| Age | 77.9 | 7.8 | 80.2(74,85) | 50 | 95 | −0.06 |
| Nonwhite (percent) | 8.9% | −0.02 | ||||
| BMI (kg/m2) | 24.6 | 4.8 | 24.1 (21.3, 27.2) | 14.0 | 49.8 | −0.03 |
| Living at Home (percent) | 88.8% | −0.02 | ||||
| Calcium (mmol/L) | 2.22 | 0.18 | 2.20 (2.0, 2.3) | 1.67 | 2.72 | 0.16** |
| Alkaline Phosphatase (U/L) | 114.9 | 76.2 | 93 (69, 131) | 13,2 | 530 | 0.01 |
| Creatinine Clearance (ml/min) | 58.1 | 23.4 | 51,9 (40.9, 68.0) | 7.25.0 | 173.9 | 0.05 |
| Total hip bone mineral density (g/cm2) | 0.65 | 0.15 | 0.63 (0.58, 0.68) | 0.18 | 1.16 | 0.22** |
| Femoral Neck BMD (g/cm2) | 0.68 | 0.17 | 0.67 (0.55, 0.74) | 0.29 | 1.15 | 0.12 |
| Albumin (g/dL) | 3.3 | 0.59 | 3.3 (2.8, 3.7) | 2 | 4.5 | 0.26 (n=62) |
Spearman Correlation
p<0.05
p<0.01
As shown in table 2, only albumin OR=0.30 (95% CI=0.11, 0.81) and calcium OR=0.16 (95% CI=0.05, 0.52 were predictors of low (<15ng/ml) levels of vitamin D in bivariate analyses. While statistically significant, low calcium was an imperfect proxy for low vitamin D (Area under the Curve=0.60), lacking sufficient sensitivity or specificity to suggest use as a proxy for low vitamin D. In multivariate models, calcium remained significantly related to low 25 hydroxyvitamin D (OR=0.02, 95% CI=0.01 0.12), controlling for race, age, BMI, living place, alkaline phosphatase, femoral neck BMD, and creatinine clearance.
Table 2.
Prediction of Low Vitamin D (<15 ng/mL) (N=385)
| Variable | Bivariate Odds (95% CI) | Multivariable Odds (95% CI) |
|---|---|---|
| Age (per 10 years) | 1.16 (0.94,1.44) | 0.84 (0.53,1.34) |
| Gender (male) | 0.69 (0.44,1.09) | 0.61 (0.30,1.26) |
| Race (non-white) | 1.34 (0.66,2.73) | 0.61 (0.20,1.89) |
| BMI (kg/m2) | 1.01 (0.97,1.06) | 1.07 (0.99,1.15) |
| Living at home | 1.14 (0.60,2.15) | 1.00 (0.34,2.94) |
| Calcium (mmol/L) | 0.16 (0.05,0.52) | 0.02 (0.01,0.12) |
| Alkaline Phosphatase (100 U/L) | 1.06 (0.81,1.38) | 1.87 (1.13,3.08) |
| Creatinine Clearance (10 ml/min) | 0.95 (0.87,1.04) | 1.01 (0.86,1.20) |
| Femoral Neck BMD (g/cm2) | 0.13 (0.02,0.88) | 0.07 (0.01,0.82) |
| Total Hip BMD (g/cm2) | 0.26 (0.03,2.47) | * Not added to full model |
| Albumin (g/dL) (N=62) | 0.30 (0.11,0.81) | * Not added to full model |
Discussion
This study demonstrates that in a large sample of elders with hip fracture, vitamin D levels are remarkably low. This high prevalence of vitamin D deficiency may be the result of low levels of ultraviolet light exposure or insufficient vitamin D dietary intake common in elders.
This study has several limitations. First, it may be that low levels of 25 hydroxyvitamin D are a byproduct of the hip-fracture process. However, as noted by Thomas et al.6, the half life of serum 25-hydoxyvitamin D is 3 weeks, substantially less than the 90 day time period in which most of our subjects were measured after their hip fracture. Second, despite being derived from a multinational sample, the sample analyzed here is a subset of all hip fracture patients who met inclusion and exclusion criteria, and, thus, our results may not generalize to the entire population of hip fracture patients. It is our expectation that those subjects not eligible or not consented were frailer with more comorbidities and, hence, likely to have even lower values of vitamin D. Third, it is possible that the low levels of 25 hydroxyvitamin D that we report in this study were actually higher than the levels reported with the Nichols Advantage 25 hydroxyvitamin D assay. Several studies have shown that commercially available 25 hydroxyvitamin D assays underestimate that amount of 25 hydroxyergocalciferol (25(OH)D2) in serum samples 19, 20. 25(OH)D2 represents vitamin that patients who have received from ergocalciferol (drisdol) or dietary sources. Thus, the 25 hydroxyvitamin D levels (representing both 25(OH)D2 and 25(OH)D3) may have been higher than we report. We were unable to predict how many more samples would have had higher 25(OH)D levels if done by an assay that correctly measures 25(OH)D2 since we did not have additional serum samples on these subjects.
It may be worth speculating that if this finding of low vitamin D is generalized to the larger population with hip fracture, numerous clinical implications may follow. First, low vitamin D may play a role in the high prevalence of hypocalcemia observed in this population. Second, clinicians may find reduced efficacy of bone active medications in the presence of lower vitamin D levels. Third, vitamin D may play a role in reduced muscle strength and, hence, increased falls. All of these factors may contribute to the increased risk of subsequent fractures observed in hip fracture patients (16).
Physicians should be encouraged to either check and follow levels of 25 hydroxyvitamin D or to empirically treat for vitamin D deficiency with a loading dose and daily vitamin D supplements in patients experiencing a low trauma hip fracture. This is especially important prior to initiating bisphosphonate therapy since serious hypocalcemia may result when vitamin D deficiency is left uncorrected21. The parent trial from which these results were derived will provide important information on the potential additional benefits of an active treatment, zoledronic acid, among this patient population, in whom vitamin D deficiency has been corrected.
Acknowledgments
Drs. Pieper, Lyles and Colon-Emeric are supported by the Claude D. Pepper Center grant, 3P60 AG11268-10S1. Dr. Colon-Emeric si supported by a Paul A. Beeson Faculty Scholars awardAward, NIA AG024787-01. Dr. Lyles receives support from the VA Medical Research Service
Footnotes
Author Contributions: Indicate authors’ role in study concept and design, acquisition of subjects and/or data, analysis and interpretation of data, and preparation of manuscript. (List all author(s) name).
| Carl F. Pieper | concept, design, analysis, interpretation, preparation |
| Cathleen Colon-Emeric | concept, design, analysis, interpretation, preparation |
| John Caminis | concept, design, analysis, interpretation, preparation, |
| Kathleen Betchyk | concept, design, |
| Jie Zhang | concept, design, analysis, |
| Cheri Janning | concept, analysis, interpretation, |
| John Shostak | data management analysis, interpretation preparation, |
| Meryl S. LeBoff | concept, design, interpretation |
| Robert Heaney | concept, design, analysis, interpretation, preparation, |
| Kenneth W. Lyles | concept, design, interpretation, preparation, |
CONFLICT OF INTEREST
Financial Disclosure(s): All authors should indicate financial support for research, consultantships, and speakers forum, as well as having any company holdings (e.g., stocks) or patents. (List all author(s) name).
| Author Name: | Carl F. Pieper | None |
| Author Name: | Cathleen Colon-Emeric | None |
| Author Name: | John Caminis | None |
| Author Name: | Kathleen Betchyk | None |
| Author Name: | Jie Zhang | None |
| Author Name: | Cheri Janning | None |
| Author Name: | John Shostak | None |
| Author Name: | Meryl S. LeBoff | None |
| Author Name: | Robert Heaney | None |
| Author Name: | Kenneth W. Lyles | None |
Sponsor’s Role: Indicate sponsor’s role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
The study from which the data reported here were derived were part of a larger industry sponsored (Novartis) clinical trial testing the efficacy of a bisphosonate on hip-fracture. The design, analysis, interpretation and preparation of the results reported here were the responsibility and were determined by the lead author.
References
- 1.Simonelli C, Weiss T, Morancey J, Swanson L, Chen Y-T. Prevalence of vitamin D inadequacy in a minimal trauma fracture population. Current Medical Research and Opinions. 2005;21(7):1069–1074. doi: 10.1185/030079905X50598. [DOI] [PubMed] [Google Scholar]
- 2.Bishcoff-Ferrari H, Dietrich T, Orav EJ, Dawson-Hughes B. Positive association between 25-Hydorxy vitamin D levels and bone mineral density: A population-based study of younger and older adults. American Journal of Medicine. 2004;116:634–639. doi: 10.1016/j.amjmed.2003.12.029. [DOI] [PubMed] [Google Scholar]
- 3.Heany R, Weaver CM. Calcium and Vitamin D. Endocrinology and Metabolism Clinics of North America. 2003;32(1):181–194. doi: 10.1016/s0889-8529(02)00063-4. [DOI] [PubMed] [Google Scholar]
- 4.Semba R, Garrett E, Johnson BA, Guralnik JM, Fried LP. Vitamin D deficiency among older women with and without disability. American Journal of Clinical Nutrition. 2000;72(6):1529–1534. doi: 10.1093/ajcn/72.6.1529. [DOI] [PubMed] [Google Scholar]
- 5.Elliot M, Binkley NC, Carnes M, Zimmerman DR, et al. Fracture risks for women in long-term care: high prevalence of calcaneal osteoporosis and hypovitaminosis. Pharmacotherapy. 2003;23(6):702–710. doi: 10.1592/phco.23.6.702.32182. [DOI] [PubMed] [Google Scholar]
- 6.Thomas M, Lloyd-Jones DM, Thadhanai RI, Shaw AC, Deraska DJ, Kitch BT, Vamvakas ED, DIck IM, Prince RL, FInkelstein JS. Hypovitaminosis D in medical inpatients. New England Journal of Medicine. 1998;3338:777–783. doi: 10.1056/NEJM199803193381201. [DOI] [PubMed] [Google Scholar]
- 7.Bishcoff-Ferrari H, Dawson-Hughes B, Willet WC, Staehelin HB, Basemore MG, Zee RY, Wong JB. Effect of vitamin D on Falls: A meta-analysis. Journal of the American Medical Association. 2004;291(16):1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 8.Michaelsson K, Melhus H, Bellocco R, Wolk A. Dietary calcium and vitamin D intake in relation to osteoporotic fracture risk. Bone. 2003;32(6):694–703. doi: 10.1016/s8756-3282(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 9.Woolf A, Akesson K. Preventing fractures in elderly people. British Medical Journal. 2003;327:89–95. doi: 10.1136/bmj.327.7406.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LeBoff M, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J. Occult vitamin D deficiency in postmenopausal women with acute hip fracture. JAMA. 1999;(281):1505–1511. doi: 10.1001/jama.281.16.1505. [DOI] [PubMed] [Google Scholar]
- 11.Passeri G, Pini G, Troiano L, Vescovini R, Sansoni P, Passeri M, Gueresi P, Delsignore R, Pedrazzoni M, Franceschi C. Low Vitamin D status, high bone turnover, and bone fractures in centenarians. Journal of Clinical Edocrinology and Metabolism. 2003;88:5109–5115. doi: 10.1210/jc.2003-030515. [DOI] [PubMed] [Google Scholar]
- 12.Lilliu H, Pamphile R, Chapuy MC, Schulten J, Arlot M, Meunier PJ. Calcuim-vitamin D3 supplementation is cost-effecti in hip fracture prevention. Maturitas. 2003;44(4):299–305. doi: 10.1016/s0378-5122(03)00038-0. [DOI] [PubMed] [Google Scholar]
- 13.Cooper L, Clifton-Bligh-Clifton PB, Nery ML, Figtree G, Twigg S, Hibbert E, Robinson B. Vitamin D supplementation and bone mineral density in early postmenopausal women. American Journal of Clinical Nutrition. 2003;77(5):1324–1329. doi: 10.1093/ajcn/77.5.1324. [DOI] [PubMed] [Google Scholar]
- 14.Bahl S, Coates PS, Greenspan SL. The Management of osteoporosis following hip fracture: Have we improved our care? Osteoporosis International. 2003;14:884–888. doi: 10.1007/s00198-003-1492-2. [DOI] [PubMed] [Google Scholar]
- 15.surusm ESBJP, Mishaela RR, Black DM, Bockman RS, Bone HG, Hochberg MC, McClung MR, Schnitzer J. Pins and plaster aren’t enough: A call for the evaluation and treatment of patients with osteoporotic fractures. Journal of Clinical Edocrinology and Metabolism. 2003;88(8):3482–3486. doi: 10.1210/jc.2003-030568. [DOI] [PubMed] [Google Scholar]
- 16.Harrington J, Broy SB, Derosa AM, Licata AA, Shewmon DA. Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis & Rheumatism (Arthritis Care & Research) 2002;47:651–654. doi: 10.1002/art.10787. [DOI] [PubMed] [Google Scholar]
- 17.Harrington T, Broy S, Derosa A, Licata A, Shewmon DA. Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis & Rheumatism (Arthritis Care & Research) 2002;47(6):651–654. doi: 10.1002/art.10787. [DOI] [PubMed] [Google Scholar]
- 18.Colon-Emeric C, Caminis J, Suh TT, Pieper CF, Janning C, Magaziner J, Adachi J, Rosario-Jansen T, Messenbrink P, Horowitz ZD, Lyles KW. The HORIZON recurrent fracture trial: Design of a clinical trial in the prevention of subsequent fractures in elders after low trauma hip fracture repair. Current Medical Research and Opinion. 2004;20(6):903–910. doi: 10.1185/030079904125003683. [DOI] [PubMed] [Google Scholar]
- 19.Turpeinen U, Hohenthal U, Stenman UH. Determination of 25-hydroxyvitamin D in serum by HPLC and immunoassay. Clinical Chemistry Sep. 2003;49(9):1521–1524. doi: 10.1373/49.9.1521. [DOI] [PubMed] [Google Scholar]
- 20.Binkley N, Krueger D, Cowgill CS, et al. Assay variation confounds the diagnosis of hypovitaminosis D: a call for standardization. Journal of Clinical Endocrinology & Metabolism. 2004 Jul;89(7):3152–3157. doi: 10.1210/jc.2003-031979. [see comment] [DOI] [PubMed] [Google Scholar]
- 21.Rosen CJ, Brown S. Severe hypocalcemia after intravenous bisphosphonate therapy in occult vitamin D deficiency. New England Journal of Medicine. 2003 Apr 10;348(15):1503–1504. doi: 10.1056/NEJM200304103481521. [DOI] [PubMed] [Google Scholar]


