Abstract
Introduction
Patients with renal insufficiency have an increased risk of atherosclerotic coronary artery disease, cardiovascular events, and sudden cardiac death. Due to under-representation of patients with renal disease in large clinical trials, outcomes of implantable cardioverter defibrillator (ICD) implantation in this group remain unclear.
Methods and Results
Inpatient and ambulatory records were reviewed for 741 consecutive patients undergoing 947 defibrillator implants or replacements at Department of Defense Medical Facilities. Demographics, medical history, and mortality were reviewed. The mean age of the cohort was 64 ± 14 years and 599 (80.8%) were male. There were 173 patients (23.3%) with chronic renal insufficiency, 22 (3.0%) undergoing hemodialysis, and 546 (73.7%) without reported renal disease. The mean number of annual hospital admissions for heart failure among patients with and without renal failure was 3.8 ± 4.0 versus 1.2 ± 1.9 (P < 0.0001), respectively. The 1-year survival for those without renal insufficiency was 96.6%, compared to 87.8% for those with chronic renal insufficiency, and 88.7% for those undergoing hemodialysis. Multivariate analysis demonstrated a significant association between mortality among ICD patients and renal insufficiency, independent of coexisting congestive heart failure, ischemic cardiomyopathy, and diabetes mellitus (P < 0.0001).
Conclusions
Among ICD recipients, those with renal insufficiency have a significantly higher mortality rate than those without renal insufficiency. Among a cohort of patients with ICDs, those with known renal insufficiency have higher rates of health care resource utilization and more heart failure admissions. Development of a national registry for ICDs should include data with regard to renal function.
Keywords: defibrillator, renal failure, dialysis
Introduction
Sudden cardiac death is reported in the U.S. Renal Data System to account for 50–60% of dialysis patient deaths, likely due to increased atherosclerotic burden.1–5 Endothelial dysfunction, ventricular repolarization heterogeneity, volume shifts, and metabolic abnormalities associated with renal insufficiency and dialysis may predispose patients to arrhythmogenesis.3,6,7 Despite progress in the management of cardiovascular disease, mortality following myocardial infarction in patients with end-stage renal disease remains significant, with an unchanged 2-year mortality of over 70% from 1977 to 1999.1–3,8
Patients with advanced renal disease were excluded from all major randomized ICD trials, leaving uncertainty as to the role of ICD therapy in this population.9–12 Both Multicenter Automatic Defibrillator Implantation Trial (MADIT) and MADIT II excluded those with a serum creatinine of > 3.0 mg/dL, and while the Sudden Cardiac Death-Heart Failure Trial (SCD-HeFT)12 was more inclusive of etiology of cardiomyopathy, it was even more restrictive of those with renal impairment, excluding those with a creatinine > 2.5 mg/dL.13 As such, it is uncertain whether patients with renal insufficiency who receive ICDs experience a significant improvement in mortality.14,15 We sought to determine the long-term mortality of patients with renal insufficiency, including those who are dialysis dependent, after implantation of cardiac defibrillators.
Methods
All patients undergoing ICD implantation between October 2000 and September 2004 in Department of Defense medical facilities were included in the study. Inpatient and ambulatory records from all Department of Defense medical treatment facilities were evaluated from the Military Health System Data Repository (MDR), an administrative database. For each inpatient or outpatient medical encounter, up to 20 diagnostic and procedural codes, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), were recorded. Eligible records were identified based on a procedure code (ICD-9-CM, 37.94 through 37.98) indicating ICD placement during the study period.
For each patient, the determination of primary or secondary prevention as the indication for implantation of the defibrillator was identified based on ICD-9 codes from the index hospitalization. Underlying cardiovascular disease and associated risk factors were identified to include percutaneous coronary revascularization, myocardial infarction, cardiomyopathy, congestive heart failure, hypertension, hyperlipidemia, and tobacco use. The presence or absence of chronic renal insufficiency was noted, as was the specific nature of renal pathology. To avoid inclusion of patients with transient causes of renal dysfunction, patients were included only if renal insufficiency was noted on more than one out-patient evaluation prior to implantation of the defibrillator. Admission to hospital for heart failure was identified by the inclusion of ICD-9 codes for heart failure within the first three discharge diagnoses associated with the hospitalization.
Continuous variables are expressed as means ± standard deviation. Student’s t-test was used for comparison of normally distributed continuous variables, and Chi-square test was used for categorical variables. Confidence intervals for the risk ratios were calculated from the formula of Green-land and Robins.16 The method of Kaplan and Meier was used, along with the log-rank test to compare survival among groups.17 The Cox proportional hazards model was used to examine the influence of covariates on survival.18 Significant P-values were < 0.05. Statistical analysis was performed using JMP Professional 5.0.1 (SAS, Cary, NC, USA).
Results
During the study period, a total of 741 patients underwent 947 defibrillator implantations. Over a mean observation period of 4.9 ± 1.4 years, these patients had 4,031 hospitalizations and 80,250 ambulatory medical encounters. The patients were followed for a mean 2.0 ± 1.7 years after index ICD implantation. The mean age of the cohort was 64 ± 14 years and 599 (80.8%) were male (Table 1). Prior to defibrillator implant 195 patients (26.3%) had chronic renal insufficiency, with 22 (2.9%) of these patients requiring hemodialysis. Among the 195 patients with chronic renal insufficiency, one or more pathologies were specified for 102. The most common cause was hypertensive renal disease (49, 25.1%), followed by nephritis (37, 19.0%), and lower nephron nephrosis (12, 6.2%).
TABLE 1.
Demographics and Medical History of 741 Patients Undergoing 947 Defibrillator Implantations During Study Period
| No Chronic Renal Insufficiency n = 546 (73.7%) | Chronic Renal Insufficiency n = 173 (23.3%) | Dialysis Dependent n = 22 (3.0%) | |
|---|---|---|---|
| Age, years† | 62.5 ± 15.6 | 68.0 ± 9.9 | 67.4 ± 8.8 |
| Male | 433 (79.3%) | 147 (85.0%) | 19 (86.4%) |
| Race | |||
| Caucasian | 393 (72.0%) | 126 (72.8%) | 14 (63.6%) |
| African American | 58 (10.6%) | 22 (12.7%) | 3 (13.6%) |
| Hispanic ethnicity‡ | 21 (3.8%) | 11 (6.4%) | 2 (9.1%) |
| Primary prevention | 508 (93.0%) | 164 (94.8%) | 21 (95.5%) |
| Electrophysiology study | 162 (29.7%) | 59 (34.1%) | 4 (18.2%) |
| Syncope | 204 (37.4%) | 80 (46.2%) | 11 (50.0%) |
| Nonsustained VT | 371 (68.0%) | 126 (72.8%) | 16 (72.7%) |
| Ischemic heart disease† | 441 (80.8%) | 161 (93.1%) | 20 (90.9%) |
| Surgical revascularization | 228 (41.8%) | 110 (63.6%) | 15 (68.2%) |
| Percutaneous revascularization | 142 (26.0%) | 56 (32.4%) | 7 (31.8%) |
| Myocardial infarction‡ | 307 (56.3%) | 112 (64.7%) | 17 (77.3%) |
| Congestive heart failure† | 378 (69.2%) | 160 (92.5%) | 19 (86.4%) |
| Diabetes mellitus† | 178 (32.6%) | 111 (64.2%) | 15 (68.2%) |
| Hypertension† | 451 (82.6%) | 167 (96.5%) | 21 (95.5%) |
| Hyperlipidemia† | 412 (75.5%) | 157 (90.8%) | 18 (81.8%) |
| Tobacco abuse | 174 (31.9%) | 65 (37.6%) | 6 (27.3%) |
P < 0.05 for comparison between those with and without chronic renal insufficiency.
P-value <0.05 for trend.
Compared to other patients, those with renal insufficiency were significantly more likely to have ischemic heart disease (92.8% vs. 80.8%, P < 0.0001), congestive heart failure (91.8% vs. 69.2%, P < 0.0001), and surgical coronary revascularization (64.1 vs. 41.8%, P < 0.0001). There was a trend toward more percutaneous coronary interventions (32.3% vs. 26.0%, P = 0.092).
Patients without renal failure had lower all-cause mortality than patients with chronic renal insufficiency. The 1-year survival for those without renal failure was 96.6%, compared to 87.8% with chronic renal insufficiency, and 88.7% for those undergoing hemodialysis. These differences further diverged over the duration of follow-up (up to 5 years) (Fig. 1). Multivariate analysis demonstrated that renal insufficiency was a statistically significant predictor of increased mortality independent of the presence of congestive heart failure, ischemic cardiomyopathy, and diabetes mellitus (Table 2). In those ≥65 years of age, the mean survival of those with renal in-sufficiency was 3.4 years (88.1% survival at 1 year) versus 4.9 years (94.6% survival at 1 year) in those without renal failure (P = 0.007). In those <65 years of age, the mean survival of those with reported renal insufficiency was 3.3 years (87.6% survival at 1 year) versus 4.8 years (99.2% survival at 1 year) in those without renal failure (P < 0.001).
Figure 1.
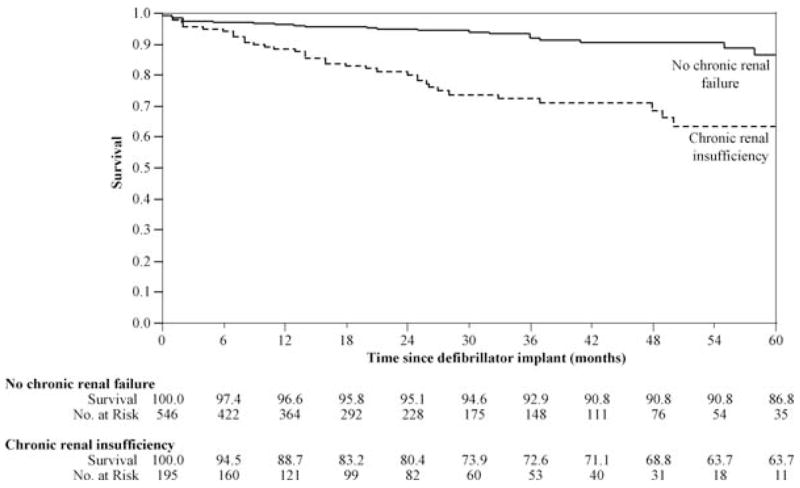
Long-term postdefibrillator implant survival of 741 patients followed for a mean of 4.9 ± 1.3 years (2.0 ± 1.7 years after defibrillator implantation) for 84,281 medical encounters stratified by documentation of renal insufficiency (with and without need for dialysis). Significant differences in mortality noted early after implant with continued separation throughout period of observation (by log-rank test, P < 0.00001).
TABLE 2.
Cox Proportional Fit Model Comparing Significant Risk Factors and Mortality for Patients Undergoing Defibrillator Implantation
| RR (95% CI) | P-value | |
|---|---|---|
| Chronic renal insufficiency | 1.69 (1.32–2.17) | <0.001 |
| Age ≥65 years at implant | 1.31 (1.01–1.74) | 0.043 |
| Ischemic cardiomyopathy | 1.28 (0.79–2.37) | 0.339 |
| Congestive heart failure | 1.25 (0.90–1.40) | 0.147 |
| Diabetes mellitus | 1.10 (0.86–1.41) | 0.437 |
Utilization of resources was evaluated for both hospitalizations and ambulatory visits, excluding those visits specifically for hemodialysis. The median number of outpatient visits per year for those with or without renal insufficiency was 28.5 versus 15.3 (P < 0.0001), respectively. The mean number of hospital admissions for heart failure during the period of observation for those with or without reported renal insufficiency was 3.8 ± 4.0 versus 1.2 ± 1.9 (P < 0.0001), respectively.
Discussion
Despite the exponential number of annual ICD implants and the increasing cost to the health care system, little is known about the prognosis of renal insufficiency patients receiving ICDs. This study demonstrates that ICD patients with renal insufficiency have significantly increased mortality and increased utilization of health care resources compared to patients without renal failure. Although our patients with renal insufficiency had increased risk for mortality by virtue of increased prevalence of diabetes, congestive heart failure, and ischemic cardiomyopathy, regression analysis reveals increased mortality in those with renal insufficiency independent of these comorbidities.
While a recent report suggested that more than 60% of ICD patients in a large, unselected population have at least mild renal insufficiency,19 the benefit of ICD therapy to this group remains unclear. This is, in a large part, due to the fact that renal patients have been under-represented in, and in many cases excluded from, the major randomized ICD trials.9,20,21 The MADIT-II trial, one of the few studies which had reasonable representation of renal patients who made up nearly one-third of the study population, demonstrated that an elevated blood urea nitrogen was associated with increased mortality in both the ICD and the control groups,22 and was associated with increased mortality following a first appropriate ICD therapy.23
MADIT-II reported a benefit of defibrillator therapy independent of renal function.10 It is uncertain, however, how representative MADIT-II renal patients are of all patients with renal insufficiency, as randomized trials are subject to selection bias. Increased overall mortality in the renal impairment group may have important implications for this subset of patients.24 Preliminary analysis of the SCD-HeFT suggests potentially favorable cost-effectiveness with ICD therapy, but this result is based on long-term extrapolations in which ICD patients have an average life expectancy of >10 years25—an assumption that clearly does not apply to most patients with chronic renal failure.
In previous studies, more than 70% of the deaths in ICD patients with mild renal impairment were non-cardiac or nonarrhythmic.26 The U.S. Renal Data System reports 2-, 4-, and 5-year cardiac arrest event rates of approximately 18%, 37%, and 53%, respectively.2,27 These figures correspond to our findings of 2-, 4-, and 5-year all-cause mortality rates of 19%, 31%, and 46%, respectively.
Limitations
Our study is retrospective and drawn from data in an administrative database, susceptible to limitations inherent to all such studies. Some measures which may be relevant to the outcome of interest are unavailable. Specifically, quantification of renal function is not possible. Although our investigation was a retrospective cohort study, confounding factors were addressed by multivariate regression methods. Importantly, this study does not attempt to specifically assess the efficacy of ICD therapy in patients with and without renal insufficiency. Rather, total mortality, an endpoint less subject to bias, is reported. Based on the observation that renal patients have worse overall prognosis, additional data collection to better assess ICD efficacy in this selected population appears warranted. Data collection could take the form of a prospective randomized trial of ICD therapy in this unique group, or could include the modification of the NCDR-ICD Registry database, which has been mandated as a condition of compensation for expanded ICD indications.28
Conclusions
Patients with renal insufficiency who undergo ICD implant have a significantly greater mortality rate and a higher heart failure admission rate than those without renal failure. These findings may have important implications for selection of appropriate patients for ICD implantation and for the cost-effective use of ICDs. Additional study to identify which renal insufficiency patients most benefit from ICD therapy is warranted.
Acknowledgments
The authors would like to thank Terri Amrhein, Patient Administration Systems and Biostatistics Activity, Fort Sam Houston, Texas, for data acquisition.
Dr. Reynolds is the recipient of grant 1 K23 HL077171 from the NHLBI.
Footnotes
Publisher's Disclaimer: Disclaimer: The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Defense, or the U.S. Government. This work is approved for public release; distribution unlimited.
References
- 1.Herzog CA. Poor long-term survival of dialysis patients after acute myocardial infarction: Bad treatment or bad disease? Am J Kidney Dis. 2000;35:1217–1220. doi: 10.1016/s0272-6386(00)70061-8. [DOI] [PubMed] [Google Scholar]
- 2.Herzog CA. Cardiac arrest in dialysis patients: Approaches to alter an abysmal outcome. Kidney Int. 2003;63(Suppl):S197–S200. doi: 10.1046/j.1523-1755.63.s84.17.x. [DOI] [PubMed] [Google Scholar]
- 3.Bleyer AJ, Russell GB, Satko SG. Sudden and cardiac death rates in hemodialysis patients. Kidney Int. 1999;55:1553–1559. doi: 10.1046/j.1523-1755.1999.00391.x. [DOI] [PubMed] [Google Scholar]
- 4.Bleyer AJ, Tell GS, Evans GW, Ettinger WH, Jr, Burkart JM. Survival of patients undergoing renal replacement therapy in one center with special emphasis on racial differences. Am J Kidney Dis. 1996;28:72–81. doi: 10.1016/s0272-6386(96)90133-x. [DOI] [PubMed] [Google Scholar]
- 5.Parfrey PS, Foley RN, Harnett JD, Kent GM, Murray D, Barre PE. Outcome and risk factors of ischemic heart disease in chronic uremia. Kidney Int. 1996;49:1428–1434. doi: 10.1038/ki.1996.201. [DOI] [PubMed] [Google Scholar]
- 6.Miyazaki H, Matsuoka H, Itabe H, Usui M, Ueda S, Okuda S, Imaizumi T. Hemodialysis impairs endothelial function via oxidative stress: Effects of vitamin E-coated dialyzer. Circulation. 2000;101:1002–1006. doi: 10.1161/01.cir.101.9.1002. [DOI] [PubMed] [Google Scholar]
- 7.Morris ST, Galiatsou E, Stewart GA, Rodger RS, Jardine AG. QT dispersion before and after hemodialysis. J Am Soc Nephrol. 1999;10:160–163. doi: 10.1681/ASN.V101160. [DOI] [PubMed] [Google Scholar]
- 8.Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: Results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35:1044–1051. doi: 10.1016/s0272-6386(00)70038-2. [DOI] [PubMed] [Google Scholar]
- 9.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 10.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 11.Moss AJ, Daubert JP, Hall WJ. Multicenter Automatic Defibrillator Implantation Trial (MADIT II): Design and clinical protocol. Ann Non-invasive Electrocardiol. 1999;4:83–91. doi: 10.1111/j.1542-474X.2005.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 13.Bardy GH. The Sudden Cardiac Death-Heart Failure Trial (SCD-HeFT) In: Singh SN, editor. Arrhythmia Treatment and Therapy. New York: Marcel Dekker; 2000. pp. 323–342. [Google Scholar]
- 14.Herzog CA, Li S, Collins AJ. Long-term survival of prevalent dialysis patients after cardiac arrest in the U.S.: The impact of implantable cardioverter-defibrillators. Circulation. 2003;108:IV385–IV386. [Google Scholar]
- 15.Herzog CA. Cardiac arrest in dialysis patients: Taking a small step. Semin Dial. 2004;17:184–185. doi: 10.1111/j.0894-0959.2004.17318.x. [DOI] [PubMed] [Google Scholar]
- 16.Greenland S, Robins JM. Identifiability, exchangeability, and epidemiological confounding. Int J Epidemiol. 1986;15:413–419. doi: 10.1093/ije/15.3.413. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan EL, Meier P. Nonparamatric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 18.Cox DR. The analysis of binary data. London: Methuen; 1970. [Google Scholar]
- 19.Centers for Medicare and Medicaid Services. Decision memo for implantable defibrillators. Medicare coverage database (online) [Accessed December 28, 2004]; http://www.cms.hhs.gov/mcd/viewdecisionmemo.asp?id=139.
- 20.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 21.Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, DeMarco T, Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–2150. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 22.Greenberg H, Case RB, Moss AJ, Brown MW, Carroll ER, Andrews ML. Analysis of mortality events in the Multicenter Automatic Defibrillator Implantation Trial (MADIT-II) J Am Coll Cardiol. 2004;43:1459–1465. doi: 10.1016/j.jacc.2003.11.038. [DOI] [PubMed] [Google Scholar]
- 23.Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, Daubert JP, McNitt S, Andrews ML, Elkin AD. Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation. 2004;110:3760–3765. doi: 10.1161/01.CIR.0000150390.04704.B7. [DOI] [PubMed] [Google Scholar]
- 24.Hlatky MA. Evidence-based use of cardiac procedures and devices. N Engl J Med. 2004;350:2126–2128. doi: 10.1056/NEJMp048071. [DOI] [PubMed] [Google Scholar]
- 25.Mark DB. Cost effectiveness of ICD therapy in the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Paper presented at American Heart Association Scientific Sessions; New Orleans, Louisiana. 2004. [Google Scholar]
- 26.Wase A, Basit A, Nazir R, Jamal A, Shah S, Khan T, Mohiuddin I, White C, Saklayen M, McCullough PA. Impact of chronic kidney disease upon survival among implantable cardioverter-defibrillator recipients. J Interv Card Electrophysiol. 2004;11:199–204. doi: 10.1023/B:JICE.0000048570.43706.34. [DOI] [PubMed] [Google Scholar]
- 27.USRDS 2004 annual data report. Am J Kidney Dis. 2005;45(1 Pt 2):8–280. doi: 10.1053/j.ajkd.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 28.Parkash R, Stevenson WG, Epstein LM, Maisel WH. Predicting early mortality after implantable defibrillator implantation: A clinical risk score for optimal patient selection. Am Heart J. 2006;151:397–403. doi: 10.1016/j.ahj.2005.04.009. [DOI] [PubMed] [Google Scholar]


