Abstract
Because sildenafil citrate is a treatment, not a cure, for erectile dysfunction (ED), many men may choose to use it for an extended period. Men with ED who had previously completed 1 of 4 double-blind trials with short-term open-label extension (combined duration, 0.9–1.2 years) were eligible for this 4-year, open-label, extension study, which assessed the safety and effectiveness of flexible doses (25, 50, and 100 mg sildenafil) used as needed. Adverse events that were serious or led to dosing changes or discontinuation (temporary or permanent) were recorded. Many of the 979 participants (mean age, 58 [range, 27–82] years; mean ED duration, 4.5 years) had concomitant hypertension (28%), diabetes (22%), or hyperlipidemia (14%). Overall, 37 (3.8%) had treatment-related adverse events (none serious) requiring dosage change or discontinuation and 62 (6.3%) discontinued because of insufficient response. At each yearly assessment, more than 94% of participants responded affirmatively to the questions: “Are you satisfied with the effect of treatment on your erections?” and “If yes, has treatment improved your ability to engage in sexual activity?” These results argue against the loss of tolerability or the development of tachyphylaxis over a prolonged period of as needed, flexible-dose sildenafil treatment of men with ED.
Keywords: sildenafil citrate, erectile dysfunction, tolerability, effectiveness
Introduction
In March 1998, the US Food and Drug Administration (FDA) approved sildenafil citrate (Viagra®, Pfizer Inc, New York, NY, USA) for the treatment of erectile dysfunction (ED) (FDA 1998). As of December 2005, more than 27 million men worldwide had received sildenafil for treatment of ED, including an estimated 17 million men in the US (Data on file, Pfizer Inc, New York, NY). Thus, the long-term safety and effectiveness of sildenafil can now be evaluated in men who have been taking the drug for several years.
The efficacy, safety, and tolerability of sildenafil in the treatment of men with ED have been demonstrated in numerous studies of 1-year duration or less. For example, 1,358 men with ED completed 1 of 4 double-blind trials and continued with open-label sildenafil treatment in extension studies for a total treatment duration of approximately 1 year (Morales et al 1998; Steers et al 2001). In the current study, 979 of these men subsequently received up to 4 more years of open-label, flexible-dose (25, 50, and 100 mg) sildenafil. Preliminary (3-year) results were reported previously (Carson et al 2002; Padma-Nathan et al 2002), and we now present the final data. The population included patients with ED of organic and psychogenic etiology and typical concomitant medical conditions for this population (ie, hypertension, diabetes, hyperlipidemia, and a history of ischemic heart disease). Our objective was to assess the long-term safety and effectiveness of sildenafil treatment in men with ED.
Methods
This was a 4-year, open-label, flexible-dose (25, 50, and 100 mg) study of sildenafil. Men who previously completed and were compliant with sildenafil or placebo treatment in 1 of 4 double-blind, placebo-controlled trials, and subsequently completed and were compliant with sildenafil treatment in initial open-label extension, were eligible for inclusion in this long-term extension study. Study medication was provided at no cost. Compliance was assessed by medication diaries and by continued study participation.
A total of 1,545 men were originally enrolled in the double-blind trials, with 1,358 of these men continuing in the initial open-label extension studies. The current study includes 979 of the original patients, who agreed to participate in the long-term extension (Figure 1). The procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional).
Figure 1.
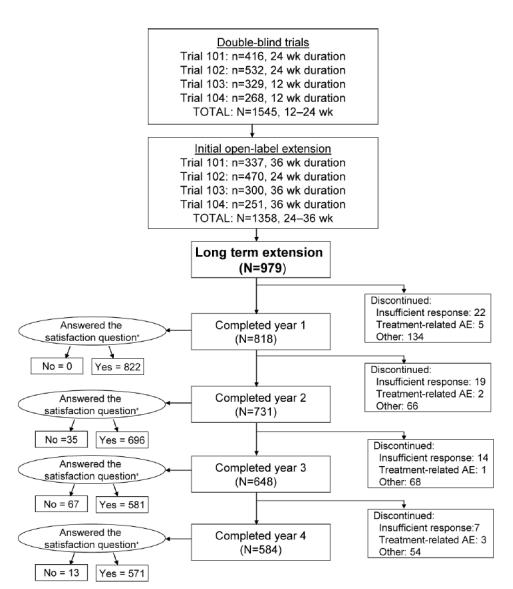
Number of patients and treatment duration in the original double-blind trials and the initial open-label extensions and disposition throughout 4 years of open-label, flexible-dose (25, 50, and 100 mg) sildenafil long-term extension study. Of the 979 participants who entered the sildenafil long-term extension study, 584 (60%) completed all 4 years. Reasons for discontinuation, other than insufficient clinical response and treatment-related adverse event (AE), included AE unrelated to treatment, protocol violation, loss to follow-up, and other (eg, loss of interest in participation in a clinical study, loss of sexual partner, and ability to afford sildenafil after approval [thus, no longer needing to participate in a clinical study to obtain the medication]). N for the satisfaction question (“Are you satisfied with the effect of treatment on your erections?”) is equal to the number of men who answered. *Some of the discontinued subjects supplied satisfaction data.
At the time the study started, the FDA stated that there were sufficient routine safety data on sildenafil to make collection of standard adverse event data unnecessary. Therefore, only serious adverse events and adverse events leading to changes in dosing or to temporary or permanent discontinuation were recorded and evaluated by the investigators for relatedness to sildenafil treatment.
Because the major focus of this study was safety, and it was designed before the development and validation of patient-reported outcomes to assess satisfaction with the quality of erection (eg, Quality of Erection Questionnaire (Porst et al 2007)) or satisfaction with ED treatment (eg, the Erectile Dysfunction Inventory of Treatment Satisfaction (Althof et al 1999)), effectiveness was assessed by asking, at yearly intervals or at discontinuation, simple, unvalidated general efficacy questions, “Are you satisfied with the effect of treatment on your erections?” and “If yes, has treatment improved your ability to engage in sexual activity?” The second question was based on the ED definition of the National Institutes of Health Consensus Conference: “…inability to attain and/or maintain penile erection sufficient for satisfactory sexual performance.” (NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence 1993). Descriptive statistics were calculated.
Results
Overall, 979 men initially agreed to participate in the study, most of whom were white (89%) and whose mean age was 58 years (Table 1). The duration of the double-blind trials plus initial open-label extension was 0.9 to 1.2 years (48–60 weeks). Median duration of participation in the open-label, long-term extension study was 4 years, the median number of doses taken was 420 (range, 1–1469) (Figure 2), and the preferred dose was 100 mg in more than 88% of the men. The retention rate was 84% (818/979) the first year, 75% (731/979) the second year, and 66% (648/979) the third year; the entire 4-year extension study was completed by 584 of the initial 979 men (60%) (Figure 1). Reasons for discontinuation included loss of interest in participation in a clinical study, loss of sexual partner, loss to follow-up, ability to afford sildenafil after approval (thus, no longer needing to participate in a clinical study to obtain the medication), insufficient clinical response, and adverse events.
Table 1.
Baseline characteristics of the 979 men
| Age, mean (range) years | 58.2 (27–82) |
| Weight, mean (range) kg | 89.2 (53.5–158.8) |
| Race, n (%) | |
| White | 873 (89.2) |
| Black | 68 (6.9) |
| Asian | 8 (0.8) |
| Other | 30 (3.1) |
| ED duration, mean (range) years | 4.5 (0.1–35.8) |
| ED etiology, % organic/mixed/psychogenic | 72/17/11 |
| Common concomitant medical conditions, n (%) | |
| Hypertension | 272 (27.8) |
| Diabetes mellitus | 213 (21.8) |
| Hyperlipidemia | 139 (14.2) |
| History of ischemic heart disease | 83 (8.5) |
Figure 2.
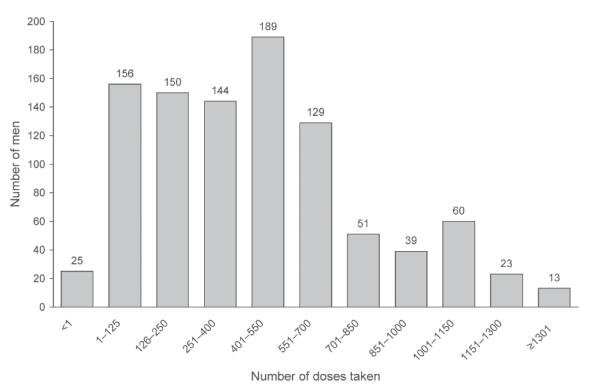
Usage of flexible-dose (25, 50, and 100 mg) sildenafil over 2–1561 days by the 979 participants who entered the study.
Tolerability
Over the 4-year study period, 37 (3.8%) of the men had 1 or more adverse events that led to changes in dosing or to temporary or permanent discontinuation and were determined by the investigators to be treatment-related (Table 2). Of the 47 events, headache and dyspepsia were most common (n = 10 each), followed by rhinitis (n = 6), flushing (n = 5), abnormal vision (n = 4), dizziness (n = 3), and 1 report each of mild palpitations, moderate tachycardia, diarrhea, nausea, myalgia, hypertonia, respiratory disorder, conjunctivitis, and photophobia. Of the few cardiovascular events determined by the investigator to be treatment related (4 cases of mild flushing and 1 each of moderate flushing, mild palpitations, and moderate tachycardia), only 1 led to permanent discontinuation. In this case the man experienced mild flushing with the first dose of sildenafil 100 mg but continued therapy after a dose reduction. After 629 days of therapy, at which time his dosage was once again 100 mg, he permanently discontinued sildenafil because of the flushing. Two other cardiovascular events led to temporary discontinuation (mild flushing and moderate tachycardia), and the remainder were addressed with a change in dosing. Of the 149 serious adverse events that occurred during the 4 years of the study, including 18 acute myocardial infarctions, none were considered by the investigator to be treatment related.
Table 2.
Adverse events that led to changes in dosing or to temporary or permanent discontinuation
| Adverse events (AEs) in 979 men | ||
|---|---|---|
| Treatment-relateda | All causality | |
| Patients with AEs, n (%) | 37 (3.8) | 210 (21.5) |
| Discontinued because of AEs, n (%) | 11 (1.1) | 55 (5.6) |
| Most frequent (≥0.5%) AEs, n (%) | ||
| Headache | 10 (1.0) | 10 (1.0) |
| Dyspepsia | 10 (1.0) | 12 (1.2) |
| Rhinitis | 6 (0.6) | 6 (0.6) |
| Flushing | 5 (0.5) | 5 (0.5) |
| Coronary artery disorder | 0 | 24 (2.5) |
| Prostatic disorder | 0 | 16 (1.6) |
| Carcinoma | 0 | 14 (1.4) |
| Myocardial infarction | 0 | 11 (1.1)b |
| Arthritis | 0 | 9 (0.9) |
| Bone fracture accidental | 0 | 9 (0.9) |
| Accidental injury | 0 | 7 (0.7) |
| Cerebrovascular disorder | 0 | 7 (0.7) |
| Atrial fibrillation | 0 | 6 (0.6) |
| Cholecystitis | 0 | 6 (0.6) |
| Sepsis | 0 | 5 (0.5) |
| Heart failure | 0 | 5 (0.5) |
| Gastrointestinal carcinoma | 0 | 5 (0.5) |
| Bone disorder | 0 | 5 (0.5) |
Other treatment-related AEs were abnormal vision (n = 4), dizziness (n = 3), and 1 report each of mild palpitations, moderate tachycardia, diarrhea, nausea, myalgia, hypertonia, respiratory disorder, conjunctivitis, and photophobia.
Because serious adverse events are collected for a longer period (30 days after the completion of treatment) than adverse events in general, numbers of events may vary between these 2 databases.
Each treatment year, less than 1% of the men who started the year discontinued sildenafil because of treatment-related adverse events, for a total of only 11 (1.1%) of the original 979 participants over the 4 years of the study (Table 3). Discontinuations were caused by dyspepsia (n = 4), rhinitis (n = 2), abnormal vision plus headache (n = 1), dyspepsia plus rhinitis (n = 1), and flushing, dizziness, and myalgia (n = 1 each).
Table 3.
Discontinuations over 4 years
| Percentage of participants who discontinued, (n/N)a | |||
|---|---|---|---|
| Study year | Treatment-related adverse event | Insufficient response | Other reasons (not treatment related) |
| 1 | 0.5 (5/979) | 2.2 (22/979) | 13.7 (134/979) |
| 2 | 0.2 (2/818) | 2.3 (19/818) | 8.1 (66/818) |
| 3 | 0.1 (1/731) | 1.9 (14/731) | 9.3 (68/731) |
| 4 | 0.5 (3/648) | 1.1 (7/648) | 8.3 (54/648) |
N = the number of men who began the study year.
Effectiveness
Of the 979 men who participated in the study, 932 (95%) were analyzed for efficacy. At the completion of each year, at least 94% of the annually decreasing number of participants reported satisfaction with the effect of sildenafil treatment on their erections, with only a 3.3 percentage point variation across the 4 yearly assessments (Table 4). Almost all of these men reported improved ability to engage in sexual activity.
Table 4.
Sildenafil treatment outcome over 4 years
| Percentage of participants (n/N)a | ||
|---|---|---|
| Study year | Satisfied with treatment effect on erections | Improved ability to have sexual activity |
| End of year | End of year | |
| 1 | 98.1 (806/822) | 99.6 (803/806) |
| 2 | 96.6 (672/696) | 99.9 (671/672) |
| 3 | 94.8 (551/581) | 99.6 (549/551) |
| 4 | 96.3 (550/571) | 100 (550/550) |
For the satisfaction analyses, N is equal to the number of men who answered the satisfaction question. For the respective sexual activity analyses, N is equal to the number of men who answered the satisfaction question affirmatively and answered the sexual activity question.
Each treatment year, less than 3% of the men who started the year discontinued sildenafil treatment because of insufficient clinical response. Over the 4 years of the study, only 62 (6.3%) of the original 979 participants discontinued because of insufficient response (Table 3).
Discussion
There are numerous data published on the efficacy and safety of sildenafil treatment for ED. Before approval, sildenafil was evaluated in 18 phase II/III double-blind, placebo-controlled trials, in which men with ED were randomized to receive treatment with sildenafil (n = 2722) or placebo (n = 1552) for up to 6 months (Morales et al 1998). Pooled data from these trials demonstrated that sildenafil is a well-tolerated oral therapy for ED (Morales et al 1998). Adverse events were mostly transient and mild to moderate in severity and included most commonly headache, flushing, dyspepsia, and rhinitis. The rate of discontinuation because of adverse events was low and comparable between patients who received sildenafil and those who received placebo. A more recent retrospective analysis, in which data were pooled from 35 Pfizer-sponsored double-blind trials involving 4819 patients who received sildenafil and 3296 patients who received placebo, supports the conclusions of the earlier pooled data but also found that sildenafil is well tolerated among patients taking antihypertensive medications, including those on multidrug regimens (Padma-Nathan et al 2002). Pooled data also support the efficacy of sildenafil; results from 11 double-blind, flexible-dose, placebo-controlled trials that included a total of 2,667 men ages 23 to 89 years with ED of broad-spectrum etiology show significantly improved erectile function for sildenafil compared with placebo as measured by the International Index of Erectile Function, a global efficacy question, and a patient-recorded event log of sexual activity (Carson et al 2002).
The population of the current 4-year open-label study of sildenafil differed from those of the pooled double-blind studies in that it was self-selected. Consequently, it is likely that men with poor tolerability or inadequate effectiveness did not opt to participate and that the population included mostly men who had previously experienced a good response to sildenafil. Also, men who could afford to purchase sildenafil may have lost incentive to participate in the long-term study when sildenafil became commercially available. This phenomenon necessitated discontinuation of a European long-term OL study when sildenafil became commercially availabile in Europe (Padma-Nathan et al 2001). Another limitation was the use of unvalidated general efficacy questions, explained by the fact that the major focus of the study was safety and by the absence at the time of the study design of appropriate validated questionnaires to assess satisfaction with ED treatment. Regardless, the results add to the previously published reports by showing continued safety and effectiveness during prolonged treatment. During 4 years of open-label, flexible-dose administration, there were few discontinuations because of either intolerable adverse events or insufficient clinical response. The majority of men were satisfied with sildenafil treatment for their ED and reported improved ability to engage in sexual activity. Throughout the 4-year study period, the consistently low incidence of adverse events of sufficient severity to negatively impact treatment argues against the loss of tolerability with time, and the low rate of discontinuation because of insufficient clinical response (<3% per year) argues against the development of tachyphylaxis. The broad usage range (1–1469 doses over 4 years) demonstrates the “real world” experience provided by the study.
Despite a preferred sildenafil dose of 100 mg (the highest recommended dose) in more than 88% of the men, treatment-related cardiovascular adverse events necessitating changes in dosing or temporary or permanent discontinuation were limited to one case each of mild palpitations and tachycardia and 5 cases of flushing. There were no treatment-related acute myocardial infarctions or other serious adverse events. Only 1.1% of participants discontinued treatment over 4 years because of treatment-related adverse events, which were most frequently dyspepsia, rhinitis, and headache. In comparison, treatment-related adverse events were responsible for discontinuation by 1.2% of men treated with sildenafil 100 mg in 6-month, double-blind, placebo-controlled trials (Morales et al 1998) and by 2% of 1008 men enrolled in 36-week or 52-week, open-label extension studies (Steers et al 2001). Adverse events were responsible for similarly low rates of discontinuation in clinical practice studies of varying duration conducted worldwide; in California 2.7% of 74 men discontinued (Marks et al 1999), in Brazil none of 256 men discontinued (Moreira et al 2000), and in China none of 1,290 men discontinued (Jiann et al 2003). Among 22,471 men treated with sildenafil in general practice in the UK, headache was the most frequently reported treatment-related adverse event and was cited as the reason for discontinuation in 0.3% of men (Boshier et al 2004).
The satisfaction with the effectiveness of sildenafil for the treatment of ED that was reported in the current study confirms previous results. In one multicenter, open-label study, 176 men with ED completed the validated Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) questionnaire after long-term successful intracavernosal prostaglandin E1 and again 12 weeks after switching to flexible-dose oral sildenafil (25, 50, and 100 mg) (Montorsi et al 2003). Sildenafil treatment was associated with significantly greater overall treatment satisfaction, ease of use, and intention to continue treatment. Moreover, partners were more satisfied with sildenafil overall, and their responses correlated with the satisfaction of the patients. Other well-controlled studies using EDITS have shown similarly high degrees of satisfaction with sildenafil (Eardley et al 2004; Lewis et al 2001).
Conclusions
In this 4-year, open-label study, there was a low incidence of adverse events that resulted in dosage change or discontinuation, and most continuing participants were satisfied with sildenafil treatment for their ED. These data are consistent with previous reports and argue against loss of tolerability or development of tachyphylaxis.
Acknowledgments
The study was sponsored by Pfizer Inc. Editorial support was provided by Deborah Campoli-Richards, RPh, at Complete Healthcare Communications, Inc., and was funded by Pfizer Inc.
Appendix
The other members of the multicenter study group (all in the US) are Jeffrey Apter, Stratford, NJ; Gilberto Brito, Phoenix, AZ; Arthur L. Burnett, Baltimore, MD; Ronald Castellanos, Fort Myers, FL; Jeoffrey Deeths, Omaha, NE; Francois Eid, New York, NY; William Fitch III, San Antonio, TX; Thomas Garland, Lawrenceville, NJ; Marc Gittelman, Aventura, FL; Donald Gleason, Tucson, AZ; Irwin Goldstein, Boston, MA; Frederick Govier, Seattle, WA; Joel M. Kaufman, Aurora, CO; Ira Klimberg, Ocala, FL; Dean Knoll, Nashville, TN; Vincent Longo, New London, CT; Tom F. Lue, San Francisco, CA; Terrence Malloy, Philadelphia, PA; Leonard Marks, Culver City, CA; Andrew McCullough, New York, NY; David F. Mobley, Houston, TX; William Moseley, San Diego, CA; Myron Murdock, Greenbelt, MD; Dana Ohl, Ann Arbor, MI; Michael O’Leary, Boston, MA; Harin Padma-Nathan, Beverly Hills, CA; Jacob Rajfer, Torrance, CA; James Regan, Washington, DC; Marc S. Rendell, Omaha, NE; Henry Ritter, Atherton, CA; Raymond Rosen, Piscataway, NJ; Ridwan Shabsigh, New York City, NY; Stephen Sharp, Nashville, TN; William Steers, Charlottesville, VA; Christopher Steidle, Fort Wayne, IN; Jacques Susset, Providence, RI; John Tuttle, Lexington, KY; Lamar Weems, Jackson, MS; Glenn Wells, Birmingham, AL; Charles White, Mobile, AL; Jay Young, Laguna Woods, CA; Norman Zinner, Torrance, CA.
Disclosures
The research reported was sponsored and supported by Pfizer Inc. The authors actively participated in the collection of data and interpretation of the results. Although the sponsor held the data, all authors had full access. The writing, review, and final approval of the manuscript were performed by a committee of 7 persons, including 4 representatives from the research and development departments of Pfizer Inc. Editorial support was provided by Deborah Campoli-Richards, RPh, at Complete Healthcare Communications, Inc, and was funded by Pfizer Inc.
James McMurray, Robert Feldman, and Stephen Auerbach are study investigators for Pfizer Inc. James McMurray has no relevant financial interest in the manuscript (ie, honoraria, stock ownership or options, expert testimony, grants received or pending, patents, royalties, or other). Robert Feldman has consulted on drug development for Pfizer Inc in the past, received honoraria for lectures, and owns Pfizer Inc stock. He has no other relevant financial interest in the manuscript (ie, expert testimony, grants received or pending, patents, royalties, or other). Stephen Auerbach has participated on advisory boards and received honoraria for lectures for Pfizer Inc, Eli Lilly and Company, GSK and Schering-Plough Corporation, Threshold Pharmaceuticals, and Indevus Pharmaceuticals. He has received grants and/or has grants pending from the above companies, Watson Pharmaceuticals, and PPD (Pharmaceutical Product Development). Herb deRiesthal is an employee of Pfizer Inc, and Neal Wilson is a former employee of Pfizer Inc.
References
- Althof SE, Corty EW, Levine SB, et al. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology. 1999;53:793–9. doi: 10.1016/s0090-4295(98)00582-2. [DOI] [PubMed] [Google Scholar]
- Boshier A, Wilton LV, Shakir SA. Evaluation of the safety of sildenafil for male erectile dysfunction: experience gained in general practice use in England in 1999. BJU Int. 2004;93:796–801. doi: 10.1111/j.1464-410X.2003.04744.x. [DOI] [PubMed] [Google Scholar]
- Carson CC, Burnett AL, Levine LA, et al. The efficacy of sildenafil citrate (Viagra®) in clinical populations: an update. Urology. 2002;60(Suppl 2B):12–27. doi: 10.1016/s0090-4295(02)01687-4. [DOI] [PubMed] [Google Scholar]
- Eardley I, Wright P, MacDonagh R, et al. An open-label, randomized, flexible-dose, crossover study to assess the comparative efficacy and safety of sildenafil citrate and apomorphine hydrochloride in men with erectile dysfunction. BJU Int. 2004;93:1271–5. doi: 10.1111/j.1464-410X.2004.04816.x. [DOI] [PubMed] [Google Scholar]
- FDA. FDA Approves Impotence Pill, VIAGRA [online] 1998 Accessed February 27, 2004. http://www.fda.gov/bbs/topics/ANSWERS/ANS00857.html. [PubMed]
- Jiann BP, Yu CC, Tsai JY, et al. What to learn about sildenafil in the treatment of erectile dysfunction from 3-year clinical experience. Int J Impot Res. 2003;15:412–7. doi: 10.1038/sj.ijir.3901047. [DOI] [PubMed] [Google Scholar]
- Lewis R, Bennett CJ, Borkon WD, et al. Patient and partner satisfaction with VIAGRA (sildenafil citrate) treatment as determined by the erectile dysfunction inventory of treatment satisfaction questionnaire. Urology. 2001;57:960–5. doi: 10.1016/s0090-4295(01)00945-1. [DOI] [PubMed] [Google Scholar]
- Marks LS, Duda C, Dorey FJ, et al. Treatment of erectile dysfunction with sildenafil. Urology. 1999;53:19–24. doi: 10.1016/s0090-4295(98)00525-1. [DOI] [PubMed] [Google Scholar]
- Montorsi F, Althof S, Sweeney M, et al. Treatment satisfaction in patients with erectile dysfunction switching from prostaglandin E1 intracavernosal injection therapy to oral sildenafil citrate. Int J Impot Res. 2003;15:444–9. doi: 10.1038/sj.ijir.3901049. [DOI] [PubMed] [Google Scholar]
- Morales A, Gingell C, Collins M, et al. Clinical safety of oral sildenafil citrate (VIAGRA) in the treatment of erectile dysfunction. Int J Impot Res. 1998;10:69–74. doi: 10.1038/sj.ijir.3900354. [DOI] [PubMed] [Google Scholar]
- Moreira SG, Brannigan RE, Spitz A, et al. Side-effect profile of sildenafil citrate (Viagra) in clinical practice. Urology. 2000;56:474–6. doi: 10.1016/s0090-4295(00)00649-x. [DOI] [PubMed] [Google Scholar]
- NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- Padma-Nathan H, Eardley I, Kloner RA, et al. A 4-year update on the safety of sildenafil citrate (Viagra®) Urology. 2002;60:67–90. doi: 10.1016/s0090-4295(02)01752-1. [DOI] [PubMed] [Google Scholar]
- Padma-Nathan H, Eardley I, Maytom M. Long-term efficacy of Viagra (sildenafil citrate): results after 2 3 years of treatment. Int J Impot Res. 2001;(Suppl 1):S21. [Google Scholar]
- Porst H, Gilbert C, Collins S, et al. Development and validation of the Quality of Erection Questionnaire. J Sex Med. 2007;4:372–81. doi: 10.1111/j.1743-6109.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- Steers W, Guay AT, Leriche A, et al. Assessment of the efficacy and safety of Viagra (sildenafil citrate) in men with erectile dysfunction during long-term treatment. Int J Impot Res. 2001;13:261–7. doi: 10.1038/sj.ijir.3900714. [DOI] [PubMed] [Google Scholar]


