Abstract
Background
Guidelines for the management of adults with hospital-acquired (HAP), ventilator-associated (VAP), and healthcare-associated (HCAP) pneumonia were recently updated. These evidence-based guidelines emphasize early, appropriate antimicrobials, as well as, de-escalation of initial therapy based upon microbiologic cultures and clinical response of the patient, and to shorten duration of therapy to a minimum effective period.
Objective
To evaluate adherence to the nosocomial pneumonia guidelines before and after a multifaceted educational intervention in conjunction with the implementation of an adult pneumonia order set.
Methods
A three phase, retrospective, observational analysis was performed among patients with nosocomial pneumonia in a tertiary care facility. The phases consisted of an analysis of medical charts to identify empiric antimicrobial therapy for patients with nosocomial pneumonia; education of physicians on the guidelines; and repeat review of medical charts of patients with nosocomial pneumonia to observe for guideline adherence. An adult pneumonia order set was introduced to the medical staff prior to the initiation of the observational analysis and provided a modality for prescribers to be most compliant with the current recommendations for treating pneumonia. Order set utilization was tracked throughout the observational analysis to determine if various educational interventions increased compliance.
Results
Thirty-three patients were evaluated pre-education: 5 transferred, 16 discharged, and 12 died. Thirty-one patients were evaluated post-education: 6 transferred, 21 discharged, and 4 died. The combined sixty-seven patients received two hundred forty-eight orders for forty-four unique antimicrobial agents from five different services. Appropriateness of antimicrobial prescribing, designated by adherence to the clinical practice guidelines, did not improve following an educational intervention. However, the adult pneumonia order set was utilized in forty-eight percent of the post-education group while only being implemented in nine percent of the pre-education group. The prescribing of single or additional antimicrobials, while utilizing the adult pneumonia order set, commonly resulted in overall noncompliance with the consensus guidelines.
Conclusion
This analysis showed that educational efforts alone were not effective in improving the appropriateness of prescribing empiric antimicrobial therapy in accordance with the guidelines. Prescribing compliance with pre-printed orders, in addition to periodic interactive educational interventions, should be addressed when introducing and maintaining adherence to new clinical practice guidelines.
Keywords: nosocomial pneumonia, clinical practice guidelines, educational intervention, pneumonia order set
Background
Hospital-acquired pneumonia (HAP) is defined as pneumonia that occurs at least forty-eight hours after hospital admission and the designation of ventilator-associated pneumonia (VAP) is given to those patients that develop pneumonia greater than 48–72 hours after endotracheal intubation. HAP is the second most common nosocomial infection in the United States and Europe, and extends total hospital length of stay by seven to nine days on average (Richards et al 1999; Klavs et al 2003; Lizioli et al 2003). Approximately 1% of hospitalized patients are affected by HAP and this infectious process increases total healthcare costs by more than forty thousand dollars. The majority of studies associated with patients diagnosed with HAP incorporate critically ill or ventilated patients and report a mortality rate of between 30% and 70% (Valles et al 2003; Leroy et al 2004). Although, a recent multicenter study of non-intensive care patients with HAP demonstrated a substantially lower mortality rate at 26% (Sopena and Sabria 2005).
Because of the significant impact of this disease on the healthcare system, a joint committee of members of the Infectious Disease Society of America (IDSA) and the American Thoracic Society (ATS) published updated guidelines for the diagnosis and management of nosocomial pneumonia in February 2005 (Niederman and Craven 2005). In these guidelines, not only did the committee acknowledge the importance of HAP and VAP, but they also introduced a new category of pneumonia, healthcare-associated (HCAP). HCAP, which is represented by hospitalization for greater than 2-days within the past 90-days; residence in a long-term care facility; recent intravenous antibiotic therapy, chemotherapy, or wound care within the past 30-days of the current infection; and recent dialysis treatment (clinic or hospital); was created due to the recognition that patients in this category are at an increased risk of acquiring multi-drug resistant (MDR) pathogens. The purpose of developing this evidence-based guideline was to ensure a consensus among how patients with nosocomial pneumonia are treated, thereby optimizing disease state management and antimicrobial therapy with the goal of decreasing morbidity and mortality associated with this infectious process.
Appropriate antimicrobials, in adequate doses, along with the consideration of pharmacodynamic profiles of the agents utilized, is essential to combat the high rate of morbidity and mortality associated with HAP (Kollef et al 1999; Hoffken and Niederman 2002). Although initial broad-spectrum antibiotic coverage is encouraged, it is recommended to discontinue unnecessary antimicrobial agents when organisms are identified, in order to minimize the risk of developing multi-drug resistant pathogens and patient adverse events (Kollef et al 1999; Neiderman and Craven 2005). While the guidelines offer many treatment options, the regimens differ based upon the time of onset of pneumonia and risk factors for MDR pathogens. Therefore, the objectives of this analysis was to evaluate adherence with recommended empiric antimicrobial selection for patients at risk for MDR pathogen associated HAP, VAP, or HCAP before and after educational interventions and to determine if the implementation of an adult pneumonia order set lead to more improved prescribing in accordance with the consensus guidelines.
Methods
This was an Institutional Review Board-approved three phase, retrospective, observational analysis conducted over 9-months at an 881-bed tertiary care facility. The first three months included observation of prescriber adherence to the treatment guidelines prior to an education initiative. Next, spanning over the course of three months was an educational endeavor that consisted of three informal discussions and five formal presentations by local opinion leaders. Audit and feedback of recent adherence to clinical practice guidelines was performed with forty physicians, who are significant antibiotic prescribers, on two separate occasions. Also, two symposiums and one round table discussion were held to educate on the most recently updated pneumonia guidelines. Each educational activity was well received with the most positive feedback received by interacting with opinion leaders who clearly outlined the importance of adhering to consensus guidelines addressing the treatment of pneumonia. There was a combined total of sixty logged hours among the authors dedicated to the above listed activities. The majority of this time was spent directly educating prescribers on their individual prescribing habits and how they may improve in order to achieve adherence with current recommendations.
Subsequent to these educational endeavors were three months used to evaluate changes in prescribing habits and improvement in appropriateness of prescribing antimicrobials for the treatment of nosocomial pneumonia. Data were obtained from physician progress notes, medication administration records, patient flow sheets, computer-based laboratory and report systems, and a database of adverse drug events. Patients were identified for observation via review of daily laboratory results for positive sputum or bronchoalveolar lavage (BAL) cultures. In order to be included in the analysis, the following inclusion criteria were applied: adolescent or adult; clinical diagnosis of HAP, VAP, and HCAP; chest radiography; physician documentation of pneumonia; positive culture results (sputum or BAL). Data collected included: gender and age; prescribing physician; specific antimicrobials utilized, dose, route, and dosing frequency; renal adjustment of antimicrobials performed; sputum and BAL culture results; length of intensive care and total hospital stay; pneumonia onset (<5 days or >5 days); discharge disposition (discharged, death, or transfer); risk factors for MDR pathogens causing HAP,VAP, or HCAP; delineation of empiric or definitive therapy; antimicrobial(s) prescribed at discharge; infectious disease consult obtained. The primary point of interest was adherence with recommended empiric antimicrobial selection for patients at risk for MDR pathogen associated HAP, VAP, or HCAP before and after educational interventions. Also evaluated was the utilization of the adult pneumonia order set which was introduced before the observational analysis. It was determined whether patients in the analysis were treated per the order set. Data was compiled in Microsoft Access™ and descriptive statistical testing was performed using Minitab (Minitab Inc 1998).
Results
Thirty-three patients, with an average length of hospital stay of 17.2-days (8.2-days in the ICU), were evaluated pre-education: 5 transferred, 16 discharged, and 12 died. Thirty-one patients, with an average length of stay of 15.4-days (6.9-days in the ICU), were evaluated post-education: 6 transferred, 21 discharged, and 4 died. The combined sixty-seven patients received two hundred forty-eight orders for forty-four unique antimicrobial agents from five different services. Suboptimal empiric therapy was prescribed at approximately the same frequency regardless of early or late onset of pneumonia (Table 1). Figure 1 illustrates the frequency of pneumonia treatment by service. The infectious disease service was consulted on only 13% of the study patients. The most common organisms cultured from sputum or BAL are shown in Table 2. The most common reasons for suboptimal adherence to the clinical practice guidelines pre- and post-education were the use of monotherapy and inadequate Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus (MRSA) coverage. These two multi-drug resistant pathogens accounted for the majority of cultured organisms during the analysis which is delineated in Table 2. Overall, the percent of patients prescribed guideline recommended empiric regimens in the post-education phase did not differ from the percent receiving recommended empiric regimens in the pre-education phase. The adult pneumonia order set was better received following the educational intervention than before considering that it was utilized in forty-eight percent of the post-education group while only being implemented in nine percent of the pre-education group. However, despite the utilization of the order set, prescribers often wrote orders for additional antimicrobials leading to decreased guideline compliance. The infectious disease service did not use the pre-printed adult pneumonia orders yet the internal medicine and pulmonary services implemented the pre-orders periodically on their patients. Compliance with the consensus guidelines was well correlated with those services utilizing the order set while refraining from ordering only one antimicrobial or an alternate, non-recommended, agent.
Table 1.
Demographics with pre- and post-education results
| Pre-education | Post-education | |
|---|---|---|
| Men, n | 23 | 15 |
| Women, n | 10 | 16 |
| Age, mean (range) | 58 (11–91) | 56 (14–90) |
| Onset | ||
| Early, n | 14 | 22 |
| Late, n | 19 | 9 |
| Early-onset appropriate therapy | ||
| Yes, n (%) | 2/9 (22%) | 4/16 (25%) |
| No, n (%) | 7/9 (78%) | 12/16 (75%) |
| Late-onset appropriate therapy | ||
| Yes, n (%) | 4/17 (24%) | 1/6 (17%) |
| No, n (%) | 13/17 76%) | 5/6 (83%) |
| Overall appropriateness | ||
| Yes, n (%) | 6/26 (23%) | 5/22 (23%) |
| No, n (%) | 20/26(77%) | 17/22 (77%) |
Figure 1.
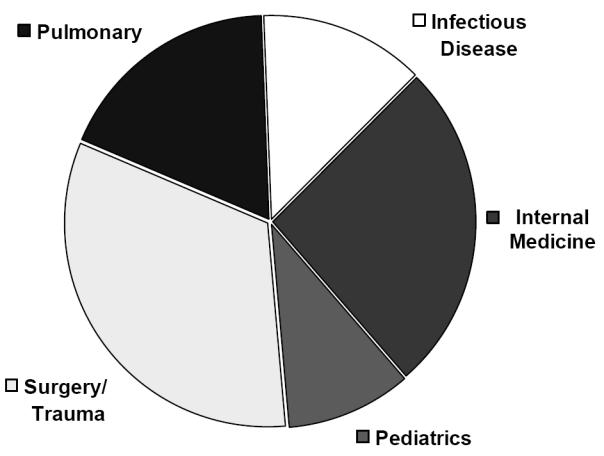
Prescribing service.
Table 2.
Pathogens cultured from sputum or bronchoalveolar lavage
| Gram-positive pathogens | Gram-negative pathogens | ||
|---|---|---|---|
| MRSA | 14 | P. aeruginosa | 15 |
| S. pneumoniae | 6 | S. maltophilia | 10 |
| MSSA | 3 | H. influenzae | 5 |
| S. epidermidis | 3 | K. pneumoniae | 4 |
| E. faecium | 3 | Serratia | 4 |
| E. faecalis | 2 | E. coli | 3 |
| S. pyogenes | 1 | E. aerogenes | 3 |
| Streptococcus | 1 | E. cloacae | 2 |
| Staphylococcus | 1 | K. oxytoca | 1 |
| Enterobacter | 1 | ||
| C. koseri | 1 | ||
| Acinetobacter | 1 | ||
| P. mirabilis | 1 | ||
| B. cepacia | 1 | ||
Discussion
An outcome analysis with this focus provides the opportunity to develop a pragmatic approach to addressing prescribing habits among patients at risk for or with bacterial infections with multi-drug resistant organisms within the healthcare organization. This analysis allowed for a two prong approach toward improving adherence with clinical practice guidelines. First, it served as an educational endeavor with an emphasis on educating all healthcare disciplines within the organization on the most recently published nosocomial pneumonia guidelines, while including an audit and feedback project. Secondly, it provided a foundation for the implementation of adult pneumonia orders, Figure 2, which can be used to guide appropriate prescribing for nosocomial pneumonia. Enhanced adherence to clinical practice guidelines for the treatment of nosocomial pneumonia will promote a standard of practice that limit future trends of bacterial resistance and improve patient care and outcomes.
Figure 2.
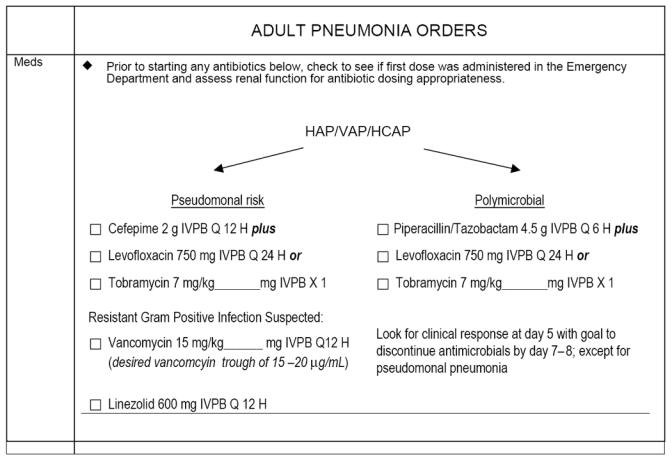
Example of an adult pneumonia order set compliant with clinical practice guidelines.
When new clinical practice guidelines are published, it is essential to introduce effective strategies to ensure guideline adherence. Clinical practice guideline adherence should be considered a safety initiative and a quality improvement project within healthcare organizations because when used inappropriately, or not at all, important healthcare outcomes may be compromised (Cook et al 2004). A sole educational endeavor, serving as the behavior change strategy, has been shown to most often be unsuccessful. However, when behavior change strategies are approached in a multifaceted manner and address documented barriers in the local environment, their success rate is greatly improved (Thomson et al 2000; Cook et al 2004). An overview of systemic reviews of interventions was published by The Cochrane Effective Practice and Organization of Care Review summarizing the importance of utilizing multiple implementation strategies to translate research findings into practice (Grimshaw et al 2001). This summary focused on primary literature that dealt with the varying effectiveness of both simple and complex behavior change strategies and their effects on clinician behavior and patient outcomes (Cabana et al 1999; Grimshaw et al 2001). It was determined that preprinted orders and periodic interactive educational interventions were most beneficial when introducing and maintaining behavioral change and that mail outs and conferences were the least beneficial. These literature findings support the premise that it is essential to not only educate yet to also provide a guide for prescribers to follow (ie, pre-printed orders) in order to improve antimicrobial selection in accordance with the most recently published guidelines.
This three phase, retrospective, observational analysis, conducted for the purpose of increasing prescriber adherence with nosocomial pneumonia clinical practice guidelines, would best be defined as a behavior change strategy know as the audit and feedback of recent performance strategy (Thomson et al 2000). This strategy has proven to be insufficient as a stand alone modality by which to effectively implement quality improvement initiatives. However, when coupled with reminders and prompts such as pre-printed orders or computer decision support systems, it may be considered the backbone for successful initiatives (Garg et al 2005). Various adjuncts may be considered to aid in behavior change such as formal presentations by local opinion leaders and informal or roundtable discussion groups. Determining the best behavior change strategies to implement for each project depends not only on the effectiveness of the strategy, as published in the literature, but also on its past success with previous projects within the organization in which it is being implemented. It is critical that when embarking upon behavior change strategies, within a healthcare setting, that a multi-disciplinary approach be taken. Incorporating the input from the medical staff and nursing staff is essential and will help aid in the success of guideline adherence. Guidance, direction, and support should be solicited from both the Chief Medical Officer and Chief Nursing Officer for the purpose of solidifying the changes in prescribing habits. This type of support, with regard to changing antimicrobial prescribing, is best achieved when first reviewed and recommended directly by each of the following committees: Anti-Infective Subcommittee, Pharmacy and Therapeutics Committee, and the Medical Executive Committee. Also, various factors such as suitability, practicality, and cost must be considered when embarking on a quality improvement program that will depend on effective and well implemented behavior change strategies (Cabana et al 1999; Garg et al 2005).
Conclusion
HAP, VAP, and HCAP are serious pulmonary infectious processes associated with significant morbidity/mortality and increased healthcare expenditures and resource consumption. Early and appropriate empiric antimicrobial therapy is imperative in order to optimize patient outcomes. This analysis showed that educational interventions consisting of informal discussions and formal presentations by local opinion leaders, audit and feedback of recent adherence to clinical practice guidelines, symposiums, and round table discussions were only moderately effective in improving the appropriateness of prescribing empiric antimicrobial therapy in accordance with the guidelines. However, the utilization of a broader, multifaceted, pragmatic approach incorporating behavioral change strategies that involve absolute adherence to pre-printed orders in addition to engaging and site specific educational endeavors may serve as the key to success.
Conflict of interest
The authors have no other similar works under review or in press. Furthermore, the authors have no conflicts of interest, no funding, royalties, honoraria, grants, stocks, or other financial or material gain associated with the writing of this manuscript.
References
- Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- Cook DJ, Montori VM, McMullin JP, et al. Improving patients’ safety locally: changing clinician behaviour. Lancet. 2004;363:1224–30. doi: 10.1016/S0140-6736(04)15955-2. [DOI] [PubMed] [Google Scholar]
- Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: A systematic review. JAMA. 2005;293:1223–38. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. MedCare. 2001;39:II2–45. [PubMed] [Google Scholar]
- Hoffken G, Niederman MS. Nosocomial pneumonia: the importance of a de-escalating strategy for antibiotic treatment of pneumonia in the ICU. Chest. 2002;122:2183–96. doi: 10.1378/chest.122.6.2183. [DOI] [PubMed] [Google Scholar]
- Klavs I, Bufon Luznik T, Skerl M, et al. Prevalance of and risk factors for hospital-acquired infections in Slovenia-results of the first national survey, 2001. J Hosp Infect. 2003;54:149–57. doi: 10.1016/s0195-6701(03)00112-9. [DOI] [PubMed] [Google Scholar]
- Kollef MH, Sherman G, Ward S, et al. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest. 1999;115:462–74. doi: 10.1378/chest.115.2.462. [DOI] [PubMed] [Google Scholar]
- Leroy O, Meybeck A, d’Escrivan T, et al. Hospital-acquired pneumonia in critically ill patients: mortality risk stratification upon onset. Treat Respir Med. 2004;3:123–31. doi: 10.2165/00151829-200403020-00006. [DOI] [PubMed] [Google Scholar]
- Lizioli A, Privitera G, Alliata E, et al. Prevalence of nosocomial infections in Italy: result from the Lombardy survey in 2000. J Hosp Infec. 2003;54:141–8. doi: 10.1016/s0195-6701(03)00078-1. [DOI] [PubMed] [Google Scholar]
- Niederman MS, Craven DE. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- Richards MJ, Edwards JR, Culver DH, et al. Nosocomial infections in medical intensive care units in the United States. National Nosocomial Infections Surveillance System. Crit Care Med. 1999;27:887–92. doi: 10.1097/00003246-199905000-00020. [DOI] [PubMed] [Google Scholar]
- Sopena N, Sabria M. Multicenter study of hospital-acquired pneumonia in non-ICU patients. Chest. 2005;127:213–19. doi: 10.1378/chest.127.1.213. [DOI] [PubMed] [Google Scholar]
- Thomson O’Brien MA, Oxman AD, Davis DA, et al. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000:CD000259. doi: 10.1002/14651858.CD000259. [DOI] [PubMed] [Google Scholar]
- Valles J, Mesalles E, Mariscal D, et al. A 7-year study of severe hospital-acquired pneumonia requiring ICU admission. Intensive Care Med. 2003;29:1981–8. doi: 10.1007/s00134-003-2008-4. [DOI] [PubMed] [Google Scholar]


