Abstract
Background and objectives: Hemodialysis is associated with hemodynamic instability, acute cardiac ischemia, and the development of regional wall motion abnormalities (RWMAs). This study used serial intradialytic H215O positron emission tomography scanning to confirm that the development of dialysis-induced RWMAs was associated with reduction in myocardial blood flow (MBF).
Design, setting, participants, & measurements: Four prevalent hemodialysis patients without angiographically significant coronary artery disease had measurements of MBF during standard hemodialysis and biofeedback dialysis. All patients underwent serial measurements of MBF using positron emission tomography. Concurrent echocardiography was used to assess left ventricular function and the development of RWMAs. Hemodynamic variables were measured using continuous pulse wave analysis.
Results: Mean prehemodialysis MBF was within the normal range. Global MBF was acutely reduced during hemodialysis. Segmental MBF was reduced to a significantly greater extent in areas that developed RWMAs compared with those that did not. Not all regions with reduced MBF were functionally affected, but a reduction in myocardial blood flow of >30% from baseline was significantly associated with the development of RWMAs. No significant differences in hemodynamic tolerability, RWMA development, or MBF between dialysis modalities were observed.
Conclusions: Hemodialysis is associated with repetitive myocardial ischemia, which, in the absence of coronary artery disease, may be due to coronary microvascular dysfunction. Stress-induced segmental left ventricular dysfunction correlates with matched reduction in MBF. Functional poststress recovery is consistent with myocardial stunning induced by hemodialysis. This process may be important in the development of heart failure in long-term hemodialysis patients.
Dialysis patients display hugely elevated rates of cardiac mortality (1), and it is becoming appreciated that this rate of cardiovascular attrition is not driven by the same variety of risk factors or pathophysiologic processes that are important in the general population (2). Classical complicated atherosclerotic disease seems not to be the predominant mode of death in hemodialysis (HD) patients. Cardiac failure develops in as many as 25 to 50% of HD patients and confers a dramatic reduction in probability of survival (3). In addition, a significant percentage of cardiac mortality is due to sudden death (4), which seems to be temporarily related to the dialysis procedure (5).
Myocardial ischemia may be precipitated by HD; a variety studies have confirmed dialysis-induced myocardial ischemia (6). Short intermittent HD treatments exert significant hemodynamic effects, and 20 to 30% of treatments are complicated by intradialytic hypotension (7,8). In conjunction with this, HD patients are particularly susceptible to myocardial ischemia. In addition to the high prevalence of coronary artery atheroma (9), diabetic dialysis patients have been shown to have a reduced coronary flow reserve (CFR) in the absence of coronary vessel stenoses (10). CFR determines the ability to increase blood flow to the myocardium during increased demand, and there is preliminary evidence that the same reduction of CFR is also seen in dialysis patients without diabetes (11). HD patients characteristically also exhibit left ventricular (LV) hypertrophy, reduced peripheral arterial compliance, impaired microcirculation (12), and ineffective vasoregulation (in response to HD with ultrafiltration). All of these factors also predispose to demand ischemia.
In patients with coronary artery disease (CAD) but without chronic kidney disease, transient myocardial ischemia may lead to LV dysfunction that can persist after the return of normal perfusion. This prolonged dysfunction is known as myocardial stunning (13). Myocardial stunning has been demonstrated in humans after exercise and dobutamine stress in patients with CAD (14,15). Repetitive episodes of ischemia can be cumulative and lead to prolonged LV dysfunction. Myocardial stunning is thought to be a causative mechanism for heart failure, with stunning and hibernation existing as part of a single spectrum (16–18).
We previously demonstrated that conventional HD is capable of inducing segmental ventricular regional wall motion abnormalities (RWMA), which resolve after dialysis. These findings are consistent with stress-induced ischemia. Use of modified dialysis procedures (biofeedback control or cooled dialysate) that reduce the level of dialysis-induced relative hypotension result in an abrogation of this cardiac injury (19,20). We hypothesized that the observed reductions in segmental contractile function are a result of ischemia. Furthermore, the repeated nature of this insult (thrice weekly) may be important in the development of dialysis-associated heart failure.
Positron emission tomography (PET) is an imaging technique that offers unrivalled specificity and sensitivity and represents the gold standard for the study of tissue perfusion, including myocardial blood flow (MBF). Using H215O (which has a short half-life) as the radiolabeled tracer allows repetitive MBF measurements at short intervals. Also, because it is metabolically inert, it equilibrates rapidly between the vascular and extravascular spaces, meaning that uptake by the heart does not vary despite wide variations in flow rate (21), and is particularly well suited to resolving segmental differences in perfusion even in morphologically abnormal myocardium. The aim of this study was to evaluate the acute effects of both standard and modified (biofeedback-controlled) dialysis on global and segmental MBF, using intradialytic H215O PET scanning as the most accurate dynamic measure of myocardial perfusion.
Concise Methods
Patients
Four patients who were on long-term HD were recruited for a randomized crossover study. Coronary angiograms had been performed as part of routine clinical care (e.g., for workup for transplantation), and none of the patients needed clinical intervention. Angiographic results and remaining characteristics are shown in Table 1. All patients underwent dialysis via native arteriovenous fistulas, and all were anuric. Patients were excluded when they had significant symptomatic cardiac failure (NYHA ≥3) or experienced an acute coronary syndrome in the preceding 4 mo or had previously received a cardiac transplant or when it was not possible to obtain echocardiographic images of sufficient quality to allow meaningful analysis.
Table 1.
Patient demographics including angiographic indications and findingsa
| Patient | Age (yr) | Months on Dialysis | Cause of ESRF | Smoker | Angiogram Indication | Angiogram Result | Antianginal or BP-Lowering Drugs |
|---|---|---|---|---|---|---|---|
| 1 | 54 | 17 | Diabetes | Yes | Chest pain | Normal | None |
| 2 | 63 | 68 | APKD | No | Assessment for transplantation (equivocal ETT) | Moderate Cx disease (50%); normal RCA, LMS, and LAD. | None |
| 3 | 56 | 46 | Diabetes | No | Assessment for transplantation (equivocal ETT) | Mild LAD disease | Lisinopril 5 mg OD, nifedipine 30 mg OD, doxazosin 2 mg OD |
| 4 | 64 | 44 | Diabetes | Yes | Assessment for transplantation (unable to perform ETT) | Trivial coronary disease | Atenolol 25 mg OD, ISMN 60 mg OD |
| Mean ± SD or n (%) | 59 ± 5 | 44 ± 21 | 2 (50) | 4 (100) |
APKD, adult polycystic kidney disease; Cx, circumflex artery; ESRF, end-stage renal failure; ETT, exercise tolerance test; IHD, ischemic heart disease; LAD, left anterior descending artery; LMS, left main stem; OD, once daily; RCA, right coronary artery; ISMN, isosorbide mononitrate.
Study Protocol
On entry to the study, patients' dry weight and antihypertensive medications remained unchanged for the duration. Patients were then randomly assigned to two groups. Group A patients were commenced on standard thrice-weekly HD; group B patients started thrice-weekly dialysis with the Hemocontrol biofeedback system (BFD). Patients but not dialysis unit staff were blinded to the intervention. Both groups underwent 2 wk of the dialysis therapy after which patients attended their initial monitored dialysis session. β-Blocking agents and calcium antagonists were withdrawn 72 h before the study (because they are known to protect against myocardial stunning), and other antianginal medication were omitted on the day of the study. Patients were asked to avoid activities that might precipitate their angina for 12 h before the study and were excluded when they had experienced angina or used their glyceryl trinitrate spray within 4 h of commencement. After the conclusion of the first study, patients then crossed over to the other dialysis modality, thereby acting as their own control subjects. After 2 wk on the alternate modality, patients underwent a second monitored session on the same day of the week as the first study session.
For each monitored dialysis treatment, MBF was measured before dialysis, during treatment, at 2 and 4 h, and again 30 min into the recovery using H215O PET scanning. Serial echocardiography was performed at the same time points. Noninvasive hemodynamic monitoring of BP and heart rate was undertaken using a Finometer. For obtain baseline values, monitoring was started 30 min before commencement of dialysis. Predialysis blood tests were drawn immediately after insertion of access needles; after dialysis, levels were taken from the arterial line 10 s after reduction of blood pump speed to 50 ml/min. Single-pool Kt/Vurea values were calculated from before and after urea levels (22). The primary end point was the frequency of new LV RWMA during HD in relation to global and regional MBF. All patients gave informed consent before commencement, and ethical approval for the project was granted by Derbyshire Local Research Ethics Committee.
PET
Regional Myocardial Perfusion.
The PET scans were performed in a three-dimensional imaging mode with a 962 (HR+) scanner (Siemens, Knoxville, TN). The scanner enables the acquisition of 15 planes of data over a 10.5-cm axial field of view, allowing the whole heart to be imaged. All emission and transmission data were reconstructed with a Hanning filter. Patients were asked to abstain from caffeine-containing beverages for 24 h before the scan. Patients were positioned in the scanner while still on HD, and a 5-min rectilinear transmission scan was acquired to determine the optimal imaging position of the left ventricle. A 20-min transmission scan was subsequently performed for the purpose of attenuation correction of all emission scans. Patient position was kept constant throughout using a low-power laser beam superimposed on a cross-shaped ink mark on the patient's chest. Starting after a 30-s background frame, a bolus of oxygen-15–labeled water H215O (185 MBq) was injected intravenously through an intravenous cannula in the opposite arm to the arteriovenous fistula over 20 s at an infusion rate of 10 ml/min. The venous line was then flushed for another 2 min. The following scanning protocol was used: 1 × 30 s (background); 1 × 20 s; 14 × 5 s; 3 × 10 s; 4 × 20 s, and 4 × 30 s for a total scanning time of 350 s. All subsequent boluses of labeled water were given through the intravenous cannula; dialysis access was not used.
PET Data Analysis.
The acquired sinograms were corrected for attenuation and reconstructed on a Microvax II computer (Digital Equipment, Marlboro, MA). Images were then transferred to a Sun Sparc 2 workstation (Sun Microsystems, Mountainview, CA) and analyzed with customized MATLAB software (The Math-works Natick, MA). Myocardial images, for the definition of regions of interest (ROI), were generated directly from the dynamic H215O, as previously reported (23). Factor images describing tissue and blood distributions were generated by iterative reconstruction as described previously (24,25). Factor images were resliced into short-axis images in an orientation perpendicular to the long axis of the left ventricle. Sixteen ROI, corresponding to the territories of distribution of the three major coronary arteries, were drawn within the LV myocardium on 10 consecutive image planes, according to the recommendations of the American Society of Echocardiography (26). For our analysis, the original 16 LV ROI were regrouped into 10 segments to correspond with echocardiographic analysis (see next section). Myocardial and blood time activity curves were then generated from the dynamic image and fitted to a single-tissue compartment tracer kinetic model to give values of MBF (ml/min per g) (24). As well as absolute values, we corrected resting MBF for the rate-pressure product (RPP), an index of myocardial oxygen consumption: MBF = (MBF/RPP) × 104 (27,28).
Echocardiography
Two-dimensional echocardiography was performed in conjunction with perfusion scans at baseline and on HD at 120 and 240 min and at 30 min after dialysis had finished (recovery; 1.5 to 3.6 MHz 3S probe; Vivid 3; GE Medical Systems, Sonigen, Germany). Standard apical two-chamber and four-chamber views (to visualize the LV endocardial border in two planes at 90° to each other) were recorded for off-line digital analysis with Echo-CMS (MEDIS, Leiden, Netherlands) as described previously (29). Each apical view was divided into five segments, and percentage shortening fraction (SF) for the chords in each segment was averaged so that 10 regions of the left ventricle were assessed at each time point. New RWMA were defined as segments that demonstrated a decline in SF of >20% from baseline. When comparing dialysis modalities, the same time point was used in the second dialysis session.
Finometer
The use of the Finometer (Finapres Medical Systems, Arnhem, Netherlands) in dialysis patients has been described in detail elsewhere (20) and was used to monitor beat-to-beat heart rate and BP. Heart rate is represented as percentage change from baseline; however, BP is calibrated against brachial readings using a return-to-flow method, so absolute values are shown.
HD Details
Dialysis was performed using a Hospal Integra monitor (Hospal, Lyon, France). Both HD and BFD were performed using low-flux polysulphone dialyzers as per individual patients' usual prescription (LOPS 18/20; Braun Medical Ltd., Sheffield, UK) for 4 h. For both treatments, dialysate contained sodium 138 mmol/L, potassium 1 mmol/L, calcium 1.25 mmol/L, magnesium 5 mmol/L, bicarbonate 32 mmol/L, glucose 1 g/L, and acetate 3 mmol/L. All treatments were of 4 h duration, and anticoagulation was achieved with unfractionated heparin. Dialysate flow was 500 ml/min, and dialysate temperature was set at 37°C. For standard HD, dialysate sodium conductivity was set at 13.6 ms/cm. For BFD, limits for relative blood volume were set on an individual basis depending on measurements taken during the week before echocardiographic assessment. The prescribed input was total weight loss and final relative blood volume. Feedback was via ultrafiltration rate and dialysate conductivity for which limits were set at 13.0 and 14.0 ms/cm. For each session, net fluid removal was set on an individual basis according to ideal dry weight. Blood pump speed varied between 250 and 450 ml/min depending on patients' vascular access, but each individual patient had the same blood flow for his or her two monitored sessions. All patients underwent dialysis using arteriovenous fistulas.
Statistical Analyses
Results are expressed as mean ± SD if parametric or as median (interquartile range) if nonparametric, unless otherwise stated. Echocardiographic, BP, and hemodynamic data were analyzed using one-way ANOVA with a design for repeated measures and Bonferroni test to correct for multiple comparisons. For other data, either the paired t test or Wilcoxon rank sum test was used depending on normality of the distribution. An α error at P < 0.05 was judged to be significant.
Results
Echocardiographic Data
Throughout the study, all patients were in sinus rhythm, and none had significant valvular disease or pulmonary hypertension. At 2 and 4 h, a total of 39 RWMA developed during both types of dialysis. There was no significant difference in the number of RWMA that developed between 2 and 4 h. At 30 min after dialysis (recovery period) compared with 4 h, 81% of RWMA had improved and 23% had regained normal function, confirming the presence of myocardial stunning in this group. There was no significant difference in either the number of RWMA or their severity in terms of SF between HD and BFD during dialysis or after the recovery period (P > 0.05 by ANOVA).
PET Data
All results were corrected for RPP; however, no significant difference was observed between corrected and noncorrected values at given time points. Previous studies have shown reduced baroreflex sensitivity and heart rate variability in this group (30); results shown are therefore noncorrected unless otherwise stated.
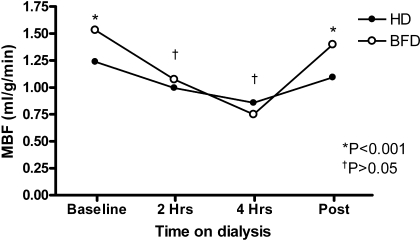
Global, mean predialysis MBF for both modalities was within the normal range. Global MBF was acutely reduced during dialysis and became progressively worse over time. There was some restoration of flow (but not complete) after the 30-min recovery period (see Figure 1).
Figure 1.
Mean global myocardial blood flow (MBF) reduced significantly during dialysis from baseline with partial restoration in the recovery period.
Segmental MBF was reduced in 67 and 90% of regions at 2 and at 4 h, respectively. Three of the four patients had universal (100%) involvement with reduction of MBF in all segments during both dialysis modalities.
Between dialysis modalities (HD and BFD), baseline MBF was compared on an individual basis for each. There were no significant differences in three of the four patients (P > 0.05); however, one patient showed a significant improvement in resting MBF after the 2 wk of BFD. There were also no significant differences in MBF between dialysis modalities at 2 or 4 h, although when observing individual patients, one had a significant improvement in MBF at 4 h during BFD (P < 0.001) without any significant difference in MBF at baseline.
After the recovery period, there was an improvement in MBF in 85% of segments demonstrating partial but not complete restoration of blood flow after 30 min. There was a greater overall restoration of MBF after BFD compared with HD (P < 0.001; Figure 2).
Figure 2.
Mean MBF during hemodialysis (HD) and biofeedback dialysis (BFD). No significant benefit was seen between dialysis modalities during treatment (†P > 0.05); however, there was an improvement in MBF in the recovery period after BFD (*P < 0.001).
The development of RWMA demonstrated by echocardiography was significantly associated with a greater percentage reduction in MBF (−30 ± 27.7 versus −12.3 ± 12.3%; P = 0.001; Figure 3). Not all regions with reduced MBF were functionally affected; however, a reduction in MBF ≥30% from baseline (mean reduction of MBF in all regions 29%) was significantly associated with the development of RWMA (P < 0.01). Also, in areas where reduction in MBF was <30%, there was actually a mean overall increase in percentage wall motion (Figure 4).
Figure 3.
The development of regional ventricular dysfunction as measured by regional wall motion abnormalities (RWMA; abnormal regions) was associated with a greater reduction in MBF from baseline than areas that maintained normal movement (normal regions; P = 0.001).
Figure 4.
An MBF reduction of ≥30% was associated with a mean reduction in wall motion of −15.2%; however, an MBF reduction of <30% was associated with a mean increase in wall motion of 5% (P < 0.01).
Hemodynamic Data
Hemodynamic data are summarized in Figure 5. Mean systolic BP was maintained slightly higher during BFD (127 ± 10 mmHg) than HD (124 ± 12 mmHg; P < 0.05). There were no significant differences between diastolic BP and mean arterial pressure between HD and BFD. None of the patients had episodes of symptomatic or asymptomatic intradialytic hypotension. Heart rate increased throughout both modalities to a similar degree, with means of 6 ± 2% during HD and 6 ± 3% during BFD (NS).
Figure 5.
(A) Overall mean BP between HD and BFD. BP was maintained higher on BFD (P < 0.05). (B) Heart rate increased similarly during both HD and BFD.
Laboratory Data
There were no differences in any of the biochemical parameters when the two types of dialysis were compared. Cardiac troponin-I levels were similar between the two modalities and did not change significantly after dialysis. Three of the four patients had normal cardiac troponin-I levels of <0.032 (Table 2).
Table 2.
Biochemical dataa
| Parameter | HD
|
BFD
|
||
|---|---|---|---|---|
| Before Dialysis | After Dialysis | Before Dialysis | After Dialysis | |
| Hemoglobin (g/dl) | 12.10 (10.70 to 13.40) | 12.50 (11.00 to 14.60) | 11.90 (11.30 to 13.60) | 12.90 (11.30 to 13.10) |
| Hematocrit | 0.36 (0.33 to 0.44) | 0.37 (0.34 to 0.43) | 0.37 (0.35 to 0.4) | 0.38 (0.35 to 0.40) |
| Na+ (mmol/L) | 137.00 (135.00 to 149.00) | 137.50 (136.00 to 138.00) | 137.00 (136.00 to 138.00) | 137.00 (135.00 to 138.00) |
| Corr. Ca2+ (mmol/L) | 2.32 (2.22 to 2.39) | 2.28 (2.15 to 2.35) | 2.46 (2.36 to 2.46) | 2.33 (2.33 to 2.33) |
| Phosphate (mmol/L) | 1.75 (1.49 to 2.05) | 0.89 (0.77 to 0.99) | 1.93 (1.49 to 3.10) | 1.05 (0.77 to 1.13) |
| Albumin (g/L) | 32.00 (31.00 to 33.50) | 36.50 (35.00 to 39.00) | 32.00 (32.00 to 33.00) | 34.00 (33.00 to 36.00) |
| CRP (mg/L) | 7.50 (3.00 to 12.00) | 7.50 (2.00 to 13.00) | 4.00 (3.00 to 9.00) | 5.00 (4.00 to 10.00) |
| cTnI (μ g/L)b | <0.032 (<0.032 to 0.050) | <0.032 (<0.032 to 0.460) | <0.032 (<0.032 to 0.410) | <0.032 (<0.032 to 0.400) |
| Kt/Vurea | 1.32 (1.30 to 1.42) | 1.44 (1.42 to 1.52) | ||
Data are median (interquartile range). There were no significant differences between hemodialysis (HD) and biofeedback dialysis (BFD) for any parameters, including Kt/Vurea. CRP, C-reactive protein; cTnI, cardiac troponin-I; Corr. Ca2+, corrected calcium.
Lowest value quoted <0.032 (normal).
Discussion
This study demonstrates for the first time that HD is associated with significant reductions in MBF and that HD stress–induced myocardial ischemia results in the development of RWMA. Furthermore, dialysis-induced myocardial stunning occurs in the absence of large-vessel epicardial coronary disease.
All of the patients in all of the HD treatments studied developed RWMA during HD. Both the pattern of abnormalities and the subsequent partial resolution after dialysis are in keeping with previous reports. We reported this phenomenon in two previous studies (19,20). In an additional cross-sectional study of 75 unselected HD patients, we also found significant dialysis-induced RWMA in 63% of patients who were undergoing conventional thrice-weekly HD (31).
Cardiac PET scanning using H215O revealed significant dialysis-induced changes in global and segmental MBF. Resting values in these patients were broadly in keeping with published values in patients without CAD or uremia (32). This is expected because ischemic potential of myocardium is determined by reduced CFR rather than resting perfusion. The values were also consistent within an individual between two study sessions. All patients experienced global reduction of MBF, which increased during the HD session and was partially restored to normality 30 min after HD. This observed pattern of change is mirrored in the development of RWMA during HD, both within this study and in others (19,20). The magnitude of the reduction in MBF at peak stress during HD is also broadly comparable with that observed in studies of pharmacologically stressed myocardial ischemia in patients with known significant CAD (14).
The reduction of MBF was significantly more marked in segments of myocardium that also displayed significant dialysis-induced reduction in contractile function. Regional subendocardial and transmural MBF has been well correlated to reduction in segmental ventricular function in studies in conscious dogs that were subjected to graded coronary restriction (33). We observed a similar scale of response in our patients who were subjected to HD.
Although these patients did not have angiographic evidence of significant CAD (indeed, two of the patients had entirely normal coronary angiograms), HD was still capable of inducing myocardial ischemia. Previous descriptions of dialysis-induced myocardial ischemia and, indeed, implied ischemia from dialysis-associated RWMA, indicate that this is a common feature, with a prevalence well in excess of even the more pessimistic estimates of significant CAD in this patient group. As already discussed, patients with chronic kidney disease (especially those who receive HD) are uniquely well primed to experience demand ischemia as a result of a variety of factors relating to the cardiac microcirculation (34), ventricular hypertrophy, and peripheral arterial stiffness (35). Even patients with mild renal insufficiency but without significant CAD have significantly reduced CFR measured at coronary artery catheterization with adenosine challenge (36).
The hemodynamic response to HD was typical of that reported previously. The relative lack of change in heart rate with ultrafiltration-induced changes in BP is also typical. Baroreflex sensitivity is characteristically significantly impaired in this patient group (30) and may account at least in part for the cardiovascular response to HD (37). Such heart rate stability also brings into question the validity of correcting MBF for RPP. Such correction, however, does not alter the pattern or significance of the results reported in this study.
Patients who underwent dialysis using biofeedback control did demonstrate significantly higher recovery of MBF in the postdialysis period. The reduction in BP was more marked when patients underwent dialysis using conventional rather than biofeedback HD. Although these patients did not experience any episodes of intradialytic hypotension (IDH), such biofeedback treatment has been associated with improvement of clinical indices of treatment tolerability even in patients who were characterized as being IDH resistant (38). The difference in BP was significant only in the latter part of the HD treatment. This was in contrast to a previous study of biofeedback dialysis on the development of RWMA (20). Comparison of this study with subsequent reduction in dialysis-induced RWMA using cooling of dialysate (19) suggests that the degree of protection from dialysis-induced cardiac injury is at least in part proportional to the maintenance of BP achieved.
Conclusions
This study demonstrates that the cardiovascular stress of HD is capable of inducing significant global and segmental reductions in MBF. These changes in myocardial perfusion are repetitive and sufficient to result in reduced ventricular contraction. Such repetitive ischemic insults in patients with CAD are widely recognized to be important in the pathogenesis of cardiac failure. HD-induced RWMA are common in dialysis patients. Dialysis-induced myocardial stunning may be an important and previously unappreciated factor in the development of cardiac failure in HD patients. Additional attention to the way in which we dialyze patients may be not only important in the subjective patient tolerability of the treatment but also a key therapeutic target to reduce the vast cardiovascular morbidity and mortality to which these patents are subjected.
Disclosures
None.
Acknowledgments
This study was sponsored by Derby Hospitals NHS Foundation Trust in collaboration with the MRC Clinical Sciences Unit at the Hammersmith Hospital, London.
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Foley RN, Parfrey PS, Sarnak MJ: Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol 9[Suppl]: S16–S23, 1998 [PubMed] [Google Scholar]
- 2.Kalantar-Zadeh K, Block G, Humphreys MH, Kopple JD: Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int 63: 793–808, 2003 [DOI] [PubMed] [Google Scholar]
- 3.Harnett JD, Foley RN, Kent GM, Barre PE, Murray D, Parfrey PS: Congestive heart failure in dialysis patients: Prevalence, incidence, prognosis and risk factors. Kidney Int 47: 884–890, 1995 [DOI] [PubMed] [Google Scholar]
- 4.Bleyer AJ, Russell GB, Satko SG: Sudden and cardiac death rates in hemodialysis patients. Kidney Int 55: 1553–1559, 1999 [DOI] [PubMed] [Google Scholar]
- 5.Bleyer AJ, Hartman J, Brannon PC, Reeves-Daniel A, Satko SG, Russell G: Characteristics of sudden death in hemodialysis patients. Kidney Int 69: 2268–2273, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Selby NM, McIntyre CW: The acute cardiac effects of dialysis. Semin Dial 20: 220–228, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Boon D, van Montfrans GA, Koopman MG, Krediet RT, Bos WJ: Blood pressure response to uncomplicated hemodialysis: The importance of changes in stroke volume. Nephron Clin Pract 96: c82–c87, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Bos WJ, Bruin S, van Olden RW, Keur I, Wesseling KH, Westerhof N, Krediet RT, Arisz LA: Cardiac and hemodynamic effects of hemodialysis and ultrafiltration. Am J Kidney Dis 35: 819–826, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Cheung AK, Sarnak MJ, Yan G, Berkoben M, Heyka R, Kaufman A, Lewis J, Rocco M, Toto R, Windus D, Ornt D, Levey AS: Cardiac diseases in maintenance hemodialysis patients: Results of the HEMO Study. Kidney Int 65: 2380–2389, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Ragosta M, Samady H, Isaacs RB, Gimple LW, Sarembock IJ, Powers ER: Coronary flow reserve abnormalities in patients with diabetes mellitus who have end-stage renal disease and normal epicardial coronary arteries. Am Heart J 147: 1017–1023, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Tok D, Gullu H, Erdogan D, Topcu S, Ciftci O, Yildirim I, Muderrisoglu H: Impaired coronary flow reserve in hemodialysis patients: A transthoracic Doppler echocardiographic study. Nephron Clin Pract 101: c200–c206, 2005 [DOI] [PubMed] [Google Scholar]
- 12.Ichimaru K, Horie A: Microangiopathic changes of subepidermal capillaries in end-stage renal failure. Nephron 46: 144–149, 1987 [DOI] [PubMed] [Google Scholar]
- 13.Braunwald E, Kloner RA: The stunned myocardium: Prolonged, postischemic ventricular dysfunction. Circulation 66: 1146–1149, 1982 [DOI] [PubMed] [Google Scholar]
- 14.Barnes E, Hall RJ, Dutka DP, Camici P: Absolute blood flow and oxygen consumption in stunned myocardium in patients with coronary artery disease. J Am Coll Cardiol 39: 420–427, 2002 [DOI] [PubMed] [Google Scholar]
- 15.Kloner RA, Allen J, Cox TA, Zheng Y, Ruiz CE: Stunned left ventricular myocardium after exercise treadmill testing in coronary artery disease. Am J Cardiol 68: 329–334, 1991 [DOI] [PubMed] [Google Scholar]
- 16.Barnes E, Dutka DP, Khan M, Camici PG, Hall RJ: Effect of repeated episodes of reversible myocardial ischemia on myocardial blood flow and function in humans. Am J Physiol Heart Circ Physiol 282: H1603–H1608, 2002 [DOI] [PubMed] [Google Scholar]
- 17.Bolli R, Zughaib M, Li XY, Tang XL, Sun JZ, Triana JF, McCay PB: Recurrent ischemia in the canine heart causes recurrent bursts of free radical production that have a cumulative effect on contractile function: A pathophysiological basis for chronic myocardial “stunning.” J Clin Invest 96: 1066–1084, 1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wijns W, Vatner SF, Camici PG: Hibernating myocardium. N Engl J Med 339: 173–181, 1998 [DOI] [PubMed] [Google Scholar]
- 19.Selby NM, Burton JO, Chesterton LJ, McIntyre CW: Dialysis induced regional left ventricular dysfunction is ameliorated by cooling the dialysate. Clin J Am Soc Nephrol 1: 1216–1225, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Selby NM, Lambie SH, Camici PG, Baker CS, McIntyre CW: Occurrence of regional left ventricular dysfunction in patients undergoing standard and biofeedback dialysis. Am J Kidney Dis 47: 830–841, 2006 [DOI] [PubMed] [Google Scholar]
- 21.Dutka DP, Camici PG: The contribution of positron emission tomography to the study of ischemic heart failure. Prog Cardiovasc Dis 43: 399–418, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Daugirdas JT: Second generation logarithmic estimates of single-pool variable volume Kt/V: An analysis of error. J Am Soc Nephrol 4: 1205–1213, 1993 [DOI] [PubMed] [Google Scholar]
- 23.Hermansen F, Ashburner J, Spinks TJ, Kooner JS, Camici PG, Lammertsma AA: Generation of myocardial factor images directly from the dynamic oxygen-15-water scan without use of an oxygen-15-carbon monoxide blood-pool scan. J Nucl Med 39: 1696–1702, 1998 [PubMed] [Google Scholar]
- 24.Hermansen F, Rosen SD, Fath-Ordoubadi F, Kooner JS, Clark JC, Camici PG, Lammertsma AA: Measurement of myocardial blood flow with oxygen-15 labelled water: Comparison of different administration protocols. Eur J Nucl Med 25: 751–759, 1998 [DOI] [PubMed] [Google Scholar]
- 25.Hermansen F, Bloomfield PM, Ashburner J, Camici PG, Lammertsma AA: Linear dimension reduction of sequences of medical images: II. Direct sum decomposition. Phys Med Biol 40: 1921–1941, 1995 [DOI] [PubMed] [Google Scholar]
- 26.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS: Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18: 539–542, 2002 [PubMed] [Google Scholar]
- 27.Jagathesan R, Kaufmann PA, Rosen SD, Rimoldi OE, Turkeimer F, Foale R, Camici PG: Assessment of the long-term reproducibility of baseline and dobutamine-induced myocardial blood flow in patients with stable coronary artery disease. J Nucl Med 46: 212–219, 2005 [PubMed] [Google Scholar]
- 28.Kaufmann PA, Gnecchi-Ruscone T, Yap JT, Rimoldi O, Camici PG: Assessment of the reproducibility of baseline and hyperemic myocardial blood flow measurements with 15O-labeled water and PET. J Nucl Med 40: 1848–1856, 1999 [PubMed] [Google Scholar]
- 29.Bosch JG, Savalle LH, van Burken G, Reiber JH: Evaluation of a semiautomatic contour detection approach in sequences of short-axis two-dimensional echocardiographic images. J Am Soc Echocardiogr 8: 810–821, 1995 [DOI] [PubMed] [Google Scholar]
- 30.Chesterton L, Sigrist M, Bennett T, Taal M, McIntyre C: Reduced baroreflex sensitivity is associated with increased vascular calcification and arterial stiffness. Nephrol Dial Transplant 20: 1140–1147, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Burton JO, Korsheed S, John SG, McIntyre CW: Haemodialysis induced cardiac injury is associated with asymptomatic hypotension [Abstract]. J Am Soc Nephrol 18: 67A, 2007 [Google Scholar]
- 32.Uren NG, Camici PG, Melin JA, Bol A, de Bruyne B, Radvan J, Olivotto I, Rosen SD, Impallomeni M, Wijns W: Effect of aging on myocardial perfusion reserve. J Nucl Med 36: 2032–2036, 1995 [PubMed] [Google Scholar]
- 33.Vatner SF: Correlation between acute reductions in myocardial blood flow and function in conscious dogs. Circ Res 47: 201–207, 1980 [DOI] [PubMed] [Google Scholar]
- 34.Camici PG, Crea F: Coronary microvascular dysfunction. N Engl J Med 356: 830–840, 2007 [DOI] [PubMed] [Google Scholar]
- 35.Ohtsuka S, Kakihana M, Watanabe H, Sugishita Y: Chronically decreased aortic distensibility causes deterioration of coronary perfusion during increased left ventricular contraction. J Am Coll Cardiol 24: 1406–1414, 1994 [DOI] [PubMed] [Google Scholar]
- 36.Chade AR, Brosh D, Higano ST, Lennon RJ, Lerman LO, Lerman A: Mild renal insufficiency is associated with reduced coronary flow in patients with non-obstructive coronary artery disease. Kidney Int 69: 266–271, 2006 [DOI] [PubMed] [Google Scholar]
- 37.McIntyre C: The functional cardiovascular consequences of vascular calcification. Semin Dial 20: 122–128, 2007 [DOI] [PubMed] [Google Scholar]
- 38.McIntyre C, Lambie S, Fluck R: Biofeedback controlled hemodialysis (BF-HD) reduces symptoms and increases both hemodynamic tolerability and dialysis adequacy in non-hypotension prone stable patients. Clin Nephrol 60: 105–112, 2003 [DOI] [PubMed] [Google Scholar]