Abstract
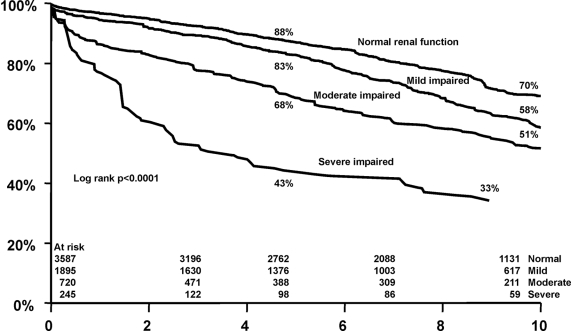
It remains unclear whether mild renal dysfunction is associated with adverse cardiovascular outcome. We investigated whether estimated glomerular filtration rate (eGFR) was associated with mortality and cardiac death among 6447 patients with known or suspected coronary artery disease over a mean follow-up of 7 yr. Cumulative 5- and 10-yr survival rates decreased in a graded fashion from 88% and 70%, respectively, for those with normal renal function to 43% and 33% for those with eGFR <30 ml/min. Compared with patients with normal renal function, the multivariable adjusted hazard ratios for all-cause mortality among patients with mild, moderate, and severe renal impairment were 1.33 (95% confidence interval [CI], 1.21–1.48), 1.67 (95% CI, 1.44–1.93), and 3.38 (95% CI, 2.73–4.19), respectively. Similar relationships between cardiac death and decreasing renal function were found. In conclusion, renal function is a graded and independent predictor of long-term mortality in patients with known or suspected coronary artery disease. Intense treatment and close surveillance of these patients is encouraged.
Chronic renal dysfunction has been shown to be an independent risk factor for cardiovascular mortality and morbidity in patients with coronary artery disease (CAD).1–7 Population-based studies have shown discordant results regarding the association of mild renal dysfunction,8–10 cardiovascular disease events, and all-cause mortality. Serum creatinine >1.5 mg/dl (133 μmol/L) was associated with a 70% increase in risk for all-cause mortality in participants who were followed for 5 yr in the Cardiovascular Health Study11; however, the Framingham Study did not show an association between baseline renal function and incident cardiovascular disease events.12 Furthermore, the results of the National Health and Nutrition Examination Survey (NHANES) study did not support moderate renal insufficiency as an independent risk factor for cardiovascular disease in the general population.13 It remains unclear whether mild renal dysfunction is related to adverse cardiovascular outcomes; therefore, the purpose of this study was to determine the association between mild renal dysfunction and mortality during long-term follow-up.
RESULTS
Mean age was 63 yr, and 26% were women (Table 1). Renal function was normal (GFR >90 ml/min) in 3587 (56%) patients, whereas 720 (11%) had moderate impairment (GFR 30 to 60 ml/min) and 245 (4%) patients had severe impairment (GFR <30 ml/min). A mild degree of renal dysfunction (GFR 60 to 90 ml/min) was present in 1895 (29%) patients. The mean follow-up time was 7 yr (range 6 mo to 12 yr). During follow-up, 37,392 patient-years were collected. Death occurred in 2007 (31%) patients, 54% of which were cardiac. The GFR (mean ± SD 83.1 ± 16) ranged from 3.8 to 265.3 ml/min per 1.73 m2.
Table 1.
Clinical characteristics stratified by the creatinine clearance (GFR)a
| Variable | Total (n = 6447) | GFR
|
P for Trend | |||
|---|---|---|---|---|---|---|
| Normal (>90 ml/min; n = 3587; 56%) | Mild (60 to 90 ml/min; n = 1895; 29%) | Moderate (30 to 60 ml/min; n = 720; 11%) | Severe (<30 ml/min; n = 245; 4%) | |||
| Age (mean ± SD) | 61 ± 11 | 60 ± 18 | 64 ± 10 | 61 ± 12 | 58 ± 13 | <0.0001 |
| Male (%) | 67 | 66 | 75 | 69 | 73 | 0.1 |
| History (%) | ||||||
| MI | 33 | 35 | 30 | 22 | 22 | <0.0001 |
| CABG | 13 | 17 | 19 | 13 | 9 | <0.0001 |
| PCI | 17 | 18 | 17 | 11 | 10 | 0.4 |
| heart failure | 15 | 13 | 16 | 26 | 31 | <0.001 |
| angina | 24 | 27 | 23 | 13 | 7 | 0.2 |
| Risk factors (%) | ||||||
| diabetes | 15 | 14 | 15 | 19 | 23 | <0.005 |
| hypertension | 45 | 39 | 55 | 64 | 72 | <0.0001 |
| dyslipidemia | 36 | 35 | 37 | 45 | 44 | <0.001 |
| smoking | 28 | 30 | 25 | 21 | 23 | <0.0001 |
| Cardiac medication (%) | ||||||
| β blockers | 42 | 36 | 46 | 60 | 63 | <0.0001 |
| nitrates | 17 | 16 | 19 | 23 | 28 | <0.0001 |
| calcium antagonists | 30 | 30 | 29 | 27 | 34 | 0.3 |
| diuretics | 11 | 9 | 15 | 15 | 11 | <0.0001 |
| ACEI | 13 | 10 | 21 | 18 | 22 | <0.0001 |
| digitalis | 3 | 3 | 3 | 4 | 4 | 0.5 |
| Serum creatinine (μmol/L; mean ± SD) | 105 ± 16 | 71 ± 14 | 101 ± 14 | 152 ± 30 | 346 ± 81 | <0.0001 |
| GFR (ml/min; mean ± SD) | 89 ± 16 | 122 ± 21 | 75 ± 8 | 47 ± 8 | 15 ± 8 | <0.0001 |
CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
After adjustment for all baseline clinical and demographic characteristics, the risk for all-cause mortality and cardiac death was significantly increased in all three groups of renal impairment compared with the group with normal renal function (Table 2). Patients with mild impaired renal function had 33% increased risk for mortality (hazard ratio [HR] 1.33; 95% confidence interval [CI] 1.21 to 1.48) as compared with patients with normal renal function. The risk for mortality was increased 1.5-fold with moderate renal insufficiency (HR 1.67; 95% CI 1.44 to 1.93) and three-fold with severe renal impairment (HR 3.38; 95% CI 2.73 to 4.19). Although renal function is related to age, no significant interaction was found. Similar strong relations with cardiac death with decreasing renal function were found. The adjusted HR for GFR as a continuous variable for all-cause mortality or cardiac death were 0.82 (95% CI 0.80 to 0.84) and 0.85 (95% CI 0.82 to 0.88), respectively.
Table 2.
HR for the incidence of all-cause mortality, cardiac death, and hard cardiac events (cardiac death or nonfatal MI) associated with renal function estimated by levels of the creatinine clearance (GFR).
| Parameter | Events (%) | HR (95% CI)
|
|
|---|---|---|---|
| Unadjusted | Adjusteda | ||
| All-cause mortality | |||
| normal renal function | 25 | 1.0 | 1.0 |
| mild impaired renal function | 36 | 1.49 (1.35 to 1.65) | 1.33 (1.21 to 1.48) |
| moderate impaired renal function | 45 | 2.07 (1.80 to 2.37) | 1.67 (1.44 to 1.93) |
| severe impaired renal function | 47 | 4.00 (3.26 to 4.93) | 3.38 (2.73 to 4.19) |
| Cardiac death | |||
| normal impaired renal function | 13 | 1.0 | 1.0 |
| mild impaired renal function | 18 | 1.39 (1.20 to 1.61) | 1.46 (1.25 to 1.71) |
| moderate impaired renal function | 26 | 2.31 (1.93 to 2.78) | 2.31 (1.90 to 2.81) |
| severe impaired renal function | 40 | 6.28 (5.00 to 7.89) | 5.57 (4.38 to 7.08) |
Adjusted for age, gender, previous MI, previous CABG, previous PCI, history of heart failure, history of typical angina, diabetes, hypertension, dyslipidemia, and current smoking.
Age-adjusted cumulative Kaplan-Meier survival curves for all-cause mortality according to renal function were 88, 83, 68, and 43% for normal, mild, moderate, and severe, respectively, at 5 yr and 70, 58, 51, and 33%, respectively, at 10 yr (P < 0.0001; Figure 1). Similar relations with cardiac death with decreasing renal function were found.
Figure 1.
Age-adjusted all-cause mortality in 6447 patients with known or suspected CAD according to the GFR.
DISCUSSION
The main finding of this study is that mild renal dysfunction defined as a GFR of 60 to 90 ml/min is a graded and independent predictor of long-term outcome of mortality and hard cardiac events. Mild or moderate impairment of renal function has also been shown to be associated with worse prognosis in patients with congestive heart failure,14 those with myocardial infarction (MI),15 and those in a normal population16; however, why even a mild renal dysfunction is related with worse prognosis is not known. One possibility might be that renal dysfunction may be a pathogenetic factor in causing the progression of cardiac deterioration. Furthermore, cardiac pump failure may lead to diminished renal function, and thus early renal dysfunction may be a marker of increased cardiac function; however, we still observed an independent association between renal function and all-cause mortality and cardiac death after adjusting for cardiovascular risk factors. Therefore, renal impairment itself might initiate and accelerate adverse cardiac events.
Usually, kidney disease is defined as GFR <60 ml/min per 1.73 m2, a cutoff value recently proposed by the National Kidney Foundation's Kidney Disease Outcomes Quality Initiative Advisory Board to identify patients who have moderate renal impairment17 and American Heart Association's Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention.5The results of this study show an increased risk for mortality and hard cardiac events, starting at earlier stages of renal dysfunction than commonly thought. This mildly decreased renal dysfunction, one quarter of this study, represent patients without symptoms and signs of renal dysfunction. As patients get older, mild degrees of renal insufficiency will become progressively more important because renal function declines with elderly age; therefore, early recognition of renal dysfunction may be a key target to prevent worsening renal function.
Treatment of patients with impaired renal function and CAD is problematic. Evidence of medical therapy both in trials and in clinical practice is limited and frequently suboptimal. Acetylsalicylic acid (ASA)18 and β blockers19 were shown to reduce mortality among patients with CAD and may also reduce mortality and morbidity in asymptomatic patients who are at increased risk for CAD. Also evidence continues to accrue that angiotensin-converting enzyme inhibitors ACEI reduce vascular morbidity and mortality.20–22 Furthermore, a systematic review demonstrated in patients who had renal insufficiency and were treated with ACEI a strong association between creatinine levels and slowing of the renal disease progression in the long term.8 The authors concluded that ACEI therapy should be offered to all patients with left ventricular systolic dysfunction and renal insufficiency, and also the sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure recommends use of ACEI for control of hypertension in patients with renal insufficiency.9 The use of statins has also been shown to reduce mortality. Although there might be a slight increase of myositis, statins are generally considered safe for use in patients with renal insufficiency9; however, these therapies are still underused among patients with renal impairment. Although there may be exceptions, therapies that have been beneficial at normal levels of kidney function are increasingly being shown also to be beneficial at lower levels of kidney function23; therefore, intensive medical treatment, especially in patients with only mild renal dysfunction and without any signs of renal disease, including β blockers, ACEI, and statins, should be considered.
Although data were prospectively collected, this analysis is retrospective. Only patients for whom a single baseline creatinine value was available were included in this study, which may have introduced a selection bias in the analysis. Thus, this study cohort was per definition a preselected one, already having a higher risk for death earlier than an average population. This includes the renal reference group; therefore, all conclusions regarding the outcome of the four GFR groups must take this into account. Another limitation is the lack of data on albuminuria, which may contribute to the cardiovascular effects of renal dysfunction.24
This study shows that renal function is a graded and independent predictor of long-term adverse cardiac outcome. In particularly, even mild renal dysfunction is an important predictor of all-cause mortality and cardiac death. Intense treatment and close surveillance of these patients is warranted.
CONCISE METHODS
Study Design and Patient Selection
We studied a cohort of 6447 patients who had known or suspected CAD, had had baseline serum creatinine determined, and were referred to the outpatient clinics of the Erasmus University Medical Center between January 1993 and January 2005. Patients who were included in our analysis were intermediate- to high-risk patients who had atherosclerotic disease and were referred for cardiac evaluation, management of underlying risk factors, or follow-up of their known ischemic heart condition.
Patients who presented at the time of examination with a history of angina, previous MI, or myocardial revascularization (i.e., previous percutaneous coronary intervention and/or coronary artery bypass graft) were considered as CAD patients. Patients with atypical chest pain, dyspnea, atypical electrocardiogram abnormalities (ST-T changes without Q-waves), or multiple risk factors for coronary disease were considered to have suspected CAD. Patients who were on hemodialysis therapy or had undergone a renal transplant were excluded. The study protocol was approved by the local medical ethics committee and was conducted in accordance with the Declaration of Helsinki.
Renal Function Assessment
Serum creatinine was assessed by a nonkinetic alkaline picrate (Jaffe) method.25 GFR was estimated by using the Modification of Diet in Renal Disease (MDRD) equation26: GFR (ml/min per 1.73 m2 body surface area) = 175 × (serum creatinine)−1.154× age−0.203× 0.742 (if female).
Clinical Follow-up and End Points
In-hospital clinical information for patients was retrieved from an electronic database that is maintained in our hospital and by review of hospital records. Survival status was obtained from the municipal civil registries. Follow-up was performed by mailed questionnaires and telephone interviews. Patients who were lost to follow-up were considered at risk until the date of last contact, at which point they were censored. When needed, referring physicians and institutions were contacted for additional information. Events and cause of death were verified by contacting the patient's primary physician and reviewing medical records. The follow-up was complete in 98.3%. The end points considered were all-cause mortality and cardiac death. Death was considered cardiac when it was caused by acute MI, significant arrhythmias, or refractory heart failure. Sudden unexpected death occurring without another explanation was included as cardiac death.
Statistical Analyses
Continuous variables are presented as the mean ± SD or as a percentage. Patients were subsequently categorized as having normal renal function (GFR >90 ml/min), mild renal impairment (GFR 60 to 90 ml/min), moderate impairment (GFR 30 to 60 ml/min), and severe impairment (GFR <30 ml/min).5 Tests of trend were performed using the four GFR groups as a categorical measurement. Continuous variables are presented as the mean ± SD or as a percentage. Cox proportional hazard regression analysis was used to investigate the independent effect of renal function on the outcome events. Analyses were conducted for crude values and adjusted for age; gender; previous MI; previous percutaneous coronary intervention; previous coronary artery bypass graft surgery; history of typical of angina; history of heart failure (defined according the New York Heart Association classification); diabetes (defined as the presence of a fasting blood glucose ≥126 mg/dl or requirement for insulin or oral hypoglycemic agents); hypercholesterolemia (defined as total cholesterol of >200 mg/dl); hypertension (defined as systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, or use of antihypertensive medication); smoking; and the use of statins, β blockers, nitrates, calcium antagonists, ACEI, digitalis, and diuretics. The association between GFR and outcome events was also assessed with GFR as a continuous variable. To investigate the relation between GFR and age, we performed a test for interaction in the Cox regression. Using Cox regression, age-adjusted Kaplan-Meier survival curves of the four GFR groups in relation to all-cause mortality were constructed and examined using the log-rank test.
DISCLOSURES
None.
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1.Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S: Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann Intern Med 134: 629–636, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA: Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med 351: 1285–1295, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Al Suwaidi J, Reddan DN, Williams K, Pieper KS, Harrington RA, Califf RM, Granger CB, Ohman EM, Holmes DR Jr; GUSTO-IIb, GUSTO-III, PURSUIT. Global Use of Strategies to Open Occluded Coronary Arteries. Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy; PARAGON-A Investigators: Platelet IIb/IIIa antagonism for the reduction of acute coronary syndrome events in a Global Organization Network: Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation 106: 974–980, 2002 [DOI] [PubMed] [Google Scholar]
- 4.Gibson CM, Pinto DS, Murphy SA, Morrow DA, Hobbach HP, Wiviott SD, Giugliano RP, Cannon CP, Antman EM, Braunwald E, TIMI Study Group: Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol 42: 1535–1543, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, McCullough PA, Kasiske BL, Kelepouris E, Klag MJ, Parfrey P, Pfeffer M, Raij L, Spinosa DJ, Wilson PW, American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention: Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 108: 2154–2169, 2003 [DOI] [PubMed] [Google Scholar]
- 6.Szczech LA, Best PJ, Crowley E, Brooks MM, Berger PB, Bittner V, Gersh BJ, Jones R, Califf RM, Ting HH, Whitlow PJ, Detre KM, Holmes D, Bypass Angioplasty Revascularization Investigation (BARI) Investigators: Outcomes of patients with chronic renal insufficiency in the bypass angioplasty revascularization investigation. Circulation 105: 2253–2258, 2002 [DOI] [PubMed] [Google Scholar]
- 7.Blackman DJ, Pinto R, Ross JR, Seidelin PH, Ing D, Jackevicius C, Mackie K, Chan C, Dzavik V: Impact of renal insufficiency on outcome after contemporary percutaneous coronary intervention. Am Heart J 151: 146–152, 2006 [DOI] [PubMed] [Google Scholar]
- 8.Bakris GL, Weir MR: Angiotensin-converting enzyme inhibitor-associated elevations in serum creatinine: Is this a cause for concern? Arch Intern Med 160: 685–693, 2000 [DOI] [PubMed] [Google Scholar]
- 9.The sixth report of Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Arch Intern Med 157: 2413–2446, 1997 [DOI] [PubMed] [Google Scholar]
- 10.Kasiske BL: Hyperlipidemia in patients with chronic renal disease. Am J Kidney Dis 32: S142–S156, 1998 [DOI] [PubMed] [Google Scholar]
- 11.Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, Robbins JA, Gardin JM: Risk actors for 5-year mortality in older adults: The Cardiovascular Health Study. JAMA 279: 585–592, 1998 [DOI] [PubMed] [Google Scholar]
- 12.Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D: Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 56: 2214–2219, 1999 [DOI] [PubMed] [Google Scholar]
- 13.Garg AX, Clark WF, Haynes RB, House AA: Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int 61: 1486–1494, 2002 [DOI] [PubMed] [Google Scholar]
- 14.Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW: The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 35: 681–689, 2000 [DOI] [PubMed] [Google Scholar]
- 15.Pfeffer MA, McMurray JJ, Velazquez EJ, Rouleau JL, Kober L, Maggioni AP, Solomon SD, Swedberg K, Van de Werf F, White H, Leimberger JD, Henis M, Edwards S, Zelenkofske S, Sellers MA, Califf RM, Valsartan in Acute Myocardial Infarction Trial Investigators: Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med 349: 1893–1906, 2003. 14610160 [Google Scholar]
- 16.Brugts JJ, Knetsch AM, Mattace-Raso FU, Hofman A, Witteman JC: Renal function and risk of myocardial infarction in an elderly population: The Rotterdam Study. Arch Intern Med 165: 2659–2665, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G, National Kidney Foundation: National Kidney Foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann Intern Med 139: 137–147, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Collaborative overview of randomised trials of antiplatelet therapy: I—Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists’ Collaboration. BMJ 308: 81–106, 1994. [published erratum appears in BMJ 308: 1540, 1994] [PMC free article] [PubMed] [Google Scholar]
- 19.Jonas M, Reicher-Reiss H, Boyko V, Shotan A, Mandelzweig L, Goldbourt U, Behar S: Usefulness of beta-blocker therapy in patients with non-insulin-dependent diabetes mellitus and coronary artery disease: Bezafibrate Infarction Prevention (BIP) Study Group. Am J Cardiol 77: 1273–1277, 1996 [DOI] [PubMed] [Google Scholar]
- 20.Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G: Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients: The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 342: 145–153, 2000 [DOI] [PubMed] [Google Scholar]
- 21.Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S, RENAAL Study Investigators: Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345: 861–869, 2001 [DOI] [PubMed] [Google Scholar]
- 22.Hou FF, Zhang X, Zhang GH, Xie D, Chen PY, Zhang WR, Jiang JP, Liang M, Wang GB, Liu ZR, Geng RW: Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med 354: 131–140, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Coresh J, Astor B, Sarnak MJ: Evidence for increased cardiovascular disease risk in patients with chronic kidney disease. Curr Opin Nephrol Hypertens 13: 73–81, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Halle JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S, HOPE Study Investigators: Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286: 421–426, 2001 [DOI] [PubMed] [Google Scholar]
- 25.Perrone RD, Madias NE, Levey AS: Serum creatinine as an index of renal function: New insights into old concepts. Clin Chem 38: 1933–1953, 1992 [PubMed] [Google Scholar]
- 26.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F, Chronic Kidney Disease Epidemiology Collaboration: Using standardized serum creatinine values in the Modification of Diet in Renal Disease study equation for estimating glomerular filtration rate. Ann Intern Med 145: 247–254, 2006 [DOI] [PubMed] [Google Scholar]