Abstract
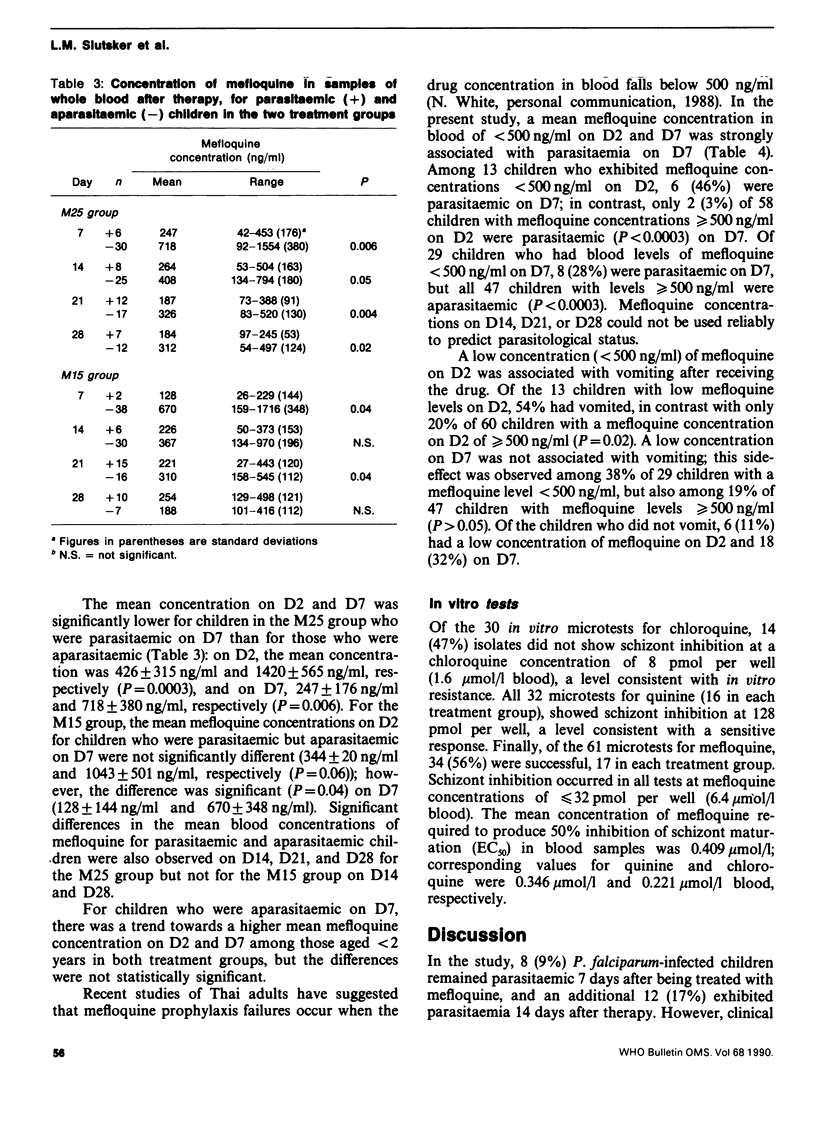
The in vivo and in vitro response of Plasmodium falciparum to a single oral dose of mefloquine (25 mg/kg body weight (M25) or 15 mg/kg (M15] was studied in children under 5 years of age in Malawi. Of the children who received mefloquine, 35% vomited at least once, and 10% did not tolerate the drug because of vomiting. The therapy failure rates for the M25 group on day 7, 14, and 28 were 15%, 18%, and 42%, respectively, and these did not differ significantly from those for the M15 group (4%, 18%, and 59%). In contrast, 34 in vitro microtests (17 per group) showed schizont inhibition at less than or equal to 32 pmol mefloquine per test well. On day 7, the concentration of mefloquine in samples of blood was significantly lower in both the M25 and M15 groups for children who were parasitaemic on day 7 than in samples from those who were aparasitaemic. A positive blood smear on day 7 was strongly associated with a mefloquine concentration of less than 500 ng/ml blood on day 2 or day 7 (P less than 0.0003). Vomiting was associated with a low mefloquine concentration on day 2 but not day 7. These results suggest that mefloquine is effective against P. falciparum in Malawi but that for young children the therapy appears to be complicated by frequent vomiting.
Full text
PDF





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dixon K. E., Williams R. G., Pongsupat T., Pitaktong U., Phintuyothin P. A comparative trial of Mefloquine and Fansidar in the treatment of falciparum malaria: failure of Fansidar. Trans R Soc Trop Med Hyg. 1982;76(5):664–667. doi: 10.1016/0035-9203(82)90238-3. [DOI] [PubMed] [Google Scholar]
- Hall A. P., Doberstyn E. B., Karnchanachetanee C., Samransamruajkit S., Laixuthai B., Pearlman E. J., Lampe R. M., Miller C. F., Phintuyothin P. Sequential treatment with quinine and mefloquine or quinine and pyrimethamine-sulfadoxine for falciparum malaria. Br Med J. 1977 Jun 25;1(6077):1626–1628. doi: 10.1136/bmj.1.6077.1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann D. L., Khoromana C. O., Wirima J. J., Campbell C. C. Comparative efficacy of alternative primary therapies for Plasmodium falciparum infections in Malawi. Trans R Soc Trop Med Hyg. 1987;81(5):722–724. doi: 10.1016/0035-9203(87)90005-8. [DOI] [PubMed] [Google Scholar]
- Khoromana C. O., Campbell C. C., Wirima J. J., Heymann D. L. In vivo efficacy of chloroquine treatment for Plasmodium falciparum in Malawian children under five years of age. Am J Trop Med Hyg. 1986 May;35(3):465–471. doi: 10.4269/ajtmh.1986.35.465. [DOI] [PubMed] [Google Scholar]
- Kofi Ekue J. M., Ulrich A. M., Rwabwogo-Atenyi J., Sheth U. K. A double-blind comparative clinical trial of mefloquine and chloroquine in symptomatic falciparum malaria. Bull World Health Organ. 1983;61(4):713–718. [PMC free article] [PubMed] [Google Scholar]
- Oduola A. M., Milhous W. K., Salako L. A., Walker O., Desjardins R. E. Reduced in-vitro susceptibility to mefloquine in West African isolates of Plasmodium falciparum. Lancet. 1987 Dec 5;2(8571):1304–1305. doi: 10.1016/s0140-6736(87)91195-0. [DOI] [PubMed] [Google Scholar]
- Schwartz D. E., Eckert G., Hartmann D., Weber B., Richard-Lenoble D., Ekue J. M., Gentilini M. Single dose kinetics of mefloquine in man. Plasma levels of the unchanged drug and of one of its metabolites. Chemotherapy. 1982;28(1):70–84. doi: 10.1159/000238062. [DOI] [PubMed] [Google Scholar]
- Sexton J. D., Deloron P., Bugilimfura L., Ntilivamunda A., Neill M. Parasitologic and clinical efficacy of 25 and 50 mg/kg of chloroquine for treatment of Plasmodium falciparum malaria in Rwandan children. Am J Trop Med Hyg. 1988 Mar;38(2):237–243. doi: 10.4269/ajtmh.1988.38.237. [DOI] [PubMed] [Google Scholar]
- de Souza J. M. A phase II clinical trial of mefloquine in Brazilian male subjects. Bull World Health Organ. 1983;61(5):815–820. [PMC free article] [PubMed] [Google Scholar]
- de Souza J. M., Heizmann P., Schwartz D. E. Single-dose kinetics of mefloquine in Brazilian male subjects. Bull World Health Organ. 1987;65(3):353–356. [PMC free article] [PubMed] [Google Scholar]
- de Souza J. M., Sheth U. K., de Oliveira R. M., Roulet H., de Souza S. D. An open, randomized, phase III clinical trial of mefloquine and of quinine plus sulfadoxine-pyrimethamine in the treatment of symptomatic falciparum malaria in Brazil. Bull World Health Organ. 1985;63(3):603–609. [PMC free article] [PubMed] [Google Scholar]


