Abstract
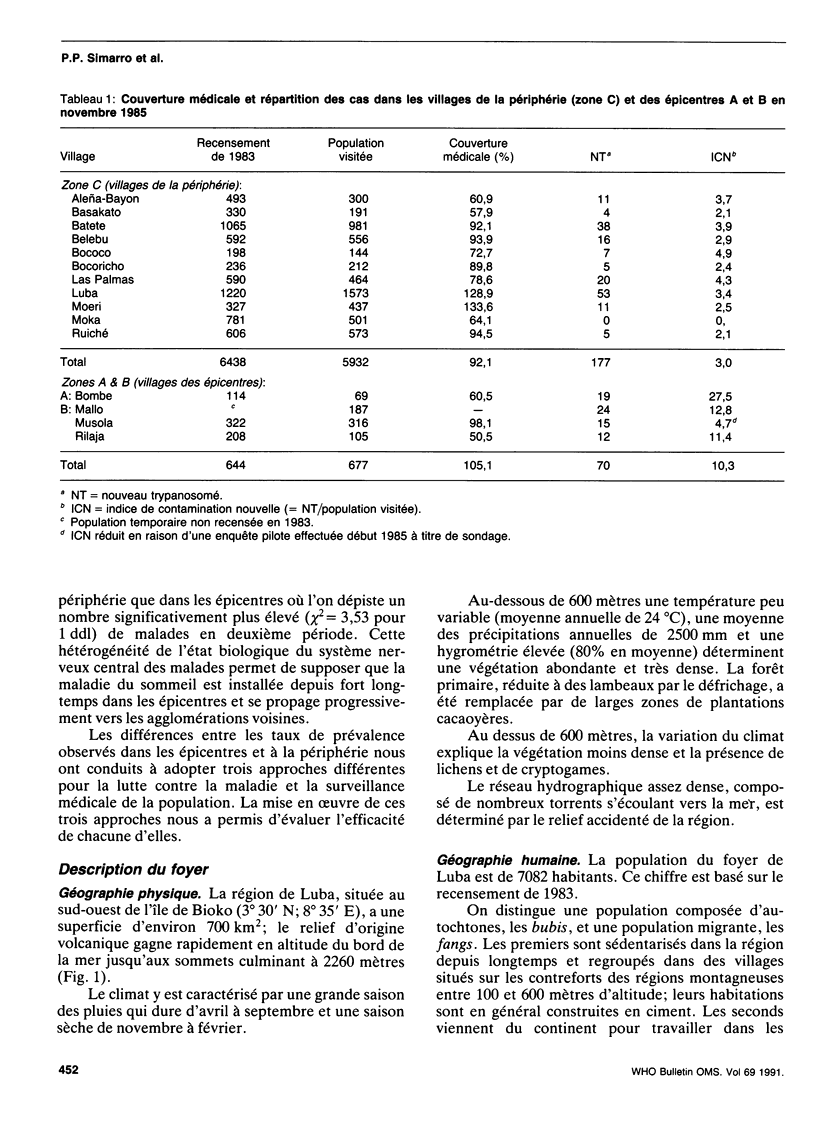
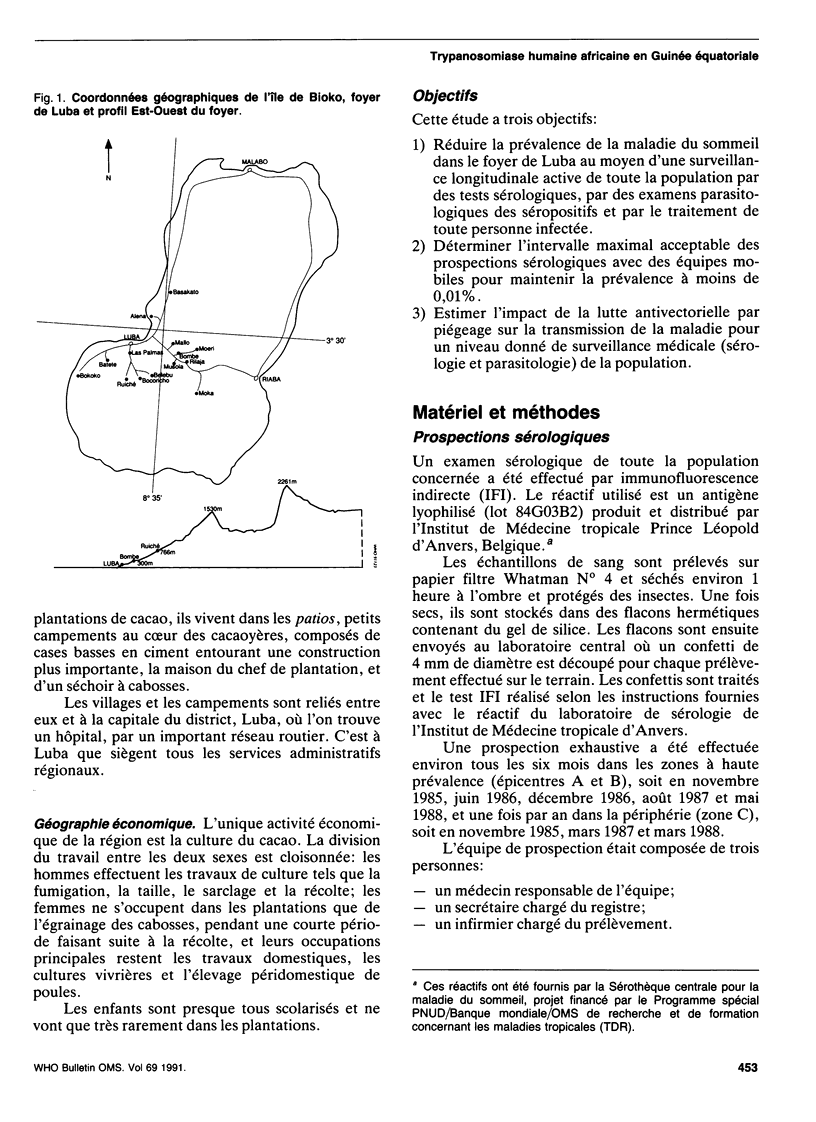
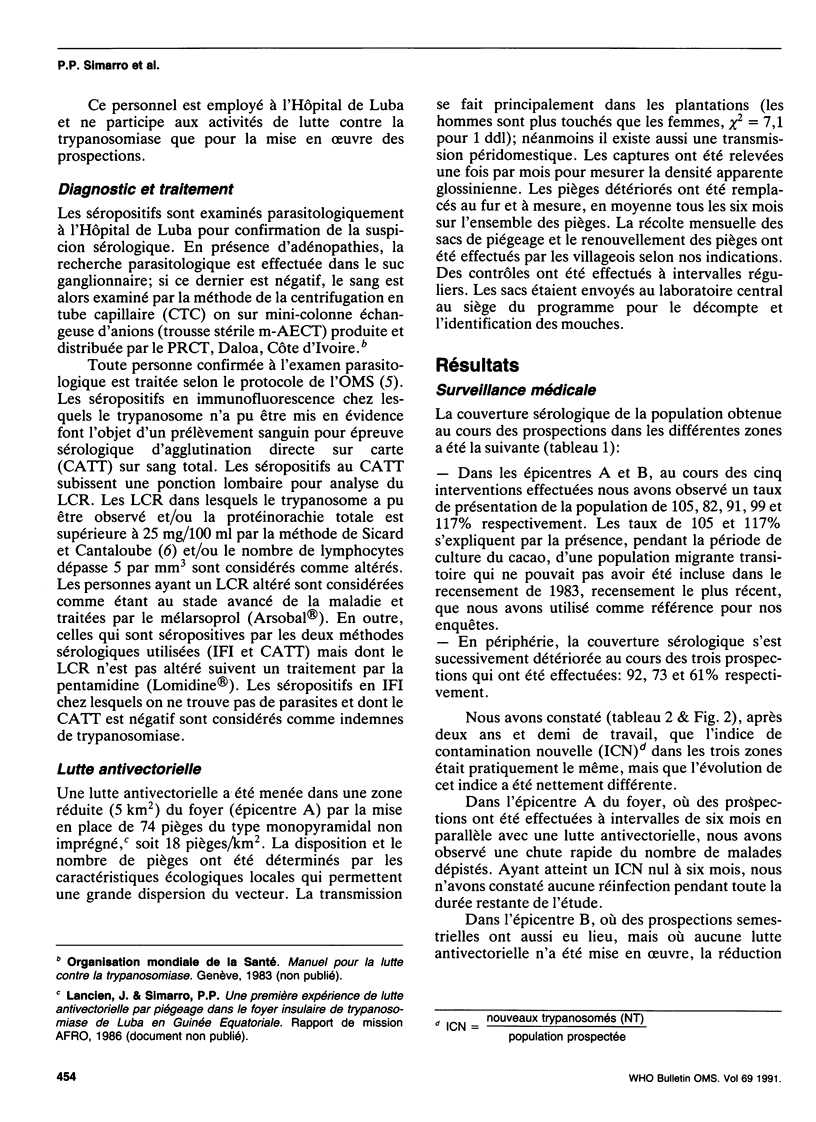
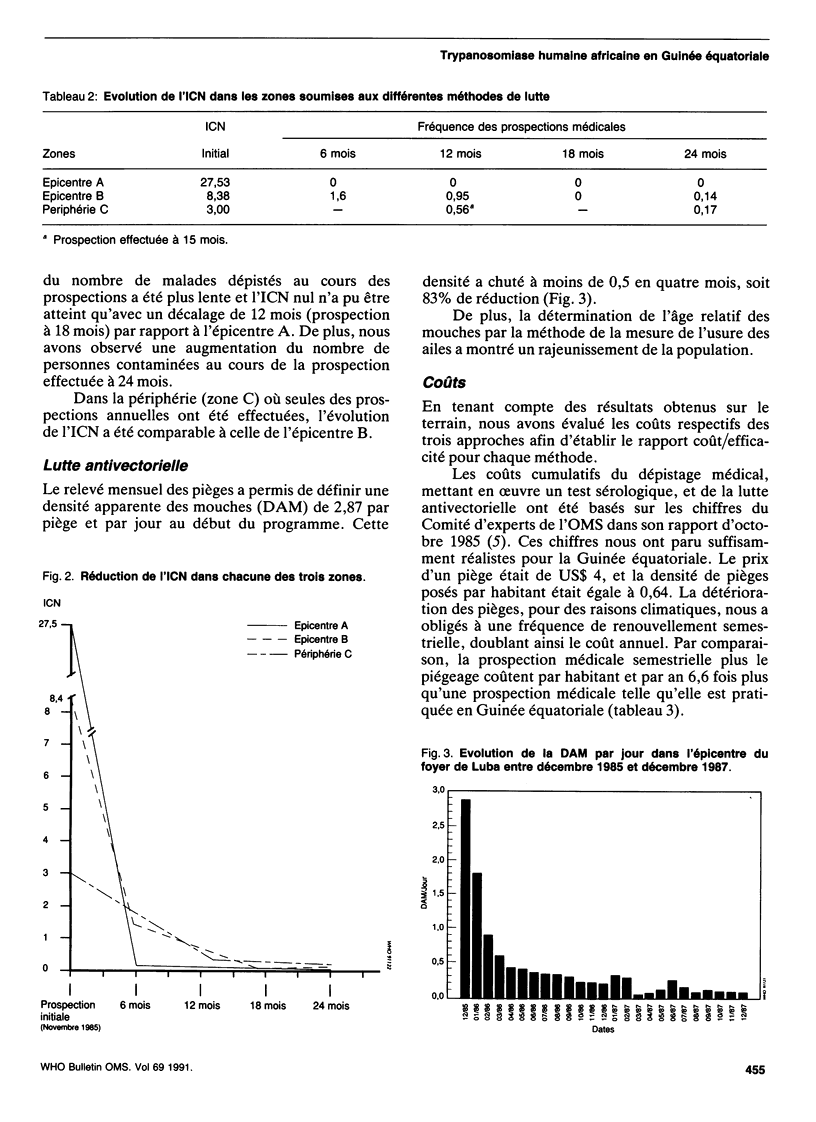
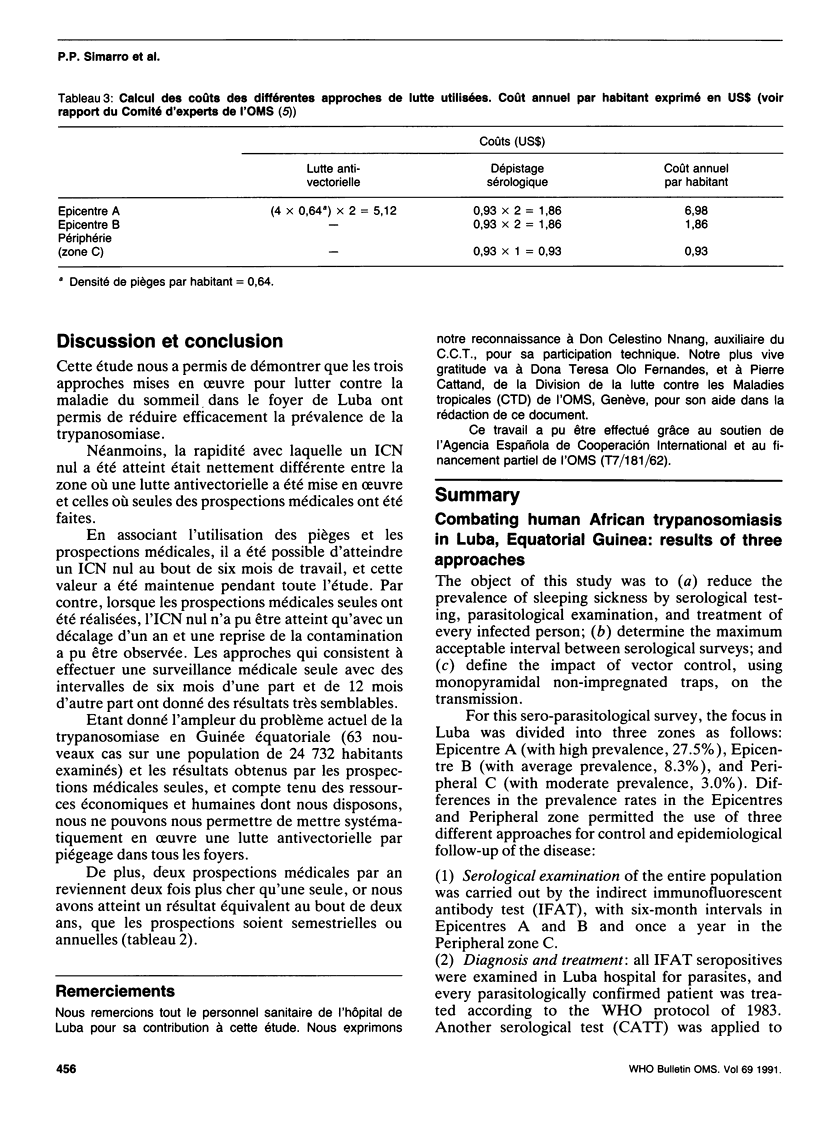
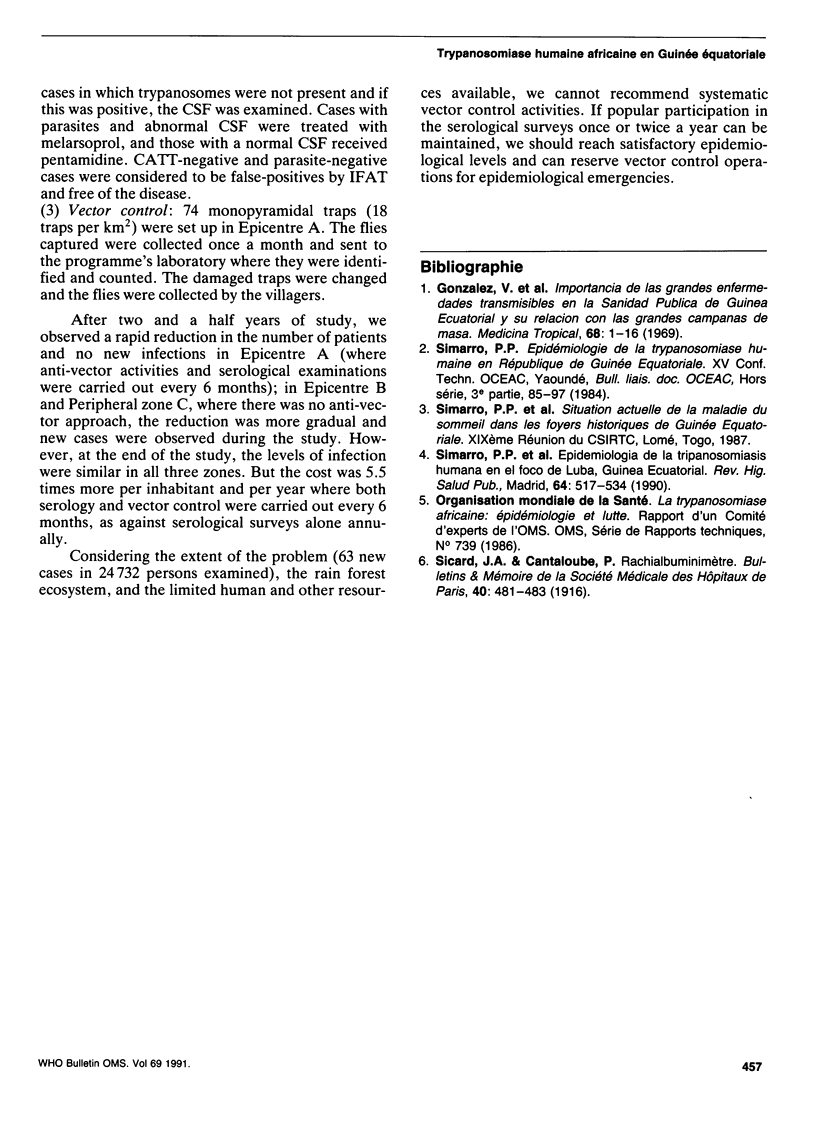
The object of this study was to (a) reduce the prevalence of sleeping sickness by serological testing, parasitological examination, and treatment of every infected person; (b) determine the maximum acceptable interval between serological surveys; and (c) define the impact of vector control, using monopyramidal non-impregnated traps, on the transmission. For this sero-parasitological survey, the focus in Luba was divided into three zones as follows: Epicentre A (with high prevalence, 27.5%), Epicentre B (with average prevalence, 8.3%), and Peripheral C (with moderate prevalence, 3.0%). Differences in the prevalence rates in the Epicentres and Peripheral zone permitted the use of three different approaches for control and epidemiological follow-up of the disease: (1) Serological examination of the entire population was carried out by the indirect immunofluorescent antibody test (IFAT), with six-month intervals in Epicentres A and B and once a year in the Peripheral zone C. (2) Diagnosis and treatment: all IFAT seropositives were examined in Luba hospital for parasites, and every parasitologically confirmed patient was treated according to the WHO protocol of 1983. Another serological test (CATT) was applied to cases in which trypanosomes were not present and if this was positive, the CSF was examined. Cases with parasites and abnormal CSF were treated with melarsoprol, and those with a normal CSF received pentamidine. CATT-negative and parasite-negative cases were considered to be false-positives by IFAT and free of the disease. (3) Vector control: 74 monopyramidal traps (18 traps per km2) were set up in Epicentre A. The flies captured were collected once a month and sent to the programme's laboratory where they were identified and counted.(ABSTRACT TRUNCATED AT 250 WORDS)
Full text
PDF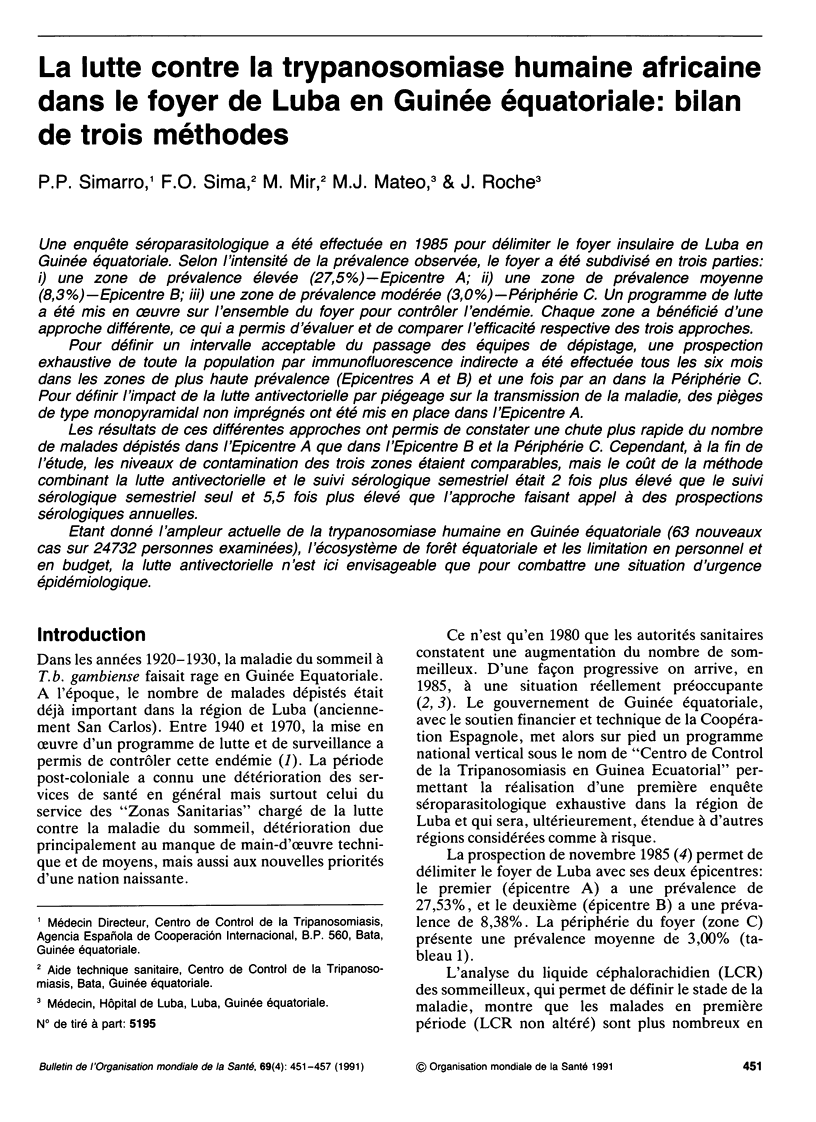
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Simarro P. P., Mas J., Lancien J., Ona Sima F., Mateo M. J., Roche J. Epidemiología de la Tripanosomiasis Humana en el foco de Luba, en Guinea Ecuatorial. Rev Sanid Hig Publica (Madr) 1990 Sep-Oct;64(9-10):517–534. [PubMed] [Google Scholar]



