Abstract
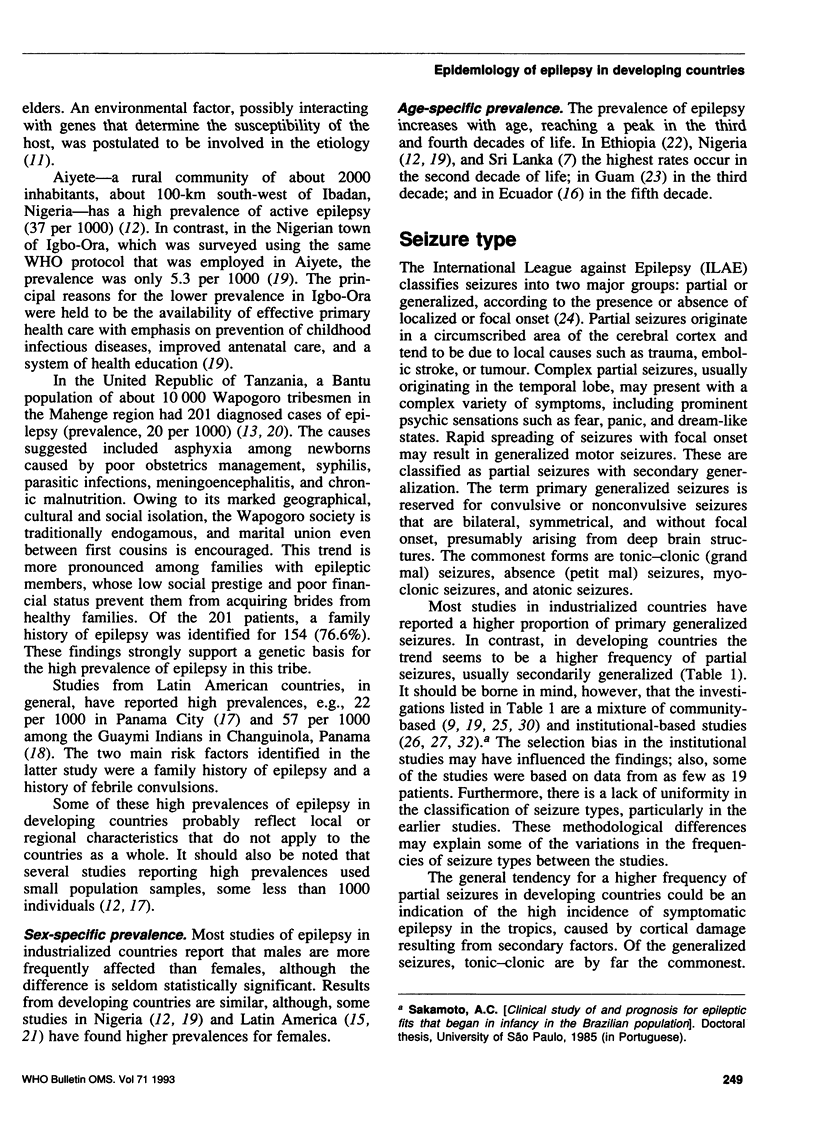
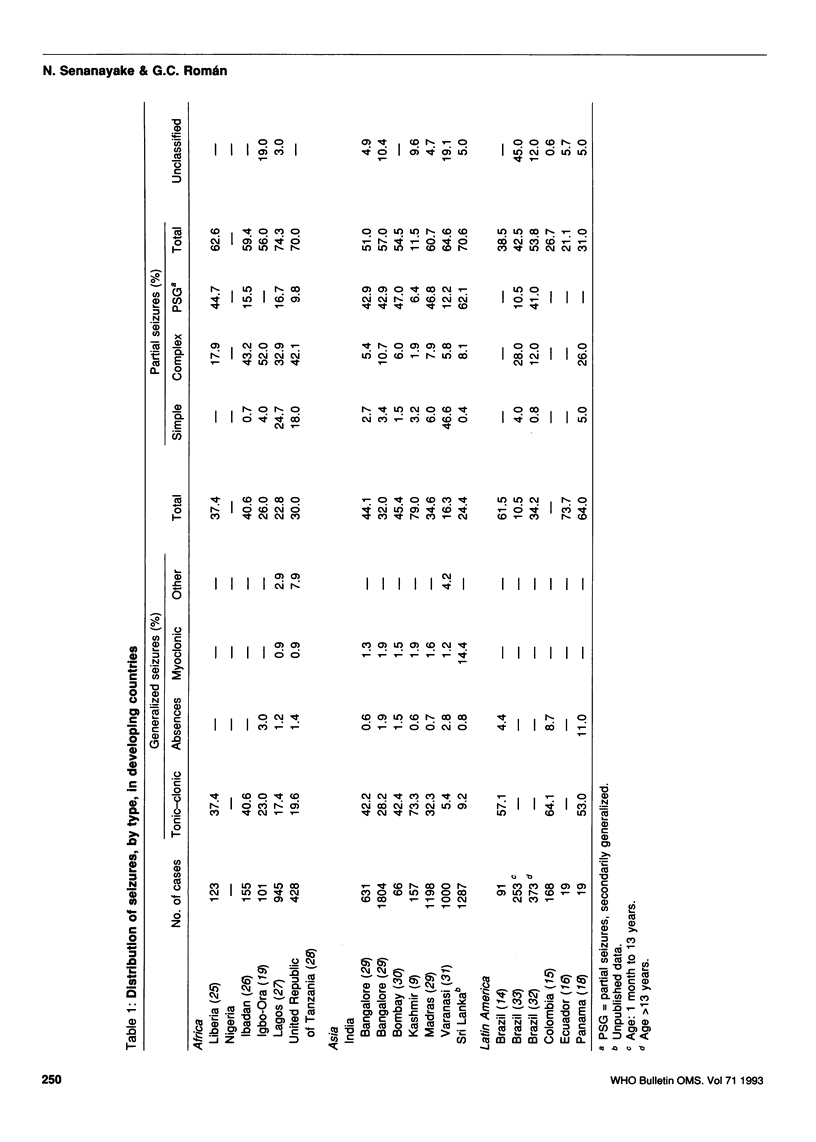
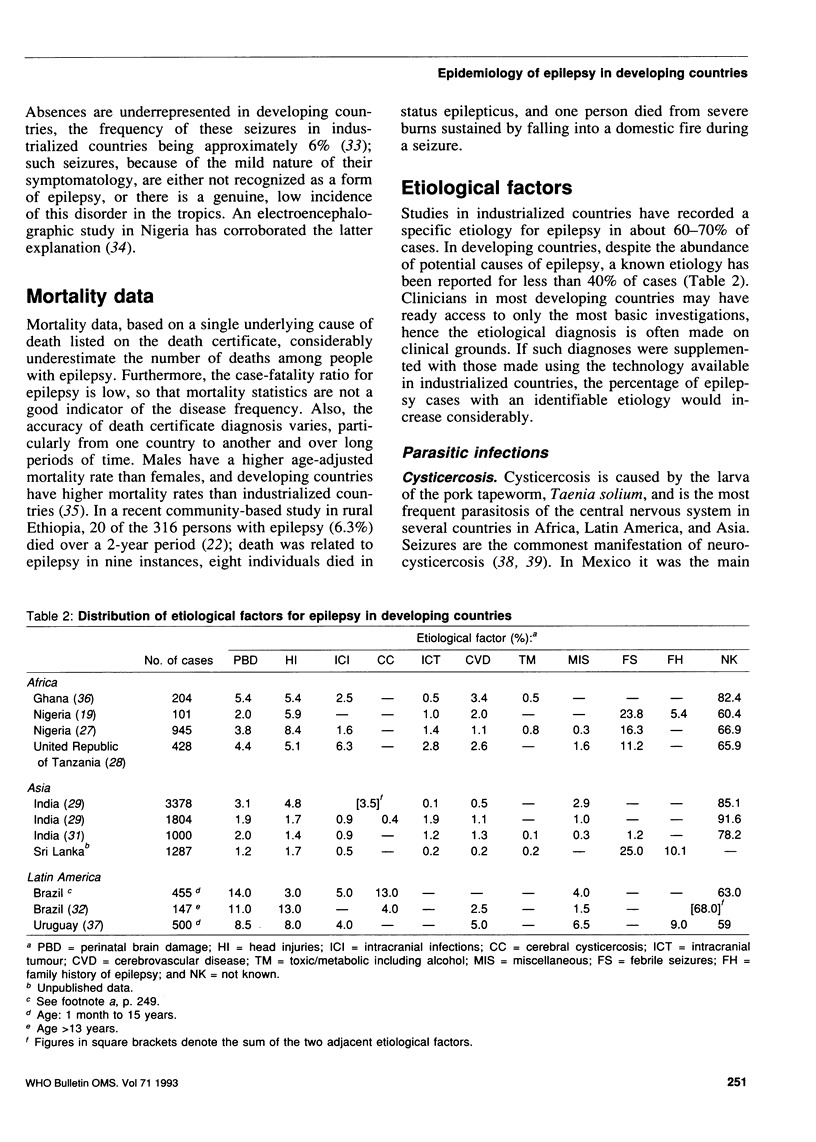
Epilepsy is an important health problem in developing countries, where its prevalence can be up to 57 per 1000 population. This article reviews the epidemiology of epilepsy in developing countries in terms of its incidence, prevalence, seizure type, mortality data, and etiological factors. The prevalence of epilepsy is particularly high in Latin America and in several African countries, notably Liberia, Nigeria, and the United Republic of Tanzania. Parasitic infections, particularly neurocysticercosis, are important etiological factors for epilepsy in many of these countries. Other reasons for the high prevalence include intracranial infections of bacterial or viral origin, perinatal brain damage, head injuries, toxic agents, and hereditary factors. Many of these factors are, however, preventable or modifiable, and the introduction of appropriate measures to achieve this could lead to a substantial decrease in the incidence of epilepsy in developing countries.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahuja G. K., Mohanta A. Late onset epilepsy. A prospective study. Acta Neurol Scand. 1982 Aug;66(2):216–226. doi: 10.1111/j.1600-0404.1982.tb04519.x. [DOI] [PubMed] [Google Scholar]
- Animashaun A. Aetiology of cerebral palsy in African children. Afr J Med Sci. 1971 Apr;2(2):165–171. [PubMed] [Google Scholar]
- Annegers J. F., Hauser W. A., Anderson V. E., Kurland L. T. The risks of seizure disorders among relatives of patients with childhood onset epilepsy. Neurology. 1982 Feb;32(2):174–179. doi: 10.1212/wnl.32.2.174. [DOI] [PubMed] [Google Scholar]
- Annegers J. F., Hauser W. A., Beghi E., Nicolosi A., Kurland L. T. The risk of unprovoked seizures after encephalitis and meningitis. Neurology. 1988 Sep;38(9):1407–1410. doi: 10.1212/wnl.38.9.1407. [DOI] [PubMed] [Google Scholar]
- Asirifi Y. Aetiology of cerebral palsy in developing countries. Dev Med Child Neurol. 1972 Apr;14(2):230–232. [PubMed] [Google Scholar]
- Bahemuka M., Murungi J. H. Tuberculosis of the nervous system. A clinical, radiological and pathological study of 39 consecutive cases in Riyadh, Saudi Arabia. J Neurol Sci. 1989 Mar;90(1):67–76. doi: 10.1016/0022-510x(89)90046-4. [DOI] [PubMed] [Google Scholar]
- Bharucha N. E., Bharucha E. P., Bharucha A. E., Bhise A. V., Schoenberg B. S. Prevalence of epilepsy in the Parsi community of Bombay. Epilepsia. 1988 Mar-Apr;29(2):111–115. doi: 10.1111/j.1528-1157.1988.tb04405.x. [DOI] [PubMed] [Google Scholar]
- Bharucha N. E., Bharucha E. P., Dastur H. D., Schoenberg B. S. Pilot survey of the prevalence of neurologic disorders in the Parsi community of Bombay. Am J Prev Med. 1987 Sep-Oct;3(5):293–299. [PubMed] [Google Scholar]
- Bruck I., Antoniuk S. A., Wittig E., Accorsi A. Neurocisticercose na infância. I. Diagnóstico clínico e laboratorial. Arq Neuropsiquiatr. 1991 Mar;49(1):43–46. doi: 10.1590/s0004-282x1991000100006. [DOI] [PubMed] [Google Scholar]
- CHANG Y. C., CHU C. C., FAN W. K. Cerebral schistosomiasis; an observation of forty-five cases. Chin Med J. 1957 Nov;75(11):892–907. [PubMed] [Google Scholar]
- COSNETT J. E. NEUROLOGICAL DISORDERS IN THE ZULU. Neurology. 1964 May;14:443–454. doi: 10.1212/wnl.14.5.443. [DOI] [PubMed] [Google Scholar]
- Cruz M. E., Schoenberg B. S., Ruales J., Barberis P., Proano J., Bossano F., Sevilla F., Bolis C. L. Pilot study to detect neurologic disease in Ecuador among a population with a high prevalence of endemic goiter. Neuroepidemiology. 1985;4(2):108–116. doi: 10.1159/000110221. [DOI] [PubMed] [Google Scholar]
- Danesi M. A. Classification of the epilepsies: an investigation of 945 patients in a developing country. Epilepsia. 1985 Mar-Apr;26(2):131–136. doi: 10.1111/j.1528-1157.1985.tb05396.x. [DOI] [PubMed] [Google Scholar]
- Dumas M., Grunitzky E., Deniau M., Dabis F., Bouteille B., Belo M., Pestre-Alexandre M., Catanzano G., Darde M. L., D'Almeida M. Epidemiological study of neuro-cysticercosis in northern Togo (West Africa). Acta Leiden. 1989;57(2):191–196. [PubMed] [Google Scholar]
- Edoo B. B., Haddock D. R. Epilepsy in Accra, Ghana: a report on classification and etiology. Afr J Med Sci. 1970 Apr;1(2):207–212. [PubMed] [Google Scholar]
- GREENGARD J., ROWLEY W., ELAM H., PERLSTEIN M. Lead encephalopathy in children. Intravenous use of urea in its management. N Engl J Med. 1961 May 18;264:1027–1030. doi: 10.1056/NEJM196105182642004. [DOI] [PubMed] [Google Scholar]
- Gerrits C. A West African epilepsy focus. Lancet. 1983 Feb 12;1(8320):358–358. doi: 10.1016/s0140-6736(83)91663-x. [DOI] [PubMed] [Google Scholar]
- Giel R. The problem of epilepsy in Ethiopia. Trop Geogr Med. 1970 Dec;22(4):439–442. [PubMed] [Google Scholar]
- Gomez J. G., Arciniegas E., Torres J. Prevalence of epilepsy in Bogota, Colombia. Neurology. 1978 Jan;28(1):90–94. doi: 10.1212/wnl.28.1.90. [DOI] [PubMed] [Google Scholar]
- Gracia F. J., Bayard V., Triana E., Castillo L. C., Benzadón A., Larreátegui M., Cerrud R., Politis S. Prevalencia de enfermedades neurológicas en el Corregimiento de Belisario Porras, Distrito de San Miguelito, en Panamá, 1986. Rev Med Panama. 1988 Jan;13(1):40–45. [PubMed] [Google Scholar]
- Gracia F., de Lao S. L., Castillo L., Larreategui M., Archbold C., Brenes M. M., Reeves W. C. Epidemiology of epilepsy in Guaymi Indians from Bocas del Toro Province, Republic of Panama. Epilepsia. 1990 Nov-Dec;31(6):718–723. doi: 10.1111/j.1528-1157.1990.tb05512.x. [DOI] [PubMed] [Google Scholar]
- Hauser W. A., Kurland L. T. The epidemiology of epilepsy in Rochester, Minnesota, 1935 through 1967. Epilepsia. 1975 Mar;16(1):1–66. doi: 10.1111/j.1528-1157.1975.tb04721.x. [DOI] [PubMed] [Google Scholar]
- Heap B. J. Cerebral cysticercosis as a common cause of epilepsy in Gurkhas in Hong Kong. J R Army Med Corps. 1990 Oct;136(3):146–149. doi: 10.1136/jramc-136-03-04. [DOI] [PubMed] [Google Scholar]
- Hellgren U., Rombo L. Malaria prophylaxis and epilepsy. BMJ. 1988 Nov 12;297(6658):1267–1267. doi: 10.1136/bmj.297.6658.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jardim E., Takayanagui O. M. Epilepsia e donença de Chagas crônica. Arq Neuropsiquiatr. 1981 Mar;39(1):32–41. doi: 10.1590/s0004-282x1981000100004. [DOI] [PubMed] [Google Scholar]
- Jilek-Aall L., Jilek W., Miller J. R. Clinical and genetic aspects of seizure disorders prevalent in an isolated African population. Epilepsia. 1979 Dec;20(6):613–622. doi: 10.1111/j.1528-1157.1979.tb04845.x. [DOI] [PubMed] [Google Scholar]
- Joshi V., Katiyar B. C., Mohan P. K., Misra S., Shukla G. D. Profile of epilepsy in a developing country: a study of 1,000 patients based on the international classification. Epilepsia. 1977 Dec;18(4):549–554. doi: 10.1111/j.1528-1157.1977.tb05003.x. [DOI] [PubMed] [Google Scholar]
- Khare S. B., Rizvi A. G., Shukla O. P., Singh R. R., Perkash O., Misra V. D., Gupta J. P., Sethi P. K. Epidemic outbreak of neuro-ocular manifestations due to chronic BHC poisoning. J Assoc Physicians India. 1977 Mar;25(3):215–222. [PubMed] [Google Scholar]
- Koul R., Razdan S., Motta A. Prevalence and pattern of epilepsy (Lath/Mirgi/Laran) in rural Kashmir, India. Epilepsia. 1988 Mar-Apr;29(2):116–122. doi: 10.1111/j.1528-1157.1988.tb04406.x. [DOI] [PubMed] [Google Scholar]
- LORBER J. Long-term follow-up of 100 children who recovered from tuberculous meningitis. Pediatrics. 1961 Nov;28:778–791. [PubMed] [Google Scholar]
- Massey E. W., Schoenberg B. S. Mortality from epilepsy. International patterns and changes over time. Neuroepidemiology. 1985;4(2):65–70. doi: 10.1159/000110216. [DOI] [PubMed] [Google Scholar]
- Mathai K. V., Dunn D. P., Kurland L. T., Reeder F. A. Convulsive disorders in the Mariana Islands. Epilepsia. 1968 Jun;9(2):77–85. doi: 10.1111/j.1528-1157.1968.tb05130.x. [DOI] [PubMed] [Google Scholar]
- Matuja W. B. Aetiological factors in Tanzanian epileptics. East Afr Med J. 1989 May;66(5):343–348. [PubMed] [Google Scholar]
- Medina M. T., Rosas E., Rubio-Donnadieu F., Sotelo J. Neurocysticercosis as the main cause of late-onset epilepsy in Mexico. Arch Intern Med. 1990 Feb;150(2):325–327. [PubMed] [Google Scholar]
- Mirando E. H., Ranasinghe L. Lead encephalopathy in children. Uncommon clinical aspects. Med J Aust. 1970 Nov 21;2(21):966–968. doi: 10.5694/j.1326-5377.1970.tb63289.x. [DOI] [PubMed] [Google Scholar]
- Monath T. P. Japanese encephalitis--a plague of the Orient. N Engl J Med. 1988 Sep 8;319(10):641–643. doi: 10.1056/NEJM198809083191009. [DOI] [PubMed] [Google Scholar]
- Navia B. A., Petito C. K., Gold J. W., Cho E. S., Jordan B. D., Price R. W. Cerebral toxoplasmosis complicating the acquired immune deficiency syndrome: clinical and neuropathological findings in 27 patients. Ann Neurol. 1986 Mar;19(3):224–238. doi: 10.1002/ana.410190303. [DOI] [PubMed] [Google Scholar]
- Ogunniyi A., Osuntokun B. O., Bademosi O., Adeuja A. O., Schoenberg B. S. Risk factors for epilepsy: case-control study in Nigerians. Epilepsia. 1987 May-Jun;28(3):280–285. doi: 10.1111/j.1528-1157.1987.tb04219.x. [DOI] [PubMed] [Google Scholar]
- Oh S. J. Cerebral paragonimiasis. J Neurol Sci. 1969 Jan-Feb;8(1):27–48. doi: 10.1016/0022-510x(69)90039-2. [DOI] [PubMed] [Google Scholar]
- Osuntokun B. O., Adeuja A. O., Nottidge V. A., Bademosi O., Olumide A., Ige O., Yaria F., Bolis C. L., Schoenberg B. S. Prevalence of the epilepsies in Nigerian Africans: a community-based study. Epilepsia. 1987 May-Jun;28(3):272–279. doi: 10.1111/j.1528-1157.1987.tb04218.x. [DOI] [PubMed] [Google Scholar]
- Osuntokun B. O., Bademosi O., Familusi J. B., Oke F. Electroencephalographic correlates of epilepsy in Nigerian children. Dev Med Child Neurol. 1974 Oct;16(5):659–663. doi: 10.1111/j.1469-8749.1974.tb04185.x. [DOI] [PubMed] [Google Scholar]
- Pomeroy S. L., Holmes S. J., Dodge P. R., Feigin R. D. Seizures and other neurologic sequelae of bacterial meningitis in children. N Engl J Med. 1990 Dec 13;323(24):1651–1657. doi: 10.1056/NEJM199012133232402. [DOI] [PubMed] [Google Scholar]
- Poneprasert B. Japanese encephalitis in children in northern Thailand. Southeast Asian J Trop Med Public Health. 1989 Dec;20(4):599–603. [PubMed] [Google Scholar]
- Senanayake N. Epilepsy control in a developing country--the challenge of tomorrow. Ceylon Med J. 1987 Dec;32(4):181–199. [PubMed] [Google Scholar]
- Senga P., Mayanda H. F., Nzingoula S. Profil des convulsions du nourrisson et du jeune enfant à Brazzaville (Congo). Ann Pediatr (Paris) 1985 May;32(5):477–480. [PubMed] [Google Scholar]
- Simanjuntak G. M., Margono S. S., Schlan R., Harjono C., Rasidi R., Sutopo B. An investigation on taeniasis and cysticercosis in Bali. Southeast Asian J Trop Med Public Health. 1977 Dec;8(4):494–497. [PubMed] [Google Scholar]
- Sotelo J., Guerrero V., Rubio F. Neurocysticercosis: a new classification based on active and inactive forms. A study of 753 cases. Arch Intern Med. 1985 Mar;145(3):442–445. [PubMed] [Google Scholar]
- Stanhope J. M., Brody J. A., Brink E. Convulsions among the Chamorro people of Guam, Mariana islands. I. Seizure disorders. Am J Epidemiol. 1972 Mar;95(3):292–298. doi: 10.1093/oxfordjournals.aje.a121396. [DOI] [PubMed] [Google Scholar]
- Subianto D. B., Tumada L. R., Margono S. S. Burns and epileptic fits associated with cysticercosis in mountain people of Irian Jaya. Trop Geogr Med. 1978 Sep;30(3):275–278. [PubMed] [Google Scholar]
- Tekle-Haimanot R., Forsgren L., Abebe M., Gebre-Mariam A., Heijbel J., Holmgren G., Ekstedt J. Clinical and electroencephalographic characteristics of epilepsy in rural Ethiopia: a community-based study. Epilepsy Res. 1990 Dec;7(3):230–239. doi: 10.1016/0920-1211(90)90020-v. [DOI] [PubMed] [Google Scholar]
- Telang B. V., Hettiaratchi E. S. Patterns of epilepsy in Kenya--a clinical analysis of 115 cases. East Afr Med J. 1981 Jun;58(6):437–444. [PubMed] [Google Scholar]
- Teoh R., Humphries M. J., O'Mahony G. Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: a report of 10 patients and review of the literature. Q J Med. 1987 May;63(241):449–460. [PubMed] [Google Scholar]
- Veliath A. J., Ratnakar C., Thakur L. C. Cysticercosis in South India. J Trop Med Hyg. 1985 Feb;88(1):25–29. [PubMed] [Google Scholar]
- Vyravanathan S., Senanayake N. Tuberculosis presenting with hemiplegia. J Trop Med Hyg. 1979 Feb;82(2):38–40. [PubMed] [Google Scholar]
- Wadia R. S., Makhale C. N., Kelkar A. V., Grant K. B. Focal epilepsy in India with special reference to lesions showing ring or disc-like enhancement on contrast computed tomography. J Neurol Neurosurg Psychiatry. 1987 Oct;50(10):1298–1301. doi: 10.1136/jnnp.50.10.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]


