Abstract
In order to assess the risk and predictors of mefloquine resistance we monitored a cohort of 113 patients in eastern Thailand who had been treated for uncomplicated falciparum malaria with a single dose of 15 mg/kg of the drug and followed up for 42 days. The overall treatment failure rate at day 42 was 59.1% (95% confidence interval (CI) = 50%, 68%) with only 2.7% of the patients being lost to follow-up. There were 6.4% RIII, 20.9% RII, 31.8% RI, and 40.9% sensitive responses, based on a modified WHO classification. A low haemoglobin level on the day of treatment and diarrhoea during the first two days after treatment were independent predictors of treatment failure. These findings remained statistically significant in a Cox proportional hazards model, after controlling for other baseline characteristics and adverse effects. Although a history of digestive disorders prior to treatment was associated with diarrhoea on day 2 (P = 0.024), it was in itself not a predictor of treatment failure (adjusted hazard ratio = 1.16; 95% CI = 0.35, 2.14). A total of 60 patients with an R response were hospitalized for 7 days to receive supervised treatment with quinine-tetracycline. Only three had a positive thick smear for asexual forms of Plasmodium falciparum 14 days later, and quinine-tetracycline therefore remains a good alternative treatment for mefloquine-resistant falciparum malaria.
Full text
PDF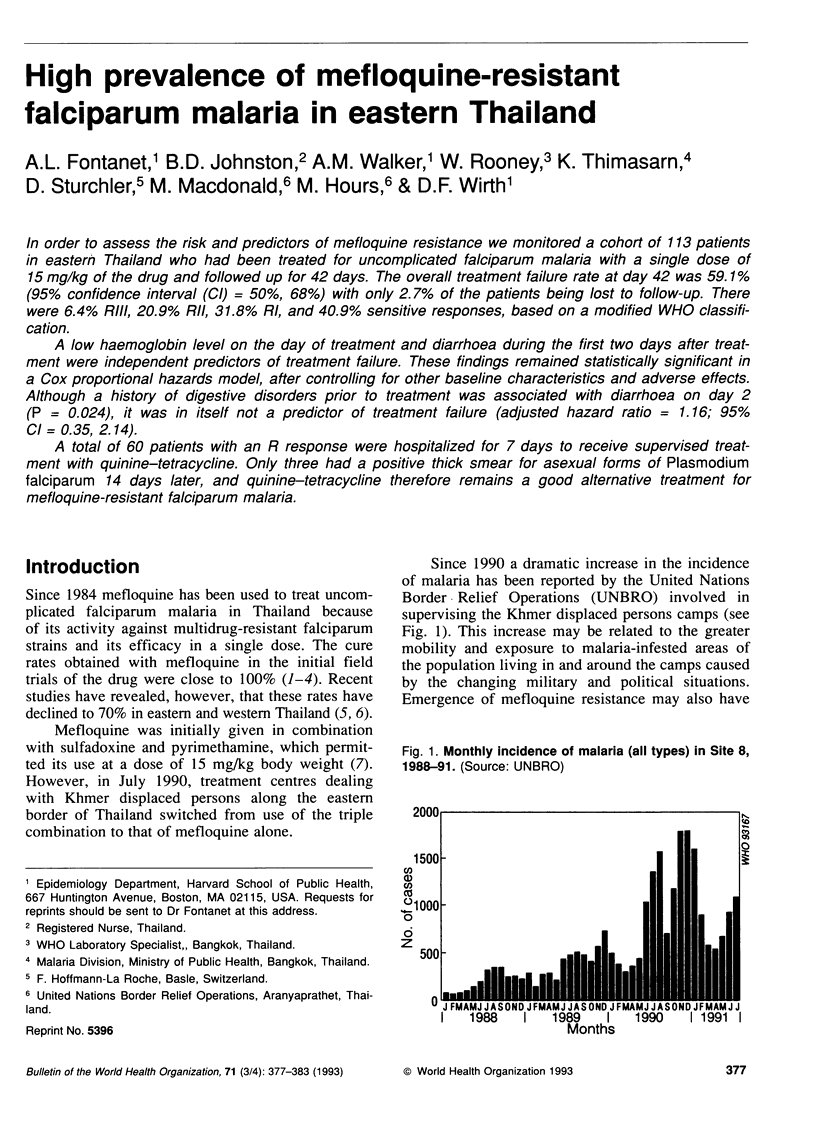





Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boudreau E. F., Fleckenstein L., Pang L. W., Childs G. E., Schroeder A. C., Ratnaratorn B., Phintuyothin P. Mefloquine kinetics in cured and recrudescent patients with acute falciparum malaria and in healthy volunteers. Clin Pharmacol Ther. 1990 Oct;48(4):399–409. doi: 10.1038/clpt.1990.168. [DOI] [PubMed] [Google Scholar]
- Chevli R., Fitch C. D. The antimalarial drug mefloquine binds to membrane phospholipids. Antimicrob Agents Chemother. 1982 Apr;21(4):581–586. doi: 10.1128/aac.21.4.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs G. E., Bourdeau E. F., Wimonwattratee T., Pang L., Milhous W. K. In vitro and clinical correlates of mefloquine resistance of Plasmodium falciparum in eastern Thailand. Am J Trop Med Hyg. 1991 May;44(5):553–559. doi: 10.4269/ajtmh.1991.44.553. [DOI] [PubMed] [Google Scholar]
- Doberstyn E. B., Phintuyothin P., Noeypatimanondh S., Teerakiartkamjorn C. Single-dose therapy of falciparum malaria with mefloquine or pyrimethamine-sulfadoxine. Bull World Health Organ. 1979;57(2):275–279. [PMC free article] [PubMed] [Google Scholar]
- Harinasuta T., Bunnag D., Wernsdorfer W. H. A phase II clinical trial of mefloquine in patients with chloroquine-resistant falciparum malaria in Thailand. Bull World Health Organ. 1983;61(2):299–305. [PMC free article] [PubMed] [Google Scholar]
- Malikul S. The current situation of the anti-malaria programme in Thailand. Southeast Asian J Trop Med Public Health. 1988 Sep;19(3):355–359. [PubMed] [Google Scholar]
- Meek S. R., Doberstyn E. B., Gaüzère B. A., Thanapanich C., Nordlander E., Phuphaisan S. Treatment of falciparum malaria with quinne and tetracycline or combined mefloquine/sulfadoxine/pyrimethamine on the Thai-Kampuchean border. Am J Trop Med Hyg. 1986 Mar;35(2):246–250. doi: 10.4269/ajtmh.1986.35.246. [DOI] [PubMed] [Google Scholar]
- Nosten F., Imvithaya S., Vincenti M., Delmas G., Lebihan G., Hausler B., White N. Malaria on the Thai-Burmese border: treatment of 5192 patients with mefloquine-sulfadoxine-pyrimethamine. Bull World Health Organ. 1987;65(6):891–896. [PMC free article] [PubMed] [Google Scholar]
- Nosten F., ter Kuile F., Chongsuphajaisiddhi T., Luxemburger C., Webster H. K., Edstein M., Phaipun L., Thew K. L., White N. J. Mefloquine-resistant falciparum malaria on the Thai-Burmese border. Lancet. 1991 May 11;337(8750):1140–1143. doi: 10.1016/0140-6736(91)92798-7. [DOI] [PubMed] [Google Scholar]
- Peters W. The problem of drug resistance in malaria. Parasitology. 1985 Apr;90(Pt 4):705–715. doi: 10.1017/s003118200005232x. [DOI] [PubMed] [Google Scholar]
- Slutsker L. M., Khoromana C. O., Payne D., Allen C. R., Wirima J. J., Heymann D. L., Patchen L., Steketee R. W. Mefloquine therapy for Plasmodium falciparum malaria in children under 5 years of age in Malawi: in vivo/in vitro efficacy and correlation of drug concentration with parasitological outcome. Bull World Health Organ. 1990;68(1):53–59. [PMC free article] [PubMed] [Google Scholar]



