Abstract
A survey was undertaken between December 1991 and February 1992 to assess the knowledge, attitudes, and practices with respect to malaria of 300 women from six randomly selected rural communities in central Ethiopia. A total of 85% were able to recognize one or more of the common symptoms of the disease; however, the modes of transmission were generally misunderstood and only 23% believed that transmission could be prevented. More women preferred to obtain antimalarials from government clinics rather than from private drug shops, mission clinics, unofficial suppliers of injections, open markets, or from leftover sources. Under-5-year-olds were identified as the most malaria-vulnerable group and given priority for treatment; severity of illness was the principal determinant in seeking treatment. Decisions about treatment were generally made jointly by both parents. Knowledge about the transmissibility of malaria decreased with increasing distance from a health unit (odds ratio: 0.48; 95% confidence interval: 0.27, 0.86). A logistic regression analysis indicated that literacy and village were the most important variables associated with knowledge about preventing malaria.
Full text
PDF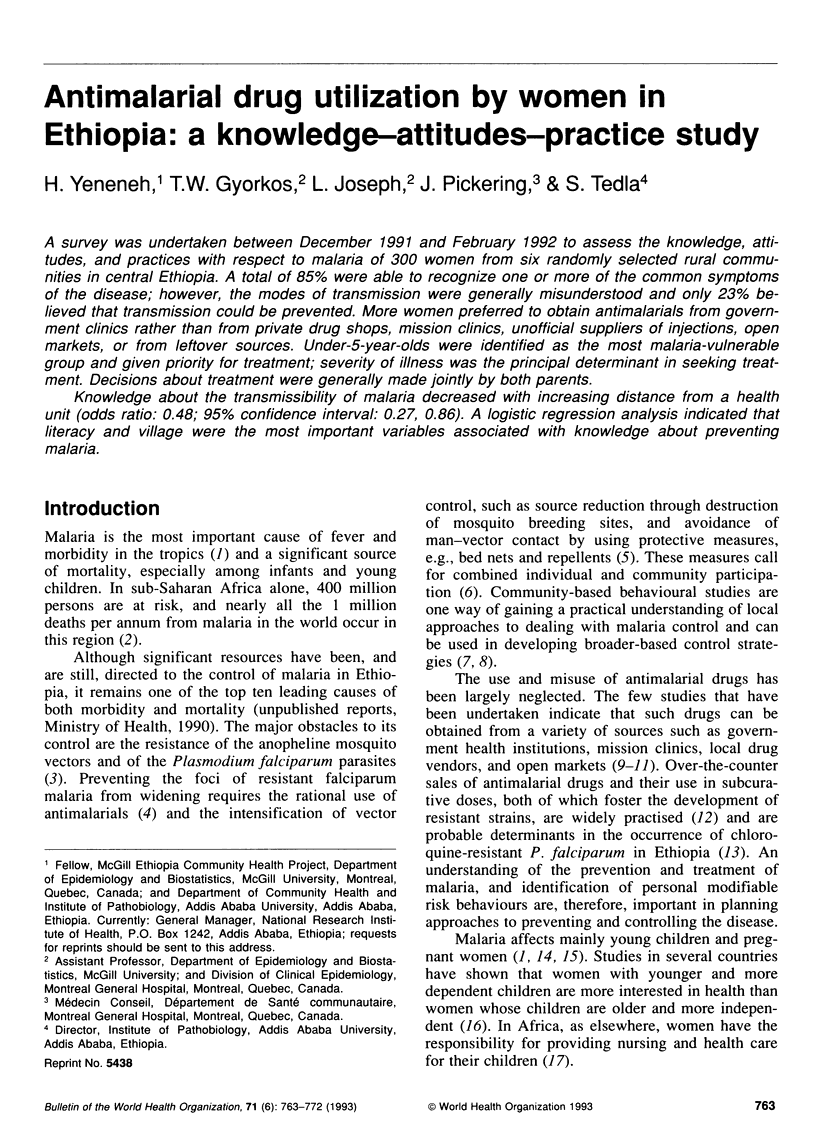



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belcher D. W., Nicholas D. D., Blumenfeld S. N. Factors influencing utilization of a malaria prophylaxis programme in Ghana. Soc Sci Med. 1975 Apr-May;9(4-5):241–248. doi: 10.1016/0037-7856(75)90029-3. [DOI] [PubMed] [Google Scholar]
- Björkman A., Phillips-Howard P. A. Drug-resistant malaria: mechanisms of development and inferences for malaria control. Trans R Soc Trop Med Hyg. 1990 May-Jun;84(3):323–324. doi: 10.1016/0035-9203(90)90302-u. [DOI] [PubMed] [Google Scholar]
- Glik D. C., Ward W. B., Gordon A., Haba F. Malaria treatment practices among mothers in Guinea. J Health Soc Behav. 1989 Dec;30(4):421–435. [PubMed] [Google Scholar]
- Greenberg A. E., Ntumbanzondo M., Ntula N., Mawa L., Howell J., Davachi F. Hospital-based surveillance of malaria-related paediatric morbidity and mortality in Kinshasa, Zaire. Bull World Health Organ. 1989;67(2):189–196. [PMC free article] [PubMed] [Google Scholar]
- Hibbard J. H., Pope C. R. Women's roles, interest in health and health behavior. Women Health. 1987;12(2):67–84. doi: 10.1300/J013v12n02_05. [DOI] [PubMed] [Google Scholar]
- Kaseje D. C., Spencer H. C. The Saradidi, Kenya, rural health development programme. Ann Trop Med Parasitol. 1987 Apr;81 (Suppl 1):1–12. doi: 10.1080/00034983.1987.11812184. [DOI] [PubMed] [Google Scholar]
- Kloos H., Etea A., Degefa A., Aga H., Solomon B., Abera K., Abegaz A., Belemo G. Illness and health behaviour in Addis Ababa and rural central Ethiopia. Soc Sci Med. 1987;25(9):1003–1019. doi: 10.1016/0277-9536(87)90005-0. [DOI] [PubMed] [Google Scholar]
- Laing R. O. Rational drug use: an unsolved problem. Trop Doct. 1990 Jul;20(3):101–103. doi: 10.1177/004947559002000303. [DOI] [PubMed] [Google Scholar]
- MacCormack C. P., Lwihula G. Failure to participate in a malaria chemosuppression programme: North Mara, Tanzania. J Trop Med Hyg. 1983 Jun;86(3):99–107. [PubMed] [Google Scholar]
- Mburu F. M., Spencer H. C., Kaseje D. C. Changes in sources of treatment occurring after inception of a community-based malaria control programme in Saradidi, Kenya. Ann Trop Med Parasitol. 1987 Apr;81 (Suppl 1):105–110. doi: 10.1080/00034983.1987.11812195. [DOI] [PubMed] [Google Scholar]
- Nevill C. G. Malaria in Sub-Saharan Africa. Soc Sci Med. 1990;31(6):667–669. doi: 10.1016/0277-9536(90)90248-q. [DOI] [PubMed] [Google Scholar]
- Ongore D., Kamunvi F., Knight R., Minawa A. A study of knowledge, attitudes and practices (KAP) of a rural community on malaria and the mosquito vector. East Afr Med J. 1989 Feb;66(2):79–90. [PubMed] [Google Scholar]
- Raikes A. Women's health in east Africa. Soc Sci Med. 1989;28(5):447–459. doi: 10.1016/0277-9536(89)90100-7. [DOI] [PubMed] [Google Scholar]
- Ruebush T. K., 2nd, Weller S. C., Klein R. E. Knowledge and beliefs about malaria on the Pacific coastal plain of Guatemala. Am J Trop Med Hyg. 1992 Apr;46(4):451–459. doi: 10.4269/ajtmh.1992.46.451. [DOI] [PubMed] [Google Scholar]
- Spencer H. C., Kaseje D. C., Collins W. E., Shehata M. G., Turner A., Stanfill P. S., Huong A. Y., Roberts J. M., Villinski M., Koech D. K. Community-based malaria control in Saradidi, Kenya: description of the programme and impact on parasitaemia rates and antimalarial antibodies. Ann Trop Med Parasitol. 1987 Apr;81 (Suppl 1):13–23. doi: 10.1080/00034983.1987.11812185. [DOI] [PubMed] [Google Scholar]
- Teklehaimanot A. Chloroquine-resistant Plasmodium falciparum malaria in Ethiopia. Lancet. 1986 Jul 19;2(8499):127–129. doi: 10.1016/s0140-6736(86)91945-8. [DOI] [PubMed] [Google Scholar]
- Wernsdorfer W. H., Kouznetsov R. L. Drug-resistant malaria--occurrence, control, and surveillance. Bull World Health Organ. 1980;58(3):341–352. [PMC free article] [PubMed] [Google Scholar]



