Abstract
The virulence of influenza virus is a multigenic trait. One determinant of virulence is the multifunctional NS1 protein that functions in several ways to defeat the cellular innate immune response. Recent large-scale genome sequence analysis of avian influenza virus isolates indicated that four C-terminal residues of the NS1 protein is a PDZ ligand domain of the X-S/T-X-V type and it was speculated that it may represent a virulence determinant. To test this hypothesis, by using mice as a model system, the four C-terminal amino acid residues of a number of influenza virus strains were engineered into the A/WSN/33 virus NS1 protein by reverse genetics and the pathogenicity of the viruses determined. Viruses containing NS1 sequences from the 1918 H1N1 and H5N1 highly pathogenic avian influenza (HPAI) viruses demonstrated increased virulence in infected mice compared with wt A/WSN/33 virus, as characterized by rapid loss of body weight, decreased survival time, and decreased mean lethal dose. Histopathological analysis of infected mouse lung tissues demonstrated severe alveolitis, hemorrhaging, and spread of the virus throughout the entire lung. The increase in pathogenicity was not caused by the overproduction of IFN, suggesting the NS1 protein C terminus may interact with PDZ-binding protein(s) and modulate pathogenicity through alternative mechanisms.
Keywords: mouse model for influenza, PDZ domains, PDZ ligand, influenza reverse genetics, H5N1 influenza
The virulence of influenza virus strains is a multigenic trait (reviewed in ref. 1). The high virulence and pathogenesis of strains such as the H5N1 high pathogenic avian influenza (HPAI) and 1918 H1N1 viruses has been shown to be caused by the specific sequence of viral proteins (2, 3) including the external surface glycoproteins, hemagglutinin (HA) and neuraminidase (NA) (4–7), the three internal polymerase proteins (5, 6, 8, 9), and the two nonstructural proteins PB1-F2 (10) and NS1 (11).
The NS1 protein has been reported to have multiple functions including controlling the temporal synthesis of viral-specific mRNA and viral genomic RNAs (12, 13) and interacting with the cellular protein phosphatidylinositol-3-kinase (PI3-kinase) (14–16), which may cause a delay in virus-induced apoptosis (17). However, the majority of previous work has focused on the ability of NS1 to circumvent the host cell antiviral responses. This is achieved in a number of ways, including blocking 2′-5′-oligoadenylate synthetase (2′-5′-OAS) activation of RNaseL (18), limiting the induction of IFN-β by preventing the activation of transcription factors (19–21), interaction with the cellular protein retinoic acid-inducible gene product I (RIG-I) (22–24), blocking host cell mRNA polyadenylation (25, 26), and blocking the PKR-mediated inhibition of protein synthesis (13, 27). It has also been shown that NS1 prevents the maturation of human primary dendritic cells, thereby limiting host T cell activation (28).
The NS1 protein of H5N1 HPAI and the 1918 H1N1 viruses has been implicated in their virulence (11, 29, 30). When the NS1 protein of the 1918 virus was introduced into a less virulent human strain it was shown to be more efficient at blocking a number of IFN-regulated genes than its parental wild-type strain (11).
Large-scale sequence analysis of avian influenza viruses indicated that the C-terminal four residues of the NS1 protein is a potential PDZ domain ligand (PL) of the X-S/T-X-V type (31). PDZ domains are protein–protein recognition modules that organize diverse cell-signaling assemblies (32). They specifically recognize short C-terminal peptide motifs of 4–5 aa, which can be used in combination to bind to an array of target proteins or to oligomerize into branched structures. PDZ domain-containing proteins play important roles in the transport, localization, and assembly of supramolecular signaling complexes, organizing cell polarity, receptors, and downstream effectors. Of the human influenza viruses, 90% have an NS1 protein with a C-terminal four-residue PL sequence of RSKV or RSEV (31). However, 7% of human viruses consist of H5N1 isolates, responsible for the recent high-mortality outbreaks, which are of avian origin and therefore contain avian-like NS1 C-terminal PL residues of ESEV or EPEV. It was shown that NS1 proteins of avian viruses bind to ≈30 known human PDZ domain-containing proteins, whereas for human NS1 proteins binding to PDZ domain-containing proteins was not observed (31). It was speculated that this binding might interfere with cellular signaling.
We have identified the extreme C terminus of the NS1 protein as a virulence determinant by the introduction of C-terminal amino acids from the NS1 protein of a number of influenza viruses into that of A/WSN/33 by using reverse genetics. Recombinant viruses containing C-terminal NS1 sequences from the 1918 H1N1 and H5N1 HPAI viruses, when used to infect mice, show increased virulence and pathogenesis, and this increased pathogenicity is independent of the IFN-antagonistic properties of NS1.
Results
The Generation and Characterization of Influenza Virus Mutants Containing Altered NS1 C Termini.
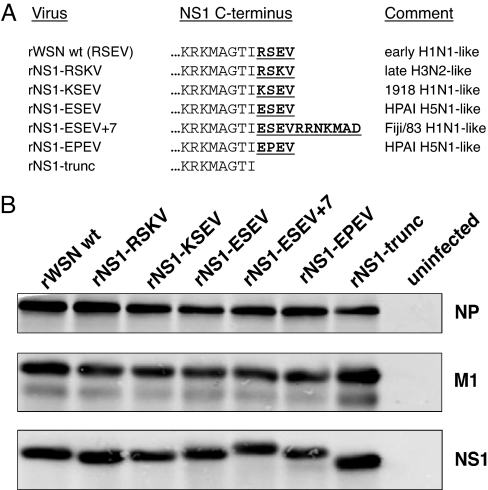
To investigate whether the PL motif affects pathogenicity in an animal model system, mutant viruses were created by reverse genetics by using the A/WSN/33 genetic backbone (Fig. 1A). The A/WSN/33 strain was selected because it is a well characterized mouse-adapted strain lethal for mice; therefore, changes in virulence could be monitored. For the early human H1N1 strains the NS1 protein was 230 aa in length, but in the 1940s nucleotide changes resulted in extension of the protein to 237 aa and the C-terminal PL motif was lost. This seven amino acid extension was retained (with a few exceptions) in human H2N2, H3N2, and H1N1 viruses until the 1980s when both the cocirculating H1N1 and H3N2 viruses reverted back to encoding a 230-aa NS1 protein, and the PL motif was regained. The H5N1 HPAI viruses isolated from humans after 1997 also encode a 230-aa protein. However, the four amino acid PL sequence differs depending on the virus isolate.
Fig. 1.
The generation of mutant viruses. (A) Mutant (rNS1) influenza A viruses were generated by reverse genetics in which mutations were introduced into the C terminus of the A/WSN/33 virus NS1 protein. The C-terminal four amino acids (RSEV) were mutated to introduce sequences from a number of influenza virus strains. Mutations are underlined. Early H1N1, influenza viruses isolated before the 1950s; Late H3N2, H3N2 influenza viruses isolated after 1990; Fiji/83 H1N1-like, the only naturally occurring H1N1 strain isolated containing glutamic acid at residue 227 of a 237-aa NS1 protein (A/Fiji/83). rNS1-trunc contains a four amino acid truncation. Because NS1 and NS2/NEP use overlapping reading frames, the mutant viruses also contained the following amino acid changes in NS2/NEP: rNS1-RSKV, no mutations; rNS1-KSEV, G70S mutation; rNS1-ESEV, G70S mutation; rNS1-ESEV + 7, G70S and F73L mutations; rNS1-EPEV, G70S mutation; rNS1-trunc, L69F and G70S mutations. As argued in Discussion, it seems extraordinarily unlikely that these changes in NS2/NEP are responsible for the observed phenotypes. (B) The expression of viral proteins from infected MDCK cells.
The rNS1-KSEV virus contained the NS1 four C-terminal residues from the 1918 H1N1 virus, whereas the rNS1-ESEV and rNS1-EPEV viruses contained the NS1 C-terminal sequences from H5N1 HPAI viruses. The rNS1-RSKV virus contained the NS1 C-terminal sequence from those H3N2 viruses isolated after the 1980s (termed late H3N2 viruses). The rNS1-ESEV + 7 virus contained not only the ESEV “avian-like” sequence but also the seven amino acid C-terminal extension found on human strains isolated between the 1940s and 1980s. The rNS1-trunc virus does not exist naturally, but it encodes an NS1 protein with a four amino acid truncation at the C terminus and therefore lacks a potential PL motif.
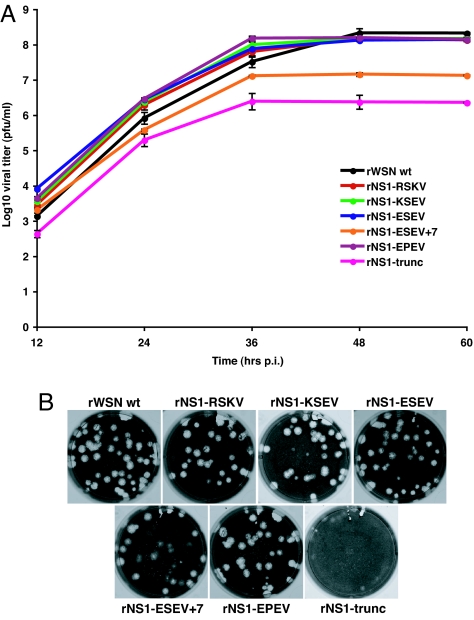
Madin–Darby canine kidney (MDCK) cells infected with the recombinant viruses showed similar levels of NP, M1, and NS1 protein expression (Fig. 1B). Immunofluorescent staining of the NS1 protein in virus-infected MDCK cells showed a nuclear and nucleolar localization, with no apparent differences among the viruses [supporting information (SI) Fig. 5]. Analysis of the virus growth kinetics in MDCK cells showed that four of the mutants (rNS1-RSKV, rNS1-KSEV, rNS1-ESEV, and rNS1-EPEV) had wild-type-like growth kinetics, and two of the viruses, rNS1-ESEV + 7 and rNS1-trunc, displayed an attenuated phenotype (Fig. 2A). These growth characteristics were mirrored in the phenotype of the plaques formed by the viruses, with four mutants (rNS1-RSKV, rNS1-KSEV, rNS1-ESEV, and rNS1-EPEV) producing wt-like plaques. Mutant virus rNS1-ESEV + 7 produced turbid plaques and rNS1-trunc virus produced pinpoint plaques (Fig. 2B) that required immunostaining of the cells to obtain an accurate virus titer.
Fig. 2.
Viral growth kinetics in MDCK cells. (A) MDCK cells were infected with wt and mutant rNS1 viruses at an MOI of 0.001, supernatants were harvested every 12 h, and samples were titrated by plaque assay in MDCK cells. Results represent the average of three independent experiments. (B) Plaque phenotype of wt and mutant rNS1 influenza viruses in MDCK cells. After titration of viruses cells were fixed in 1% glutaraldehyde and stained with napthylene blue.
In Vivo Characterization of Recombinant Viruses in the Mouse Model.
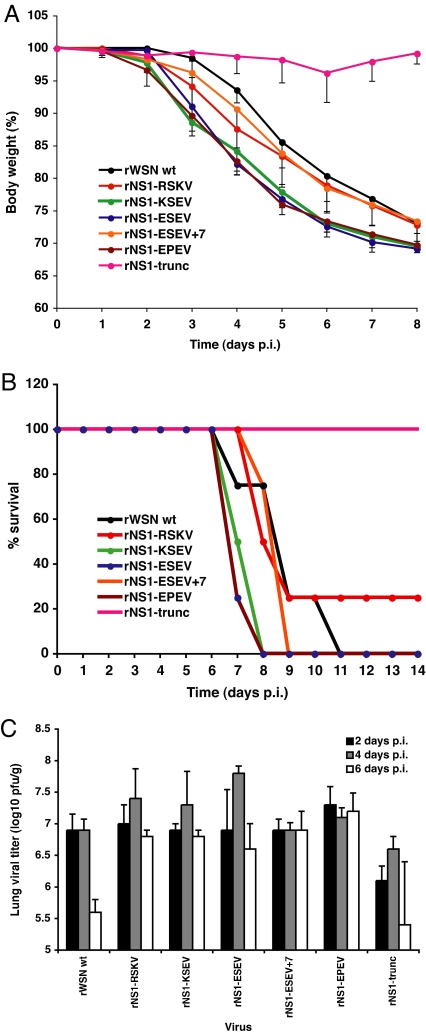
Five-week-old BALB/c mice (groups of four) were inoculated intranasally with 103, 104, or 105 plaque-forming units (pfu) of the recombinant viruses. The body weight of each mouse was measured daily until 14 days postinfection (p.i.). When body weight was reduced to 70% of the starting weight, mice were presumed to be dying and they were euthanized. All mice infected with 105 pfu of wt or any of the mutant viruses were euthanized by day 8 p.i. (data not shown). For mice infected with 104 pfu virus, all mutant viruses, except the rNS1-trunc virus, caused more significant weight loss than wt virus (P < 0.0001). The two viruses containing the avian-like NS1 C-terminal sequences (ESEV and EPEV) caused the most rapid body weight loss (Fig. 3A), and the virus with the 1918 H1N1 NS1 C terminus (rNS1-KSEV) caused rapid weight loss. Viruses containing the H3N2-like C-terminal NS1 residues (rNS1-RSKV) and the virus with the seven amino acid extension at the NS1 C terminus (rNS1-ESEV + 7) showed slightly greater weight loss than wt virus over the first 8 days p.i. The rNS1-trunc virus that lacks the NS1 protein C-terminal residues caused virtually no weight loss. When the data were plotted as a survival curve, all of the viruses except the rNS1-trunc and rNS1-RSKV viruses led to reduced survival compared with wt virus, with the rNS1-ESEV, rNS1-EPEV, and rNS1-KSEV viruses resulting in 0% survival by 8 days p.i. (Fig. 3B). When mice were inoculated with 103 pfu of the recombinant viruses all of the mutant viruses, except rNS1-trunc virus, caused significant body weight loss (P < 0.0001) that was greater than wt virus (SI Fig. 6A). However, although rNS1-ESEV and rNS1-EPEV viruses resulted in the greatest weight loss, rNS1-KSEV at an inoculum of 103 pfu did not cause as extensive weight loss as when a 104 pfu inoculum was used relative to other viruses.
Fig. 3.
Mouse experiments. Five-week-old BALB/c mice were inoculated intranasally with 104 pfu of wt or mutant rNS1 influenza viruses, with four mice per group. (A) The body weight of mice infected was measured up to 14 days p.i. Mice were euthanized after the loss of 30% of their initial body weight. (B) The data expressed as the percentage survival of mice infected with 104 pfu. (C) The titers of infectious wt or mutant rNS1 influenza virus isolated from homogenized lung tissues 2, 4, or 6 days p.i. Results represent the average infectious titers from the lungs of four infected mice per group.
The mean lethal dose (MLD50) of the recombinant viruses were determined after inoculation of groups of four mice with 102, 103, 104, and 105 pfu. As shown in Table 1, the rNS1-RSKV, rNS1-KSEV, and rNS1-ESEV + 7 viruses had a MLD50 similar to that of wt virus, whereas that of rNS1-trunc was 14-fold higher than wt. Importantly, the MLD50 of the rNS1-ESEV and rNS1-EPEV viruses were 10% and 14% that of wt, respectively.
Table 1.
Mouse lethal dose (MLD50) in pfu for wt and mutant influenza viruses
| Virus | MLD50, pfu |
|---|---|
| rWSN wt | 5 × 103 |
| rNS1-RSKV | 7 ×103 |
| rNS1-KSEV | 2 × 103 |
| rNS1-ESEV | 5 × 102 |
| rNS1-ESEV + 7 | 2 × 103 |
| rNS1-EPEV | 7 × 102 |
| rNS1-trunc | 7 × 104 |
Groups of four mice per dose were inoculated intranasally with 102, 103, 104, or 105 pfu per mouse. Mice that lost 30% body weight were assumed to be near death and were euthanized. Survival of mice was monitored for 14 days after inoculation.
The titers of infectious virus isolated from infected mouse lung tissue were found to be not significantly different among the recombinant viruses. For each virus the titer peaked at 4 days p.i. (Fig. 3C). However, there was a pronounced difference in the ability of the mice to clear the viruses by 6 days p.i. Lung titers of both wt and rNS1-trunc viruses were significantly reduced by 6 days p.i. compared with those at 2 days p.i. However, all of the viruses that caused greater weight loss than wt virus showed lung titers at 6 days p.i. that were virtually indistinguishable from those observed at 2 days p.i.
Histological Analysis of Infected Mouse Lung Tissues.
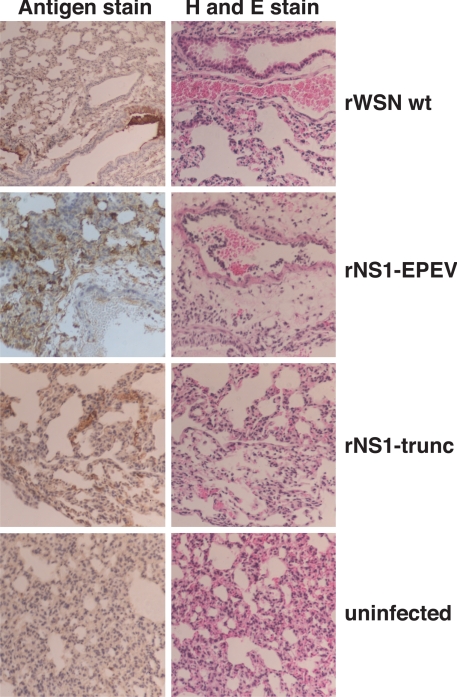
To examine the pathology of the lungs of infected mice lungs were isolated four days p.i., serial sectioned and stained with hematoxylin and eosin (H&E) or stained for viral antigen. For wt virus, antigen staining showed the presence of virus-infected cells in localized areas of the lung and H&E staining indicated moderate to severe alveolitis (Fig. 4). The rNS1-RSKV, rNS1-ESEV + 7, and rNS1-trunc virus-infected tissues showed a very similar pattern of antigen staining to those of wt virus, but the H&E staining showed only mild alveolitis. H&E staining of rNS1-ESEV, rNS1-EPEV, and rNS1-KSEV virus-infected tissues showed severe alveolitis and hemorrhage, and antigen staining demonstrated a significant increase in viral spread compared with wt virus-infected tissues with the presence of virus-infected cells throughout the entire lung (Fig. 4). This increase in viral spread may explain the increased virulence of the viruses containing the avian-like and “1918-like” NS1 C-terminal four amino acid PL sequences.
Fig. 4.
Histopathological analysis of infected mouse lung tissue. Wt or mutant rNS1 influenza virus-infected mouse lung samples were preserved in formalin, embedded in paraffin, and sectioned into serial 4-μm sections. Tissues were stained with H&E or antigen-stained by using a goat anti-Udorn polyclonal antiserum. Images were captured at ×20 magnification.
Increased Virulence of Recombinant Viruses Is Not Caused by an Increase in IFN Production.
The increased virulence of the rNS1 viruses could be caused by changes in the host cell IFN response. To examine this possibility, A549 cells were either infected with the rNS1 viruses or treated with IFN-β for 6 h, followed by infection with an IFN-sensitive reporter virus, the Newcastle disease virus that expresses green fluorescent protein (NDV-GFP) (33). IFN treatment of cells prevented GFP expression in NDV-GFP-infected cells, whereas in cells infected with the rNS1 viruses high levels of GFP were expressed by 24 h p.i. (SI Fig. 7). These data suggest that high levels of IFN were not produced in the rNS1 virus-infected cells. To extend this observation, the abundance of IFN-α mRNA in recombinant virus-infected MDCK cells was determined by using quantitative PCR (SI Fig. 8). As a test, a number of control viruses were used to validate the assay. rUd-NS1-rna is a mutant influenza virus that contains an R38A mutation that ablates the dsRNA-binding properties of NS1 and reduces its IFN antagonistic property in virus-infected cells (28). As shown in SI Fig. 8, rUd-NS1-rna caused a 4-fold increase in IFN-α mRNA levels over rWSN wt virus and a 12-fold increase over its relative rUd wt. PIV5 VdelC is a mutant paramyxovirus known to induce IFN-β production (34). As shown in SI Fig. 8, in PIV5 VdelC-infected cells, a 10-fold higher level of IFN-α mRNA was found compared with wt PIV5 virus. Sendai virus is a known inducer of IFN and it was found that in Sendai virus-infected cells IFN-α mRNA levels were more than 2-fold higher than in rWSN wt-infected cells (SI Fig. 8). However, IFN-α mRNA levels in cells infected with the rNS1 influenza viruses were equivalent to or reduced compared with those in wt virus-infected cells (SI Fig. 8). When IFN-β mRNA levels were measured by quantitative PCR, similar data were obtained (data not shown). Thus, the available data indicate that the mutant rNS1 viruses do not show increased pathogenicity as a result of changes in the IFN response.
Discussion
Several molecular determinants of influenza virus pathogenicity have been identified, including the nature of the residues found at the HA cleavage-activation site, the residues governing receptor specificity of HA (α2,3 or α2,6 sialic acid), the ability of NA to bind plasminogen, specific amino acid changes in PB2 that alter the rate of RNA synthesis, the presence of the PB1-F2 ORF and the ability of PB1-F2 to induce apoptosis, and the differing ability of NS1 proteins to counteract the IFN system (reviewed in ref. 1).
We tested the hypothesis that the nature of the four C-terminal residues of the NS1 protein derived from different influenza virus strains would affect pathogenicity based on the prior observation that these residues constituted a PL sequence (31). By using the mouse-adapted A/WSN/33 strain of influenza virus as a genetic background, the C-terminal four residues of NS1 were altered by using reverse genetics to represent the sequences found at the C terminus of various human influenza virus isolates. The caveat has to be added that all of the rNS1 viruses, except rNS1-RSKV, contained a G70S mutation in the NS2/NEP protein. In addition, rNS1-ESEV + 7 gained a second mutation, F73L, and rNS1-trunc, a second mutation of L69F. A priori it seems most unlikely that the G70S mutation was responsible for the increased virulence, because the same mutation is found in the attenuated viruses rNS1-ESEV + 7 and rNS1-trunc. Furthermore, for this mutation to affect the data obtained, it would be necessary to argue that the second mutation in rNS1-ESEV + 7 and rNS1-trunc was dominant over G70S. Last, because the function of NS2/NEP is known to be involved in the export of assembled ribonucleoprotein complexes out of the nucleus (35, 36), and all of the viruses except rNS1-ESEV + 7 and rNS1-trunc have wt growth kinetics, the data suggest that the presence of NS2/NEP mutation G70S has no effect on virus growth in tissue culture. It is not possible to rule out that the secondary mutations introduced into NS2/NEP of rNS1-ESEV + 7 and rNS1-trunc viruses were responsible for the attenuation of these viruses in tissue culture. However, it is unlikely that they adversely affected the function of NS2/NEP, because replication of both viruses occurred in the mouse lung and infection with 105 pfu of either virus resulted in 0% survival. To eliminate any effects of the NS2/NEP mutations on viral replication one would require a control virus containing these mutations alone. However, this is not possible without altering the NS1 coding sequence.
Supplanting NS1 C-terminal residues (ESEV or EPEV) from human isolates of H5N1 HPAI virus NS1 did not affect the ability of the virus to grow in tissue culture, but it significantly increased the virulence and pathogenicity of the virus in infected mice and caused extensive pathology in infected mouse lungs. Substitution of the NS1 C terminus with KSEV from the 1918 H1N1 virus also increased pathogenicity as observed by the morphology of lung sections, but this virus caused a little less weight loss in mice compared with viruses with the H5N1 HPAI NS1 sequences. The virus containing the H5N1 HPAI sequence (ESEV), followed by a seven amino acid extension, found on a number of avirulent human influenza virus strains (e.g., A/Fiji/83), was attenuated in tissue culture, and demonstrated a significant decrease in virulence and pathogenicity in infected mice when compared with wt virus. Furthermore, when the C-terminal four amino acid sequence was deleted from NS1, the rNS1-trunc virus was severely attenuated in tissue culture, did not cause infected mice to lose weight, and had a 14-fold increase in MLD50 compared with wt virus. However, the data show that the function of this C-terminal sequence is not absolutely essential because the virus replicates both in tissue culture and in the lungs of infected mice, as demonstrated by histological antigen staining and the measurement of increased infectious viral titers within the lung tissues.
Infection of cells with the rNS1-trunc virus demonstrated that removal of the C-terminal amino acid sequence did not alter the expression, stability, or intracellular localisation of the NS1 protein, nor did it reduce the ability of NS1 to circumvent the host IFN response. However, it is possible that the truncation disrupted or reduced the binding of PABII to NS1 that is required to prevent the export of cellular premRNAs from the nucleus in infected cells (37). Disruption of this feature may be responsible for the attenuation of the rNS1-trunc virus in tissue culture and the increase in MLD50 in infected mice.
The extensive pathology (severe alveolitis and hemorrhage) caused by the rNS1 viruses containing the H5N1 HPAI NS1 sequences and 1918 sequences (rNS1-ESEV, rNS1-EPEV, and rNS1-KSEV) would be consistent with increased cytokine production, as observed in mice infected with 1918 H1N1 virus (38). This pathology was mirrored by the increased spread of the virus throughout the entire lung tissue compared with minimal localized viral antigen staining in the wt virus-infected tissues.
These data identify the C-terminal four residues of the NS1 protein as a pathogenicity factor of influenza virus. Further studies may help to determine the identity of the specific interacting PDZ domain-containing protein, among many shown to interact with NS1 (31) and to identify the cellular pathway that is affected by the NS1 protein.
Materials and Methods
Cells and Viruses.
293-T, A549, and Madin–Darby canine kidney (MDCK) cells were maintained in Dulbecco's modified Eagle's medium (DMEM) (Invitrogen) supplemented with 10% FBS. Influenza A/WSN/33 wild-type (wt) (rWSN wt) virus and all recombinant mutant viruses were propagated in MDCK cells overlaid with serum-free DMEM containing 2.5 μg/ml N-acetyl trypsin (Sigma–Aldrich) at 37°C. Wt influenza virus and recombinant rNS1 mutant viruses were generated by plasmid-based reverse genetics, essentially as described in refs. 39 and 40. Viruses were propagated through two passages followed by plaque assay titration on MDCK cells. Viral RNA was extracted by using the QIAamp viral RNA kit (Qiagen), followed by reverse-transcriptase PCR by using genome-specific primers and the resultant cDNA sequenced by using a 3100-Avant genetic analyzer (Applied Biosystems). Recombinant Newcastle disease virus-encoding green fluorescent protein (NDV-GFP) (33) was kindly provided by Adolfo Garcia-Sastre and Peter Palese (Mount Sinai School of Medicine, New York). The virus was propagated in 10-day-old embryonated chicken eggs.
Antibodies.
A goat antiserum (goat anti-Udorn), raised to purified A/Udorn/72 virus, was used to detect influenza virus NP and M1 proteins by immunoblotting and influenza viral antigen-positive cells by histopathology. The NS1 protein was detected by using a rabbit polyclonal anti-GST-NS1 antiserum by immunoblotting and immunofluorescence. The anti-GST-NS1 antiserum was kindly provided by Robert M. Krug (University of Texas, Austin, TX).
Immunoblotting.
MDCK cells were infected with wt or mutant viruses at a multiplicity of infection (MOI) of 3 for 18 h at 37°C. Cells were lysed in 1× RIPA buffer (0.15 M NaCl/0.01 M Tris·HCl, pH 7.4/1% Triton X-100/1% sodium deoxycholate/0.1% SDS) (41) containing protease inhibitors and clarified by ultracentrifugation at 100,000 × g for 10 min in a Beckman TLA 100.2 rotor. SDS/PAGE and immunoblotting were performed as described in ref. 42 by using goat anti-Udorn sera (for NP and M1) or a rabbit anti-NS1 serum as primary antibody and an AlexaFluor 680-conjugated secondary antibody (Molecular Probes). Proteins were detected with an Odyssey infrared imaging system (Li-Cor Biosciences).
Viral Growth Kinetics.
Confluent MDCK cells were infected with wt or rNS1 viruses at an MOI of 0.001, overlaid with serum-free DMEM containing 2.5 μg/ml N-acetyl-trypsin and incubated at 37°C. Cell supernatants were harvested every 12 h until 60 h p.i., cell debris removed by centrifugation at 1,000 × g for 5 min in a tabletop centrifuge, and samples titrated by plaque assay on MDCK cells as described in ref. 42.
Immunofluorescence.
Immunofluorescent staining of NS1 protein in virus-infected MDCK cells was performed as described in ref. 43. Images were captured by using an Axiovert 200M/Apotome microscope (Zeiss).
For the NDV-GFP virus replication assay, A549 cells were either infected with wt or mutant influenza virus at an MOI of 5 or treated with 150 units/ml IFN-β (R&D Systems) and incubated at 37°C for 6 h. Cells were washed in PBS, infected with NDV-GFP at an MOI of 10, and incubated at 37°C for 18 h. Cells were then fixed in ice-cold methanol/acetone (1:1) for 10 min and washed in PBS; coverslips were mounted on glass slides by using Vectashield mounting media (Vector Laboratories). Images were captured by using an Axiovert 200M/Apotome microscope (Zeiss).
Mouse Experiments.
All experiments were carried out under BSL-2 conditions with investigators wearing appropriate protective equipment and being compliant with all Institutional Animal Care and Use Committee (IACUC) of University of Maryland approved protocol and under Animal Welfare (AWA) regulations.
Female 4- to 5-week-old BALB/c mice (Charles River Laboratories) were used throughout the study. To determine the mouse lethal dose (MLD50), groups of four mice were anesthetized with isoflurane followed by intranasal inoculation with various doses of wt or rNS1 viruses diluted in 50 μl of PBS. Mice were monitored for signs of disease and their body weight was measured for either 14 days or until the loss of 30% of their body weight, at which point they were euthanized. Survival of mice was monitored until 14 days p.i. and the MLD50 for each virus was determined. To determine the statistical significance of the effects of virus, dosage, and time on the loss of body weight, a repeated-measures ANOVA model was used.
To monitor growth kinetics in the lung, groups of four mice were intranasally inoculated with 104 pfu of wt or rNS1 viruses in 50 μl of PBS under isoflurane anesthetic conditions. Lungs were collected at 2, 4, and 6 days p.i. A portion of the lung was preserved in formalin for histological investigation. For titration of virus, lung homogenates were prepared in 1.5 ml of PBS by using a sterile mortar, pestle, and sea sand. The homogenate was clarified by centrifugation at 2,000 rpm for 15 min at 4°C. Lung homogenates were serially 10-fold diluted from 10−1 to 10−7 in PBS. MDCK cells were infected with 500 μl of diluted lung homogenate for 1 h at 37°C. Cells were washed with PBS, overlaid with 3 ml of MEM medium (Sigma–Aldrich) containing 0.9% agar supplemented with 1 μg/ml l-1-tosylamido-2-phenylethyl chloromethyl ketone-trypsin (TPCK-trypsin) and incubated at 37°C for 4 days. Cells were fixed in 1% gluteraldehyde and stained with crystal violet. The virus titer in the lung was expressed in log10 pfu/g.
For histopathological analysis of lung tissues the formalin-preserved lung samples were embedded in paraffin and sectioned. Serial 4-μm sections were stained with either H&E or antigen-stained by using the goat anti-Udorn antibody and a horseradish peroxidase-conjugated secondary antibody.
Supplementary Material
Acknowledgments.
We thank B. Thomas Carr of Carr Consulting Inc, Wilmette, IL, for performing the statistical analysis and Ivan Gomez Osorio for assisting with animal studies; Drs. Adolfo Garcia-Sastre and Peter Palese for the NDV-GFP virus; and Dr. Robert Krug for NS1 antiserum. This work was supported by National Institutes of Health Grants R01 AI 052155 (to D.R.P.) and R01 AI 20201(to R.A.L.). D.J. was an Associate and R.A.L. is an Investigator of the Howard Hughes Medical Institute.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0800482105/DC1.
References
- 1.Wright PF, Neumann G, Kawaoka Y. In: Fields Virology. Knipe DM, Howley PM, editors. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 1691–1740. [Google Scholar]
- 2.Kash JC, et al. Genomic analysis of increased host immune and cell death responses induced by 1918 influenza virus. Nature. 2006;443:578–581. doi: 10.1038/nature05181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taubenberger JK. The origin and virulence of the 1918 “Spanish” influenza virus. Proc Am Philos Soc. 2006;150:86–112. [PMC free article] [PubMed] [Google Scholar]
- 4.Glaser L, et al. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol. 2005;79:11533–11536. doi: 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen H, et al. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Res. 2007;128:159–163. doi: 10.1016/j.virusres.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Tumpey TM, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 7.Tumpey TM, et al. Pathogenicity and immunogenicity of influenza viruses with genes from the 1918 pandemic virus. Proc Natl Acad Sci USA. 2004;101:3166–3171. doi: 10.1073/pnas.0308391100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 9.Hatta M, et al. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 2007;3:e133. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zamarin D, Ortigoza MB, Palese P. Influenza A virus PB1–F2 protein contributes to viral pathogenesis in mice. J Virol. 2006;80:7976–7983. doi: 10.1128/JVI.00415-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geiss GK, et al. Cellular transcriptional profiling in influenza A virus-infected lung epithelial cells: The role of the nonstructural NS1 protein in the evasion of the host innate defense and its potential contribution to pandemic influenza. Proc Natl Acad Sci USA. 2002;99:10736–10741. doi: 10.1073/pnas.112338099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falcon AM, et al. Defective RNA replication and late gene expression in temperature-sensitive influenza viruses expressing deleted forms of the NS1 protein. J Virol. 2004;78:3880–3888. doi: 10.1128/JVI.78.8.3880-3888.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Min JY, Li S, Sen GC, Krug RM. A site on the influenza A virus NS1 protein mediates both inhibition of PKR activation and temporal regulation of viral RNA synthesis. Virology. 2007;363:236–243. doi: 10.1016/j.virol.2007.01.038. [DOI] [PubMed] [Google Scholar]
- 14.Ehrhardt C, et al. Influenza A virus NS1 protein activates the PI3K/Akt pathway to mediate antiapoptotic signaling responses. J Virol. 2007;81:3058–3067. doi: 10.1128/JVI.02082-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hale BG, Jackson D, Chen YH, Lamb RA, Randall RE. Influenza A virus NS1 protein binds p85β and activates phosphatidylinositol-3-kinase signaling. Proc Natl Acad Sci USA. 2006;103:14194–14199. doi: 10.1073/pnas.0606109103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin YK, Liu Q, Tikoo SK, Babiuk LA, Zhou Y. Influenza A virus NS1 protein activates the phosphatidylinositol 3-kinase (PI3K)/Akt pathway by direct interaction with the p85 subunit of PI3K. J Gen Virol. 2007;88:13–18. doi: 10.1099/vir.0.82419-0. [DOI] [PubMed] [Google Scholar]
- 17.Zhirnov OP, Klenk HD. Control of apoptosis in influenza virus-infected cells by up-regulation of Akt and p53 signaling. Apoptosis. 2007;12:1419–1432. doi: 10.1007/s10495-007-0071-y. [DOI] [PubMed] [Google Scholar]
- 18.Min JY, Krug RM. The primary function of RNA binding by the influenza A virus NS1 protein in infected cells: Inhibiting the 2′-5′ oligo (A) synthetase/RNase L pathway. Proc Natl Acad Sci USA. 2006;103:7100–7105. doi: 10.1073/pnas.0602184103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Talon J, et al. Activation of interferon regulatory factor 3 is inhibited by the influenza A virus NS1 protein. J Virol. 2000;74:7989–7996. doi: 10.1128/jvi.74.17.7989-7996.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang X, et al. Influenza A virus NS1 protein prevents activation of NF-κB and induction of alpha/beta interferon. J Virol. 2000;74:11566–11573. doi: 10.1128/jvi.74.24.11566-11573.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ludwig S, et al. The influenza A virus NS1 protein inhibits activation of Jun N-terminal kinase and AP-1 transcription factors. J Virol. 2002;76:11166–11171. doi: 10.1128/JVI.76.21.11166-11171.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo Z, et al. NS1 protein of influenza A virus inhibits the function of intracytoplasmic pathogen sensor, RIG-I. Am J Respir Cell Mol Biol. 2007;36:263–269. doi: 10.1165/rcmb.2006-0283RC. [DOI] [PubMed] [Google Scholar]
- 23.Mibayashi M, et al. Inhibition of retinoic acid-inducible gene I-mediated induction of beta interferon by the NS1 protein of influenza A virus. J Virol. 2007;81:514–524. doi: 10.1128/JVI.01265-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Opitz B, et al. IFNβ induction by influenza A virus is mediated by RIG-I which is regulated by the viral NS1 protein. Cell Microbiol. 2007;9:930–938. doi: 10.1111/j.1462-5822.2006.00841.x. [DOI] [PubMed] [Google Scholar]
- 25.Nemeroff ME, Barabino SM, Li Y, Keller W, Krug RM. Influenza virus NS1 protein interacts with the cellular 30 kDa subunit of CPSF and inhibits 3′ end formation of cellular pre-mRNAs. Mol Cell. 1998;1:991–1000. doi: 10.1016/s1097-2765(00)80099-4. [DOI] [PubMed] [Google Scholar]
- 26.Noah DL, Twu KY, Krug RM. Cellular antiviral responses against influenza A virus are countered at the posttranscriptional level by the viral NS1A protein via its binding to a cellular protein required for the 3′ end processing of cellular pre-mRNAS. Virology. 2003;307:386–395. doi: 10.1016/s0042-6822(02)00127-7. [DOI] [PubMed] [Google Scholar]
- 27.Bergmann M, et al. Influenza virus NS1 protein counteracts PKR-mediated inhibition of replication. J Virol. 2000;74:6203–6206. doi: 10.1128/jvi.74.13.6203-6206.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernandez-Sesma A, et al. Influenza virus evades innate and adaptive immunity via the NS1 protein. J Virol. 2006;80:6295–6304. doi: 10.1128/JVI.02381-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Basler CF, et al. Sequence of the 1918 pandemic influenza virus nonstructural gene (NS) segment and characterization of recombinant viruses bearing the 1918 NS genes. Proc Natl Acad Sci USA. 2001;98:2746–2751. doi: 10.1073/pnas.031575198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seo SH, Hoffmann E, Webster RG. The NS1 gene of H5N1 influenza viruses circumvents the host anti-viral cytokine responses. Virus Res. 2004;103:107–113. doi: 10.1016/j.virusres.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 31.Obenauer JC, et al. Large-scale sequence analysis of avian influenza isolates. Science. 2006;311:1576–1580. doi: 10.1126/science.1121586. [DOI] [PubMed] [Google Scholar]
- 32.Sheng M, Sala C. PDZ domains and the orgaqnization of supramolecular complexes. Annu Rev Neurosci. 2001;24:1–29. doi: 10.1146/annurev.neuro.24.1.1. [DOI] [PubMed] [Google Scholar]
- 33.Park MS, et al. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J Virol. 2003;77:1501–1511. doi: 10.1128/JVI.77.2.1501-1511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.He B, et al. Recovery of paramyxovirus simian virus 5 with a V protein lacking the conserved cysteine-rich domain: The multifunctional V protein blocks both interferon-beta induction and interferon signaling. Virology. 2002;303:15–32. doi: 10.1006/viro.2002.1738. [DOI] [PubMed] [Google Scholar]
- 35.Neumann G, Hughes MT, Kawaoka Y. Influenza A virus NS2 protein mediates vRNP nuclear export through NES-independent interaction with hCRM1. EMBO J. 2000;19:6751–6758. doi: 10.1093/emboj/19.24.6751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Neill RE, Talon J, Palese P. The influenza virus NEP (NS2 protein) mediates the nuclear export of viral ribonucleoproteins. EMBO J. 1998;17:288–296. doi: 10.1093/emboj/17.1.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li Y, Chen ZY, Wang W, Baker CC, Krug RM. The 3′-end-processing factor CPSF is required for the splicing of single-intron pre-mRNAs in vivo. RNA. 2001;7:920–931. doi: 10.1017/s1355838201010226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tumpey TM, et al. Pathogenicity of influenza viruses with genes from the 1918 pandemic virus: Functional roles of alveolar macrophages and neutrophils in limiting virus replication and mortality in mice. J Virol. 2005;79:14933–14944. doi: 10.1128/JVI.79.23.14933-14944.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fodor E, et al. Rescue of influenza A virus from recombinant DNA. J Virol. 1999;73:9679–9682. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Neumann G, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci USA. 1999;96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lamb RA, Choppin PW. Synthesis of influenza virus proteins in infected cells: Translation of viral polypeptides, including three P polypeptides, from RNA produced by primary transcription. Virology. 1976;74:504–519. doi: 10.1016/0042-6822(76)90356-1. [DOI] [PubMed] [Google Scholar]
- 42.Chen BJ, Takeda M, Lamb RA. Influenza virus hemagglutinin (H3 subtype) requires palmitoylation of its cytoplasmic tail for assembly: M1 proteins of two subtypes differ in their ability to support assembly. J Virol. 2005;79:13673–13684. doi: 10.1128/JVI.79.21.13673-13684.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nemeroff ME, Qian X-Y, Krug RM. The influenza virus NS1 protein forms multimers in vitro and in vivo. Virology. 1995;212:422–428. doi: 10.1006/viro.1995.1499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.