Abstract
This study examined whether conduct disorder (CD) was associated with war zone stress and war-related post-traumatic stress disorder (PTSD) symptoms in American Indian (AI) Vietnam veterans. Cross-sectional lay-interview data was analyzed for 591 male participants from the American Indian Vietnam Veterans Project. Logistic regression evaluated the association of CD with odds of high war zone stress and linear regression evaluated the association of CD and PTSD symptom severity. Childhood CD was not associated with increased odds of high war zone stress. CD was associated with elevated war-related PTSD symptoms among male AI Vietnam Veterans independent of war zone stress level and other mediators. Future efforts should examine reasons for this association and whether the association exists in other AI populations.
Posttraumatic stress disorder (PTSD) is a common and serious problem among U.S. military combat veterans (Koenen et al., 2002). Studies consistently find that the severity of war-related PTSD symptoms is positively associated with the degree of exposure to war zone stress. Combat is the form of stress most commonly studied (Green, Grace, Lindy, Gleser, & Leonard, 1990; King, King, Foy, Keane, & Fairbank, 1999). However, war zone stress can be defined as a combination of both objective and subjective factors. Objective factors include direct combat experience and exposure to atrocities, while subjective factors include perceived threat and deprivation in the war zone. Each of these types of stress differentially affect PTSD symptoms (King, King, Gudanowski, & Vreven, 1995). Factors occurring before and after the war also affect war zone stress and PTSD symptoms. These factors can include demographic variables such as age and education, service factors such as rank, and the presence of other mental illness, including substance dependence (Brewin, Andrews, & Valentine, 2000; Davidson, Hughes, Blazer, & George, 1991; Frueh, Brady, & de Arellano, 1998; Green et al., 1990; King, King, Foy, & Gudanowski, 1996; Wolfe, Erickson, Sharkansky, King, & King, 1999). For instance, males who are younger when they enter the military experience higher levels of combat than those who are older at entry (King et al., 1996).
Childhood antisocial behavior is another important factor associated with exposure to war zone combat and PTSD symptoms in national samples of Vietnam veterans (King et al., 1999; Koenen et al., 2002). People with antisocial characteristics may perceive less threat in a war zone than those without (King et al., 1996), and risk-taking behavior associated with childhood conduct disorder (CD) may increase chances of trauma exposure (Koenen et al, 2002). Individuals with CD may have insufficient resources to cope with the sequelae of stressful or traumatic events once exposed (Koenen et al., 2002). Since onset of CD precedes the minimum age for military enrollment, the veteran population is well suited to study the potential association between CD and PTSD symptoms.
Relatively little is known about PTSD in American Indian (AI) Vietnam veterans. A recent study found that AI Vietnam veterans have higher rates of PTSD and PTSD symptoms than White veterans (Beals et al., 2002). Increased exposure to objective and subjective war zone stress largely accounted for this difference. However, whether childhood factors may be associated with level of war zone stress and PTSD symptoms in AI veterans has not been specifically examined. An examination of childhood factors could help those caring for AI veterans address salient factors pre-dating the war. Findings also could have important policy implications for military recruitment and combat training, given the persistent nature of PTSD (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995) as well national concern about the emotional well-being of military personnel.
The American Indian Vietnam Veterans Project (AIVVP) was a Congressionally mandated effort to examine PTSD in AIs. Six hundred twenty one AI Vietnam veterans were interviewed by non-military personnel concerning childhood and pre-military history, Vietnam experience, and post-service factors, as well as symptoms of mental illnesses such as CD and PTSD. Using the cross-sectional data of the AIVVP, this analysis addressed the following questions: 1) Is CD associated with increased odds of high war zone stress in AI Vietnam veterans? 2) Adjusting for level of war zone stress, is CD associated with elevated war-related PTSD symptoms in AI Vietnam veterans? We hypothesized that CD would be associated with higher odds of war zone stress and elevated war-related PTSD symptoms after adjusting for other potentially mediating variables.
Methods
Sample
We conducted a retrospective analysis using cross-sectional data from the AIVVP. A comprehensive description of the AIVVP sample and methodology is described elsewhere (National Center for Posttraumatic Stress Disorder & The National Center for American Indian and Alaska Native Mental Health Research, 1996). Briefly, the AIVVP was a national survey of AI Vietnam veterans conducted between 1993 and 1994 as mandated under Public Law 101–507. Congress directed the National Center for PTSD within the Department of Veterans Affairs to extend the National Vietnam Veteran Readjustment Study (NVVRS) to minority groups beyond Blacks and Hispanics (Kulka et al., 1990). The National Center for American Indian and Alaska Native Mental Health Research conducted the AI portion of this effort (Beals et al., 2002; Gurley et al., 2001).
The AIVVP sample included one Southwest tribe and two closely affiliated Northern Plains tribes that are not identified in order to preserve community confidentiality (Norton & Manson, 1996). The former is referred to as the Southwest tribal group, and the latter are combined into a Northern Plains tribal group. These two tribal groups share common experiences, such as forced colonization, with other AI groups, but also differ in levels of income, education, and acculturation (Beals, Spicer et al., 2003; Mitchell, Beals, Novins, & Spicer, 2003; Spicer et al., 2003). Thus, selection of these two tribal groups accounts simultaneously for common experiences and diversity in the AI population (Beals, Manson, Mitchell, & Spicer, 2003).
The AIVVP used a three stage sampling strategy. Women were excluded due to the small numbers of AI female veterans who served. First, tribal rolls identified all recognized male members of the given tribal groups (Beals et al., 2002). Men born between 1930 and 1958 were selected from the rolls. Using NVVRS estimates, roughly 3% of male Vietnam theater veterans were born before 1930 (Kulka et al., 1990). The year of 1958 was chosen as the upper birth year since those born in 1959 would have been 16 when the Vietnam era ended in 1975 and not eligible for enlistment. Therefore, it was estimated 97% of eligible AI veterans would fall in that birth date range. Second, males in this age range were located with a 93.6% and 90.8% success rate respectively in Northern Plains and Southwest. Third, the men were queried in person regarding service in Vietnam. They were invited to participate in the AIVVP if they were in the Vietnam theatre and living on or near the reservation. For Northern Plains, 29.4% of those located were eligible (n = 362) and 37.3% (n = 355) of Southwest tribal members were eligible. For the Northern Plains and Southwest tribes, 91.7% and 94.9% of veterans located and found eligible agreed to participate. All participants completed a 4–5 hour lay-administered interview similar to the NVVRS interview Lay personnel were trained in interview administration and stringent quality control measures were implemented. The final AIVVP sample comprised 621 male AI veterans from the Southwest and Northern Plains tribal group (National Center for Posttraumatic Stress Disorder & The National Center for American Indian and Alaska Native Mental Health Research, 1996).
Measures
Conduct Disorder
The Composite International Diagnostic Interview (World Health Organization, 1994) modified for the National Comorbidity Study by University of Michigan (Kessler et al., 1994) was used to determine symptoms of CD according to the third revised edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) (American Psychiatric Association, 1987) and ninth version of the International Statistical Classification of Diseases (ICD-9) (World Health Organization, 1978) criteria. Thirteen CD symptoms were assessed as present or not present before the age of 15. CD was coded as present if three or more symptoms were endorsed; otherwise, it was coded as not present.
War Zone Stress
The AIVVP used the same war zone stress measure employed in the NVVRS (Kulka et al., 1990) with revisions made to improve the comprehensibility for the two tribal groups. Revisions included shortening, deleting, or altering the wording of prefaces, deleting confusing adjectives, and the addition of clarifying phrases. Changes made to this section of the interview are detailed fully elsewhere (National Center for Posttraumatic Stress Disorder & The National Center for American Indian and Alaska Native Mental Health Research, 1996). The war zone stress construct reflects the severity of each veteran’s war experiences across four objective and subjective dimensions: traditional combat, exposure to atrocities, loss of meaning and control, and deprivation. Items contributing to the war zone stress variables were scaled to have a mean of 0 and a standard deviation of 1. The four factor scores were computed by averaging the scores for items contributing to the factor. The four factor scores were then converted to z-scores with the NVVRS sample as the population standard. This approach was taken in order to enable comparison of AIs in the AIVVP to other racial/ethnic groups in the NVVRS. In addition to the continuous scale, a high war zone stress indicator variable was constructed by coding scores in the upper NVVRS quartile as denoting high war zone stress exposure.
War-related PTSD symptoms
We used the Mississippi Scale for Combat Related Posttraumatic Stress Disorder (Keane, Caddell, & Taylor, 1988) to measure symptoms of war-related PTSD. The Mississippi Scale was administered to all 621 participants and specifically queried about their military experience. It assessed all the required PTSD criteria delineated in the DSM-III-R, such as intrusive memories and interpersonal adjustment problems. Participants rated each of 35 items on a 5-point Likert scale. Items were summed to provide a continuous measure of PTSD symptom severity ranging from 35 to 175. The Mississippi Scale has an acceptable level of agreement with the Structured Clinical Interview for DSM-III-R as demonstrated by sensitivity and specificity coefficients. Although scores above 89 have been used to indicate PTSD positive cases in other efforts (Kulka et al., 1990), there are no thresholds validated for use in the AI population. Therefore, we used the continuous Mississippi PTSD scale score as the outcome of interest.
Pre-military factors
Trauma occurring before military enrollment was assessed by self report of any of nine lifetime traumatic events meeting DSM-III-R PTSD Criterion A (e.g., a traumatic event beyond the range of usual human experience) for which the age when the trauma occurred was younger than the participant’s age at military enrollment. Possible traumas included experiencing sexual or physical assault, suffering serious neglect, being threatened with a weapon, being kidnapped, experiencing a life-threatening accident, witnessing someone getting badly injured or killed, and experiencing natural disasters. Information was only collected for up to three traumatic events per participant. Participants reporting four or more traumas specified the three worst, and information was not available for the other events. We created a “previous trauma” variable coded as present if one or more of the worst traumas occurred before military enrollment, and not present for participants without reported traumas or whose three worst traumas all occurred after military enrollment. This construction could have missed qualifying pre-military traumas in the latter group, but we were limited by the information available in the AIVVP data set.
The CIDI was also used to determine DSM-III-R and ICD-9 symptoms and age of onset of specific mental illness, including PTSD, major depressive disorder, dysthymia, panic disorder, generalized anxiety disorder, social phobia, alcohol and/or drug abuse, and alcohol and/or drug dependence. Disorders were coded as present or not present before entry into Vietnam service based on age of onset compared to age of entry into the military. The pre-military DSM-III-R PTSD symptoms referenced the nine traumatic life events, and were evaluated for up to three events per person, as described in the previous paragraph. A composite variable for previous mental illness indicated the presence of one or more of the following: major depressive disorder, dysthymia, panic disorder, generalized anxiety disorder, and/or social phobia. The composite was created to minimize Type II error. Indicators of alcohol and/or drug abuse and dependence were evaluated separately from the composite mental illness variable.
Factors at entry to military
Variables which might mediate the relationship between war zone stress and war-related PTSD symptoms included age at entry into the military (≤ 18 years, 18–19 years, ≥ 20 years), employment status at entry into the military (employed, unemployed/laid-off, student, other – including disabled), and educational attainment at entry into the military (less than high school graduate, high school graduate/GED, at least some college). Educational category was determined by comparing the month and year of entry into the military with the month and year of high school graduation, receipt of GED, and/or graduation from college.
Military service factors
Military factors included military status (drafted, enlisted/activated/commissioned) and whether the participant ever achieved the rank of officer (yes, no).
Weighting and Statistical Analyses
AIVVP participants had different probabilities of being included in the data set based on whether they were living on or near the reservation and whether they were successfully located. To accommodate the complex weighting structure, this analysis was conducted using the SVY commands in Stata version 8 (StataCorp, 2003). We plotted mean Mississippi PTSD symptom scores by CD status across war zone stress quartiles to rule out a significant interaction between CD and war zone stress. We calculated descriptive statistics for the outcome variables and potential mediating factors, stratified by the presence or absence of CD, using percents to describe categorical variables and means with standard deviations for continuous variables. To address the first specific aim we used logistic regression to evaluate the association of CD with odds of high war zone stress, including the potentially mediating variables described above as independent variables. To address the second specific aim we used linear regression to assess the association of CD with Mississippi PTSD symptom scores in three models. The first model was unadjusted. Since war zone stress is associated with war-related PTSD (King et al., 1999), the association of CD and PTSD symptoms was also adjusted for war zone stress in the second model. The third model included war zone stress and all other potentially mediating variables. All inferential statistics are presented as point estimates with 95% confidence intervals.
Results
Participants were excluded from our study if they were missing information for CD, war zone stress, war-related PTSD, or any of the potentially mediating variables. Thirty (4.8%) of the 621 participants were excluded because of missing data fields, yielding 591 participants for analysis.
As shown in Figure 1, the mean Mississippi PTSD symptom score plotted against the war zone stress quartiles increased consistently for veterans with and without CD, with no evidence of an interaction between CD and war zone stress. The war zone stress variable was a normally distributed z-score scale (M = 0.03, SD = 0.6).
Figure 1.
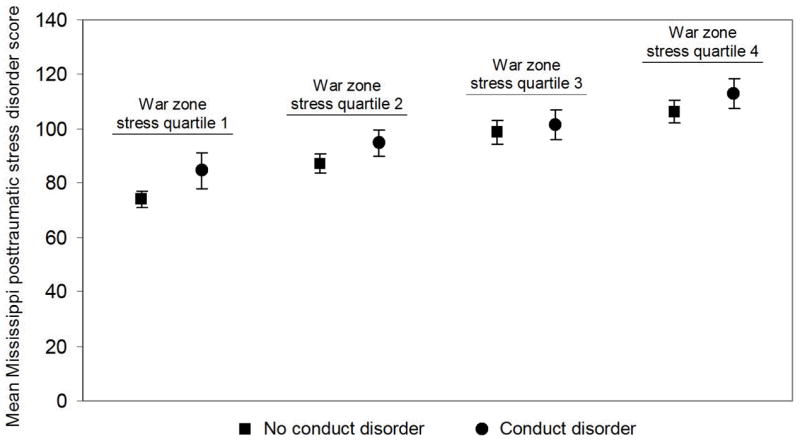
Mean Mississippi posttraumatic stress disorder (PTSD) symptom scores stratified by war zone exposure quartile and conduct disorder diagnosis. Error bars indicate 95% confidence intervals.
Table 1 shows the sociodemographic characteristics of the AI veterans stratified by CD status. Twenty-seven percent of veterans with CD and 23% without CD reported high war zone stress, χ2 (587, N = 591) = .67, p = .41, whereas the mean Mississippi PTSD symptom score was 99.4, SD = 1.6, for respondents with CD, compared to 90.6, SD = 1.1, for respondents without CD, t (587) = 4.44, p < .001. Veterans with and without CD appeared to have similar distributions of other variables before, at entry, or during the military except alcohol and/or drug dependence. Veterans with CD were more likely to report alcohol and/or drug dependence prior to military service than veterans without CD, χ2 (587, N = 591) = 19.6, p < .001.
Table 1.
Descriptive statistics stratified by conduct disorder diagnosis
| Conduct Disorder
|
||
|---|---|---|
| Variable | Present (n = 173) % | Not present (n = 418) % |
| Outcome | ||
| High war zone stress exposurea | 27 | 23 |
| Mississippi PTSD symptoms score, M (SD) | 99.4* (1.6) | 90.6 (1.1) |
| Before entry to military | ||
| Trauma | 19 | 14 |
| Non-war-related posttraumatic stress disorder | 7 | 3 |
| Mental illnessc | 14 | 12 |
| Alcohol and/or drug abuse | 13 | 12 |
| Alcohol and/or drug dependence | 26* | 12 |
| At entry to military | ||
| Age | ||
| <18 | 9 | 8 |
| 18–19 | 47 | 50 |
| 20+ | 44 | 42 |
| Education | ||
| Less than high school | 40 | 39 |
| High school/GED | 25 | 25 |
| College (2 or 4 year) | 35 | 36 |
| Employment | ||
| Working | 41 | 40 |
| Unemployed/laid off | 26 | 25 |
| Student | 31 | 33 |
| Other | 1 | 2 |
| During military service | ||
| Status: | ||
| Drafted | 39 | 34 |
| Enlisted | 61 | 66 |
| Achieved officer rank | 42 | 48 |
High exposure indicates upper quartile of war zone exposure.
Mississippi Scale for Combat-Related Posttraumatic Stress Disorder score ≥ 89.
Includes social phobia, panic disorder, generalized anxiety disorder, dysthymia, and depression.
Frequency higher than counterpart, p < .001.
CD was not associated with higher odds of high war zone stress in the unadjusted (OR = 1.2, 95% CI = 0.8 – 1.8, ns) or adjusted (OR = 1.2, 95% CI = 0.8 – 1.9, ns) logistic regression models. CD was associated with higher mean Mississippi PTSD symptom scores in the unadjusted model (Mdiff = 8.8, 95% CI = 4.9 – 12.7, p < .001) (Table 2). The association persisted even after adjusting for war zone stress (Mdiff = 8.1, 95% CI = 4.6=11.7, p < .001) and the combination of war zone stress with all other potentially mediating variables (Mdiff = 7.4, 95% CI = 3.9 – 10.9, p < .001).
Table 2.
Linear regression models comparing Mississippi PTSD scores in AI Vietnam veterans with and without conduct disorder
| Model # | Adjustment variables | Conduct Disorder M (SD)b | No Conduct Disorder M (SD)c | 95% CIa for difference |
|---|---|---|---|---|
| 1 | (none) | 99.4 (21.0) | 90.6 (22.5) | (4.9 – 12.7)* |
| 2 | High war zone stress | 99.5 (19.7) | 90.6 (20.5) | (4.6 – 11.7)* |
| 3 | High war zone stress + all covariatesd | 99.5 (18.4) | 90.8 (20.5) | (3.9 – 10.9)* |
CI = confidence interval.
Mean Mississippi PTSD score for veterans with conduct disorder.
Mean Mississippi PTSD score for veterans without conduct disorder.
Includes psychosocial variables before military service (trauma, PTSD, mental illness, alcohol and/or drug abuse, and alcohol and/or drug dependence), sociodemographic variables at entry to military (age, education, employment status), and military service factors (military status, officer rank).
p ≤ .001.
Discussion
Current efforts in PTSD research focus on identifying factors that might affect exposure to trauma and PTSD symptoms in some individuals. This study is the first to examine the relationship between childhood CD, level of war zone stress, and war-related PTSD symptoms in AI Vietnam veterans. We did not find CD to be associated with high war zone stress in the AIVVP. However, our results indicate CD is strongly associated with elevated mean scores of war-related PTSD symptoms in AI Vietnam veterans, even after adjusting for level of war zone stress and other potentially mediating variables.
A robust association between CD and higher levels of war zone combat has been found in previous studies with non-AI populations (Kessler et al., 1995; King et al., 1996; King et al., 1999; Koenen et al., 2002). However, in our analysis, AI Vietnam veterans had similar odds of high levels of war zone stress regardless of childhood CD status. Likewise, others have discerned numerous differences between people with and without CD according to demographic variables, mental illnesses, and previous trauma. In our analysis, AI Vietnam veterans with CD did not appear to differ from those without CD by age, education, employment status, or indicators of mental health pathology before military service (trauma, PTSD, other mental illnesses). Only alcohol and/or drug dependence appeared to have a positive correlation associated with CD, but this variable was not associated with level of war zone stress or war-related PTSD symptoms. One possible explanation for these results could be a ceiling effect, given the elevated rates of CD and war zone stress in AI veterans compared to White veterans (Beals et al., 2002). Blacks and Hispanics have also been found to have higher absolute rates of PTSD but are likewise exposed to higher levels of war zone stress (Frueh et al., 1998). However, the normal distribution of the variable measuring war zone stress refutes a lack of heterogeneity for this sample. In other words, there is not support for a ceiling effect for war zone stress. Compared to other ethnic groups, the AI veterans sampled were no more likely to meeting criteria for antisocial personality disorder than veterans of other ethnicities(National Center for Posttraumatic Stress Disorder & The National Center for American Indian and Alaska Native Mental Health Research, 1996). Antisocial personality disorder requires that criteria for CD are met as a child.
Previous analyses of the AIVVP data indicated that AI Vietnam veterans had higher rates of PTSD than whites in NVVRS and that higher levels of war zone stress largely accounted for this disparity (Beals et al., 2002). In our analysis, the presence of childhood CD was associated with higher mean PTSD symptoms. This effect occurred independently of level of war zone stress and other potentially mediating variables such as pre-military trauma and mental illness. Some authors have hypothesized that CD predisposes people to PTSD symptoms by impairing their ability to cope with the stress of traumatizing events (Koenen et al., 2002). Cognitive deficits as well as limited emotional regulation skills have also been noted in individuals with CD (Clarizio, 1997; Giancola & Tarter, 1999; Hill, 2002), and the nature of the disorder involves conflict with people and social institutions that could reduce available support to buffer the attendant stress (Hill, 2002; King et al., 1999).
There are some limitations to our study. First, assessments of the presence and onset of CD, PTSD, and other mental illnesses were retrospective in nature. If individuals with CD or PTSD are more likely than those without to inaccurately recall childhood history, this would affect the observed associations. Some authors have not found retrospective designs to affect reporting of childhood adversity or trauma (e.g., Brewin et al., 2000) while others have found childhood experiences like sexual abuse are associated with overendorsement of self-reported psychiatric symptoms (Smith, Frueh, Sawchuk, & Johnson, 1999). In addition, reports of war zone stress may change over time and it is not known if AIs are more prone toward overreporting or underreporting war zone stress (Frueh et al., 1998). We do not consider this a serious limitation, however, since all studies of the lifetime occurrence of PTSD and other mental illnesses are retrospective in nature, and previous work has supported the use of AIVVP measures (Beals et al., 2002). Since the CIDI only assesses PTSD symptoms for the three worst self-reported worst events, pre-military PTSD might have been missed in some veterans. In addition, Mississippi PTSD threshold scores are not validated in this population. Although the CIDI directly corresponds to DSM diagnostic symptoms (American Psychiatric Association, 1987), this measure was not used given the construction of the PTSD section. Veterans with significant war-related trauma and PTSD symptomatology might not have ranked the traumatic events among their three worst, whereas the Mississippi PTSD scale was administered to all participants and was specific to their war experiences. The DSM-III-R symptoms of CD have also been criticized for focusing on behavior rather than on underlying personality dynamics of sociopathy, such as the inability to experience remorse. Antisocial behaviors may be normative and even adaptive in the societal contexts of limited earning capacity and rapid social change (Gerstley, Alterman, McLellan, & Woody, 1990). Many AIs live in such communities. We also did not examine the age of onset of CD and personality dysfunction varies according to early vs. late onset (Hill, 2002). There are also differences between subgroups of those with CD according to type of antisocial behaviors (overt vs. covert) (Clarizio, 1997). These findings also may not apply to veterans from other wars. Very few studies have compared groups of veterans but one comparison of Vietnam, World War II, and Korean veterans found Vietnam veterans witnessed more abusive violence and were more frequently the target or observers of killing than other veterans (Fontana & Rosenheck, 1994). The higher levels of war zone stress among Vietnam War veterans could affect the association between conduct disorder and war related PTSD symptoms. However, any inference to American Indian Veterans from other wars is purely speculative.
Despite these limitations, the marked underrepresentation of AIs in other studies of veterans certainly underscores the value of these results. Future efforts should examine reasons why the symptoms of CD are associated with increased levels of war-related PTSD symptoms in AIs. Limited coping capacity and diminished social support are logical candidates for empirical testing. In addition, sub-types of war zone stress such as experiencing atrocities and deprivation have been found to differentially influence PTSD (King et al., 1996; King et al., 1995) and ethnic variations on war zone stress sub-scale loadings have been reported (National Center for Posttraumatic Stress Disorder & The National Center for American Indian and Alaska Native Mental Health Research, 1996). Hence, CD symptoms might pose increased risk of war zone stress if war zone stress sub-scales are examined at a more detailed level. Subgroups of those with CD might also differ according to level of war zone stress. It is also not known whether these results would persist in other military populations such as WWII or Gulf War veterans. Moving beyond the veteran population, determining if symptoms of CD are associated with other traumas and/or PTSD symptoms in non-military AIs may inform efforts to address the disproportionate burden of trauma in the AI population at large (Manson, Beals, Klein, & Croy, 2005).
In summary, in this analysis of AI Vietnam veterans, CD was associated with higher means on a measure of war-related PTSD symptoms, independent of the magnitude of war zone stress. Programs designed to treat PTSD are often less effective for people who have a history of interpersonal disruption, as is often the case in CD (Bailey, 1985). Therefore, symptoms of CD may be common and important elements for providers to consider when treating AI Vietnam veterans with PTSD symptoms. Symptoms of CD may also be an important consideration for the military in assessing appropriateness for combat in AIs, given its strong association with the development of war-related PTSD symptoms.
Acknowledgments
We express our appreciation to Jack Goldberg, Dedra Buchwald, Yvette Roubideaux, Dorrie Rhoades, Jeff Henderson, and other faculty of the Native Elder Research Center for their assistance.
Grant Support: The funding for the American Indian Vietnam Veterans Project was provided by the Veterans Administration as a supplement to a National Institute of Mental Health award (MH43175, SM Manson, PI). This effort was additionally supported by National Institutes of Health/National Institute of Aging (P30 AG15297, SM Manson, PI), Agency for Healthcare Research and Quality (P01 HS10854, SM Manson, PI), and the National Center for Minority Health and Health Disparities (P60 MD000507, SM Manson, PI).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd, revised ed. Washington, DC: Author; 1987. [Google Scholar]
- Bailey JE. Differential diagnosis of posttraumatic stress and antisocial personality disorders. Hosp Community Psychiatry. 1985;36(8):881–883. doi: 10.1176/ps.36.8.881. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Mitchell CM, Spicer P. Cultural specificity and comparison in psychiatric epidemiology: walking the tightrope in American Indian research. Cult Med Psychiatry. 2003;27(3):259–289. doi: 10.1023/a:1025347130953. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Shore JH, Friedman M, Ashcraft M, Fairbank JA, et al. The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: disparities and context. J Trauma Stress. 2002;15(2):89–97. doi: 10.1023/A:1014894506325. [DOI] [PubMed] [Google Scholar]
- Beals J, Spicer P, Mitchell CM, Novins DK, Manson SM, Big Crow CK, et al. Racial disparities in alcohol use: comparison of 2 American Indian reservation populations with national data. Am J Public Health. 2003;93(10):1683–1685. doi: 10.2105/ajph.93.10.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Clarizio HF. Conduct disorder: Developmental considerations. Psychology in the Schools. 1997;34(3):253–265. [Google Scholar]
- Davidson JR, Hughes D, Blazer DG, George LK. Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med. 1991;21(3):713–721. doi: 10.1017/s0033291700022352. [DOI] [PubMed] [Google Scholar]
- Fontana A, Rosenheck R. Traumatic war stressors and psychiatric symptoms among World War II, Korean, and Vietnam War veterans. Psychol Aging. 1994;9(1):27–33. doi: 10.1037//0882-7974.9.1.27. [DOI] [PubMed] [Google Scholar]
- Frueh BC, Brady KL, de Arellano MA. Racial differences in combat-related PTSD: empirical findings and conceptual issues. Clin Psychol Rev. 1998;18(3):287–305. doi: 10.1016/s0272-7358(97)00087-1. [DOI] [PubMed] [Google Scholar]
- Gerstley LJ, Alterman AI, McLellan AT, Woody GE. Antisocial personality disorder in patients with substance abuse disorders: a problematic diagnosis? Am J Psychiatry. 1990;147(2):173–178. doi: 10.1176/ajp.147.2.173. [DOI] [PubMed] [Google Scholar]
- Giancola PR, Tarter RE. Executive cognitive functioning and risk for substance abuse. Psychological Science. 1999;10(3):203–205. [Google Scholar]
- Green BL, Grace MC, Lindy JD, Gleser GC, Leonard A. Risk factors for PTSD and other diagnoses in a general sample of Vietnam veterans. Am J Psychiatry. 1990;147(6):729–733. doi: 10.1176/ajp.147.6.729. [DOI] [PubMed] [Google Scholar]
- Gurley D, Novins DK, Jones MC, Beals J, Shore JH, Manson SM. Comparative use of biomedical services and traditional healing options by American Indian veterans. Psychiatr Serv. 2001;52(1):68–74. doi: 10.1176/appi.ps.52.1.68. [DOI] [PubMed] [Google Scholar]
- Hill J. Biological, psychological and social processes in the conduct disorders. J Child Psychol Psychiatry. 2002;43(1):133–164. doi: 10.1111/1469-7610.00007. [DOI] [PubMed] [Google Scholar]
- Keane TM, Caddell JM, Taylor KL. Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: three studies in reliability and validity. J Consult Clin Psychol. 1988;56(1):85–90. doi: 10.1037//0022-006x.56.1.85. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Foy DW, Gudanowski DM. Prewar factors in combat-related posttraumatic stress disorder: structural equation modeling with a national sample of female and male Vietnam veterans. J Consult Clin Psychol. 1996;64(3):520–531. doi: 10.1037//0022-006x.64.3.520. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Foy DW, Keane TM, Fairbank JA. Posttraumatic stress disorder in a national sample of female and male Vietnam veterans: risk factors, war-zone stressors, and resilience-recovery variables. J Abnorm Psychol. 1999;108(1):164–170. doi: 10.1037//0021-843x.108.1.164. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Gudanowski DM, Vreven DL. Alternative representations of war zone stressors: relationships to posttraumatic stress disorder in male and female Vietnam veterans. J Abnorm Psychol. 1995;104(1):184–195. doi: 10.1037//0021-843x.104.1.184. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Harley R, Lyons MJ, Wolfe J, Simpson JC, Goldberg J, et al. A twin registry study of familial and individual risk factors for trauma exposure and posttraumatic stress disorder. J Nerv Ment Dis. 2002;190(4):209–218. doi: 10.1097/00005053-200204000-00001. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, et al. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. New York: Bruner/Mazel; 1990. [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD. Social epidemiology of trauma among 2 American Indian reservation populations. Am J Public Health. 2005;95(5):851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell CM, Beals J, Novins DK, Spicer P. Drug use among two American Indian populations: prevalence of lifetime use and DSM-IV substance use disorders. Drug Alcohol Depend. 2003;69(1):29–41. doi: 10.1016/s0376-8716(02)00253-3. [DOI] [PubMed] [Google Scholar]
- National Center for Posttraumatic Stress Disorder, & The National Center for American Indian and Alaska Native Mental Health Research. Matsunaga Vietnam Veterans Project. White River Junction: Author; 1996. [Google Scholar]
- Norton IM, Manson SM. Research in American Indian and Alaska Native communities: navigating the cultural universe of values and process. J Consult Clin Psychol. 1996;64(5):856–860. doi: 10.1037//0022-006x.64.5.856. [DOI] [PubMed] [Google Scholar]
- Smith DW, Frueh BC, Sawchuk CN, Johnson MR. Relationship between symptom over-reporting and pre- and post-combat trauma history in veterans evaluated for PTSD. Depress Anxiety. 1999;10(3):119–124. doi: 10.1002/(sici)1520-6394(1999)10:3<119::aid-da5>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Spicer P, Beals J, Croy CD, Mitchell CM, Novins DK, Moore L, et al. The prevalence of DSM-III-R alcohol dependence in two American Indian populations. Alcohol Clin Exp Res. 2003;27(11):1785–1797. doi: 10.1097/01.ALC.0000095864.45755.53. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 8.1. College Station: Stata Corporation; 2003. [Google Scholar]
- Wolfe J, Erickson DJ, Sharkansky EJ, King DW, King LA. Course and predictors of posttraumatic stress disorder among Gulf War veterans: a prospective analysis. J Consult Clin Psychol. 1999;67(4):520–528. doi: 10.1037//0022-006x.67.4.520. [DOI] [PubMed] [Google Scholar]
- World Health Organization. ICD-9: International statistical classification of diseases. Geneva: Author; 1978. [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (Version 1.0) Geneva: World Health Organization; 1994. [Google Scholar]


