Abstract
The protection of poultry from H5N1 highly pathogenic avian influenza A (HPAI) and Newcastle disease virus (NDV) can be achieved through vaccination, as part of a broader disease control strategy. We have previously generated a recombinant influenza virus expressing; (i) an H5 hemagglutinin protein, modified by the removal of the polybasic cleavage peptide and (ii) the ectodomain of the NDV hemagglutinin – neuraminidase (HN) protein in the place of the ectodomain of influenza neuraminidase (Park, M.S., et al., 2006. Proc Natl Acad Sci U S A, 103 (21), 8203–8208). Here we show this virus is attenuated in primary normal human bronchial epithelial (NHBE) cell culture, and demonstrate protection of C57BL/6 mice from lethal challenge with an H5 HA-containing influenza virus through immunisation with the recombinant virus. In addition, in-ovo vaccination of 18-day-old embryonated chicken eggs provided 90% and 80% protection against highly stringent lethal challenge by NDV and H5N1 virus respectively. We propose that this virus has potential as a safe in-ovo live, attenuated, bivalent avian influenza and Newcastle disease virus vaccine.
Keywords: in-ovo, avian influenza, NDV
1. Introduction
Influenza viruses are enveloped, segmented RNA viruses, classified in the family Orthomyxoviridae. Of the three influenza virus genera (Influenzavirus A, B, and C), Influenzavirus A viruses pose the most significant threat to human and animal health, and are subdivided into 16 HA subtypes [1]. Aquatic avian species are the main reservoir of all type A influenza subtypes, and although each subtype is normally non-pathogenic in waterfowl and poultry, subtypes H5 and H7 have occasionally become highly pathogenic in some avian species [2], including gallinaceous poultry [3, 4], and waterfowl [5, 6], and can constitute a serious veterinary health problem.
Between 1996 and the present day, outbreaks of H5N1 highly pathogenic avian influenza (HPAI) in poultry in Asia have caused significant economic and public health difficulties [7]. As of the 25th June 2007, 43 countries have seen outbreaks of H5N1 HPAI (http://www.oie.int) in poultry, resulting in the culling or death of upwards of 200 million poultry. Contrary to HPAI infection in poultry, HPAI infection in domestic ducks is lethal considerably less often, and surviving ducks shed virus over a prolonged period without presenting signs of disease [8]. Transmission of H5N1 viruses between gallinaceous poultry and domestic ducks has been implicated in establishing endemicity of HPAI viruses in Asia, and in the continuing global spread of these viruses [9] [8].
Newcastle disease virus is a non-segmented, negative sense RNA virus of the genus Avulavirus, subfamily Paramyxovirinae, family Paramyxoviridae. It is a highly contagious avian disease agent, transmissible to poultry and over 250 other species of birds. Mortality from infection with virulent strains of NDV can reach 100 percent in poultry flocks unprotected by vaccination [10], and thus vaccination is relied upon in most countries with commercial and non-commercial poultry production.
Traditionally, control of HPAI has been achieved through the culling of infected flocks. However, where HPAI is endemic to a large geographical area, with virus infecting poultry and indigenous wildfowl, the culling of infected poultry flocks alone has not proven sufficient to eradicate disease. Thus, a comprehensive strategy which incorporates each of the following measures has been recommended by OIE/FAO in collaboration with WHO (www.OIE.int) (OIE/FAO International Scientific Conference on Avian Influenza, Paris (France), 7–8th April, 2005) to prevent the outbreak and spread of influenza: (i) sufficient biosecurity in farms and industrial units, (ii) a coordinated regional or national surveillance and diagnostic program, (iii) the culling of all infected poultry, and (iv) the vaccination of uninfected flocks. In addition, immunisation of poultry can benefit human public health by limiting the source of virus responsible for transmission to human or intermediate mammalian hosts.
The development of an efficacious live bivalent vaccine against avian influenza virus and NDV is therefore desirable. Practical considerations regarding the development of such a vaccine include price per dose, speed of production, choice of substrates for growth of virus, efficacy in poultry populations, safety, and acceptance by regulatory agencies [11].
Previously we have reported the rescue of a chimeric bivalent virus which expressed the surface antigens HN of NDV and HA of H5N1 (attenuated by removal of the polybasic cleavage site) [12]. However, this virus provided no protection in 5-week-old chickens from lethal challenge by either H5N1 or by NDV, and the mechanism for this lack of protection was unknown. Furthermore it was unknown whether the antigenic proteins were incorporated into the chimeric virion. Here we provide evidence of virion incorporation of the HA protein, low growth of challenge virus in three-week-old chickens following vaccination in-ovo, and protection of mice against a lethal challenge with an H5 HA-containing mouse adapted influenza virus. In addition, we show the virus to be highly attenuated in differentiated normal human bronchial epithelial (NHBE) culture, and crucially, demonstrate protection to chickens from challenge with both HPAI and NDV following in-ovo vaccination of 18-day-old specific pathogen free (SPF) chicken embryos.
2. Materials and Methods
2.1. Cells
293T cells were maintained in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal calf serum. Cells were maintained at 37°C in 5% CO2. Cryopreserved normal human bronchial cells (NHBE) (Cambrex) were cultivated as previously described [13]. Briefly, cells were passaged twice in bronchial epithelial growth medium (BEGM) (Cambrex) supplemented with retinoic acid and seeded onto Transwell-Clear Permeable filters (12mm diameter, 0.4μm pores; Corning Inc.) at a density of 5 × 104 cells/filter. Before seeding, filters were coated with collagen I from human placenta (Sigma). Cells were submerged for one week in 1:1 mixture of DMEM and BEGM medium containing necessary supplements and growth factors. At full confluence, media was removed from the apical surface and cells maintained at the air-liquid interface for 2 weeks. Medium was replaced every second day when cells were submerged and daily when cells were incubated at the air-liquid interface. Cell differentiation was confirmed by the presence of ciliated cells using monoclonal anti-β-tubulin antibodies (Sigma).
2.2. Viruses
Newcastle disease virus (Hitchner B1 strain), influenza A/WSN/33 (H1N1) and A/PR/8/34 (H1N1) viruses were generated by reverse genetics as previously described ([14], [15], [16]), and propagated in 10-day-old embryonated chicken eggs. Influenza A/Memphis/7/01 (H1N1) was propagated in 10-day-old embryonated chicken eggs.
2.3. Generation of recombinant influenza viruses
Chimeric influenza virus expressing the NDV HN ectodomain (designated VN/HN virus), was generated using reverse genetics as previously described [12]. Briefly, 1μg each of 15 plasmids was transfected into 293T cells in monolayer. Each transfection contained vRNA expression plasmids for the A/Vietnam/1203/04 PA, PB1, PB2, HALo, NP, M and NS segments, and the chimeric HN segment, in addition to protein expression plasmids pCAGGS WSN –PA, PB1, PB2, NP, HA, NA, and NS1 (pCAGGS expression plasmid was kindly provided by J. Miyazaki, Osaka University, Osaka, Japan [17]). The HALo plasmid encodes the HA segment from A/Vietnam/1203/04, modified to remove the encoded polybasic cleavage site. Forty-eight hours following transfection, supernatants were harvested, and transfectant virus passaged into 10-day-old embryonated eggs.
Recombinant WSN/HALo virus was obtained as described above, except that the vRNA expression plasmids encoded A/WSN/33 PA, PB1, PB2, NP, NA, M and NS segments and the A/Vietnam/1203/04 HALo segment [12].
2.4. Western blot of purified virions
Virus particles were purified from the allantoic fluid of 10-day-old embryonated chicken eggs by centrifugation through a sucrose cushion. Virus pellets were resuspended in NTE buffer (NaCl 100mM, Tris pH 7.4 10mM, EDTA 1mM) and further purified through a 30 – 60 % sucrose gradient. Viral proteins were separated under reducing conditions on a 12% SDS-PAGE acrylamide gel, transferred to nitrocellulose membrane and probed with H5 HA specific primary antibody (HALo Mab #8) overnight at 4°C, washed, and probed with rabbit anti-mouse IgG peroxidase conjugate (Dakocytomation; Carpinteria, CA). HA specific protein bands were visualised using ECL protein detection system (PerkinElmer Life Sciences; Boston, MA.).
2.5. Viral growth
Ten day-old embryonated chicken eggs were inoculated with recombinant VN/HN virus, and incubated for 48h at 37°C. Virus present in allantoic fluid was subsequently passaged at limiting dilution in 10-day-old embryonated chicken eggs until maximal growth was obtained. The titre of virus stocks was determined by plaque assay on MDCK cells. Plaque phenotype was examined in the presence and absence of trypsin.
2.6. Growth kinetics of virus in 10-day-old embryonated chicken eggs
Ten day-old embryonated chicken eggs were inoculated with recombinant VN/HN virus. Allantoic fluid was harvested, and subsequently assayed for viral growth at 0h, 24h, 48h, and 72h time points. The titre of virus present in allantoic fluid was determined by plaque assay on MDCK cells.
2.7. Growth kinetics of virus in Normal Human Bronchial Epithelial (NHBE) Cultures
Cultures of differentiated NHBE cells (Cambrex) were washed extensively with growth medium to remove accumulated mucus, and infected with VN/HN or influenza A/Memphis/7/01 (H1N1) virus at an MOI of 0.001 in the absence of exogenous TPCK trypsin. Following infection, cells were maintained at the air-liquid interface, and cell culture supernatant was harvested at 0h, 24h, 48h, 72h and 96h time points, following the addition of medium to the apical surface of the cells for 30 minutes. The titre of virus released into the cell culture supernatant at each time point was determined by plaque assay on MDCK cells.
2.8. Mean Death Time (MDT) of 10-day-old embryonated chicken eggs
The pathogenicity of the VN/HN virus in 10-day-old embryonated eggs was determined by MDT. Groups of six 10-day-old embryonated eggs were inoculated with 100 μl of 10-fold serial dilutions of virus or sham inoculated with PBS by the chorioallantoic sac route. Eggs were incubated at 37°C and candled at 6 hour intervals for 5 days. Eggs were scored as alive or dead, and the time of death recorded. The highest dilution which killed all embryos was determined to be the minimum lethal dose. MDT was calculated as the mean time of death in eggs inoculated with the minimum lethal dose of virus.
2.9 Lethality of WSN/HALo virus in mice
Six- to 8-week-old C57BL/6 mice were intranasally inoculated (n = 4) with 102, 103, 104, 105 or 106 PFU of WSN/HALo virus in 50 μl of phosphate buffered saline (PBS). Animals were monitored daily for mortality, weight loss or other signs of disease over a two week period.
Animals were sacrificed if they lost greater than 20% of their body weight, or showed obvious signs of distress.
2.10. Immunisation and infection in mice
Six to 8-week-old C57BL/6 mice were intranasally inoculated (n = 4) with 105.7 PFU of VN/HN virus in 50 μl of phosphate buffered saline (PBS), or with a mock PBS inoculum. Mice were monitored daily for weight loss or other signs of disease over a two week period. Three weeks after the initial inoculation, mice were boosted by a second intranasal inoculation of 105 PFU of VN/HN virus. Vaccinated mice were challenged three weeks later with 106 PFU of WSN/HALo virus which is equivalent to 101.8 (62.5) MLD50 by intranasal route, and monitored daily for weight loss or other signs of disease over a two week period.
2.11. Immunisation and infection in chickens
Groups of 2 week-old SPF White Leghorn chickens (n = 20) were inoculated with 107.2 EID50 of VN/HN virus in 0.1 mL of PBS either intranasally (IN) or by eyedrop, or sham inoculated with PBS by both IN and eyedrop routes. This dose was 102 EID50 greater than the standard ND virus vaccine field dose. At 5 weeks of age, 10 chickens from each group were challenged with either 106.1 EID50 of influenza A/Vietnam/1203/04 (H5N1) by intranasal route or with 105.3 EID50 of the Fontana strain of vNDV by intranasal/eyedrop (50/50) route in 0.1 mL of PBS.
2.12. Immunisation in-ovo and challenge in chicken
18-day-old SPF White leghorn chicken embryos were inoculated in-ovo with 105.2 EID50 of VN/HN virus or sham inoculated with 0.1 mL of PBS. At 3 weeks post hatching, 10 chickens from each vaccinated group were challenged intranasally with 106.1 EID50 of influenza A/Vietnam/1203/04 (H5N1) virus, or challenged by intranasal/eyedrop route with 105.2 EID50 of Fontana strain of vNDV in 0.1 mL PBS. Oropharyngeal and cloacal swabs were taken 2 days post-challenge and assayed by quantitative real-time RT-PCR (RRT-PCR) for AI virus and NDV for respective challenge groups.
2.13. Quantitative Real-time RT-PCR (qRRT-PCR)
RNA was extracted from oral or cloacal swab material as follows: 100μl of swab material was added to 750μl of Trizol LS (Invitrogen Inc., Carlsbad, CA) and 150μl RNA grade water. The sample was mixed by vortexing and incubated at room temperature for 10 minutes, then 200μl of chloroform was added. The samples were mixed by vortexing and incubated at room temperature for ten minutes then centrifuged for 15 minutes at approximately 12 000×g. The aqueous phase was collected and RNA isolation was completed by extracting the RNA from the aqueous phase with the MagMAX AI/ND viral RNA isolation kit (Ambion, Inc. Austin, TX) in accordance with the kit instructions using the KingFisher magnetic particle processing system (Thermo Scientific, Waltham, MA).
The A/Vietnam/1203/04 (H5N1) HPAI virus and Fontana strain of vNDV were used as the source of the RNA for the quantitative standards for their respective treatment groups. Virus stocks in allantoic fluid were diluted in brain heart infusion broth (BHI) (Becton-Dickinson, Sparks, MD) and titrated in embryonated chicken eggs by standard methods [18]. Whole virus RNA was extracted from ten-fold dilutions of titrated virus as described for swab material. Real-time RT-PCR for the influenza matrix gene or avian paramyxovirus-type 1 matrix gene was performed as previously described [19, 20]. Virus titres in samples were calculated based on the standard curves by the Smart Cycler II (Cepheid, Inc. Sunnyvale, CA) software.
2.14. Statistical methods
All statistical operations were performed with Sigma Stat Version 2.03 (SPSS, 1992–1997). The unpaired t-test was used to compare two groups if the groups contained normally distributed data with equal variance. If these requirements were not met, the Mann-Whitney test (rank sum test) was used instead. P-values < 0.05 were considered statistically significant.
For statistical purposes, negative RRT-PCR samples were assigned titre values equal to the detection limit of the RRT-PCR run minus 100.1 EID50/mL. Mean titres from groups containing negative RRT-PCR values were reported with a ≤ symbol. The detection limit of each RRT-PCR run was calculated from the standard curve, setting the cycle threshold value equal to the number of cycles run. Negative HI samples were assigned a well number of 0.01.
3.0. Results
3.1. Biological characterization of the virus
To determine the stability of the HALo and NA-HN genes in the VN/HN virus, we passaged the recombinant virus 10 times in 10-day-old embryonated SPF chicken eggs. RT-PCR was performed on virion RNA from the tenth passasge, and the sequence of the recombinant NA-HN segment was shown to be unchanged from the original plasmid sequence. The sequence of the HALo segment remained unchanged at the polybasic cleavage site, exhibiting the avirulent consensus amino acid sequence PQRETR ↓ G. One amino acid change was noted in the HA protein around the region of the receptor binding site (S203F; H3 numbering). Virus was shown to require TPCK trypsin for efficient growth in MDCK cells (data not shown).
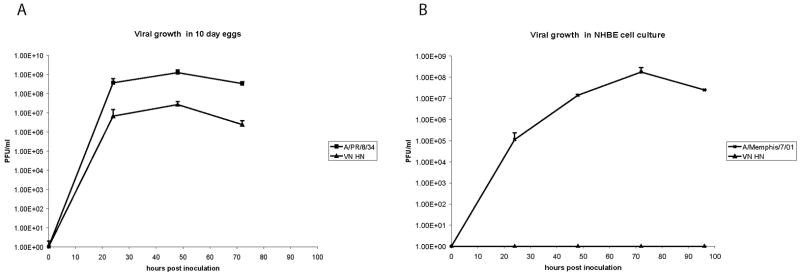
3.2. Incorporation of HALo protein into the virion
Incorporation of HALo protein into virions was confirmed by Western blot. Bands corresponding to the HA0 and HA1 proteins were observed at the expected molecular sizes for VN/HN virus and control WSN/HALo virus, but were not observed for WSN virus or mock extract (Fig 1A). The identity of the HALo protein was verified by PNGase F treatment: following deglycosylation, Western blot analysis demonstrated migration of HA0 and HA1 protein bands of the expected molecular sizes of 62.5 and 32 kDa respectively (Fig 1B). The most likely reason for the difference in mobility of the H5 HA proteins derived from WSN/HALo virus and VN/HN virus, as observed in Fig. 1, is a difference in glycosylation of the two proteins. WSN/HALo virus was grown in MDCK cells, while VN/HN virus was grown in eggs. It has been previously established that the HA molecule from egg-grown influenza virus is glycosylated to a lesser extent, and the glycosylation is less branched in nature, relative to the HA of MDCK cell-grown virus [21] [22] resulting in differences in mobility of the proteins in SDS-PAGE.
Fig. 1.
Western blot analysis of purified virion preparations. A. Incorporation of H5 specific HALo protein into the VN/HN virion is shown by the presence of specific bands corresponding to the uncleaved HA0 and to the HA1 subunit of hemagglutinin. Corresponding HA0 and HA1 bands were also present in the WSN/HALo lane (positive control), but not in WSN virus and mock-infected lanes (negative controls). B. Treatment of VN/HN sample with PNGase F leads to the deglycosylation of the HALo protein, visualised as faster migrating forms of the HA0 protein and the HA1 subunit. No bands were present in the WSN lanes (negative control).
3.3. Growth of VN/HN virus in 10-day-old embryonated eggs
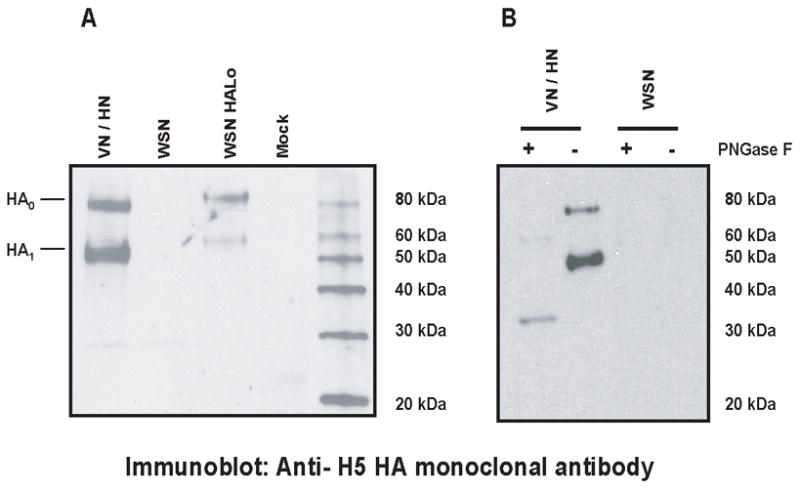
Multicycle growth of the bivalent virus VN/HN was studied in 10-day-old embryonated SPF chicken eggs. Infections were carried out at a low MOI (100 PFU/egg) and infectious virus in the allantoic fluid of eggs was titrated on MDCK cells in the presence of TPCK trypsin at the time points indicated (Fig. 2a). The VN/HN virus replicated in embryonated chicken eggs to a titre of 107 PFU/mL, which corresponds to approximately 2 logs lower growth than that observed for the high growth influenza A/PR/8/34 virus.
Fig. 2.
A. Growth of VN/HN virus in 10-day-old embryonated eggs. Eggs were infected with A/PR/8/34 (H1N1) virus or with VN/HN virus at a low MOI (100 PFU/egg). Virus in allantoic fluid was quantified by plaque assay on MDCK cells at the timepoints indicated. B. Growth of VN/HN virus in NHBE culture. Normal human bronchial epithelial cultures were infected at an MOI of 0.001 with A/Memphis/7/01 (H1N1) or with VN/HN virus. Virus released to the culture supernatant was quantified by plaque assay on MDCK cells at the timepoints indicated.
3.4. Mean Death Time
Ten day-old embryonated chicken eggs inoculated with VN/HN virus demonstrated a MDT of 81h, and maximum titres of virus were achieved by 48h (Fig. 2a). Similarly, influenza A/PR/8/34 has a MDT in 10 day-old-eggs of greater than 96h [23], while peak titres are achieved by 48h. Both viruses are therefore suitable for growth in eggs. In contrast, H5N1 HPAI viruses have been shown to have a MDT of around 44h [23], which prevents the use of 10-day-old eggs as a substrate for the growth of these viruses. These data demonstrate that the bivalent VN/HN virus is sufficiently attenuated for the use of embryonated eggs as a substrate for virus growth.
3.5. Growth of virus in mammalian models
3.5.1. Growth of VN/HN virus in Differentiated Normal Human Bronchial Epithelial (NHBE) cell cultures
To determine the ability of the bivalent virus to grow in human cells, multicycle growth of the VN/HN virus or of a human control virus, influenza A/Memphis/7/01 (H1N1) was carried out in differentiated normal human bronchial epithelial (NHBE) cultures. Infections were carried out at a low MOI (0.001) in the absence of exogenous trypsin and infectious virus released to the cell culture supernatant was titrated on MDCK cells at the time points indicated in figure 2b. The VN/HN virus was shown to be incapable of replication in differentiated NHBE culture, while the control virus, A/Memphis/7/01 (H1N1) could replicate to a titre of 108 PFU/mL under identical conditions (Fig. 2b).
3.5.2. Lethality of WSN/HALo virus in mice
We required a mouse lethal influenza virus bearing an H5 HA protein, to be used as a challenge virus in a vaccination - challenge study. To this end, we engineered a recombinant virus containing seven gene segments from the mouse adapted influenza strain A/WSN/33, and the HA segment from A/Vietnam/1203/04, modified by the removal of the polybasic cleavage site. The 50% mouse lethal dose (MLD50) of the resultant WSN/HALo virus was determined. Groups of four animals were inoculated intranasally with 102, 103, 104, 105 or 106 pfu, as determined by plaque assay on MDCK cells. The status of each mouse was then monitored daily for weight loss and signs of disease. The results obtained (shown in Fig 3a) were used to calculate the MLD50 by the method of Reed and Muench [24]. The 50% lethal dose was found to be 104.2 PFU, indicating that WSN/HALo virus is suitable for use as a lethal H5 HA-containing challenge virus in vaccination studies.
Fig. 3.
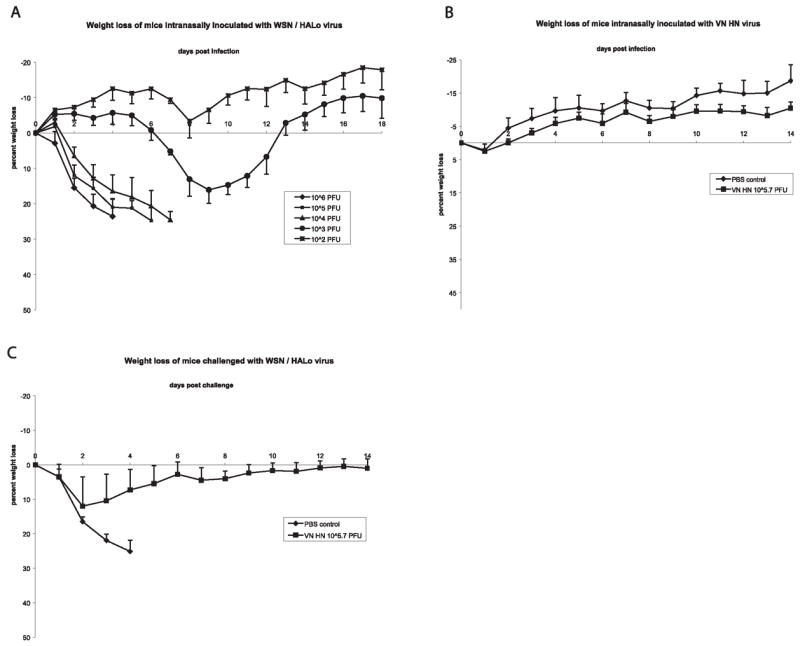
Fig. 3A. Suceptibility of mice to infection with WSN/HALo virus. Groups of C57BL/6 mice (n = 4) were intranasally inoculated with 102 103 104 105 or 106 PFU of WSN/HALo virus. Body weight was assessed daily and is expressed as the average percent change in body weight for each group of animals. B. Body weight of mice following vaccination with VN/HN virus. C57BL/6 mice (n = 4), inoculated with 105.7 PFU of VN/HN virus, or sham vaccinated with PBS (n = 4), demonstrated no weight loss or other signs of disease over a two week period.
C. Protection of mice from lethal challenge with WSN/HALo virus. PBS treated control mice (n = 4) and mice vaccinated with 105.7 PFU of VN/HN virus (n = 4) followed by a boost with 105 PFU of VN/HN virus three weeks post vaccination were challenged with 62.5 MLD50 of WSN/HALo virus at six weeks post vaccination. Body weights of mice were followed for 14 days. VN/HN vaccinated mice demonstrated a slight and transient weight loss between days two and five, whereas all PBS inoculated control mice rapidly lost weight and were sacrificed on day 4 post challenge.
3.5.3. Immunisation and challenge in mice
Groups of 4 mice (C57BL/6) were infected intranasally with 105.7 PFU of VN/HN virus or mock infected with PBS and monitored daily for weight loss and other symptoms of disease. Infected mice exhibited no signs of disease, and no difference in weight was observed between the PBS control group and the infected group (Fig. 3b.). All animals in the infected group recovered fully. Mice were boosted at three weeks post vaccination with 105 PFU of VN/HN virus or PBS as appropriate. At 3 weeks post boost, 25% of mice infected with VN/HN virus had developed a quantifiable increase in antibody to H5 HA as assayed by HI. Upon challenge with a lethal dose of WSN/HALo virus (62.5 MLD50), at three weeks post boost, 100% of VN/HN vaccinated mice were protected from death, and displayed only a modest and transient weight loss between days 2 and 5 post challenge. In contrast, all sham inoculated mice died when challenged with WSN/HALo virus (Fig. 3c).
3.6. Immunisation in-ovo and challenge in chickens
To examine the efficacy of the VN/HN virus as a vaccine, 18-day-old embryos of SPF chickens were vaccinated with 105.2 EID50 of VN/HN virus. 75% of chickens developed quantifiable HI titres to NDV by three weeks of age while only 30% of chickens had measurable immune response to H5 avian influenza virus and the titres were minimal (Table 1). No sham inoculated birds developed HI titres to either virus. Upon challenge with highly virulent NDV (105.2 EID50), at three weeks of age, 90% of VN/HN vaccinated chickens were protected from death and upon challenge with influenza A/Vietnam/1203/04 (H5N1) (106.1 EID50), 80% of VN/HN vaccinated chickens were protected from death. In contrast, all sham vaccinated chickens died when challenged with either virulent virus. Ninety-four percent of surviving chickens mounted a quantifiable anamnestic response to NDV, and 88% of surviving chickens mounted a quantifiable anamnestic response to H5 avian influenza virus. Both of the VN/HN-vaccinated groups displayed a significant increase in protective antibody titre 14 days post-challenge. Although all of the VN/HN-vaccinated birds that died lacked detectable antibodies to both AI virus and vNDV before challenge, not all of the VN/HN-vaccinated birds lacking detectable antibodies died. These survivors may have possessed antibodies detectable by a more sensitive assay, and cellular immunity could have helped clear the infection.
Table 1.
Mortality, serology, and quantitative RT-PCR analysis of viral shedding in White Leghorn chickens challenged with A/VN/1203/04 or NDV Fontana at three weeks of age following in-ovo vaccination.
| Vaccine group | Challenge virus | Mortality (MDT)a | Serologyb |
Quantitative RRT-PCR analysis
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 21 DPH
|
14 DPC
|
Positive samples
|
Mean virus titre/mL (S.D.)c |
|||||||
| AIV | B1 | AIV | B1 | oral | cloacal | Oral | cloacal | |||
| sham | AIV | 10/10 (1.6) | 0/10 | 0/10 | NA | NA | 10/10 | 10/10 | 7.6 (0.5) | 7.4 (0.5) |
| VN/HN | AIV | 2/10 (2.5) | 3/10 (6) | 7/10 (32) | 8/8 (30) | 7/8 (56) | 3/10 | 1/10 | ≤4.1 (1.5)d | ≤4.9 (1.0)d |
| sham | NDV | 10/10 (5.7) | 0/10 | 0/10 | NA | NA | 10/10 | 8/10 | 6.0 (0.5) | ≤4.9 (0.7) |
| VN/HN | NDV | 1/10 (6.0) | 3/10 (7) | 8/10 (24) | 7/9 (11) | 9/9 (891) | 8/10 | 0/10 | ≤5.1 (0.7) | ≤4.0 (0)e |
MDT, mean death time in days. All birds displaying clinical signs (morbidity) died.
Hemagglutination inhibition assay performed 21 days post-hatch (DPH) and 14 days post-challenge (DPC). The proportion of positive birds is indicated, with the geometric mean titres in parentheses.
Titres calculated from quantitative RRT-PCR standard curve and expressed as log10EID50/mL. Unless otherwise indicated, the mean and median titres for each group did not differ by more than 100.2 EID50/mL.
Because most of the RRT-PCR samples were negative, the median titres/mL were equal to the values assigned to the negative AIV samples (3.3 for oral swabs and 4.6 for cloacal swabs).
4.0 is the titre/mL value assigned to negative RRT-PCR NDV cloacal swabs.
The challenge HPAI virus replicated to very high titres in the respiratory and alimentary tracts of all sham vaccinated birds while significantly fewer chickens in the VN/HN vaccine group had recoverable challenge virus from respiratory and alimentary tracts and of much lower titres (Table 1). By contrast, the challenge vNDV replicated to high titres in respiratory tract of all sham vaccinated chickens and was also recovered from alimentary tract in most chickens but at very low titres. In the VN/HN vaccinated chickens, similar numbers of birds had virus in respiratory tract but the titres were significantly lower than those in the sham group. No challenge vNDV was recovered from the alimentary tract of vaccinated birds.
Significantly less challenge virus was shed from the respiratory and intestinal tracts of the VN/HN-vaccinated group compared to the sham-vaccinated group 2 days post-challenge with A/VN/1203/04. If the medians for the VN/HN-vaccinated group are used for comparison (see footnotes for Table 1), at least a 103–4 fold reduction in shedding of the challenge virus was achieved. The reduction in viral shedding observed in VN/HN-vaccinated birds following challenge with vNDV was smaller, but statistically significant. The mean titre of oral swab samples from the VN/HN-vaccinated group was at least 100.9 fold lower than that from the sham-vaccinated group, and none of the cloacal swab samples from the VN/HN-vaccinated group were virus positive.
3.7. Immunisation and challenge in chickens
Following a single vaccination of VN/HN virus in 2-week-old white leghorn chickens, no quantifiable HI titres to NDV or to H5 avian influenza were observed in sera by three weeks post vaccination (Table 2). No sham inoculated birds developed HI titres to either virus. Upon challenge with either the Fontana strain of vNDV or A/Vietnam/1203/04 (H5N1) HPAI virus, at three weeks post vaccination, no protection was observed in any birds. All sham inoculated chickens died when challenged with either vNDV or HPAI virus. The VN/HN virus grew to very low titres in 2-week-old chickens, and interestingly, was detected only in cloacal swabs but not from tracheal swabs of vaccinated birds as shown in Table 2. This minimal replication in the birds may explain the lack of immune response and the absence of protection from challenge.
Table 2.
HI, serology and survival of White Leghorn chickens challenged with A/VN/1203/04 or NDV Fontana, following vaccination at 2 weeks of age.
| Vaccine Group * | Challenge Virus | Morbidity | Mortality (MDT) | HI Serology | Virus isolation3 days post vaccination (EID50 log 10/mL) | ||||
|---|---|---|---|---|---|---|---|---|---|
| 21 DPV | 14 DPC | ||||||||
| AIV | B1 | AIV | B1 | oral | cloacal | ||||
| VN/HN Eyedrop | NDV Fontana | 10/10 | 10/10 (4.0) | 0/10 | 0/10 | NA | NA | 0/5 | 5/5 (1.28) |
| VN/HN Eyedrop | VN/1203/04 | 10/10 | 10/10 (2.0) | 0/10 | 0/10 | NA | NA | 0/5 | 5/5 (1.47) |
| Sham | NDV Fontana | 10/10 | 10/10 (4.0) | 0/10 | 0/10 | NA | NA | ND | ND |
| Sham | VN/1203/04 | 10/10 | 10/10 (1.5) | 0/10 | 0/10 | NA | NA | ND | ND |
Chickens were vaccinated with VN HN (105.2 EID50), or PBS (sham) followed by vNDV (105.2 EID50) or influenza A/Vietnam/1203/04 virus (106.1 EID50). Mortality is shown as number of dead birds/no of infected chickens. Mean death time is shown in parenthesis. HI titres are shown as number of chickens with HI positive serum/number of chickens vaccinated. Geometric mean titre is shown in parenthesis. NA: not applicable.
n = 10 chickens per vaccine group.
4.0. Discussion
We describe the characterisation of an attenuated live bivalent influenza virus with potential for use as a vaccine against the economically important pathogens H5 HPAI virus and vNDV. We have previously generated a recombinant influenza virus expressing the ectodomain of the HN protein from NDV B1 virus in place of the influenza neuraminidase ectodomain [12]. As this virus expresses the major antigenic proteins of both influenza virus and NDV, the H5 HA protein and the HN protein respectively, we reasoned that it should elicit immune responses against both agents. The evaluation of the bivalent virus for efficacy as a live attenuated vaccine confirmed that a single inoculation into 18-day-old chicken embryos provided protection against a lethal challenge of Fontana strain of vNDV in 90% of vaccinated chickens at three weeks of age, with significant reduction in challenge virus replication in respiratory and alimentary tracts. Furthermore, HI antibody responses to NDV were generated in these chickens, and titres were boosted following challenge. Similarly, protection against a lethal challenge of HPAI was observed at three weeks of age in 80% of VN/HN vaccinated chickens, with a significant reduction in the number of infected chickens and decreased virus replication in respiratory and alimentary tracts. These results demonstrate the potential of a bivalent influenza virus for in-ovo immunisation against NDV and HPAI. Detailed hatchability records were not maintained during the present work, and future studies would be required to examine the impact of in-ovo vaccination with this virus on hatchability. The purpose of the initial study was to provide a proof of concept that in-ovo administration would produce post hatch protective immunity against virulent challenge and not to investigate hatchability, which would require a study involving several hundred eggs. Post hatch vaccination with VN/HN vaccine virus failed to elicit sufficient viral replication to provide measurable serological response and no protection resulted from lethal HPAI virus and vNDV challenge. This was presumably due to over-attenuation of the virus which prevented efficient growth in the post-hatch bird, which would possess a more fully developed immune system than that present in an 18 day old chicken embryo.
The use of an influenza virus as a live attenuated vaccine vector has several advantages. Firstly, influenza is known to produce a strong humoral and cell mediated immune response, and as an RNA virus, cannot integrate into the host cell genome. Furthermore, the virus grows quickly in embryonated eggs and requires minimal downstream processing, rendering the production of a live attenuated virus cost-effective. These benefits are amplified in the case of a multivalent vaccine, where one immunisation can lead to protection from two pathogens. Furthermore, the use of an in-ovo vaccination strategy allows for the protection of chickens from as early as three weeks of age. Thus we propose that recently developed reverse genetics techniques [15] are ideal for the generation of effective, economical and convenient bivalent live attenuated vaccines.
In addition to the influenza virus-based bivalent vaccine virus described herein, three NDV-based bivalent, live attenuated vaccine viruses have recently been described [12] [25] [26].
Several properties shared by NDV and influenza virus make them suitable starting points for the design of live attenuated vaccines. Both viruses possess an RNA genome which does not integrate into host cell DNA, and the ability to stably incorporate foreign genes over multiple passages in culture. The bivalent vaccine approach can therefore be applied to either influenza virus or NDV platforms. The value of the bivalent approach applies equally to vaccines based on both viruses. Firstly, this approach avoids the difficulties associated with simultaneous vaccination using multiple live attenuated viruses (the presence of one virus may have adverse effects on the growth or immunogenicity of a second virus). Secondly, the bivalent vaccine approach lowers the burden of cost for vaccination, both at the stage of vaccine production and administration. Thirdly, both the NDV and influenza virus based vaccine approaches are compatible with the DIVA (Differentiating Infected from Vaccinated Animal) strategy for vaccination. In vaccination with either bivalent NDV or influenza virus based vaccine, the recipient animals will lack an immune response to antigen which is present in the natural virus. One difference between the NDV based vaccine viruses and the influenza based bivalent vaccine is that the current influenza based virus is too highly attenuated to provide protection against challenge when administered to two week old chickens; the NDV based viruses are not over-attenuated to this degree. It remains to be seen whether further research can produce an influenza based vaccine which will provide comparable protection to that shown by the NDV based viruses in two week old birds. Conversely, it remains to be demonstrated whether NDV based vaccines would be efficacious when administered in-ovo. A MDT in egg of >80 h observed with NDV based bivalent virus (Park et al., 2006) suggests that NDV is likely to be suitable for in-ovo vaccination in addition to its application in the vaccination of older birds.
The high pathogenicity of currently circulating H5N1 strains creates two difficulties for vaccine production: (i) the viruses are too virulent to be grown to a maximum titre in 10-day-old embryonated eggs, the industry standard substrate for the production of inactivated influenza vaccines, and (ii) high containment facilities are required in order to protect workers and the environment. Both issues have been addressed herein by the use of reverse genetics technology. The removal of nucleotides encoding the polybasic cleavage site in the HA resulted in the generation of an attenuated recombinant virus suitable for growth in embryonated chicken eggs. The virus grew to maximal titre in 48h, considerably shorter than its MDT of 81h, demonstrating that 10-day-old eggs can be safely and conveniently used for the production of the vaccine. The attenuated nature of our influenza based bivalent virus was further confirmed in two week old White Leghorn chickens. In contrast to H5N1 HPAI influenza virus, which killed chickens with a mean death time of 1.6 days (Table 1), our live attenuated bivalent virus did not cause death or signs of disease in chickens, grew to very low titres, detectable only in the cloaca, and was actually over-attenuated for use as a vaccine in chickens of this age; i.e. not producing a protective immune response.
It was observed that there was a change in the hemagglutinin protein at residue 203 (H3 numbering) which altered a seine to a phenylalanine. While the change of residue at position 203 of the hemagglutinin protein may simply be a neutral mutation resulting from passage of the virus at limiting dilution in eggs, it is also possible that the alteration was an adaptive mutation to growth in eggs. Egg adaptive changes in the hemagglutinin molecule have been previously reported for human influenza A virus [27]. Alternatively, the mutation in the hemagglutinin molecule may have acted to compensate for a putative imbalance between the hemagglutination and neuraminidase activities of the virus, which may have arisen as a result of the replacement of the wt neuraminidase with the NA-HN protein. Further experiments are necessary to determine the exact role, if any, played by the hemagglutinin S203F mutation to the fitness of the virus.
In the mouse model, we observed that VN/HN virus offered complete protection from challenge with a lethal dose (62.5 MLD50) of a mouse adapted recombinant virus containing the A/Vietnam/1203/04 HALo segment, indicating that influenza based bivalent viruses may also be suitable as mammalian vaccines. A bivalent influenza based virus vaccine with a background of the mouse adapted strain of influenza A/WSN/33, which incorporated the ectodomain of Sendai virus HN in place of the ectodomain of the WSN neuraminidase has recently been reported. This virus afforded protection to mice from challenge with both a mouse adapted influenza strain, and a mouse adapted parainfluenza virus [28].
Our recombinant vaccine need not be grown in high containment facilities because while the introduction of a polybasic cleavage site into the HA of H5 and H7 influenza viruses correlates strongly with pathogenicity [29, 30], over at least 10 passages in eggs, the virus was shown to be stable in the region of the polybasic cleavage site, with no introduction or substitution of nucleotides observed. Furthermore, an assessment of the growth of the virus in differentiated NHBE cell culture (Fig. 2b) demonstrated that, while contemporary human influenza A virus replicated to high titres, the bivalent virus was unable to grow to detectable titres. Thus the bivalent virus would not be predicted to replicate or cause disease in humans, and this attenuation suggests that the VN/HN virus can be used safely for the manufacture of live attenuated vaccine. In mice, doses of up to 105.7 PFU of the bivalent virus were shown to be tolerated with no observable ill-effects. In contrast, the wild-type A/Vietnam/1203/04 (H5N1) virus has been shown to be highly pathogenic in mice, with a 50% mouse lethal dose as low as 102.2 EID50 [31].
In summary, we have demonstrated that an influenza based live attenuated bivalent vaccine can protect chickens against mortality and morbidity from both HPAI and Newcastle disease virus. Furthermore we would predict that similar bivalent viruses could be applied to the prevention of disease caused by other pathogens in many animal hosts. Future studies should be conducted with the attenuated bivalent VN/HN vaccine to verify the lack of reduced hatchability following in-ovo vaccination, the potential use of the in-ovo vaccination as a priming vaccine followed by post-hatch boost with other AI vaccines, and a risk assessment on environmental safety of the attenuated bivalent VN/HN vaccine.
Acknowledgments
We thank Joan Beck for excellent technical assistance. This work was supported by grants (to A.G.-S. and P.P.) from the National Institutes of Health (NIH), and the U.S. Department of Agriculture, Agricultural Research Service (D.S.). P.P is a senior fellow of the Ellison Medical Foundation. Partial support of this work was provided by NIH grants UO1AI070469 (Live Attenuated Vaccines for Epidemic and Pandemic Flu) HHSN2662000700010C (Center for Research on Influenza Pathogenesis), U54 AI057158-04 (Northeast Biodefense Center) and 1 UC19 AI062623-023 (Center For Investigating Viral Immunity and Antagonism)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fouchier RA, Munster V, Wallensten A, Bestebroer TM, Herfst S, Smith D, et al. Characterization of a novel influenza A virus hemagglutinin subtype (H16) obtained from black-headed gulls. J Virol. 2005;79(5):2814–22. doi: 10.1128/JVI.79.5.2814-2822.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Becker WB. The isolation and classification of Tern virus: influenza A-Tern South Africa--1961. J Hyg (Lond) 1966;64(3):309–20. doi: 10.1017/s0022172400040596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, et al. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci U S A. 2004;101(5):1356–61. doi: 10.1073/pnas.0308352100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia M, Suarez DL, Crawford JM, Latimer JW, Slemons RD, Swayne DE, et al. Evolution of H5 subtype avian influenza A viruses in North America. Virus Res. 1997;51(2):115–24. doi: 10.1016/s0168-1702(97)00087-7. [DOI] [PubMed] [Google Scholar]
- 5.Capua I, Mutinelli F, Pozza MD, Donatelli I, Puzelli S, Cancellotti FM. The 1999–2000 avian influenza (H7N1) epidemic in Italy: veterinary and human health implications. Acta Trop. 2002;83(1):7–11. doi: 10.1016/s0001-706x(02)00057-8. [DOI] [PubMed] [Google Scholar]
- 6.Sturm-Ramirez KM, Ellis T, Bousfield B, Bissett L, Dyrting K, Rehg JE, et al. Reemerging H5N1 influenza viruses in Hong Kong in 2002 are highly pathogenic to ducks. J Virol. 2004;78(9):4892–901. doi: 10.1128/JVI.78.9.4892-4901.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horimoto T, Kawaoka Y. Influenza: lessons from past pandemics, warnings from current incidents. Nat Rev Microbiol. 2005;3(8):591–600. doi: 10.1038/nrmicro1208. [DOI] [PubMed] [Google Scholar]
- 8.Sturm-Ramirez KM, Hulse-Post DJ, Govorkova EA, Humberd J, Seiler P, Puthavathana P, et al. Are ducks contributing to the endemicity of highly pathogenic H5N1 influenza virus in Asia? J Virol. 2005;79(17):11269–79. doi: 10.1128/JVI.79.17.11269-11279.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen H, Smith GJ, Zhang SY, Qin K, Wang J, Li KS, et al. Avian flu: H5N1 virus outbreak in migratory waterfowl. Nature. 2005;436(7048):191–2. doi: 10.1038/nature03974. [DOI] [PubMed] [Google Scholar]
- 10.Alexander DJ. Newcastle disease and other avian paramyxoviruses. Rev Sci Tech. 2000;19(2):443–62. doi: 10.20506/rst.19.2.1231. [DOI] [PubMed] [Google Scholar]
- 11.Palese P. Making better influenza virus vaccines? Emerg Infect Dis. 2006;12(1):61–5. doi: 10.3201/eid1201.051043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park MS, Steel J, Garcia-Sastre A, Swayne D, Palese P. Engineered viral vaccine constructs with dual specificity: avian influenza and Newcastle disease. Proc Natl Acad Sci U S A. 2006;103(21):8203–8. doi: 10.1073/pnas.0602566103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gray TE, Guzman K, Davis CW, Abdullah LH, Nettesheim P. Mucociliary differentiation of serially passaged normal human tracheobronchial epithelial cells. Am J Respir Cell Mol Biol. 1996;14(1):104–12. doi: 10.1165/ajrcmb.14.1.8534481. [DOI] [PubMed] [Google Scholar]
- 14.Nakaya T, Cros J, Park MS, Nakaya Y, Zheng H, Sagrera A, et al. Recombinant Newcastle disease virus as a vaccine vector. J Virol. 2001;75(23):11868–73. doi: 10.1128/JVI.75.23.11868-11873.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fodor E, Devenish L, Engelhardt OG, Palese P, Brownlee GG, Garcia-Sastre A. Rescue of influenza A virus from recombinant DNA. J Virol. 1999;73(11):9679–82. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia-Sastre A, Egorov A, Matassov D, Brandt S, Levy DE, Durbin JE, et al. Influenza A virus lacking the NS1 gene replicates in interferon-deficient systems. Virology. 1998;252(2):324–30. doi: 10.1006/viro.1998.9508. [DOI] [PubMed] [Google Scholar]
- 17.Miyazaki J, Takaki S, Araki K, Tashiro F, Tominaga A, Takatsu K, et al. Expression vector system based on the chicken beta-actin promoter directs efficient production of interleukin-5. Gene. 1989;79(2):269–77. doi: 10.1016/0378-1119(89)90209-6. [DOI] [PubMed] [Google Scholar]
- 18.Swayne DE, Senne DA, Beard CW. Avian Influenza. In: Swayne DE, editor. A Laboratory Manual for the Isolation and Identification of Avian Pathogens. Vol. 4. Pennsylvania: American Association of Avian Pathologists, Kennett Square; 1998. pp. 150–55. [Google Scholar]
- 19.Spackman E, Suarez DL. Use of a novel virus inactivation method for a multicenter avian influenza real-time reverse transcriptase-polymerase chain reaction proficiency study. J Vet Diagn Invest. 2005;17(1):76–80. doi: 10.1177/104063870501700117. [DOI] [PubMed] [Google Scholar]
- 20.Wise MG, Suarez DL, Seal BS, Pedersen JC, Senne DA, King DJ, et al. Development of a real-time reverse-transcription PCR for detection of newcastle disease virus RNA in clinical samples. J Clin Microbiol. 2004;42(1):329–38. doi: 10.1128/JCM.42.1.329-338.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inkster MD, Hinshaw VS, Schulze IT. The hemagglutinins of duck and human H1 influenza viruses differ in sequence conservation and in glycosylation. J Virol. 1993;67(12):7436–43. doi: 10.1128/jvi.67.12.7436-7443.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Romanova J, Katinger D, Ferko B, Voglauer R, Mochalova L, Bovin N, et al. Distinct host range of influenza H3N2 virus isolates in Vero and MDCK cells is determined by cell specific glycosylation pattern. Virology. 2003;307(1):90–7. doi: 10.1016/s0042-6822(02)00064-8. [DOI] [PubMed] [Google Scholar]
- 23.Horimoto T, Takada A, Fujii K, Goto H, Hatta M, Watanabe S, et al. The development and characterization of H5 influenza virus vaccines derived from a 2003 human isolate. Vaccine. 2006;24(17):3669–76. doi: 10.1016/j.vaccine.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 24.Reed LJ, Muench H. A simple method for estimating fifty percent end points. Am J Hyg. 1938;27:493–97. [Google Scholar]
- 25.Veits J, Wiesner D, Fuchs W, Hoffmann B, Granzow H, Starick E, et al. Newcastle disease virus expressing H5 hemagglutinin gene protects chickens against Newcastle disease and avian influenza. Proc Natl Acad Sci U S A. 2006;103(21):8197–202. doi: 10.1073/pnas.0602461103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ge J, Deng G, Wen Z, Tian G, Wang Y, Shi J, et al. Newcastle disease virus-based live attenuated vaccine completely protects chickens and mice from lethal challenge of homologous and heterologous H5N1 avian influenza viruses. J Virol. 2007;81(1):150–8. doi: 10.1128/JVI.01514-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Widjaja L, Ilyushina N, Webster RG, Webby RJ. Molecular changes associated with adaptation of human influenza A virus in embryonated chicken eggs. Virology. 2006;350(1):137–45. doi: 10.1016/j.virol.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 28.Maeda Y, Hatta M, Takada A, Watanabe T, Goto H, Neumann G, et al. Live bivalent vaccine for parainfluenza and influenza virus infections. J Virol. 2005;79(11):6674–9. doi: 10.1128/JVI.79.11.6674-6679.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klenk HD, Rott R, Orlich M. Further studies on the activation of influenza virus by proteolytic cleavage of the haemagglutinin. J Gen Virol. 1977;36(1):151–61. doi: 10.1099/0022-1317-36-1-151. [DOI] [PubMed] [Google Scholar]
- 30.Perdue ML, Suarez DL. Structural features of the avian influenza virus hemagglutinin that influence virulence. Vet Microbiol. 2000;74(1–2):77–86. doi: 10.1016/s0378-1135(00)00168-1. [DOI] [PubMed] [Google Scholar]
- 31.Maines TR, Lu XH, Erb SM, Edwards L, Guarner J, Greer PW, et al. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005;79(18):11788–800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]