Abstract
Moving from paper records to electronic health records (EHRs) has been a challenge for many Alabama hospitals. Implementation of this innovative technology will assist in providing better patient care by allowing for and providing more accurate and available patient information. The purposes of this study were to assess
the status of implementation of EHRs among Alabama hospitals;
the factors that are associated with EHR implementation; and
the benefits of, barriers to, and risks of EHR implementation.
A self-completed survey was mailed to 131 directors in the health information management (HIM) department of Alabama hospitals. Of 91 responding hospitals (69 percent response rate), only 12.0 percent have completed implementation of EHRs. The key factor driving electronic health record (EHR) implementation was to improve clinical processes or workflow efficiency. Lack of adequate funding and resources was the major barrier to EHR implementation. Rural hospitals were less likely to implement EHRs when compared with urban hospitals (p = .07). Adoption of EHRs should be evaluated in depth for hospitals, and particularly for rural hospitals. Ways to seek appropriate funding and provide adequate resources should be explored.
Keywords: Electronic health records, barriers, benefits, implementation, rural hospitals
Background/Introduction
In 2004, President Bush called for widespread adoption of the EHR within 10 years. Moving from paper to EHRs has been a challenge for many hospitals and physicians' offices. Although efforts toward EHR implementation started about two decades ago, the process has been slow.1 According to a recent report on EHR progress, the adoption of EHRs “is not occurring as rapidly as hoped,”2 and the U.S. is lagging in adoption of EHRs.3 Recent surveys suggested that EHR implementation was between 17 to 24 percent in physicians' offices in an ambulatory care setting.4,5 EHR use in any format in hospital settings was estimated to be 20 to 25 percent, and the use of computerized physician order entry (CPOE) was about 15 percent.6 Compared to urban hospitals, EHR use in rural hospitals was less common.7,8 Ward's study indicated that more than 80 percent of urban hospitals reported using computers to collect basic clinical information for potential use in an EHR and CPOE system, while only 30 to 40 percent of rural hospitals were doing so.9 With the majority of hospitals located in rural areas, little is known about EHR implementation status and related issues in the state of Alabama.
Geographic Challenges
Alabama is one of the three poorest states in the country, with 22 percent of residents living beneath the federal poverty level and 44 percent of the population having low-income status.10 The median household income in 2000 was $33,433, which ranked 44th nationally among states for per capita income.11 The lower socioeconomic status has a direct impact on the health status of the population. According to a 2006 United Health Foundation report, Alabama was ranked 45th in terms of health profiles in the overall national population health, was 10th nationally in the teen birth rate (52.4 per 1,000 population), and had the second-highest preterm birth rate (16.1 percent), the fourth-highest low birth weight rate (10.4 percent), and the sixth-highest infant mortality rate (9.1 per 1,000 population).12,13
Many medical illnesses and health conditions rely on continuing treatments and routine care. In Alabama, 45 percent of the state population lives in rural areas. The geographic dispersion of the population creates barriers to medical care and challenges to accessing health information. For example, HIV/AIDS patients in Alabama traveled 50 miles or more to receive HIV care.14 Electronic health records can be even more important and useful to improve the health outcomes of unmet rural health needs in areas like Alabama. EHRs can communicate patient information between providers in urban settings and remote areas. In addition, access to EHRs can provide the best of patient care to those who have multiple chronic conditions and diseases and who seek multiple providers who are distant from each other. As stated by Cass Pennington, chief executive officer of Delta Health Alliance, a key advantage of the EHR is that it “will bring all the patient information together in one place and will be easily accessible by all providers no matter where they are.”15
The purpose of this research study was threefold:
to determine the status of implementation of EHRs in hospitals in the state of Alabama;
to assess the factors that are driving the decision making for implementation of EHRs; and
to assess the perceptions of HIM professionals of the benefits, barriers, and risks that are associated with implementation of EHRs.
Methods
Survey Sample and Procedure
We obtained a mailing list from the 2006 Alabama Hospital Association directory. The Alabama Association of Health Information Management provided names for HIM directors at each listed hospital. The mailings were addressed to the HIM directors of all 131 hospitals that were listed in the directory. Five surveys were returned with incorrect addresses. We subsequently acquired updated addresses and remailed these returned surveys. A follow-up letter and e-mail were sent one month after the initial survey was sent to those whose surveys had not been received. A total of 91 valid surveys were received, which gave a response rate of 69 percent.
Survey Development and Measures
The self-completed survey consisted of 12 questions. We referenced the annual survey on EHR trends and usage by the Medical Records Institute.16 The survey questions assessed the status of EHR implementation in the hospital, HIM directors' decision-making role in EHR implementation in their hospitals, and their perceptions of driving factors, benefits, risks, and barriers of EHR implementation. The demographic information was focused on hospital characteristics (bed size and location). All questions were closed-ended or partially closed-ended, which required checking a response box or filling in other items if the answer choices were not given in the survey. For clarity of the survey questions, we pretested the survey in the local office and further revisions were made. The responses were maintained in Microsoft Excel and analyzed using Statistical Package for Social Sciences (SPSS) version 15.0. Descriptive analyses of frequency distributions, cross tabulations, and chi-square tests were performed.
For the EHR status, we asked, “Has your hospital implemented EHR?” The response categories were as follows: yes, EHR has already been implemented; no, EHR has not already been implemented; and implementation for EHR in progress. For those who responded no or in progress, we further asked how soon the hospital would implement EHRs. For the EHR driving factors, benefits, and barriers, we asked each respondent to select the items based on his or her opinion or perception.
Results
Characteristics of Respondents
Of a total of 91 survey respondents, a large majority (93 percent) were HIM directors, and the remaining respondents (7 percent) were hospital administrative personnel. While 42 percent of them have strong input, another 51 percent have little or only some input on decisions regarding EHR implementation in the hospital. There were only two people who held the final decision-making power related to EHR implementation in their hospitals.
Among these survey respondents, 47 percent of their hospitals have less than 100 beds. Three-quarters of the hospitals were nonteaching hospitals, and 35 percent were for-profit hospitals (Table 1). More than half of the respondents were from rural hospitals (58 percent). Of those, almost all were nonteaching hospitals (91 percent), government-owned or nonfederal hospitals (42 percent), and for-profit hospitals (38 percent), with an average bed size of 89.
Table 1.
Characteristics of Survey Respondents and Nonrespondents (n = 131)
| Respondents** (n = 91) | Nonrespondents*** (n = 40) | ||||
|---|---|---|---|---|---|
| Characteristics | N* | % | N* | % | p-value |
| Position | |||||
| HIM Director | 85 | 93.4 | N/A | N/A | N/A |
| Other | 6 | 6.6 | |||
| Decision-Making on EHR | |||||
| No input | 5 | 5.5 | N/A | N/A | N/A |
| Little or some input | 46 | 50.5 | |||
| Strong input | 38 | 41.8 | |||
| Final decision | 2 | 2.2 | |||
| Type of Hospital | |||||
| Nonfederal government | 32 | 36.0 | 13 | 35.1 | .927 |
| Nongovernment not-for-profit | 23 | 25.8 | 8 | 21.6 | |
| Investor-owned for-profit | 31 | 34.8 | 15 | 40.5 | |
| Federal government (VA) | 3 | 3.4 | 1 | 2.7 | |
| Hospital Location | |||||
| Rural | 53 | 58.2 | 17 | 42.5 | .069 |
| Urban | 31 | 34.1 | 15 | 37.5 | |
| Suburban | 7 | 7.7 | 8 | 20.0 | |
| Teaching Hospital | |||||
| Yes | 21 | 23.6 | 7 | 17.5 | .420 |
| No | 68 | 76.4 | 33 | 82.5 | |
| Hospital Bed size | |||||
| Less than 100 | 43 | 47.3 | 20 | 51.3 | .872 |
| 100–199 | 26 | 28.6 | 12 | 30.8 | |
| 200–299 | 11 | 12.1 | 4 | 10.3 | |
| 300 or more | 11 | 12.1 | 3 | 7.7 | |
Numbers of subjects do not always add up to total sample size due to missing data.
Subjects who returned surveys and were included in the study
Subjects who did not return the surveys and were excluded from the study
From a total of 131 possible hospital respondents, 91 (69 percent) responded and 40 (31 percent) did not respond. For all variables where values are known, there were no statistically significant differences between respondents and nonrespondents (Table 1).
Status of EHR Implementation
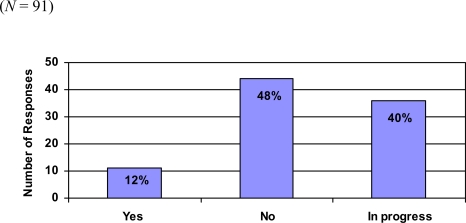
When asked about the status of EHR implementation in their hospitals, only 11 (12 percent) of the 91 survey respondents reported that their hospitals had implemented an EHR system. Almost half, or 44 (48 percent), of the hospitals had not implemented an EHR system when the survey was conducted, with the remaining 36 hospitals (40 percent) being in the implementation process (Figure 1).
Figure 1.
Status of EHR Implementation
Of those hospitals who had implemented an EHR system, four had completed the process before the year 2000, and another seven had implemented it between 2000 and 2006. Five of them are nonfederal government hospitals, four are nongovernment, not-for-profit hospitals, and the other two are VA hospitals. All 11 hospitals have both inpatient and outpatient capabilities for EHR support.
From the survey results, hospital location was associated with EHR implementation status. When compared to urban and suburban hospitals, the hospitals located in rural areas were less likely to have completed implementation of an EHR system (p = .06). Almost 60 percent of rural hospitals were not engaged in EHR implementation. There were significant differences in EHR implementation status by ownership of the hospitals. From the survey responses, all 11 hospitals that had implemented EHR systems are government-owned or not-for-profit hospitals, while none of the 31 (0 percent) of the investor-owned for-profit hospitals had completed EHR implementation (p = .012). We further examined EHR implementation status within for-profit hospitals and found that only one-third of these hospitals were currently in the process of implementing an EHR system, while the remaining two-thirds were not. There were no observed differences in hospital bed size or teaching status in relationship to EHR implementation status.
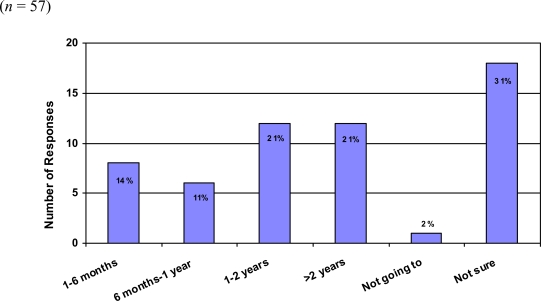
Of the hospitals that had not implemented or were in the process of implementing an EHR system, 25 percent indicated that they would implement EHRs within a year, 21 percent stated that they would implement EHRs in the next two years, another 21 percent indicated more than two years, and 31 percent of respondents reported that they were not sure when EHR implementation would take place (Figure 2).
Figure 2.
Answers to the Question “How Soon Will Your Hospital Implement EHR?”
Factors Driving the Need for EHR Systems
When asked “What factors drive the need for the EHR systems within your hospitals?” 73 (80 percent) of respondents felt that the major need or concern was to improve clinical processes or workflow efficiency. Other factors were the need to share patient information with patient care providers (70 respondents, or 77 percent) and the need to improve healthcare quality (66 respondents, or 73 percent; see Table 2). We examined these perceived needs and factors by EHR implementation status (hospitals that had or had not completed EHR implementation or with EHR implementation in progress). There were no differences in top three perceived major factors that drive EHR implementation (to improve clinical or workflow efficiency, to share patient record information, and to improve healthcare quality) by each implementation status group. About 64 percent of respondents from hospitals with completed EHR implementation considered the choice “EHR can reduce cost in HIM department” as a major driving factor as compared to those from hospitals without EHR systems (45.5 percent) and those from hospitals with EHR implementation in progress (36.1 percent; see Table 2).
Table 2.
Factors Driving the Need for EHR Implementation by EHR Implementation Status
| Factors | Overall | Implemented EHR | Not Implemented EHR | EHR Implementation in Progress |
|---|---|---|---|---|
| N = 91 | N = 11 | N = 44 | N = 36 | |
| N (%) | N (%) | N (%) | N (%) | |
| To improve clinical or workflow efficiency | 73 (80.2) | 9 (81.8) | 32 (72.7) | 32 (88.9) |
| The need to share the patient record information among healthcare professionals | 70 (76.9) | 9 (81.8) | 30 (68.2) | 31 (86.1) |
| To improve healthcare quality | 66 (72.5) | 8 (72.7) | 28 (63.6) | 30 (83.3) |
| Reduce cost in the HIM department and elsewhere | 40 (44.0) | 7 (63.6) | 20 (45.5) | 13 (36.1) |
| Regulatory requirement of JCAHO or NCQA | 38 (41.8) | 3 (27.3) | 21 (47.7) | 14 (38.9 |
| The implementation can reduce healthcare delivery costs | 33 (36.3) | 5 (45.5) | 15 (34.1) | 13 (36.1) |
| Value-based purchasing for performance | 15 (16.5) | 1 (9.1) | 12 (27.3) | 2 (5.6) |
Benefits of Implementing EHRs
The respondents were asked, “What would be the benefit of implementing the EHR system?” A majority of the respondents, 93 percent, indicated that improving workflow would be the major benefit of implementing the system. Some other benefits were stated as reducing medical errors (67 percent), reducing cost and treatment time (43 percent), and increasing revenue (43 percent). Additional benefits from EHR implementation were improving patient care by having better linkage to all caregivers, and reducing the need for file space, supplies, and workers for retrieval and filing of medical records. Among the top three major benefits, there were no perceived differences by EHR implementation status (Table 3).
Table 3.
Perceived Benefits of EHR Implementation by EHR Implementation Status
| Benefits | Overall | Implemented EHR | Not Implemented EHR | EHR Implementation in Progress |
|---|---|---|---|---|
| N = 91 | N = 11 | N = 44 | N = 36 | |
| N (%) | N (%) | N (%) | N (%) | |
| Improve workflow | 85 (93.4) | 10 (90.9) | 40 (90.9) | 35 (97.2) |
| Reduce medical errors | 61 (67.0) | 6 (54.5) | 29 (65.9) | 26 (72.2) |
| Reduce costs | 39 (42.9) | 5 (45.5) | 19 (43.2) | 15 (41.7) |
| Reduce treatment time/length of stay | 39 (42.9) | 6 (54.5) | 16 (36.4) | 17 (47.2) |
| Increase revenue | 28 (30.8) | 2 (18.2) | 15 (34.1) | 11 (30.6) |
| Minimize malpractice claims | 20 (22.0) | 3 (27.3) | 10 (22.7) | 7 (19.4) |
Barriers to Implementing EHRs
The number one perceived barrier for implementing an EHR system was lack of adequate funding and resources (75 percent). Some other barriers were lack of knowledge of EHRs (35 percent), lack of support from medical staff (33 percent), lack of structured technology (28 percent), and lack of employee training (28 percent). Implementation and interpretation of the Health Insurance Portability and Accountability Act (HIPAA) and other privacy issues were also noted as barriers (Table 4).
Table 4.
Perceived Barriers and Risks of EHR Implementation by EHR Implementation Status
| Barriers and Risks | Overall | Implemented EHR | Not Implemented EHR | EHR Implementation In Process |
|---|---|---|---|---|
| N = 91 | N = 11 | N = 44 | N = 36 | |
| N (%) | N (%) | N (%) | N (%) | |
| Lack of adequate funding or resources | 68 (74.7) | 6 (54.5) | 38 (86.4) | 24 (66.7) |
| Lack of knowledge of EHR | 32 (35.2) | 4 (36.4) | 16 (36.4) | 12 (33.3) |
| Lack of support from medical staff | 30 (33.0) | 5 (45.5) | 11 (25.0) | 14 (38.9) |
| Lack of structured technology | 25 (27.5) | 2 (18.2) | 10 (22.7) | 13 (36.1) |
| Lack of employee training | 25 (27.5) | 5 (45.5) | 8 (18.2) | 12 (33.3) |
| Privacy issues | 15 (16.5) | 4 (36.4) | 6 (13.6) | 5 (13.9) |
| Inadequate or incomplete healthcare information standards or code sets | 13 (14.3) | 3 (27.3) | 6 (13.6) | 4 (11.1) |
Some of these perceived barriers were different when broken down by EHR implementation status. About 86 percent of respondents from hospitals without EHR systems perceived “lack of adequate funding or resources” as a major barrier, while only 55 percent of respondents from hospitals with EHR implementation completed considered this a major barrier. Perceptions also varied for other barriers. Respondents from hospitals with EHR systems perceived the barriers of lack of support from medical staff, lack of employee training, and privacy issues to be higher than did respondents from hospitals without EHR systems or hospitals with EHR implementation in progress (Table 4).
There were also differences in perceived barriers by hospital location. Respondents from rural hospitals perceived the barriers of lack of knowledge of EHRs and lack of support from medical staff to be higher than did respondents from nonrural hospitals. Compared with respondents from rural hospitals, those from urban and suburban hospitals perceived the barriers of lack of structured technology, lack of employee training, and privacy issues to be higher (Table 5).
Table 5.
Perceived Barriers and Risks of EHR Implementation by Hospital Locations
| Barriers and Risks | Overall | Rural Hospital | Urban Hospital | Suburban Hospital |
|---|---|---|---|---|
| N = 91 | N = 53 | N = 31 | N = 7 | |
| N (%) | N (%) | N (%) | N (%) | |
| Lack of adequate funding or resources | 68 (74.7) | 39 (73.6) | 23 (74.2) | 6 (85.7) |
| Lack of knowledge of EHR | 32 (35.2) | 21 (39.6) | 9 (29.0) | 2 (28.6) |
| Lack of support from medical staff | 30 (33.0) | 22 (41.5) | 6 (19.4) | 2 (28.6) |
| Lack of structured technology | 25 (27.5) | 10 (18.9) | 11 (35.5) | 4 (57.1) |
| Lack of employee training | 25 (27.5) | 13 (24.5) | 9 (29.0) | 3 (42.9) |
| Privacy issues | 15 (16.5) | 9 (17.0) | 4 (12.9) | 2 (28.6) |
| Inadequate or incomplete healthcare information standards or code sets | 13 (14.3) | 7 (13.2) | 5 (16.1) | 1 (14.3) |
Discussions/Conclusion
EHR implementation is an important yet major challenge and is a slow process in Alabama hospitals. Our results from the Alabama hospital survey indicated that EHR implementation is far from complete. According to survey responses, only 12 percent of Alabama hospitals have completed EHR implementation while 40 percent of additional hospitals are in the process of implementation. A major effort needs to be made in order to achieve President Bush's 10-year goal of implementing the EHR system.
Nationally, EHR adoption rates among hospitals vary widely, as documented in several studies. Jha's study reviewed 36 different surveys conducted between 1995 and 2005 and recorded a range between 4 percent and 21 percent for implementation of CPOE among hospitals.17 Unlike other studies, our study did not find any association between hospital bed size and EHR implementation status.18,19 Also, there was no association between the teaching status of hospitals and EHR implementation. However, in agreement with other studies, our study results indicated that rural hospitals were less likely than nonrural hospitals to have implemented EHR systems.20 Lack of support in financial and other resources is the major factor that contributes to fewer rural hospitals' having completed EHR implementation. In addition, lack of knowledge regarding EHR and lack of support from medical staff may also contribute to the situation. We also identified associations between EHR implementation and hospital ownership status. None of the for-profit hospitals had completed EHR implementation at the survey time, and only one-third of these hospitals were in the process of implementing EHR systems. This finding was supported by a study by Cutler et al., which found that for-profit hospitals are less likely to adopt CPOE systems when compared with government and nonprofit hospitals.21 Future studies may be conducted to examine the factors limiting implementation of EHRs among for-profit hospitals and to explore the driving factors and solutions to increase EHR implementation.
The low rate and slow process of EHR implementation is associated with many barriers and risks. According to the 2006 Executive Summary of Health Information Technology in the United States: The Information Base for Progress, there are four factors that drive EHR adoption: financial incentives and barriers, laws and regulations, the state of the technology, and organization influences.22 The identified barriers and risks associated with EHR implementation from our study are similar to these four factors; however, the major challenges to EHR implementation are largely due to inadequate funding and lack of financial support. Currently, large-scale funding through federal legislation to support EHR implementation efforts is limited. A major effort should be made to seek or make available state funding and also to seek any existing external private sources for financial support.
Recently there have been positive efforts in the areas of electronic health records and health IT statewide. A recent Commonwealth Fund report on state e-health activities in 2007 noted that only 10 states indicated that EHRs or electronic medical records (EMRs) were significant activities in the state. Alabama was one of three states indicating significant activities in developing Web-based tools.23 The Alabama Medicaid Agency has been awarded a two-year, $7.6 million federal grant to create and implement an electronic health information network for Medicaid providers. The network is projected to provide state health agencies, providers, private payers, and other healthcare facilities with accurate health information in a timely manner.24 The Alabama Medicaid Agency selected Affiliated Computer Services for a two-year, $3.7 million award to create an electronic health record database of the state's Medicaid beneficiaries. This EHR database will help physicians view the results of lab tests and treat patients with chronic conditions.25 For rural health facilities, the Alabama Department of Public Health is one of the grantees that received the FLEX Critical Access Hospitals Health Information Technology network grant to support the president's goal of implementing EHRs by 2014. The program selected pilot programs to receive this grant to support the development of various EHR systems and other clinical applications.26 The more these efforts are made, the faster EHR implementation will move forward.
HIM professionals play an important role in EHR implementation. Fenton stated that the HIM professional can have a positive impact on EHR implementation, and she foresaw the successful implementation of EHRs when HIM professionals become actively involved.27 Similar to Fenton's study findings of HIM professionals being very involved in their facilities' EHR implementation, our study revealed that about 95 percent of surveyed HIM directors in Alabama hospitals have some degree of involvement related to EHR decision making in their hospitals. Of those, 44 percent have strong and final input on EHR decision making. To speed up EHR implementation, there will be great demand for HIM professionals with knowledge and education in IT and EHR application. According to the newly passed 10,000 Trained by 2010 Act in the House of Representatives, there is a call for 10,000 trained healthcare professionals with knowledge and skills in applied health and medical informatics.28 More qualified HIM professionals should be prepared and trained to meet this challenge and to take a major role in EHR implementation and operation.
A limitation of this study is that we used self-reported survey data. Although we achieved a 69 percent survey response rate, for those who did not respond to the survey, we have no way to know the EHR implementation status of their hospitals and issues related to it. Because there is no clear definition of EHR implementation, some of the respondents may have been confused about partial or complete EHR implementations. In addition, our survey was targeted to only the HIM directors in each Alabama hospital instead of IT or other information specialists. This may have created the potential of missing some different perceptions from those who have stronger inputs on EHR implementation.
If the U.S. is to achieve the goal of implementation of EHRs within a decade, healthcare facilities will need to make a greater effort to speed up the EHR implementation process. In this study alone, nearly half of the hospitals had not begun the process. It will be necessary in each instance to identify and overcome the barriers and shortcomings of EHR implementation. Increased awareness and the importance of EHR implementation also could be more actively advocated by HIM professional organizations and local, state, and national hospital associations.
Contributor Information
Shannon H. Houser, Health services administration at the University of Alabama at Birmingham in Birmingham, AL.
Lucretia A. Johnson, QuadraMed Corporation in Reston, VA.
Notes
- 1.Amatayakul M.K. Electronic Health Records: A Practical Guide for Professionals and Organizations. 3rd ed. Chicago: AHIMA; 2007. [Google Scholar]
- 2.Robert Wood Johnson Foundation, MGH Institute for Health Policy, and George Washington University. Health Information Technology in the United States: The Information Base for Progress. Executive Summary. 2006. Available at www.rwjf.org/files/publications/other/EHRExecSummary0609 (retrieved August 22, 2007).
- 3.Powell, A. “1U.S. Lagging in Adoption of Electronic Health Records. President Bush Wants Majority of Patients Covered by 2014.” Harvard News Office. October 12, 2006. Available at www.news.harvard.edu/gazette/2006/10.12/13-healthrecords.html (retrieved August 22, 2007).
- 4.Robert Wood Johnson Foundation, MGH Institute for Health Policy, and George Washington University. Health Information Technology in the United States: The Information Base for Progress. Executive Summary.
- 5.Jha, A. K., T. G. Ferris, K. Donelan, C. DesRoches, A. Shields, S. Rosenbaum, and D. Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” Health Affairs 25, no. 6 (October 2006): w496–w507. [DOI] [PubMed]
- 6.Blumenthal, D. “Health Information Technology: What Is the Federal Government's Role?” The Commonwealth Fund, Commission on a High Performance Health System. March 2006. Available at www.commonwealthfund.org/usr_doc/Blumenthal_HIT_907.pdf?section=4039 (retrieved March 1, 2008).
- 7.Bahensky J.A., Jaana M., Ward M.M. The Journal of Rural Health. 2. Vol. 24. 2008. “Health Care Information Technology in Rural America: Electronic Medical Record Adoption Status in Meeting the National Agenda.”; pp. 101–105. [DOI] [PubMed] [Google Scholar]
- 8.Ward M.M., Jaana M., Bahensky J.A., Vartak S., Wakefield D.S. “Clinical Information System Availability and Use in Urban and Rural Hospitals.”. Journal of Medical Systems. 2006;30:429–438. doi: 10.1007/s10916-006-9014-3. [DOI] [PubMed] [Google Scholar]
- 9.Ward M.M., Jaana M., Bahensky J.A., Vartak S., Wakefield D.S. “Clinical Information System Availability and Use in Urban and Rural Hospitals.”. Journal of Medical Systems. 2006;30:429–438. doi: 10.1007/s10916-006-9014-3. [DOI] [PubMed] [Google Scholar]
- 10.The Kaiser Family Foundation, statehealthfacts.org. Data Source: Urban Institute and Kaiser Commission on Medicaid and the Uninsured, estimates based on the Census Bureau's March 2005 and 2006 Current Population Survey (CPS: Annual Social and Economic Supplements).
- 11.U.S. Census Bureau, 2003 Supplementary Survey: Median Household Income (in 2003 Inflation-Adjusted Dollars) (State Level). Available at www.census.gov/acs/www/Products/Ranking/2000/R07T040.htm (retrieved August 24, 2007).
- 12.America's Health Rankings, 2005 edition. A Call to Action for People and Their Communities. Available at www.unitedhealthfoundation.org/shr2005/states/Alabama.html (retrieved August 24, 2007).
- 13.Martin, J. A., H. B. Sutton, P. D. Ventura, S. J. Menacker, F. Kirmeyer, and S. Births. “Final Data for 2004, Table 11, National Vital Statistics Report.” Division of Vital Statistics, National Center for Health Statistics. Vol. 55, No. 1, September 29, 2006. Available at www.cdc.gov/nchs/data/nvsr/nvsr55/nvsr55_01 (retrieved August 24, 2007). [PubMed]
- 14.Marks, G., N. Crepaz, J. W. Senterfitt, and R. S. Janssen. “Meta-analysis of High-Risk Sexual Behavior in Persons Aware and Unaware They Are Infected with HIV in the United States: Implications for HIV Prevention Programs.” Journal of Acquired Immune Deficiency Syndromes 39, no. 4 (2005, August 1): 446–453. [DOI] [PubMed]
- 15.“Delta Health Alliance Selects Allscripts Electronic Health Record for 500 Physicians.” Medem Press Release. Available at www.medem.com/press/press_medeminthenews_detail.cfm?ExtranetPressNewsKey=214 (retrieved August 22, 2007).
- 16.Medical Records Institute's Sixth Annual Survey of Electronic Health Record Trends and Usage for 2004. Available at www.medrecinst.com/uploadedFiles/resources/EHR%20SURVEY%20RESULTS-2004-Web (retrieved October 2006).
- 17.Jha, A. K., T. G. Ferris, K. Donelan, C. DesRoches, A. Shields, S. Rosenbaum, and D. Blumenthal. “How Common Are Electronic Health Records in the United States? A Summary of the Evidence.” [DOI] [PubMed]
- 18.Healthcare Financial Management Association (HFMA). Overcoming Barriers to Electronic Health Record Adoption. February 2006. Available at www.hfma.org/NR/rdonlyres/4FE68E23-0A47-4674-ABBA-F1A4AA1E73A9/0/ehr (retrieved August 24, 2007).
- 19.Thakkar, M., and D. C. Davis. “Risks, Barriers, and Benefits of EHR Systems: A Comparative Study Based on Size of Hospital.” Perspectives in Health Information Management 3, no. 5 (2006, August 14). [PMC free article] [PubMed]
- 20.Healthcare Financial Management Association (HFMA). Overcoming Barriers to Electronic Health Record Adoption.
- 21.Cutler D.M., Feldman N.E., Horwitz J.R. Health Affairs. 6. Vol. 24. 2005. “U.S. Adoption of Computerized Physician Order Entry Systems.”; pp. 1654–1663. [DOI] [PubMed] [Google Scholar]
- 22.Robert Wood Johnson Foundation, MGH Institute for Health Policy, and George Washington University. Health Information Technology in the United States: The Information Base for Progress. Executive Summary.
- 23.Smith, V. K., K. Gifford, S. Kramer, et al. “State E-Health Activities in 2007: Findings from a State Survey.” The Commonwealth Fund. February 2008. Available at www.commonwealthfund.org/publications/publications_show.htm?doc_id=669309 (retrieved March 1, 2008).
- 24.Office of the Governor, Bob Riley, Press Office. “Governor Riley Sees Health Technology in Action.” Available at www.governorpress.alabama.gov/pr/pr-2007-08-14-02-health_tech-photo.asp) and www.govhealthit.com/online/news/102899-1.html (retrieved March 22, 2008).
- 25.“Alabama Contract for Medicaid Database Sparks Controversy,” citing AP/Montgomery Advertiserreports (Johnson, AP/Montgomery Advertiser). Available at www.ihealthbeat.org/articles/2007/8/22/Alabama-Contract-for-Medicaid-Database-Sparks-Controversy.aspx (retrieved March 22, 2008).
- 26.“FLEX Critical Access Hospital–Health Information Technology Network Implementation Grant.” Available at http://ruralhealth.hrsa.gov/funding/flexpurpose.htm (retrieved March 22, 2008).
- 27.Fenton, S. H., M. Amatayakul, and M. Work. “HIM Impact on EHRs: Newly Released Study Links HIM Professionals and Successful EHR Implementations.” Journal of AHIMA 77, no. 9 (October 2006): 36–40. [PubMed]
- 28.Ainsley, M. “Kloss: Skilled HIM Professionals Needed.” Advance 17, no. 22 (October 22, 2007).