Abstract
Background
Patients undergoing hip or knee replacement are at high risk of developing a postoperative venous thromboembolism even after discharge from hospital. We sought to identify hospital and patient characteristics associated with receiving thromboprophylaxis after discharge and to compare the risk of short-term mortality among those who did or did not receive thromboprophylaxis.
Methods
We conducted a retrospective cohort study using system-wide hospital discharge summary records, physician billing information, medication reimbursement claims and demographic records. We included patients aged 65 years and older who received a hip or knee replace ment and who were discharged home after surgery.
Results
In total we included 10 744 patients. Of these, 7058 patients who received a hip replacement and 3686 who received a knee replacement. The mean age was 75.4 (standard deviation [SD] 6.8) years and 38% of patients were men. In total, 2059 (19%) patients received thomboprophylaxis at discharge. Patients discharged from university teaching hospitals were less likely than those discharged from community hospitals to received thromboprophylaxis after discharge (odds ratio [OR] 0.89, 95% confidence interval [CI] 0.80–1.00). Patients were less likely to receive thromboprophylaxis after discharge if they had a longer hospital stay (15–30 days v. 1–7 days, OR 0.69, 95% CI 0.59–0.81). Patients were more likely to receive thromboprophylaxis if they had hip (v. knee) replacement, osteoarthritis, heart failure, atrial fibrillation or hypertension, higher (v. lower) income or if they were treated at medium-volume hospitals (69–116 hip and knee replacements per year). In total, 223 patients (2%) died in the 3-month period after discharge. The risk of short-term mortality was lower among those who received thromboprophylaxis after discharge (hazard ratio [HR] 0.34, 95% CI 0.20–0.57).
Interpretation
Fewer than 1 in 5 elderly patients discharged home after a hip-or knee-replacement surgery received postdischarge thromboprophylaxis. Those prescribed these medications had a lower risk of short-term mortality. The benefits of and barriers to thromboprophylaxis therapy after discharge in this population requires further study.
Venous thromboembolism is a leading cause of mortality among patients in hospital.1,2 Major orthopedic surgery (e.g., hip or knee replacement) is associated with a high risk for postoperative venous thromboembolism.1,3,4 Because the clinical diagnosis of venous thromboembolism is unreliable and its first manifestation may be a life-threatening pulmonary embolism,5 it is recommended that patients undergoing hip or knee replacement receive routine thromboprophylaxis with anticoagulant therapy after surgery unless they have contraindications to anticoagulant therapy.1,3,5,6
Thromboprophylaxis is commonly administered for the entire hospital stay, which is usually between 4 and 14 days.7 Expert consensus guidelines recommend that patients undergoing hip or knee replacement receive thromboprophylaxis medications for at least 10 days after surgery.6 These guidelines also recommend extended thromboprophylaxis for up to 28–35 days after surgery for patients undergoing hip replacement.6 Although there is evidence that extended thromboprophylaxis after hospital discharge is effective for reducing the risk of venous thromboembolism among patients who undergo hip replacement,8 the benefit among patients who undergo knee replacement has not been established.6 Thromboprophylaxis after discharge is likely to most benefit patients at high risk for venous thromboembolism, such as those with cancer, heart failure or major respiratory disease.6–9 However, given that patients who undergo joint replacement are often elderly and have multiple comorbidities, the risks associated with extended thromboprophylaxis, particularly gastrointestinal bleeding and hemorrhagic strokes, may be substantial and may be relative contraindications for this therapy.10
Among patients discharged home after hip-or knee-replacement surgery, we sought characterize the use of thromboprophylaxis after discharge and its consequences on risk of short-term mortality.
Methods
Study design and data sources
We conducted a retrospective population-based cohort study using hospital admissions, physician claims, drug claims and demographic records obtained from health services administrative databases in Quebec. In this Canadian province, coverage for outpatient and inpatient physician services is provided for the entire population (about 7.5 million people). In addition, people aged 65 years or older (966 014 people), those who receive social assistance (508 809 people) and those who do not have private drug insurance (1 703 437 people) have their prescription drugs covered by the provincial government.
The prescription drug database contains information about all dispensed prescriptions, including drug name, dispensation date, dosage, form, duration and quantity dispensed. Drugs dispensed to patients during stays in hospitals or public nursing homes and over-the-counter drugs are not included in the database. This database has been validated and found to be both accurate and reliable.11 The demographic database provides information on age, sex, postal code, type and dates of coverage by drug insurance plan, and date of death if applicable. For people aged 65 years or older, 3 types of drug insurance plans exist: guaranteed revenue supplement, partial revenue supplement or no revenue supplement. Enrollment in the guaranteed revenue supplement plan indicates a lower income; all other patients were classified as having higher income. The date of death in this database is considered to be accurate, but the cause of death is not recorded.
The hospital discharge summary database contains information about all admissions to short-term care hospitals. This information includes the type of hospital (university teaching or community-based), primary and secondary discharge diagnoses, procedures performed, admission date, provenance (home, another hospital or emergency department), length of stay, in-hospital death and cause, and discharge date and destination. This database has been validated for a number of conditions including hip fracture,12 stroke,13 myocardial infarction14 and injury.15 For these conditions, data accuracy is generally high. Hospitalization data have not been validated specifically for hip and knee replacement, but these procedures have been validated in a similar database in the province of Manitoba.16
The databases used in this study are linkable through a unique patient identifier. Permission to link the data was obtained from the ethics board in Quebec (Commission d'accès à l'information)
Inclusion and exclusion criteria
We included patients 65 years of age or older who underwent elective hip-or knee-replacement surgery (Canadian Classification of Diagnostic, Therapeutic and Surgical Procedures [total hip replacement 93.5x, partial hip replacement 93.6x, total knee replacement 93.41]) between January 1997 and December 2004. A surgery was classified as elective if the admission data indicated that the patient was admitted from home. We included only patients who were discharged home because the database used does not include medication information for patients in nursing homes or rehabilitation centres (medications are covered through institutional budgets for these patients). Thromboprophylaxis is recommended for up to 35 days after surgery for patients who received a hip replacement;6 thus, we excluded patients with a hospital stay of more than 30 days because the need for outpatient thromboboprophylaxis for these patients was uncertain. We also excluded patients who experienced a venous thromboembolism during their hospital stay because anticoagulants prescribed at discharge would have been as treatment rather than as prophylaxis.
Hospital and patient characteristics at discharge
We included the following patient characteristics assessed at hospital discharge: demographic variables (age, sex, region of residence, income [high v. low as classified in the provincial drug plan for reimbursement purposes]); concurrent chronic diseases (assessed from hospital discharge summary diagnoses codes [cancer, ischemic heart disease, atrial fibrillation, congestive heart failure, cerebrovascular disease, hypertension, diabetes mellitus, osteoarthritis, rheumatoid arthritis, renal failure, gastrointestinal bleeding, hemorrhagic stroke]); type of admission as recoded in the database (urgent, semi-urgent, not urgent); length of hospital stay; type of surgery (total hip replacement, partial hip replacement, total knee replacement); type of hospital (teaching v. community); hospital volume (average number of hip-and knee-replacement surgeries performed per year [categorized according to quartiles]); and acetylsalicylic acid prescription dispensed at discharge
Outcome variables
We considered 2 dichotomous outcome variables: receipt of thromboprophylaxis after discharge and death within 3 months of discharge (short-term mortality). We identified thromboprophylaxis prescriptions from the prescription drug database (using drug identification numbers, available from the authors on request), including warfarin, low molecular-weight heparin, unfractionated heparin and fondaparinux. Patients who were dispensed any 1 of these medications within 1 day of the discharge date were classified as having received thromboprophylaxis after discharge. We considered only short-term mortality to limit the likelihood of including deaths unrelated to the joint surgery.
Statistical analyses
We used means and standard deviations or proportions to report patient characteristics and outcome variables. To study the association between patient characteristics and thromboprophylaxis after discharge, patients were separated into 2 groups according to whether they had received thromboprophylaxis after discharge. We compared the unadjusted patient characteristics between these groups using crude odds ratios (ORs) and 95% confidence intervals (CIs). An OR greater than 1 reflects a higher likelihood of receiving thromboprophylaxis after discharge.
Because extended thromboprophylaxis is more strongly recommended in the earlier days following surgery, we categorized the length of hospital stay into 3 categories (1–7, 8–14 and 16–30 days) based on quartiles, and we examined the characteristics and proportions of those dispensed thromboprophylaxis after discharge in these categories. Multivariable logistic regression models were used to assess the association between patient and hospital characteristics and thromboprophylaxis after discharge. We expressed the results as ORs and 95% CIs. Multicolinearity was assessed using the variance inflation factor (a factor of 10 or greater indicates multicolinearity).17 We examined the goodness-of-fit of the model using the Hosmer–Lemeshow test. Receivers operating characteristics curves were also plotted. A larger area under the curve indicates better fit. We plotted Kaplan–Meir curves to display the unadjusted time-to-death in the 3-month period after discharge among those who did or did not receive thromboprophylaxis after discharge.
We constructed Cox regression models to examine the association between patient and hospital characteristics and short-term mortality. We checked the proportional hazard assumption by examining the plots of log (–log[survival]) versus log survival time for those who did or did not receive thromboprophylaxis therapy. We also examined interactions between thromboprophylaxis therapy and ischemic heart disease, heart failure, atrial fibrillation and cancer. Analyses by propensity score were also conducted. In these analyses, the propensity score was defined as the likelihood of being dispensed thromboprophylaxis at discharge.18 We divided patients into 5 groups by propensity score quintiles and used Cox regression models to stratify by propensity score category.
We performed subgroup analyses using separate models for each type of surgery (total hip, partial hip or total knee replacement). We repeated the analysis after excluding patients with cancer, heart failure, ischemic heart disease, atrial fibrillation, cerebrovascular disease and renal failure. We also repeated the analysis using separate models for patients aged more or less than 75 years of age, and we constructed separate models in each stratum based on the length of hospital stay (1–7, 8–14 and 15–30 days).
Results
Patient characteristics
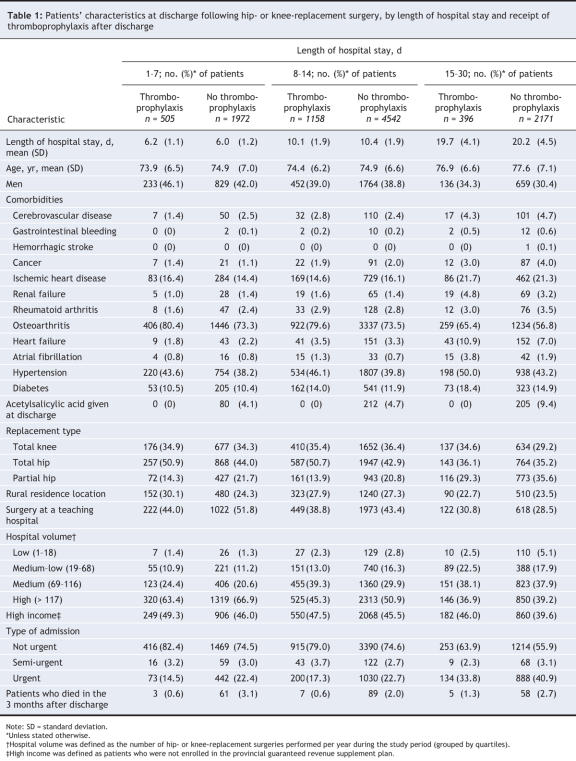
In total, 32 884 patients underwent hip-or knee-replacement surgery during the study period in 64 hospitals, of which 19 were university teaching hospitals). Of the 64 hospitals, 16 were low-volume hospitals (1–18 hip-or knee-replacement surgeries per year during the study period), 16 were medium–low-volume hospitals (19–68 surgeries per year), 16 were medium-volume hospitals (69–116 surgeries per year) and 16 were high-volume hospitals (> 116 surgeries per year). In total, 30 468 underwent the procedure electively. Of these patients, 1161 died in hospital and 656 experienced a venous thromboembolism during their hospital stay and were therefore excluded. We excluded an additional 2365 patients because their hospital stay was longer than 30 days. Of the remaining 26 286 patients, 10 744 (4566 total hip replacements, 2492 partial hip replacements, 3686 total knee replacements) were discharged home and were included in our study cohort (Figure 1).
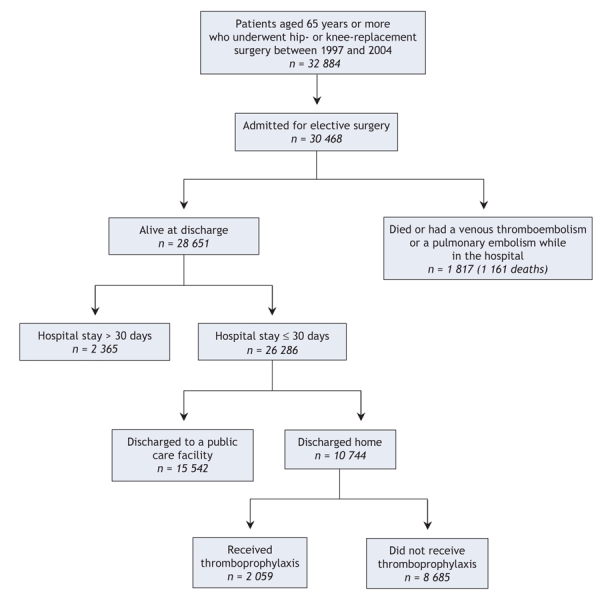
Figure 1: Selection of patients for inclusion in the study.
On average, study patients were aged 75.4 (standard deviation [SD] 6.8) years, 37.9% were men and 65.7% received hip replacements. Of the included patients, 2059 (19.2%) filled a prescription for a thomboprophylaxis agent within 1 day of discharge. The remaining 8685 patients were grouped as having received no thromboprophylaxis. The proportion of study patients who received thromboprophylaxis after discharge varied widely between hospitals, ranging from 0% in some low-volume hospitals to 72% in one medium-low volume hospital (median 13.6%, interquartile range 7.9%–27.1%).
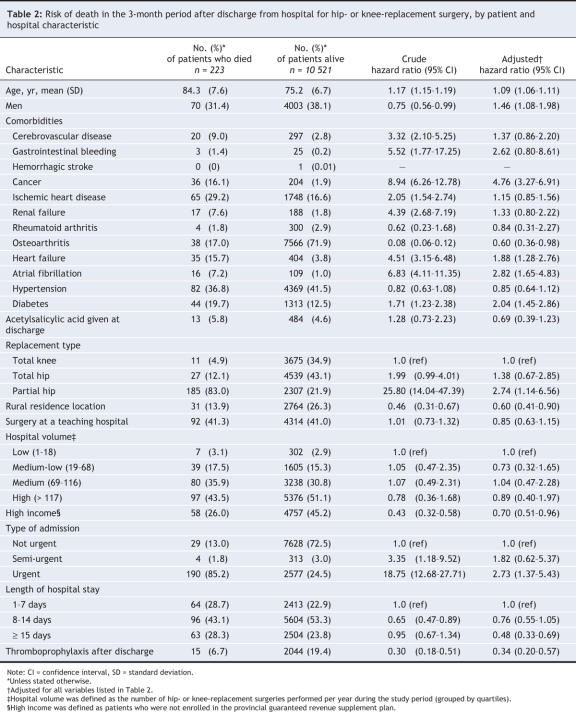
Our unadjusted analysis showed that, compared with patients who received no thromboprophylaxis after discharge, those who received thromboprophylaxis were slightly younger. They were also more likely to be men, to have osteoarthritis, hypertension or diabetes, to have a higher income and to have received surgery in a medium-volume hospital (69–116 hip and knee surgeries per year). However, they were less likely than those who received no thromboprophylaxis to have been treated at a university teaching hospital, to have had an urgent admission or to have had a longer hospital stay (Figure 2).
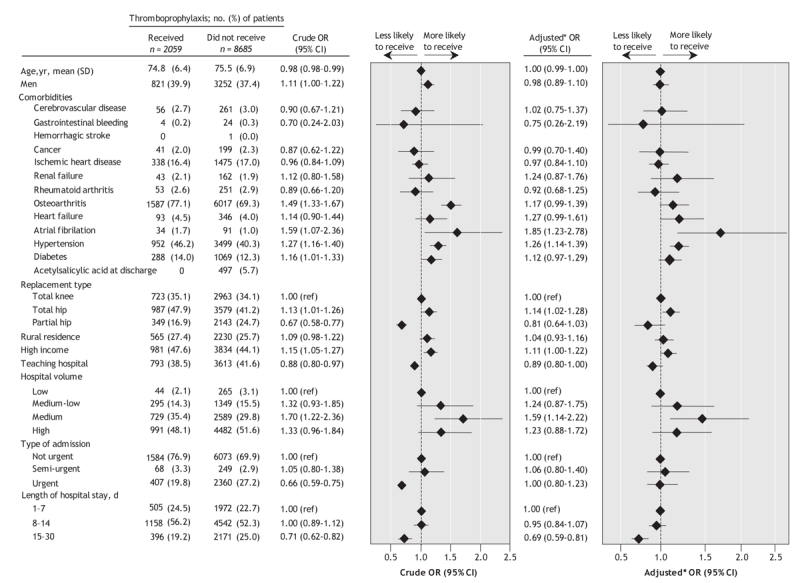
Figure 2: Crude and adjusted odds ratios for receiving thromboprophylaxis after discharge among patients aged 65 years and older who underwent hip or knee replacement surgery between January 1997 and December 2004. Note: OR = odds ratio, CI = confidence interval, SD = standard deviation. *Adjusted for all variables listed in Figure 2.
The proportion of patients who received thromboprophylaxis after discharge was low regardless of length of hospital stay. Of those discharged within 7 days of surgery, 20.4% received thromboprophylaxis, compared with 20.3% of those discharged within 8–14 days and 15.4% of those discharged within 15–30 days. Patient and hospital characteristics are shown in Table 1. Compared with patients in hospital for 14 or less days, patients in hospital for 15 or more days were older and they were more likely to be women, to have more comorbidities, urgent hospital admission or to have had a partial (v. total) hip replacement.
Table 1
Multivariable logistic-regression models showed that patients with longer hospital stays were less likely than those with shorter stays to receive thromboprophylaxis after discharge (15–30 v. 1–7 days, OR 0.69, 95% CI 0.59–0.81). Patients admitted to a teaching hospital were less likely than those admitted to a community hospital to receive thromboprophylaxis after discharge (OR 0.89, 95% CI 0.80–1.00). Patients with atrial fibrillation (OR 1.85, 95% CI 1.23–2.78) or hypertension (OR 1.26, 95% CI 1.14–1.39) as well as those with higher income (OR 1.11, 95% CI 1.00–1.22), those treated in medium-volume hospital (v. low volume, OR 1.69, 95% CI 1.14–2.22) and those who received a total hip replacement (v. total knee replacement, OR 1.14, 95% CI 1.02–1.28) were more likely to have received thromboprophylaxis after discharge (Figure 2). Multivariable logistic models constructed within each stratum of length of hospital stay gave similar results (data not shown). However, among patients in hospital for 15–30 days, the likelihood of receiving thromboprophylaxis after discharge did not differ by type of hospital (teaching v. community hospital, OR 1.17, 95% CI 0.66–2.09), nor did it differ by type of surgery received (total hip v. total knee replacement, OR 0.65, 95% CI 0.22–2.04).
Death within 3 months of discharge
Kaplan–Meier curves showing time to death in the 3-month period after discharge are shown in Figure 3. These curves suggest that the risk of death is higher among patients who did not receive thromboprophylaxis than among those who received the medication. Table 2 presents the patient and hospital characteristics for patients at the end of the 3-month period after discharge. Predictors of short-term mortality were increased age (hazard ratio [HR] for 1 year increase 1.09, 95% CI 1.06–1.11), being male (HR 1.46, 95% CI 1.08–1.98), and having cancer (HR 4.76, 95% CI 3.27–6.91), heart failure (HR 1.88, 95% CI 1.28–2.76), atrial fibrillation (HR 2.82, 95% CI 1.65–4.83), diabetes (HR 2.04, 95% CI 1.45–2.86), partial hip replacement (v. knee replacement, HR 2.74, 95% CI 1.14–6.56) and urgent admission (HR 2.73, 95% CI 1.37–5.43). The risk of short-term mortality was lower among those who received thromboprophylaxis after discharge (HR 0.34, 95% CI 0.20–0.57). We did not find an interaction between thromboprophylaxis and ischemic heart disease, heart failure, atrial fibrillation or cancer (data not shown). Patients who lived in rural areas (HR 0.60, 95% CI 0.41–0.89) and those with higher income (HR 0.70, 95% CI 0.51–0.96) were at lower risk of dying. The risk of short-term mortality was inversely associated with the length of hospital stay (8–14 v. 1–7 days, HR 0.76, 95% CI 0.55–1.05; 15–30 v. 1–7 days, HR 0.48, 95% CI 0.33–0.69) (Table 2). Analyses stratified by propensity score gave similar results (data not shown). Of note, propensity scores ranged from 0–0.5, indicating that patient characteristics did not explain much of the decision to prescribe thromboprophylaxis.
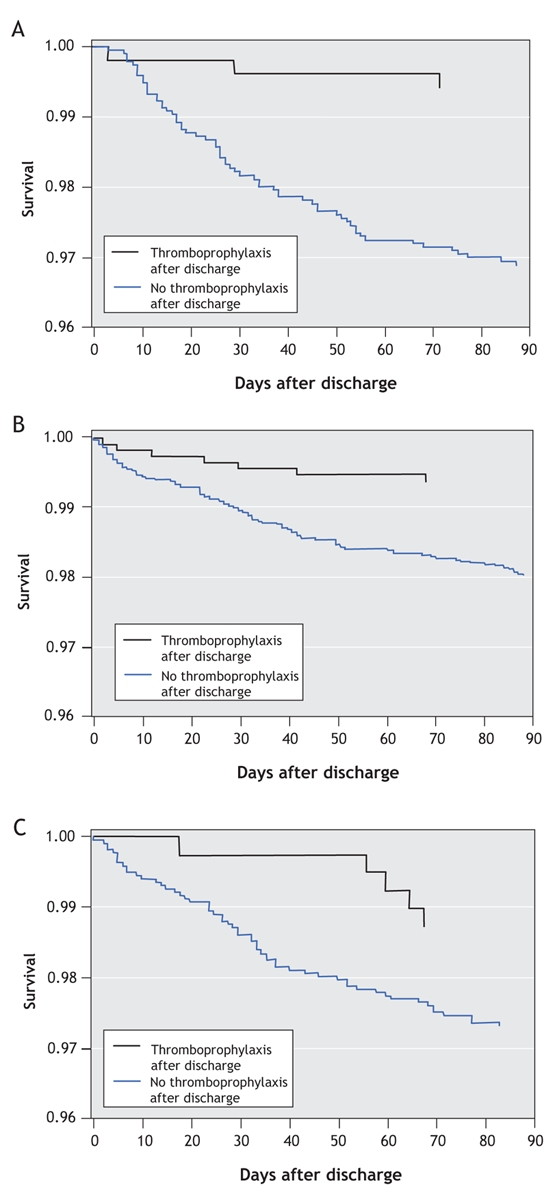
Figure 3: Kaplan–Meier survival curves for patients aged 65 years and older who did or did not receive thromboprophylaxis after discharge. A) Patients in hospital for 1–7 days after surgery, B) patients in hospital for 8–14 days after surgery and C) patients in hospital for 15–30 days after surgery.
Table 2
Secondary analysis
Separate models constructed for patients with total hip or partial hip or knee replacements gave similar results overall. However, the analysis including patients who received total hip and total knee replacements lacked statistical power because of the low number deaths that occurred in the 3-month period after discharge (11 and 27 deaths respectively). The hazard ratio for thromboprophylaxis was 0.30 among patients with total hip replacement (95% CI 0.07–1.32), 0.33 among those with partial hip replacement (95% CI 0.18–0.60) and 0.40 among those with total knee replacement (95% CI 0.05–3.17) (data not shown).
We found a significant effect of thromboprophylaxis on mortality risk in analyses restricted to patients who did not have cancer, heart failure, atrial fibrillation or ischemic heart disease (HR 0.25, 95% CI 0.11–0.57) and in analyses restricted to patients who had 1 or more of these diseases (HR 0.46, 95% CI 0.25–0.85). We found a similar result when we grouped patients by age (HR 0.45 among those aged < 75 years, 95% CI 0.13–1.62; HR 0.32 among those aged ≥ 75 years, 95% CI 0.17–0.57); however, the result in the younger age group was not statistically significant because of the low number of death (27) in this group. When we analyzed the data using separate models for length of hospital stay, we found similar results, although the number of deaths was low among patients who received thromboprophylaxis (length of hospital stay 1–7 days, HR 0.29, 95% CI 0.08–0.93; 8–14 days, HR 0.32, 95% CI 0.15–0.70; 15–30 days, HR 0.44, 95% CI 0.17–1.14).
Interpretation
We found that only 19% of elderly patients discharged home after hip or knee replacement surgery received postdischarge thromboprophylaxis. After discharge use was low regardless of the type of surgery, ranging from 14.0% to 21.6%. It was also low among patients who stayed in hospital for 7 days or less (20%). Compared with patients who did not receive thromboprophylaxis after discharge, those who received thromboprophylaxis after discharge were at lower risk of short-term mortality. This result was robust because of the the analytical methodology used, and it was consistent regardless of age, patient comorbidities and type of surgery.
Expert consensus guidelines recommend that patients receive thromboprophylaxis for at least 10 days after knee-replacement surgery and from 10 to 35 days following hip-replacement surgery.6,19 In spite of these recommendations, only 19% of patients in our study received thromboprophylaxis after discharge. The prolonged length of stay only partly explained the low rate of use. Although it is not possible to determine with certainty from our database if a patient who would have benefited from thromboprophylaxis did not receive it, the observed proportion of thromboprophylaxis after discharge is suboptimal even if we assumed that 30%–40% of study patients did not require the medication. Published literature also reports lower than recommended use of thromboprophylaxis after discharge following hip-and knee-replacement surgery; however, the determinants of this low use are not well understood.6,20–25 In our study, patients who received hip-or knee-replacement surgery at a teaching hospital were less likely than those who received surgery at a community hospital to receive thromboprophylaxis after discharge, and those with higher income were more likely to receive these medications after discharge. These findings require further investigation to assess whether they reflect differences in physician behaviour or health status between patients with higher and lower incomes and differences between patients at teaching and community hospitals.
Our study also revealed that patients who received thromboprophylaxis after discharge were at lower risk of short-term mortality than patients who did not receive these medications. Although only a small proportion of the deaths is expected to be from thromboembolic causes, we do not believe that confounding is responsible for this result because the risk of mortality from other causes is expected to be the same among those who did or did not receive thromboprophylaxis and because our model adjusted for comorbidities. Nonetheless, a causal link between thromboprophylaxis after discharge and decreased mortality cannot be definitely established based on our results alone because the reasons for not prescribing extended thromboprophylaxis therapy are not known.
Study patients with higher incomes were at lower risks of short-term mortality than those with lower incomes, perhaps reflecting better health among these patients.,26,27 Patients with longer hospital stays compared to those with shorter stays were also at lower risks of short-term mortality. Of note, patients who received surgery at high-volume hospitals were more often discharged within 7 days of surgery compared to patients who received surgery at lower-volume hospitals. A prospective study is needed to establish whether some patients are being prematurely discharged.
A few published studies have examined the risk of short-term mortality after discharge following hip-and knee-replacement surgery.28–30 In general, these studies reported lower short-term mortality risks compared with our study. For example, using a hospital discharge database in California, White and colleagues reported that 0.9% of hip-replacement patients and 0.6% of knee-replacement patients died in the 3-month period after discharge.28 The mortality risk was higher in our study (2.1%) because we included patients who had partial hip replacements. The mortality among these patients was 7.4%, compared with 0.6% among patients with total hip replacements and 0.3% among those with total knee replacements.
The strengths of our study include the use of large, population-based administrative databases that contained data collected independently of our study objectives. These databases included a large number of variables relevant to the study questions. The databases and study design afforded us the opportunity to examine the outpatient thromboprophylaxis among patients aged 65 years and older who were discharged home after a hospital stay because of hip-or knee-replacement surgery. The database and study design also allowed us to examine the risk of short-term mortality after discharge. Our study results were robust to the analytical methodology used (multivariable modeling, propensity score adjustment and stratified analyses) and were consistent in all subgroups examined, which indicates limited residual confounding.
Limitations
The limitations of our study are also related to the use of administrative databases, which do not include the indication for which a medication is prescribed and actual drug consumption. For example, warfarin could have been prescribed at discharge for atrial fibrillation but not for prophylaxis against venous thromboembolism. However, if this were true, some patients prescribed warfarin were at higher risk of death at baseline compared with those not prescribed this medication, which would have biased our mortality results toward a higher risk. Indeed, when we excluded patients with atrial fibrillation, heart failure, cancer and ischemic heart disease, the association between thromboprophylaxis and mortality was stronger. In addition, if some of the prescribed anticoagulants were for indications other than the prevention of venous thromboembolism, the prevention of venous thromboembolism with postdischarge thromboprophylaxis was less frequent than reported in our study. However, some patients prescribed thromboprophylaxis could have been healthier than those not prescribed these medications for reasons that were not apparent in the databases. For example, physicians may refrain from prescribing extended thromboprophylaxis to patients with numerous comorbidities for fear of bleeding. Although our analyses adjusted for known comorbidities, information about some comorbidities (e.g., history of gastrointestinal bleeding, venous thromboembolism) may have been incomplete; thus, there is a possibility that healthier patients may have been channeled into the thromboprophylaxis group and that our analyses did not fully adjust for channeling bias.31
Lack of information about compliance with the prescription regimen is also a limitation of our study. Although elderly postoperative patients are believed to be generally compliant with their prescription regimens, patients who were not would have been included in the thromboprophylaxis group even if they were not actually taking these medications, which would result in a risk of death that was lower than reported. Finally, our study considered only patients discharged home following a hospital stay because of hip-or knee-replacement surgery; therefore, our results may not be generalizable to all patients undergoing these surgeries. Further studies are needed to examine the relations between the duration of thromboprophylaxis and the risk of venous thromboembolism and bleeding after discharge.
In conclusion, fewer than 1 in 5 patients received thromboprophylaxis after discharge following hip or knee replacement despite clinical guidelines. This is particularly concerning because those who received thromboprophylaxis at discharge were less likely to die within the 3-month period after discharge compared with those who did not receive these medications.
@ See related article page 1571
Supplementary Material
Acknowledgments
Elham Rahme is a research scholar funded by The Fonds de la Recherche en Santé du Quebec. Kaberi Dasgupta and Sasha Bernatsky are physician–scientists funded by the Canadian Institutes of Health Research. Susan Kahn is a recipient of Clinical Investigator Awards from the Fonds de la Recherche en Santé du Québec. Hongjun Yin is a research scholar funded by the US National Institute on Aging.
Footnotes
Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/178/12/1545/DC1
This article has been peer reviewed.
Contributors: All of the authors had full access to the data and participated in the design and conduct of the study. All of the authors participated in the analysis and interpretation of the data and in the writing of the manuscript. All of the authors approved the final version submitted for publication.
This study was supported by a grant from The Canadian Institutes of Health Research (MOP-77815).
Competing interests: None declared.
Correspondence to: Dr. Elham Rahme, Division of Clinical Epidemiology, McGill University Health Centre, 687 Pine Ave. W, V Building, Montréal QC H3A 1A1; fax 514 934-8293; elham.rahme@mcgill.ca
REFERENCES
- 1.Geerts WH, Heit JA, Clagett GP, et al. Prevention of venous thromboembolism. Chest 2001;119:132S-75S. [DOI] [PubMed]
- 2.Silverstein MD, Heit JA, Mohr DN, et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 1998;158:585-93. [DOI] [PubMed]
- 3.Prevention of venous thromboembolism. International consensus statement (guidelines according to scientific evidence). Int Angiol 1997;16:3-38. [PubMed]
- 4.Pini M, Spyropoulos AC. Prevention of venous thromboembolism. Semin Thromb Hemost 2006;32:755-66. [DOI] [PubMed]
- 5.Weinmann EE, Salzman EW. Deep-vein thrombosis. N Engl J Med 1994;331:1630-41. [DOI] [PubMed]
- 6.Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;126(Suppl 3):338S-400S. [DOI] [PubMed]
- 7.Eikelboom JW, Quinlan DJ, Douketis JD. Extended-duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta-analysis of the randomised trials. Lancet 2001;358:9-15. [DOI] [PubMed]
- 8.Prandoni P, Bruchi O, Sabbion P, et al. Prolonged thromboprophylaxis with oral anticoagulants after total hip arthroplasty: a prospective controlled randomized study. Arch Intern Med 2002;162:1966-71. [DOI] [PubMed]
- 9.Kearon C. Duration of venous thromboembolism prophylaxis after surgery. Chest 2003;124:386S-92S. [DOI] [PubMed]
- 10.Levine MN, Raskob G, Beyth RJ, et al. Hemorrhagic complications of anticoagulant treatment: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;126:287S-310S. [DOI] [PubMed]
- 11.Tamblyn R, Lavoie G, Petrella L, et al. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Quebec. J Clin Epidemiol 1995;48:999-1009. [DOI] [PubMed]
- 12.Levy AR, Mayo NE, Grimard G. Rates of transcervical and pertrochanteric hip fractures in the province of Quebec, Canada, 1981–1992. Am J Epidemiol 1995;142:428-36. [DOI] [PubMed]
- 13.Mayo NE, Danys I, Carlton J, et al. Accuracy of hospital discharge coding for stroke. Can J Cardiol 1993;9(Suppl):121D-4D.
- 14.Jollis JG, Ancukiewicz M, Delong ER, et al. Discordance of databases designed for claims payment versus clinical information-systems — implications for outcomes research. Ann Intern Med 1993;119:844-50. [DOI] [PubMed]
- 15.Tamblyn R, Reid T, Mayo N, et al. Using medical services claims to assess injuries in the elderly: sensitivity of diagnostic and procedure codes for injury ascertainment. J Clin Epidemiol 2000;53:183-94. [DOI] [PubMed]
- 16.Roos LL, Sharp SM, Wajda A. Assessing data quality — a computerized approach. Soc Sci Med 1989;28:175-82. [DOI] [PubMed]
- 17.Weisberg S. Applied linear regression. 3rd ed. Hoboken (NJ): Wiley-Interscience; 2005.
- 18.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med 1997;127:757-63. [DOI] [PubMed]
- 19.Hull RD, Pineo GF, Stein PD, et al. Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 2001;135:858-69. [DOI] [PubMed]
- 20.Planes A, Vochelle N, Darmon JY, et al. Risk of deep-venous thrombosis after hospital discharge in patients having undergone total hip replacement: double-blind randomised comparison of enoxaparin versus placebo. Lancet 1996;348:224-8. [DOI] [PubMed]
- 21.Dahl OE, Pleil AM. Investment in prolonged thromboprophylaxis with dalteparin improves clinical outcomes after hip replacement. J Thromb Haemost 2003;1:896-906. [DOI] [PubMed]
- 22.Abad JI. Prophylaxis of venous thromboembolism in orthopaedic surgery. Pathophysiol Haemost Thromb 2002;32:403-5. [DOI] [PubMed]
- 23.Mesko JW, Brand RA, Iorio R, et al. Venous thromboembolic disease management patterns in total hip arthroplasty and total knee arthroplasty patients: a survey of the AAHKS membership. J Arthroplasty 2001;16:679-88. [DOI] [PubMed]
- 24.Anderson FA Jr, Hirsh J, White K, et al. Temporal trends in prevention of venous thromboembolism following primary total hip or knee arthroplasty 1996-2001: findings from the Hip and Knee Registry. Chest 2003;124:349S-56S. [DOI] [PubMed]
- 25.Warwick D, Friedman RJ, Agnelli G, et al. Insufficient duration of venous thromboembolism prophylaxis after total hip or knee replacement when compared with the time course of thromboembolic events: findings from the Global Orthopaedic Registry. J Bone Joint Surg Br 2007;89:799-807. [DOI] [PubMed]
- 26.Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging 2006;23:191-202. [DOI] [PubMed]
- 27.Murray MD, Morrow DG, Weiner M, et al. A conceptual framework to study medication adherence in older adults. Am J Geriatr Pharmacother 2004;2:36-43. [DOI] [PubMed]
- 28.White RH, Romano PS, Zhou H, et al. Incidence and time course of thromboembolic outcomes following total hip or knee arthroplasty. Arch Intern Med 1998;158:1525-31. [DOI] [PubMed]
- 29.Nunley RM, Lachiewicz PF. Mortality after total hip and knee arthroplasty in a medium-volume university practice. J Arthroplasty 2003;18:278-85. [DOI] [PubMed]
- 30.Lie SA, Engesaeter LB, Havelin LI, et al. Early postoperative mortality after 67,548 total hip replacements: causes of death and thromboprophylaxis in 68 hospitals in Norway from 1987 to 1999. Acta Orthop Scand 2002;73:392-9. [DOI] [PubMed]
- 31.MacDonald TM, Pettitt D, Lee FH, et al. Channelling of patients taking NSAIDs or cyclooxygenase-2-specific inhibitors and its effect on interpretation of outcomes. Rheumatology (Oxford) 2003;42(Suppl3):iii3-10. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.