A 72-year-old woman was referred to our dermatology clinic with a 6-month history of severe diffuse pruritus. Examination with a hand-held epiluminescent stereomicroscope (dermoscope) (Figure 1) revealed scabies mites (Figure 2) within minutes, and we began a topical treatment with 5.0% permethrin cream.

Figure 1: A hand-held epiluminescent stereomicroscope in use.

Figure 2: Traditional microscopic image of a female scabies mite suspended in oil (original magnification × 200).
The female Sarcoptes scabiei mite is 0.2–0.4 mm long and burrows into the host's corneal skin layer to lay its eggs. Burrows are often shaped like an “s” or “z.” They are characteristically found in areas such as the finger webs, axillae, buttocks, scrotum and under the breasts. However, other locations, such as the palm, as in our patient's case, are possible (Figure 3). Local hypersensitivity reactions often also develop in patients, leading to highly pruritic groups of red papules 2–5 mm wide. Symptoms develop within 2 to 6 weeks of being infested; however, in patients with previous infestations, symptoms develop within a few days.

Figure 3: Photograph of patient's palm, showing a straight burrow that is about 5 mm long and visible to the naked eye.
Scabies is traditionally diagnosed clinically and confirmed by microscopic examination of burrow skin scrapings, suspended in mineral oil or saline. Visualization of the mites (Figure 4), eggs or feces confirms the diagnosis. However, handling and processing scrapings rapidly and effectively in the office is not always straightforward.
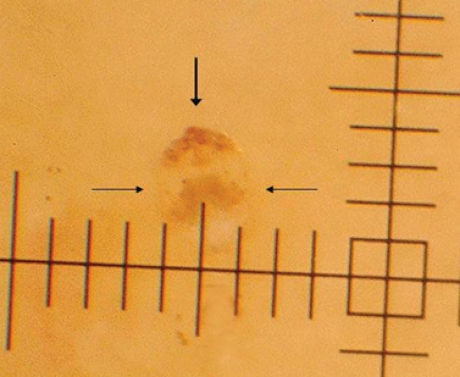
Figure 4: Photographic image of a female scabies mite taken through a hand-held epiluminescent stereomicroscope (original magnification × 40). Note the hang-glider-like triangle of the mite's head (vertical arrow) and round body (horizontal arrows). The hash marks on the axes are at 0.1-mm intervals.
Dermoscopy is an alternative technique for diagnosing scabies. An illuminated magnifier, also known as an epiluminescent stereomicroscope (magnification × 20–60) is required. The hand-held device, designed in 1996 by the dermatologist JF Kreusch, is held perpendicular to the skin (Figure 1). At magnification × 20–40, the typical appearance of the mite's head and 2 pairs of forelegs resemble the triangular shape of a hang-glider. Sometimes the contour of the round body of the mite can also be identified (Figure 4).
Dermoscopy for scabies is 91% sensitive (95% confidence interval [CI] 80%–92%) and 86% specific (95% CI 80%–92%) (magnification × 10).1 For busy clinicians, dermoscopy represents a simple, accurate and rapid technique that is worth considering for the diagnosis of scabies.
Sven Neynaber MD Hans Wolff MD Department of Dermatology and Allergy Ludwig-Maximilians-University Munich, Germany
Footnotes
CMAJ invites contributions to the Innovations in care column, which highlights recent diagnostic and therapeutic advances. Novel uses of older treatments will also be considered. For publication, the benefits of the innovation, its availability and its limitations must be highlighted clearly, but briefly. Visual elements (images) are essential. Submit brief evidence-based articles (maximum 1000 words and 5 references) to http://mc.manuscriptcentral.com/cmaj or email eric.wooltorton@cma.ca to discuss ideas.
Competing interests: None declared.


