Abstract
Mushrooms are low calorie food with very little fat and are highly suitable for obese persons. With no starch and very low sugars, they are the ‘delight of the diabetics’. Combination of herbal drugs (or isolated phytochemicals) is found to be beneficial in certain diseases when given along with conventional drugs. The aim of the present study was to evaluate the effects of aqueous extract of Pleurotus pulmonarius (Lentinaceae) (called as PP-aqu) and its interaction with glyburide in alloxan induced diabetic mice. The diabetic mice treated were with PP-aqu (500 mg/kg, p.o.) alone or combination with glyburide (10 mg/kg, p.o.) for 28 days. Blood samples were collected by orbital sinus puncture using heparinized capillary glass tubes and were analyzed for serum glucose on 0, 7th, 14th, 21st and 28th days. Body weights and mortality were noted during the study period. In oral glucose tolerance test (OGTT), glucose (2.5 g/kg, p.o.) was administered with either vehicle, PP-aqu alone or in combination with glyburide and serum glucose level analyzed at 0, 30, 60 and 120 min after drug administration. Administration of PP-aqu (500 mg/kg) and its combination with glyburide (10 mg/kg) significantly (P < 0.001) decreased serum glucose level in diabetic mice. In OGTT, glyburide or PP-aqu treatment alone or their combination produced significant (P < 0.001) increase in glucose threshold. Thus we suggest that P. pulmonarius showed potent and synergistic antihyperglycemic effect in combination with glyburide.
Keywords: Pleurotus pulmonarius, glyburide, serum glucose, oral glucose tolerance test (OGTT)
Introduction
Mushrooms are a group of fleshy macroscopic fungi, which until recently, as other fungi, were induced in the plant kingdom because of cell wall and spores. Mushroom have been valued throughout the world as both food and medicine for thousands of years (1–3). There are many varieties of mushrooms, species of which Pleurotus are characterized by a white spore print, attached to gills, often with an eccentric stip, or no stip at all. They are commonly known as ‘oyster mushrooms’ (4).
Mushrooms are highly nutritive as they contain good quality proteins, vitamins and minerals (5,6). Mushrooms are low calorie food with very little fat and are highly suitable for obese persons. With no starch and very low sugars, they are the ‘delight of the diabetics’ (7). In adequate quantities and low in sugars they can serve as medicinal foods for diabetes. Earlier studies have reported insulin release and insulin like activity of other mushroom species like Agaricus campestris (8–10). However, there is paucity of reports on the antihyperglycemic activity of Pleurotus.
The increasing use of herbal medicinal products in the community where people are also receiving prescription medicines suggests that adverse herb-drug interactions may be of significant public health consequence (11). Geriatric patients often add herbal medicines to medications prescribed by their physicians, yet do not always inform the physician (12). Whereas most herbal remedies, when used as directed and under the supervision of knowledgeable individuals, are safe, the potential for adverse effects or intoxications certainly exists. In addition, because nearly all herbal remedies contain multiple, biologically active constituents, interaction with conventional drugs is a concern (13–15). Hence, the likelihood of herb–drug interactions is theoretically higher than drug–drug interactions (16). On the other hand, combination of herbal drugs (or isolated phytochemicals) are found to be beneficial in certain diseases (17–19) when given along with conventional drugs. Herbal agents when given in combination with prescription medication may favorably alter pharmacokinetic (20) as well as pharmacodynamic (19,21,22) of prescription medications. However, to date there is less evidence relating to herb–drug interaction in case of antidiabetic medicines and understanding of the involved mechanisms is also far from complete (16).
Recently, we have reported the hypoglycemic effects of aqueous extract of Pleurotus pulmonarius (Fr.) Quel.-Champ in alloxan-induced diabetic mice and increased oral glucose tolerance in diabetic (OGTT model) mice at dose levels ≥250 mg/kg, p.o. (23). In this article we are reporting interaction of aqueous extract of P. pulmonarius with glyburide on serum glucose levels and oral glucose tolerance test (OGTT) in alloxan-induced diabetic mice.
Methods
Drugs and Chemicals
The mushroom of P. pulmonarius (Fr.) Quel.-Champ (Lentinaceae) was provided to us as a gift sample from Bajaj Orchard, Pvt. Ltd, Mumbai, India. It was authenticated by Dr A. M. Mujumdar, Department of Botany, at Agharkar Research Institute, Pune and voucher specimen was deposited at that Institute. Glyburide (Ranbaxy Pharma. Ltd, India), alloxan monohydrate (Spectrochem, India), glucose estimation kit (Accurex Biomedical Pvt. Ltd, India) and d-glucose (S.D. Fine-Chem. Ltd, India) were purchased from respective companies.
Experimental Animals
Swiss albino male mice (25–30 g) were purchased from National Toxicology Centre, Pune, India. They were maintained at a temperature of 25 ± 1°C and relative humidity of 45–55% under 12-h light:12-h dark cycle. The animals had free access to food pellets (Chakan Oil Mills, Pune, India) and water ad libitum. The experimental protocol was approved by the Institutional Animal Ethics Committee (IAEC) of Poona College of Pharmacy, Pune, India.
Preparation of Aqueous Extract of P. pulmonarius (PP-aqu)
Weighed quantity powder of air-dried P. pulmonarius was added to distilled water (1 : 15), boiled for 20 min on water bath, cooled to room temperature and filtered. The filtrate was dried on tray dryer at 70°C (yield 24% w/w). The dry extract powder was dissolved in distilled water to prepare drug solution at a concentration of 100 mg/ml and used for pharmacological studies.
Induction of Experimental Diabetes
Diabetes was induced in mice by a single intravenous injection of aqueous alloxan monohydrate (70 mg/kg, i.v.) (24). After 48 h, the animals showing serum glucose level above 200 mg/dl (diabetic) were selected for the study. All mice were allowed free access to tap water and pellet diet.
Collection of Blood and Determination of Serum Glucose
Blood samples from the control and experimental mice were collected by orbital sinus puncture using heparinized capillary glass tubes. The blood samples so collected were analyzed for glucose levels by glucose oxidase peroxidase (GOD/POD) method as described earlier (25) and serum glucose levels were expressed in mg/dl.
Alloxan Treated Diabetic Mice Model
The diabetic mice were divided into four groups of six animals each. The mice were administered orally with either vehicle (distilled water, 10 ml/kg), PP-aqu (500 mg/kg), glyburide (10 mg/kg) and the combination of PP-aqu (500 mg/kg) with glyburide (10 mg/kg).
Acute study involved estimation of serum glucose at 0, 2, 4, 6 and 24 h after drug administration. Subacute study involved repeated administration of drug for 28 days at prefixed time and serum glucose level was estimated on 7th, 14th, 21st and 28th day. Mean change in serum glucose level and standard error mean (SEM) were calculated. The mice were weighed daily during the study period of 28 days and their body weights were noted. From this data, mean change in body weight and SEM were calculated. The mortality of mice was also noted during the study period and percentage mortality was calculated.
Oral Glucose Tolerance Test in Alloxan Treated Diabetic Mice
Diabetic mice were divided into four groups of six animals each. The animals were fasted overnight before commencing the experiment.They were adminstred orally with either vehicle (distilled water, 10 ml/kg), PP-aqu (500 mg/kg), glyburide (10 mg/kg) and the combination of PP-aqu (500 mg/kg) with glyburide (10 mg/kg). The mice of all the groups were loaded with d-glucose (2.5 gm/kg) solution after half an hour of drug administration. Serum glucose levels were estimated 30 min prior to glucose administration and at 0, 30, 60 and 120 min after glucose loading.
Statistical Analysis
The results are expressed as mean ± SEM. Comparison between the groups was made by two-way analysis of variance (ANOVA) followed by post hoc Dunnett's test.
Results
Antihyperglycemic Influence on Serum Glucose Level in Alloxan-induced Diabetes
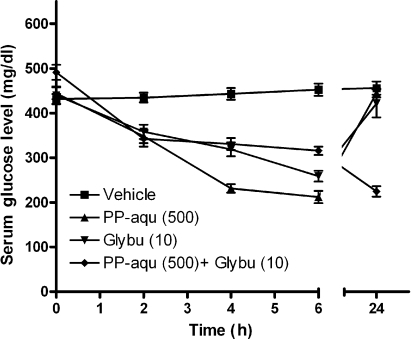
Figure 1 showed antihyperglycemic effects of various treatments against alloxan-induced diabetic mice. Acute administration of PP-aqu (500 mg/kg) showed peak decrease in serum glucose levels in alloxan-induced diabetic mice at 2 h (P < 0.001). However, effects gradually reduced at 4 h (P < 0.01) and 6 h (P <0.01). Glyburide (10 mg/kg) showed potent and significant effect (P < 0.001) at all time points tested. However, combination of PP-aqu (500 mg/kg) and glyburide (10 mg/kg) demonstrated sharp decrease (P < 0.001) in serum glucose levels at all the time points tested (Fig. 1).
Figure 1.
Effect of acute pretreatment of aqueous extract of P. pulmonarius and glyburide on serum glucose level in alloxan-induced diabetes in mice.
Sub-acute Antihyperglycemia on Serum Glucose Levels in Alloxan Induced Diabetes
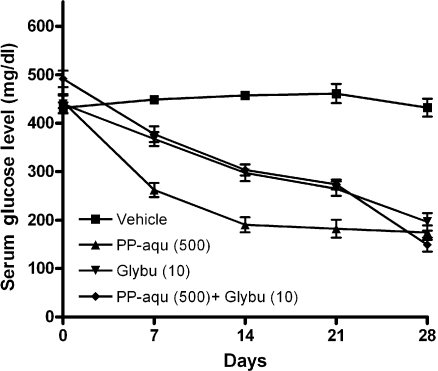
Glyburide (10 mg/kg), PP-aqu (500 mg/kg) or their combinations showed significant (P < 0.001) antihyperglycemic effect after 7th, 14th, 21st and 28th day of treatments. The effects of combinations were more pronounced than single drug treatment (Fig. 2).
Figure 2.
Effect of subacute pretreatment of aqueous extract of P. pulmonarius and glyburide on serum glucose level in alloxan induced diabetes in mice.
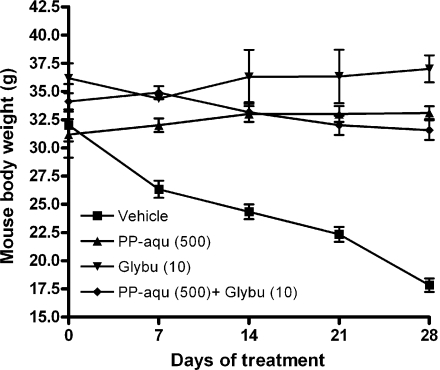
Reversal of Loss of Body Weight and Mortality Rate in Alloxan Induced Diabetes
Administration of vehicle (distilled water, 10 ml/kg, p.o.) in alloxan induced diabetic mice resulted in gradual decease (P < 0.001) in body weight during the period of 28 days (Fig. 3). All the treatments (PP-aqu or glyburide or their combinations) could reverse alloxan-induced weight loss in mice after 7th, 14th, 21st and 28th day of treatments (Fig. 3). Administration of PP-aqu alone caused 14% mortality in alloxan induced diabetic mice during 28 days study period (Data not tabulated). On single drug treatment of glyburide (10 mg/kg) caused 25% mortality, whereas combination of PP-aqu with glyburide (10 mg/kg) caused 25% mortality in mice.
Figure 3.
Effect of sub-acute pretreatment of aqueous extract of P. pulmonarius and glyburide on body weights of alloxan induced diabetes in mice.
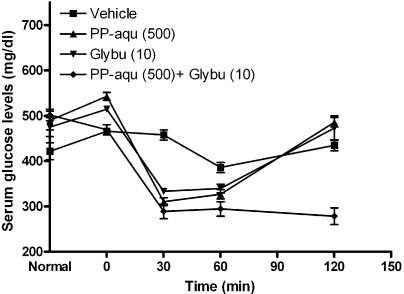
Increased Glucose Threshold in OGTT by Treatments
In the OGTT, administration of glucose load (2.5 g/kg) increased serum glucose levels significantly (P < 0.001) after 30 min of glucose loading in alloxan treated diabetic mice (Fig. 4). Glyburide (10 mg/kg) or PP-aqu treatment alone or in combination produced significant (P < 0.001) increase in glucose threshold within 30 min of glucose loading and the effects persisted till 120 min (Fig. 4 and Table 1).
Figure 4.
Effect of acute pretreatment of aqueous extract of P. pulmonarius and glyburide on serum glucose level in OGTT in mice.
Table 1.
Effect of treatments on increased glucose threshold in OGTT
| Treatment (dose in mg/kg, p.o.) | Mean serum gluose level (mg/dl) | ||||
|---|---|---|---|---|---|
| −30 | O min | 30 min | 60 min | 120 min | |
| Vehicle | 421.53 ± 18.59 | 465.76 ± 4.54 | 457.46 ± 11.22 | 385.90 ± 11.02 | 434.62 ± 12.16 |
| PP-aqu (500) | 489.35 ± 20.75 | 542.69 ± 8.44 | 310.43 ± 8.37*** | 326.69 ± 10.29*** | 485.56 ± 10.39* |
| Glybu (10) | 474.80 ± 20.85 | 514.38 ± 6.47 | 333.05 ± 5.13*** | 339.13 ± 9.56*** | 472.68 ± 7.28 |
| PP-aqu (500) + Glybu (10) | 501.44 ± 12.78 | 468.95 ± 1.25 | 288.81 ± 15.90*** | 294.37 ± 15.81*** | 278.35 ± 18.22*** |
N = 6, PP-aqu- of aqueous extract of P. pulmonarius; Glybu-Glyburide. All the groups were administrated with glucose load (2.5 g/kg) at 0 min.
*P< 0.05, ***P< 0.001.
Discussion
In the past, many mushroom varieties have been reported to possess hypoglycemic activities in animals (8,10) as well as in diabetic patients (26). Studies in normal and streptozotocin diabetic mice treated with mushroom variety, Agaricus bisporus, retards the development of hyperglycemia, hyperphagia, polydipsia, body weight loss and glycated hemoglobin in streptozotocin treated mice (10) by counteracting reduction in plasma and pancreatic insulin concentration and by improving hypoglycemic effect of exogenous insulin.
The antihyperglycemic effect of PP-aqu was limited to 6 h (with peak effect at second h) when administered alone. But combination of PP-aqu and gliburide showed sustained anti-hyperglycemic effect at 24 h (Fig. 1) suggesting the advantage of combination in long-term treatment. The more pronounced effect of the extract in alloxan-induced diabetic mice may possibly be due to limited or compromised action of insulin in diabetic condition, and conversely a greater and more direct role of the antihyperglycemic principle present in the extract. Several antihyperglycemic principles from plant origin have been reported to have antihyperglycemic effects upto 24 h (27–29). On the other hand, combination of PP-aqu with glyburide showed its peak effect at 24 h. It thus seems possible that more than one phytochemical from PP-aqu showed antihyperglycemic effect.
Moreover, PP-aqu alone or in combination with glyburide also protected the weight loss induced by alloxan in the present study (Fig. 3) and this result is supported by earlier studies from few other plant extracts (10) and so substantiates the usefulness of combination in long-term treatment of diabetes.
In OGTT, the doses of PP-aqu (500 mg/kg, p.o.) increased the tolerance for glucose (Fig. 4) suggesting increased peripheral utilization of glucose in both diabetic as well as nondiabetic (normal) mice.
Antihyperglycemic effects observed in alloxan induced mice and in OGTT can be attributed to several mechanisms. Many varieties of mushrooms have been reported to possess antihyperglycemic activity through various mechanism like glucose/insulin metabolism and/or by enhancing peripheral insulin sensitivity (9,30) or by enhancing insulin release by Islets of Langerhans (8,31). Insulin-releasing and insulin-like activity in A. campestris (a variety of mushroom) is reported earlier (8). Lectins from A. bisporus and A. campestris stimulate insulin and glucagon release from isolated rat islets in the presence of glucose and specific interaction between mushroom lectin and its receptors (leading to conformational changes in the structure of the membranes of the islet α2- and β-cells) that facilitate exocytosis is also proposed earlier (31). Effects of water-soluble extract of maitake mushroom have been reported to have antihyperglycemic activity by lowering of circulating glucose and insulin concentrations and suggested to work primarily by enhancing peripheral insulin sensitivity (32). Therefore, P. pulmonarius mediated decrease in serum glucose level in diabetic mice may mediated by one of these mechanisms.
Guanide, a known hypoglycemic substance related to biguanide class of oral antidiabetic drugs, has been detected in edible mushroom of Pleurotus species (33) and might be responsible for the antidiabetic effect. This phytochemical may be responsible for synergistic action of PP-aqu with glyburide against alloxan-induced diabetic mice as well as OGTT that is observed in our study. It is generally agreed that glyburide binds to insulin receptors on beta cells. Following this binding, closure of ATP-dependent potassium channels leads to opening of voltage-gated Ca2+ channels, an increased Ca2+ influx and the subsequent stimulation of insulin containing granules' exocytosis. (34–37) and reduces fasting plasma glucose concentration.
Mushrooms contain a variety of secondary metabolites, including various phenolic compounds, which have been may act as excellent anti-oxidants (38–42). Oxidative stress, defined as an imbalance between the production of reactive oxygen species (ROS) and anti-oxidant defense, is considered to be an important pathogenic factor in diabetes mellitus and its complications (43). It has been postulated that enhanced generation of ROS may take part in the pathogenesis of diabetic microvascular complication—retinopathy (44). The relationship of anti-oxidant potential of herbs and their antidiabetic activity have been shown many times in the past (45–50). Niacin-bound chromium constituent from Maitake mushroom (9,51) and nicotinamide (52) is reported to ameliorate diabetes mellitus in laboratory animals as well as in clinics. Therefore, anti-oxidant components in PP-aqu (niacin and ascorbic acid that are present in remarkable proportion) might play important contributory factor in the antihyperglycemic effect of P. pulmonarius.
Preliminary phytochemical analysis of P. pulmonarius showed the presence of proteins, minerals, vitamins and carbohydrates (Data not tabulated). Such constituents are confirmed also by Food and Agriculture Organization of United Nations (53). Mushrooms consist of ∼20–35% proteins. The glycoproteins constituents have been shown to have antihypergycemic effect (54).
Conclusions
It was thus apparent from the results that PP-aqu (500 mg/kg) showed significant antihyperglycemic effect in alloxan induced diabetic mice. It not only halts progression of diabetes (as it reduced weight loss) but also reduced the mortality of alloxan induced diabetic mice by ∼50%. PP-aqu (500 mg/kg) in combination with glyburide (10 mg/kg) showed potent synergistic antihyperglycemic effects probably due to increased insulin secretion. The results from OGTT also supports the possibility of effective combination therapy of P. pulmonarius with glyburide as an effective anti-diabetic therapy. The marked and prolonged activity necessitates a more comprehensive chemical and pharmacological investigation to elucidate the exact mechanism and to isolate and identify it's active principle(s).
Acknowledgements
The authors acknowledge Dr S. S. Kadam, Principal and Dr K. R. Mahadik Vice-Principal, Poona College of Pharmacy, Bharati Vidyapeeth Deemed University, Pune for providing necessary facilities to carry out the study. We are also thankful to Bajaj Orchard, a division of Trinity Bio-Tech, Mumbai, India, for sending us a gift sample of P. Pulmonarius.
References
- 1.Lindequist U, Niedermeyer TH, Julich WD. The pharmacological potential of mushrooms. Evid Based Complement Alternat Med. 2005;2:285–99. doi: 10.1093/ecam/neh107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wright T. Nutraceuticals World. Ramsey, NJ: Roman Publishing; 2004. Medicinal mushrooms; pp. 26–9. [Google Scholar]
- 3.Tribe I, Tosco U. The World of Mushrooms. Vol viii. London: Orbis Publishing; 1973. [Google Scholar]
- 4.Miles PG, Chang S-T. Mushroom Biology: Concise Basics and Current Development. New York: World Scientific Publishing Company; 1997. [Google Scholar]
- 5.Khanna P, Garcha HS. Pleurotus mushroom- A source of food protein. Mushroom News Lett Tropics. 1984;4:9–14. [Google Scholar]
- 6.Flegg PB, Maw GA. Mushroom and their possible contribution to world protein needs. Mushroom J. 1976;48:396–405. [Google Scholar]
- 7.Bano Z. The nutritive value of mushrooms. Paper presented at: First Symposium on survey and cultivation of edible mushrooms of India; 1976; Regional Research Laboratory, Jammu. pp. 148–69. [Google Scholar]
- 8.Gray AM, Flatt PR. Insulin-releasing and insulin-like activity of Agaricus campestris (mushroom) J Endocrinol. 1998;157:259–66. doi: 10.1677/joe.0.1570259. [DOI] [PubMed] [Google Scholar]
- 9.Talpur N, Echard B, Dadgar A, Aggarwal S, Zhuang C, Bagchi D, et al. Effects of Maitake mushroom fractions on blood pressure of Zucker fatty rats. Res Commun Mol Pathol Pharmacol. 2002;112:68–82. [PubMed] [Google Scholar]
- 10.Swanston-Flatt SK, Day C, Flatt PR, Gould BJ, Bailey CJ. Glycaemic effects of traditional European plant treatments for diabetes. Studies in normal and streptozotocin diabetic mice. Diabetes Res. 1989;10:69–73. [PubMed] [Google Scholar]
- 11.Coxeter PD, McLachlan AJ, Duke CC, Roufogalis BD. Herb-drug interactions: an evidence based approach. Curr Med Chem. 2004;11:1513–25. doi: 10.2174/0929867043365198. [DOI] [PubMed] [Google Scholar]
- 12.Bressler R. Herb-drug interactions: interactions between kava and prescription medications. Geriatrics. 2005;60:24–25. [PubMed] [Google Scholar]
- 13.Poppenga RH. Herbal medicine: potential for intoxication and interactions with conventional drugs. Clin Tech Small Anim Pract. 2002;17:6–18. doi: 10.1053/svms.2002.27785. [DOI] [PubMed] [Google Scholar]
- 14.Fugh-Berman A, Ernst E. Herb-drug interactions: review and assessment of report reliability. Br J Clin Pharmacol. 2001;52:587–95. doi: 10.1046/j.0306-5251.2001.01469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woodward KN. The potential impact of the use of homeopathic and herbal remedies on monitoring the safety of prescription products. Hum Exp Toxicol. 2005;24:219–33. doi: 10.1191/0960327105ht529oa. [DOI] [PubMed] [Google Scholar]
- 16.Izzo AA. Herb-drug interactions: an overview of the clinical evidence. Fundam Clin Pharmacol. 2005;19:1–16. doi: 10.1111/j.1472-8206.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 17.Samane S, Noel J, Charrouf Z, Amarouch H, Haddad PS. Insulin-sensitizing and anti-proliferative effects of Argania spinosa seed extracts. Evid Based Complement Alternat Med. 2006;3:317–27. doi: 10.1093/ecam/nel015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng C, Liu Y, Wang Z, He D, Huang L, Yu P, et al. Activation of D3 dopamine receptor decreases angiotensin II type 1 receptor expression in rat renal proximal tubule cells. Circ Res. 2006;99:494–500. doi: 10.1161/01.RES.0000240500.96746.ec. [DOI] [PubMed] [Google Scholar]
- 19.Kelly KM. Complementary and alternative medical therapies for children with cancer. Eur J Cancer. 2004;40:2041–6. doi: 10.1016/j.ejca.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Singh M, Varshneya C, Telang RS, Srivastava AK. Alteration of pharmacokinetics of oxytetracycline following oral administration of Piper longum in hens. J Vet Sci. 2005;6:197–200. [PubMed] [Google Scholar]
- 21.Lin YC, Bioteau AB, Ferrari LR, Berde CB. The use of herbs and complementary and alternative medicine in pediatric preoperative patients. J Clin Anesth. 2004;16:4–6. doi: 10.1016/j.jclinane.2003.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Awang DV, Fugh-Berman A. Herbal interactions with cardiovascular drugs. J Cardiovasc Nurs. 2002;16:64–70. doi: 10.1097/00005082-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Badole SL, Shah SN, Patel NN, Thakurdesai PA, Bodhankar SL. Hypoglycemic activity of aqueous extract of Pleurotus pulmonarius (Fr.) Quel.-Champ in alloxan induced diabetic mice. Pharm Biol. 2006;44:421–5. doi: 10.1093/ecam/nem010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rao BK, Kesavulu MM, Giri R, Appa Rao C. Antidiabetic and hypolipidemic effects of Momordica cymbalaria Hook. fruit powder in alloxan-diabetic rats. J Ethnopharmacol. 1999;67:103–9. doi: 10.1016/s0378-8741(99)00004-5. [DOI] [PubMed] [Google Scholar]
- 25.Abdel-Barry JA, Abdel-Hassan IA, Al-Hakiem MH. Hypoglycaemic and antihyperglycaemic effects of Trigonella foenum- graecum leaf in normal and alloxan induced diabetic rats. J Ethnopharmacol. 1997;58:149–55. doi: 10.1016/s0378-8741(97)00101-3. [DOI] [PubMed] [Google Scholar]
- 26.Konno S, Tortorelis DG, Fullerton SA, Samadi AA, Hettiarachchi J, Tazaki H. A possible hypoglycaemic effect of maitake mushroom on type 2 diabetic patients. Diabet Med. 2001;18:1010. doi: 10.1046/j.1464-5491.2001.00532-5.x. [DOI] [PubMed] [Google Scholar]
- 27.Hikino H, Takahashi M, Konno C, Ishimori A, Kawamura T, Namiki T. Effect of glycans of Saccharum officinarum on carbohydrate and lipid metabolism of rats. J Ethnopharmacol. 1985;14:261–8. doi: 10.1016/0378-8741(85)90092-3. [DOI] [PubMed] [Google Scholar]
- 28.Akhtar MS, Khan QM, Khaliq T. Effects of Portulaca oleracae (Kulfa) and Taraxacum officinale (Dhudhal) in normoglycaemic and alloxan-treated hyperglycaemic rabbits. J Pak Med Assoc. 1985;35:207–10. [PubMed] [Google Scholar]
- 29.Takahasi M, Konno C, Hikino H. Isolation and hypoglycemic activity of Anemorans A, B, C and D, glycans of Anemarrhema asphodelcides rhizomes. Planta Med. 1985;51:100–2. doi: 10.1055/s-2007-969417. [DOI] [PubMed] [Google Scholar]
- 30.Talpur NA, Echard BW, Fan AY, Jaffari O, Bagchi D, Preuss HG. Antihypertensive and metabolic effects of whole Maitake mushroom powder and its fractions in two rat strains. Mol Cell Biochem. 2002;237:129–36. doi: 10.1023/a:1016503804742. [DOI] [PubMed] [Google Scholar]
- 31.Ewart RB, Kornfeld S, Kipnis DM. Effect of lectins on hormone release from isolated rat islets of langerhans. Diabetes. 1975;24:705–14. doi: 10.2337/diab.24.8.705. [DOI] [PubMed] [Google Scholar]
- 32.Manohar V, Talpur NA, Echard BW, Lieberman S, Preuss HG. Effects of a water-soluble extract of maitake mushroom on circulating glucose/insulin concentrations in KK mice. Diabetes Obes Metab. 2002;4:43–8. doi: 10.1046/j.1463-1326.2002.00180.x. [DOI] [PubMed] [Google Scholar]
- 33.Windholz M. The Merck index: an encyclopedia of chemicals, drugs and biologicals. 10th. New Jersey: Merck & Co.; 1983. [Google Scholar]
- 34.Boyd AE. Sulfonylurea receptors, ion channels, and fruit flies. Diabetes. 1988;37:847–50. doi: 10.2337/diab.37.7.847. [DOI] [PubMed] [Google Scholar]
- 35.Groop LC. Sulfonylureas in NIDDM. Diabetes Care. 1992;15:737–54. doi: 10.2337/diacare.15.6.737. [DOI] [PubMed] [Google Scholar]
- 36.Patane G, Piro S, Anello M, Rabuazzo AM, Vigneri R, Purrello F. Exposure to glibenclamide increases rat beta cells sensitivity to glucose. Br J Pharmacol. 2000;129:887–92. doi: 10.1038/sj.bjp.0703131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elmi A, Idahl LA, Sehlin J. Relationships between the Na(+)/K(+) pump and ATP and ADP content in mouse pancreatic islets: effects of meglitinide and glibenclamide. Br J Pharmacol. 2000;131:1700–06. doi: 10.1038/sj.bjp.0703745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ishikawa Y, Morimoto K, Hamasaki T. Flavoglaucin, a metabolite of Eurotium Chevalieri, its antioxidation and synergism with tocopherol. J Am Oil Chem Soc. 1984;61:1864–8. [Google Scholar]
- 39.Mau JL, Lin HC, Song SF. Antioxidant properties of several specialty mushrooms. Food Res Int. 2002;35:519–26. [Google Scholar]
- 40.Cheung PC, Lee MY. Fractionation and characterization of mushroom dietary fiber (nonstarch polysaccharides) as potential nutraceuticals from sclerotia of Pleurotus tuber-regium (Fries) singer. J Agric Food Chem. 2000;48:3148–51. doi: 10.1021/jf000382s. [DOI] [PubMed] [Google Scholar]
- 41.Fu H, Shieh DE. Antioxidant and free radical scavenging activities of edible mushrooms. J Food Lipids. 2002;9:35–46. [Google Scholar]
- 42.Yang JH, Lin HC, Mau JL. Antioxidant properties of several commercial mushrooms. Food Chem. 2002;77:229–35. [Google Scholar]
- 43.Gumieniczek A, Hopkala H, Rolinski J, Bojarska-Junak A. Antioxidative and anti-inflammatory effects of repaglinide in plasma of diabetic animals. Pharmacol Res. 2005;52:162–6. doi: 10.1016/j.phrs.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 44.Siemianowicz K, Gminski J, Telega A, Wojcik A, Posielezna B, Grabowska-Bochenek R, et al. Blood antioxidant parameters in patients with diabetic retinopathy. Int J Mol Med. 2004;14:433–7. [PubMed] [Google Scholar]
- 45.Reddy SV, Tiwari AK, Kumar US, Rao RJ, Rao JM. Free radical scavenging, enzyme inhibitory constituents from antidiabetic Ayurvedic medicinal plant Hydnocarpus wightiana Blume. Phytother Res. 2005;19:277–81. doi: 10.1002/ptr.1491. [DOI] [PubMed] [Google Scholar]
- 46.Satheesh MA, Pari L. Antioxidant effect of Boerhavia diffusa L. in tissues of alloxan induced diabetic rats. Indian J Exp Biol. 2004;42:989–92. [PubMed] [Google Scholar]
- 47.Sabu MC, Kuttan R. Antidiabetic activity of Aegle marmelos and its relationship with its antioxidant properties. Indian J Physiol Pharmacol. 2004;48:81–8. [PubMed] [Google Scholar]
- 48.Ramkumar KM, Latha M, Venkateswaran S, Pari L, Ananthan R, Bai VN. Modulatory effect of Gymnema montanum leaf extract on brain antioxidant status and lipid peroxidation in diabetic rats. J Food Med. 2004;7:366–71. doi: 10.1089/jmf.2004.7.366. [DOI] [PubMed] [Google Scholar]
- 49.Vedavanam K, Srijayanta S, O'Reilly J, Raman A, Wiseman H. Antioxidant action and potential antidiabetic properties of an isoflavonoid-containing soyabean phytochemical extract (SPE) Phytother Res. 1999;13:601–8. doi: 10.1002/(sici)1099-1573(199911)13:7<601::aid-ptr550>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 50.Kumari K, Augusti KT. Antidiabetic and antioxidant effects of S-methyl cysteine sulfoxide isolated from onions (Allium cepa Linn) as compared to standard drugs in alloxan diabetic rats. Indian J Exp Biol. 2002;40:1005–9. [PubMed] [Google Scholar]
- 51.Talpur N, Echard BW, Yasmin T, Bagchi D, Preuss HG. Effects of niacin-bound chromium, Maitake mushroom fraction SX and (-)-hydroxycitric acid on the metabolic syndrome in aged diabetic Zucker fatty rats. Mol Cell Biochem. 2003;252:369–77. doi: 10.1023/a:1025564930088. [DOI] [PubMed] [Google Scholar]
- 52.Pan J, Chan EK, Cheta D, Schranz V, Charles MA. The effects of nicotinamide and glimepiride on diabetes prevention in BB rats. Life Sci. 1995;57:1525–32. doi: 10.1016/0024-3205(95)02125-3. [DOI] [PubMed] [Google Scholar]
- 53.Food and Agriculture Organization of the United Nations. Food Composition Table for Use in Africa. Vol ix. Bethesda, MD: US Department of Health, Education, and Welfare, Nutrition Program, and Food Consumption and Planning Branch, Food and Agriculture Organization of the United Nations; 1968. [Google Scholar]
- 54.Kusano S, Abe H, Tamura H. Isolation of antidiabetic components from white-skinned sweet potato (Ipomoea batatas L.) Biosci Biotechnol Biochem. 2001;65:109–14. doi: 10.1271/bbb.65.109. [DOI] [PubMed] [Google Scholar]