Abstract
In the current study, 96 married chronic pain patients were recruited from the community to test hypotheses about the roles of catastrophizing and psychological distress in relation to perceived support from close others. It was expected that pain duration would moderate the relationship between catastrophizing and perceived support and between catastrophizing and psychological distress. In addition, distress was hypothesized to mediate the relationship between the pain duration-catastrophizing interaction and support. Hierarchical regression analyses showed that pain duration interacted with catastrophizing such that at shorter pain durations, pain catastrophizing was related to more perceived solicitous spouse responses; however no such relationship existed for patients with longer pain durations. In contrast, catastrophizing was significantly related to less perceived spousal support (i.e. support not specific to pain) in patients with longer durations of pain whereas no significant relationship existed for patients with shorter pain durations. Pain duration did not interact with catastrophizing in relating to psychological distress, which precluded the examination of distress as a mediator between the pain duration-catastrophizing interaction and support. Moreover, psychological distress did not significantly mediate the relationships between pain catastrophizing and perceived support. These findings are discussed in the context of cognitive-behavioral and interpersonal perspectives of pain.
Keywords: Pain catastrophizing, Psychological distress, Social support
1. Introduction
Recent conceptualizations of pain catastrophizing (i.e. a negative and exaggerated focus on pain) have focused on the interpersonal (Sullivan et al., 2000, 2001a) nature of this construct. According to the communal coping perspective, individuals with chronic pain (ICPs) may communicate distress and garner support from close others by verbalizing catastrophic thoughts or engaging in pain or catastrophizing behaviors (Sullivan et al., 2000, 2001a; Thorn et al., 2003). Research supports a relationship between catastrophizing as assessed by the Pain Catastrophizing Scale (Sullivan et al., 1995) and solicitous responses from others (Giardino et al., 2003). Further study of the catastrophizing-support association may provide additional insights into the consistent relationship between others’ responses and ICPs’ negative outcomes (e.g. psychological distress, disability; Cano et al., 2000, 2004; Flor et al., 1987; Kerns et al., 1990; Romano et al., 1995; Turk et al., 1992).
In the current study of married ICPs, pain duration is identified as a variable with important implications for the study of catastrophizing and support. At shorter pain durations, spouses may reinforce the catastrophizing by providing emotional and pain-specific support because they believe that ICPs are making reasonable requests for help. However, spouses may withdraw from or react negatively to catastrophizing after helping attempts are unsuccessful and frustrating. Therefore, pain catastrophizing is expected to be related positively to perceived support in the early stages of the pain problem but negatively to support at longer pain durations. Several support variables are assessed to determine the extent of the catastrophizing effect.
In contrast to the interpersonal view, catastrophizing has also been conceptualized as a cognitive strategy that prevents ICPs from disengaging their attention from pain stimuli (Crombez et al., 1998; Eccleston and Crombez, 1999; Van Damme et al., 2004). Continued catastrophizing may be associated with helplessness and depressive symptoms (Keefe et al., 1989; Rosenstiel and Keefe, 1983; Turner et al., 2000) because ICPs cannot escape from chronic pain or maintain attention on other tasks. From this perspective, it is expected that the relationship between catastrophizing and psychological distress will be especially strong for ICPs with longer pain durations because they may feel more helpless.
The interpersonal and cognitive perspectives noted above are not necessarily mutually exclusive. Catastrophizing may simultaneously exacerbate psychological distress and serve a communicative function. Consequently, distress may also have a role in the catastrophizing-support association. Interactional perspectives (e.g. Coyne, 1976) suggest that depressed ICPs seek reassurance from close others in a manner that elicits unsupportive and rejecting reactions. Indeed research supports this hypothesis (e.g. Joiner et al., 1992; Wade and Kendler, 2000). In ICPs with longer pain durations, catastrophizing per se may not be related to less perceived support. Rather, psychological distress and associated reassurance-seeking may be more important in relating to support. In the current study, distress is expected to explain the relationship between catastrophizing and support in ICPs with longer pain durations. In other words, distress is expected to mediate the association between the catastrophizing-pain duration interaction and perceived support.
2. Method
2.1. Participants
Married ICPs (N = 96) were recruited from the Detroit metropolitan area community via newspaper advertisements A married patient sample offers the best opportunity to study the communal coping hypothesis because committed romantic relationships can be very intimate and because partners are expected to have a high frequency of contact with each other. The majority of patients were women (59.8%, n = 58). Caucasians comprised 57.7% of the sample (n = 56), followed by African-Americans (38.1%, n = 37), and participants of other ethnicities (4.1%, n = 4). All ICPs had musculoskeletal pain with the most common pain diagnoses being osteoarthritis (n = 42, 44% and spine problems (e.g. degenerative disc disease, scoliosis; n = 31, 32%). Participants also reported other chronic muscle pain, chronic post-surgical pain, and pain stemming from fractures and bone spurs. The most common pain sites were low back (n = 41, 43%) and knee (n = 38, 40%) but participants also reported musculoskeletal pain in other sites (e.g. upper back, shoulders). Table 1 presents other descriptive information about this sample. The vast majority of ICPs reported seeking treatment for their pain (89%, n = 85). Of those who sought pain treatment, most reported seeking treatment from their primary care physicians. ICPs reported a wide range of pain durations with a mean of 9.56 years (SD 10.96; minimum 3 months, maximum 50 years). There were no significant gender differences on pain catastrophizing, pain duration, support variables, psychological distress, or pain severity.
Table 1.
Demographic characteristics of the sample
| Variable | M | SD |
|---|---|---|
| Age | 53.34 | 13.82 |
| Education in years | 14.32 | 2.67 |
| Years married | 21.36 | 16.71 |
| Pain duration in years | 9.56 | 10.96 |
| % |
n |
|
| Work statusa | ||
| Student, part- or full-time work | 38 | 36 |
| Worker's compensation/disability | 20 | 19 |
| Retired | 33 | 31 |
| Unemployed (not retired or receiving benefits) | 7 | 7 |
| Pain treatment soughtb | ||
| Primary care physician | 75 | 67 |
| Physical or occupational therapy | 75 | 67 |
| Neurologist or anesthesiologist | 46 | 41 |
| Chiropractor | 37 | 33 |
| Multidisciplinary pain clinic | 15 | 13 |
| Psychologist | 5 | 6 |
| Other (e.g. massage, acupuncture) | 32 | 28 |
N = 96 unless otherwise noted.
N = 93.
N = 89; percentages do not sum to 100% because some participants chose multiple categories.
2.2. Measures
2.2.1. Pain catastrophizing
Pain Catastrophizing was measured with the Pain Catastrophizing Scale (PCS; Sullivan et al., 1995). The PCS was designed to assess various dimensions of catastrophizing about pain. Factor analyses show that the PCS consists of the magnification (e.g. “I wonder whether something serious may happen”), rumination (e.g. “I keep thinking about how much it hurts”), and helplessness (e.g. “There is nothing I can do to reduce the intensity of the pain”) subscales (Sullivan et al., 1995; Van Damme et al., 2002). These subscales were highly correlated with one another in the current sample (r ranged from 0.72 to 0.79) and results were similar for each of the subscales. Therefore, the total catastrophizing score was used to prevent redundancy in the results and control for Type 1 error. The mean PCS score was 18.30 (SD 13.16). The PCS had excellent internal consistency in the current study (α = 0.95).
2.2.2. Psychological distress
Psychological Distress was measured with the Mood and Anxiety Symptom Questionnaire (MASQ; Watson and Clark, 1991). The MASQ is a theoretically- and empirically-derived measure of depressive and anxiety symptoms with excellent discriminant and convergent validity (Watson et al., 1995a,b), and a stable factor structure in clinic and community chronic pain patient samples (Geisser et al., 2003). The MASQ comprises 3 factors: lack of positive affect (e.g. “Felt like I had a lot to look forward to,” “Felt really good about myself” [both reverse coded]), general distress (e.g. “Felt withdrawn from others, ” “Worried a lot about things,” “Felt dissatisfied with everything”), and physiological hyperarousal (e.g. “Felt dizzy or light-headed,” “Had a lump in my throat,” “Hands were cold or sweaty”). Participants reported on their psychological distress during the past week including the day of assessment. Only the general distress scale (18 items; α = 0.93) was used because it consists of diffuse depressive and anxiety symptoms that are commonly considered psychological distress. Anhedonia and somatic symptoms are less theoretically important to the issues addressed in the current study.
2.2.3. Perceived support variables
Perceived support variables in this study included pain-specific spousal support (i.e. spouse responses to pain), perceived social support without reference to a specific person (i.e. general support), and spousal support that was not pain-specific. Spouse responses are conceptualized as perceived support because the communal coping hypothesis does not differentiate between general and pain-specific forms of social support. In addition, ICPs may consider solicitousness (i.e. getting the patient something to eat when s/he is in pain) as supportive behavior. Including both pain-specific and general forms of support will ascertain whether the communal coping hypothesis extends to all forms of perceived support. Perceived spouse responses to pain were assessed with the negative (4 items; e.g. “Your spouse expresses irritation at you when you are in pain”), solicitous (6 items; e.g. “Your spouse gets you something to eat or drink when you are in pain”), and distracting (4 items; e.g. “Your spouse talks to you about something else to take your mind off the pain”) spouse response to pain subscales of the Multidimensional Pain Inventory (Kerns et al., 1985), which has been shown to have good construct and discriminant validity, internal consistency, and test–retest reliability (Kerns et al., 1985; Kerns and Jacob, 1992). Inter-item reliability was good for all 3 spouse response subscales (α ranged from .72 to .84). ICPs reported means of 1.87 (SD. 1.63) on negative spouse responses to pain, 3.84 (SD 1.48) on solicitous spouse responses, and 2.73 (SD 1.48) on distracting responses. The negative spouse response mean is similar to clinic samples of pain patients (e.g. Cano et al., 2004; Kerns et al., 1990) whereas the solicitous and distracting spouse response means were approximately 1 point higher than means found in clinic samples (e.g. Kerns et al., 1990). The standard deviations were also similar if not slightly larger than in clinic samples.
2.2.4. Perceived social support
Perceived social support was assessed with the Social Provisions Scales (Cutrona, 1989; Cutrona and Russell, 1987) which allow participants to respond to each item using a 5-point Likert scale. The social support scale (24 items; Cutrona and Russell, 1987) was used to assess perceived general support from the entire social network of the patient. Different patterns of relationships between catastrophizing and spousal versus other sources of support were not expected; however, it is possible that the catastrophizing and support are only associated when considering support from the spouse versus support from others with whom the patient does not have as much contact. Only Giardino et al. (2003) approached this idea of specificity. They found that catastrophizing was more strongly related to solicitous responses for patients who live with romantic partners than for patients who live with others. However, they did not use a measure of perceived social support. Items tapping general support include “There are people I can depend on to help me if I really need help,” “I have close relationships that provide me with a sense of emotional security and well-being,” and “There are people I can count on in an emergency.” The romantic partner-specific scale (12 items; Cutrona, 1989) was used to measure perceived spousal support. Sample items from the spousal support scale include “I would feel comfortable talking about problems with my spouse” and “Would your relationship with your spouse provide you with a sense of emotional security and well-being?” Reliability was good for the general support scale (α = 0.65−0.76; Cutrona and Russell, 1987) and for the spouse-specific scale (α = 0.88; Cutrona, 1989). In the current study, inter-item reliabilities were excellent (general support α = 0.90; spousal support α = 0.85). For clarity, ‘spousal support’ is used to denote the spouse-specific Social Provisions scale, ‘general support’ is used to denote the general Social Provisions scale, and ‘spouse responses’ are used to denote the pain-specific support scales from the MPI. Note that each of these measures assessed perceived, not actual, support.
2.2.5. Pain severity
Last, pain severity was also assessed by the MPI (Kerns et al., 1985) and was used in this study as a potential covariate. In the current study, inter-item reliability was good (α = 0.76). Participants reported a mean pain severity of 2.76 (SD 0.88), which is slightly lower than in clinic samples (e.g. Cano et al., 2000, 2004; Kerns et al., 1990).
2.3. Procedure
Newspaper advertisements were used to recruit married couples in which one spouse reported chronic pain for a larger study of couples and pain. Interested callers were screened over the telephone to ensure they met the following inclusion requirements: they were married and living together, both spouses were interested in participating in the study, one spouse reported chronic musculoskeletal pain, neither spouse was terminally ill, neither spouse was currently psychotic, and both spouses had adequate cognitive function as measured by the Mini-Mental Status Examination (Folstein et al., 1975). Adequate cognitive function was suggested by a minimum score of 18 out of the maximum 20 points that could be obtained for verbal responses. Only verbal items were administered because the screening was conducted over the telephone. Eligible couples were then scheduled for an appointment at the laboratory where they completed consent forms, surveys, and interviews. Couples were paid $100 upon completion of the study. Only data from ICPs are included in this paper.
3. Results
3.1. Analysis plan
The variables were first subjected to a Kolmogorov–Smirnov test to determine whether the variables were normally distributed. The analyses indicated that pain duration and psychological distress were positively skewed whereas perceived spousal support was negatively skewed. A similar pattern of results was found when using transformed or untransformed variables; therefore, untransformed variables were used for ease of interpretation.
Pearson Product-Moment Correlations were first conducted to examine the bivariate relationships between ICPs’ catastrophizing, perceived spouse responses to pain, perceived general support, perceived spousal support, and psychological distress. Given the number of correlations, a more conservative significance level of P < 0.01 was chosen to control for Type I error.
Next, hierarchical multiple regressions were conducted to test the hypotheses that the main effects of catastrophizing and pain duration and the interaction between the two were related to the five support variables (i.e. perceptions of negative, solicitous, and distracting spouse responses to pain, perceived general support, perceived spousal support). Thus, the regressions would reveal potentially different patterns of associations between catastrophizing and pain duration in relating to the various support constructs. A similar hierarchical regression was conducted to test the hypothesis that the main effects of catastrophizing and pain duration and the interaction between the two were related to psychological distress. Cohen's (1988) guidelines were used to describe the size of the correlation and regression effects (i.e. small, medium, large).
Pain severity was included as a covariate in the regression analyses when its correlation with the dependent variables approached or achieved significance as per Keppel (1982) (i.e. perceptions of negative spouse responses, perceived general support, perceived spousal support, psychological distress, see Table 2). Following the recommendations of Cohen (1988) and Holmbeck (2002), the main effects of catastrophizing and pain duration were centered prior to analysis and entered in the next step of the hierarchical regression. The interaction term was entered last. Post hoc probing of significant interactions was performed to provide the simple slopes of pain catastrophizing for one standard deviation above the mean on pain duration (i.e. +1 SD; M = 20.52 years), the mean on pain duration (M = 9.56 years), and one standard deviation below (i.e. −1 SD; M = −1.40 years) the mean on pain duration. Although one standard deviation below the mean is a negative number that cannot be achieved, including this level along with the other levels of analysis shows the changing patterns of relationships between catastrophizing and support at different pain durations while keeping with the recommendation of Cohen (1988) and Holmbeck (2002) in the post hoc analysis of interactions. Of primary interest was whether the simple slopes were significant and in the hypothesized directions; therefore, a more conservative significance level of .01 was chosen to control for Type 1 error in detecting simple slopes.
Table 2.
Correlations between catastrophizing, support variables, and psychological distress
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Pain catastrophizing | ||||||||
| 2 | Pain duration | −0.11 | |||||||
| 3 | Psychological distress | 0.56** | −0.02 | ||||||
| 4 | Solicitous spouse responses | 0.26† | 0.06 | 0.04 | |||||
| 5 | Distracting spouse responses | 0.22† | 0.14 | 0.06 | 0.74* | ||||
| 6 | Negative spouse responses | 0.16 | −0.10 | 0.40** | −0.22† | −0.11 | |||
| 7 | Perceived general support | −0.29* | 0.03 | −0.52** | 0.10 | 0.07 | −0.53** | ||
| 8 | Perceived spousal support | −0.19 | 0.05 | −0.34** | 0.27* | 0.21† | −0.66** | 0.49** | |
| 9 | Pain severity | 0.30* | 0.03 | 0.43** | 0.02 | 0.09 | 0.34** | −0.27* | −0.21† |
N = 96
P < 0.05
P < 0.01
P < 0.001.
If the conditions for mediation were supported (Baron and Kenny, 1986; Holmbeck, 2002), the third hypothesis about distress as a mediator of the relationship between the catastrophizing-pain duration interaction and support would also be tested with hierarchical regression. In this case, variables would be entered in separate steps in the following order: pain severity (if significant covariate), main effects of pain catastrophizing and pain duration, the interaction between catastrophizing and pain duration, and psychological distress. If the entry of psychological distress diminished the effect of the interaction, mediation is suggested. The extent of the mediation effect can be tested using Holmbeck's (2002) and Baron and Kenny's (1986)'s procedures.
3.2. Correlations
Although the support variables were significantly correlated with each other or approached significance, the moderate size of the correlations suggests that the measures assessed different types of support. However, the high correlation between perceptions of distracting and solicitous spouse responses, r = 0.74, P < 0.001, suggests that there is substantial overlap between these two variables. Pain catastrophizing was correlated negatively with perceived general support, a medium effect. There were trends for catastrophizing to relate positively to both perceptions of distracting and solicitous spouse responses (small to medium effects). Catastrophizing was also positively related to psychological distress, a large effect. Psychological distress was positively correlated with perceptions of negative spouse responses and negatively correlated with spousal support and general support (medium to large effects).
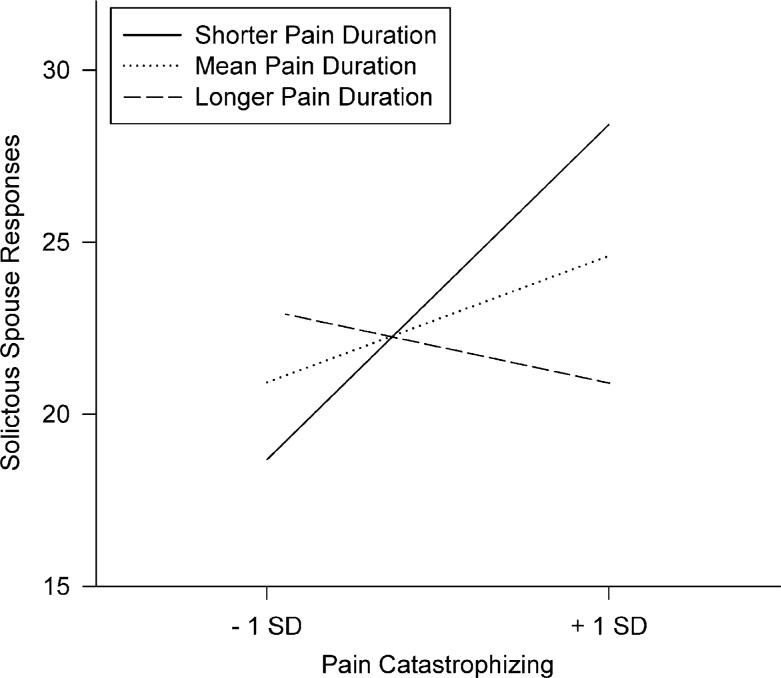
3.3. Hierarchical regressions: perceived support
The interaction between pain duration and catastrophizing was significant for perceived solicitous spouse responses, a medium effect (see Table 3). The simple slopes from post-hoc probing are displayed in Fig. 1. As predicted, pain catastrophizing was positively and significantly related to perceived solicitous spouse responses to pain among participants with shorter pain durations. Pain catastrophizing was also positively related to perceived solicitous spouse responses among participants with average pain durations; however, this relationship failed to reach the significance set at P < 0.01 for the post-hoc comparisons. Catastrophizing and solicitous spouse responses were not significantly related to each other in participants with longer pain durations.
Table 3.
Summary of hierarchical regression for pain catastrophizing, pain duration, and their interaction in relating to perceived support
| B | SE | Beta | |
|---|---|---|---|
| Solicitous spouse responses to paina | |||
| Step 1 | |||
| Pain duration | 0.01 | 0.01 | 0.08 |
| Pain catastrophizing | 0.15 | 0.07 | 0.22* |
| Step 2 | |||
| Pain duration X | −0.002 | 0.001 | −0.29* |
| Pain catastrophizing | |||
| Perceived spousal supportb | |||
| Step 1 | |||
| Pain severity | −0.37 | 0.27 | −0.15 |
| Pain duration | 0.003 | 0.01 | 0.04 |
| Pain catastrophizing | −0.12 | 0.07 | −0.18* |
| Step 2 | |||
| Pain duration X | −0.002 | 0.001 | −0.32* |
| Pain catastrophizing |
N = 96; ** P < 0.01.
P < 0.05
R2 = 0.05 for step 1; ΔR2 = 0.05 for step 2 (P < 0.05).
R2 = 0.07; P < 0.08 for step 1; ΔR2 = 0.07, P < 0.01 for step 2.
Fig. 1.
The interaction between pain duration and pain catastrophizing in relating to perceptions of solicitous spouse responses to pain. Post-hoc probing of the simple slopes indicated that pain catastrophizing was positively related to solicitous spouse responses to pain among participants with shorter (−1 SD) pain durations (B 0.37, SE 0.12, Beta = 0.55, t = 3.22, P < 0.01). There was a trend for mean pain duration in the same direction (B = 0.14, SE 0.07, Beta = 0.21, t = 2.16, P < 0.04). However, catastrophizing and solicitous spouse responses were not significantly related in participants with longer (+1 SD) pain durations (B = −0.08, SE = 0.12, Beta = −0.13, t = −0.70 P > 0.48).
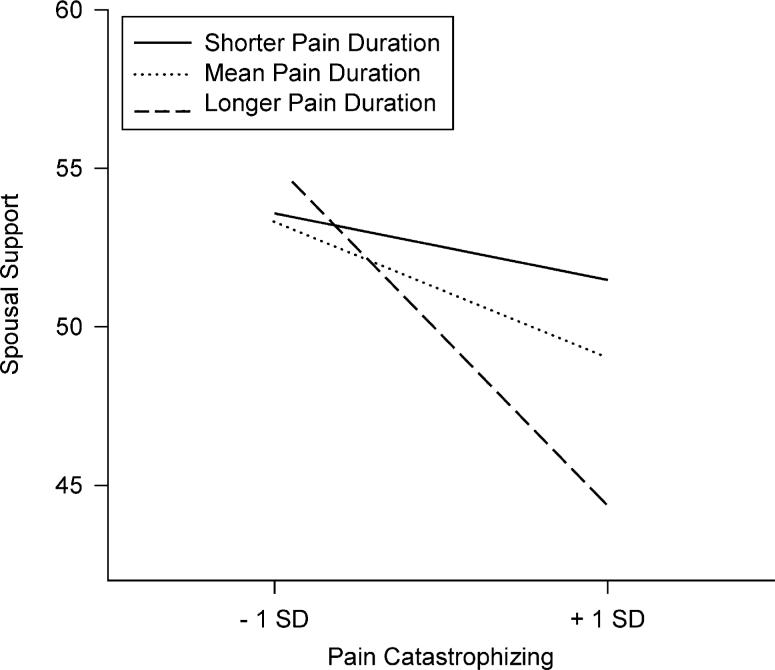
A significant interaction between pain duration and catastrophizing, a medium effect, was also found for perceived spousal support even when pain severity was entered in the first step of the analysis (see Table 3). Post-hoc probing showed that pain catastrophizing was negatively and significantly related to perceived spousal support for participants with longer pain durations (see Fig. 2 for presentation of simple slopes). A similar trend was found for participants with average pain durations. These findings are consistent with the hypothesis. However, catastrophizing and spousal support were not significantly related for participants with shorter pain durations. These results were the same whether or not pain severity was included in the post-hoc probing; therefore, simple slopes were computed without pain severity.
Fig. 2.
The interaction between pain duration and pain catastrophizing in relating to perceived spousal support. Post-hoc probing of the simple slopes indicated that pain catastrophizing was negatively related to perceived spousal support for participants with longer (+1 SD) pain durations (B = −0.41, SE 0.12, Beta = −0.61, t = −3.45, P < 0.001). There was a trend for mean pain duration in the same direction (B = −0.16, SE 0.07, Beta = −0.24, t = −2.43; P < 0.02). In contrast, for participants with shorter pain durations (−1 SD), catastrophizing and spousal support were not significantly related (B = 0.09; SE 0.11, Beta = 0.13, t = 0.78, P > 0.43).
Contrary to expectations, the interactions between pain duration and catastrophizing in relating to the other forms of support (i.e. perceptions of distracting and negative spouse responses, perceived general support) were not significant. Each of the interaction effects was small. The main effect of pain duration was not significant. Because the main effects of pain catastrophizing were similar in size to those of the correlations shown in Table 2, the regression results are not presented here.
The hierarchical regression analyses were repeated with duration of marriage as the moderator to rule out the possibility that years spent living with the spouse was the true moderator of catastrophizing. Similarly, the difference between pain duration and marriage duration was examined as a moderator. However, none of these analyses resulted in significant interactions. Therefore, absolute pain duration, not years married or pain duration relative to length of marriage, interacts with catastrophizing in relating to some support variables.
3.4. Hierarchical regressions: psychological distress
Hierarchical multiple regressions were also conducted to test the hypothesis that catastrophizing would interact with pain duration in correlating with psychological distress. Pain severity was included as a covariate because it was a significant correlate of psychological distress. The main effects of pain severity and pain catastrophizing were significantly related to distress whereas pain duration was not (see Table 4). Contrary to the hypothesis, the interaction between pain duration and catastrophizing was not significantly related to distress. Indeed the value of change in R2 indicated that the interaction effect was small. Hierarchical regressions with marriage duration and the difference between pain duration and marriage duration yielded similar results, with significant main effects for catastrophizing and pain severity only and no significant interactions between the duration variables and catastrophizing.
Table 4.
Summary of hierarchical regression for pain catastrophizing, pain duration, and their interaction in relating to psychological distress
| B | SE | Beta | |
|---|---|---|---|
| Step 1 | |||
| Pain severity | 0.92 | 0.31 | 0.26** |
| Pain duration | 0.002 | 0.01 | 0.02 |
| Pain catastrophizing | 0.46 | 0.08 | 0.49** |
| Step 2 | |||
| Pain duration X | −0.001 | 0.001 | 0.15 |
| Pain catastrophizing |
N = 96; R2 = 0.39; P < 0.001 for step 1; ΔR2 = 0.02, P > 0.12 for step 2.
P < 0.01.
3.5. Psychological distress as mediator
As noted in the statistical literature (Baron and Kenny, 1986; Holmbeck, 2002), one of the conditions of mediator analyses is that the independent variable (i e., the interaction between catastrophizing and pain duration) should be significantly related to the mediator (i.e. psychological distress). Therefore, the nonsignificant relationship between the interaction and distress precluded analyses testing the hypothesis of whether psychological distress mediated the relationship between the catastrophizing-pain duration interaction and perceived support. However, distress might still mediate the relationship between catastrophizing and support at the different levels of pain duration. Only perceived spousal support and perceptions of solicitous spouse responses were investigated in this manner because interaction effects were found for only these forms of support. The post-hoc regressions were conducted again, this time with distress entered at the first step. Results showed that distress did not mediate the effect of catastrophizing at long (+1 SD) or short (−1 SD) pain durations on perceived spousal support or perceptions of solicitous spouse responses.
The main effects regressions were also repeated to determine whether psychological distress mediated the relationship between the main effect of catastrophizing on perceived general support because catastrophizing was related to both distress and to this support variable. Pain duration and severity were dropped from the regression because (a) pain duration was not a significant correlate of perceived general support or psychological distress and (b) the inclusion of pain severity would not have allowed a straightforward test of the potential mediation of psychological distress. At step 1, there was a main effect for catastrophizing (B = −0.33; SE 0.11, Beta = −0.31, t = −3.16, P < 0.01), overall R2 = 0.10, F(1.94) = 10.01, P < 0.001. At step 2, the effect of psychological distress was large and significant (B = −0.59, SE 0.12, Beta = −0.52, t = −4.79, P < 0.0001), ΔR2 = 0.18, F(2,93) = 22.91, P < 0.0001, whereas the effect of catastrophizing was no longer significant, P > 0.89. While it appeared that distress mediated the relationship between pain catastrophizing and perceived general support, a Sobel test showed that this partial mediation was not significant, z = 1.52; P > 0.05.
4. Discussion
The aim of the current study was to examine the relationship between pain catastrophizing and support in a manner that incorporated pain duration as a moderator and distress as a mediator of this relationship. Correlations showed that catastrophizing was negatively related to perceptions of social support from others. In contrast, there were trends for catastrophizing to be related to more distracting and solicitous responses on the part of the spouse. At first glance, these correlational results suggest that the communal coping hypothesis (Sullivan et al., 2001a) might be limited to pain-specific support.
However, moderator analyses revealed a more complex relationship between pain catastrophizing and certain types of support. The findings provided mixed support for the hypothesis that pain catastrophizing would be positively related to perceived support at shorter pain durations but negatively related to perceived support at longer pain durations. Specifically, catastrophizing was significantly related to greater perceptions of pain-specific spousal support in ICPs with shorter pain durations. No significant relationship was found for ICPs with longer pain durations. In contrast, pain catastrophizing was significantly related to diminished perceptions of non-pain-specific spousal support in ICPs with longer pain durations whereas no such relationship was found for ICPs with shorter pain durations. The association between catastrophizing and pain-specific spousal support at shorter pain durations partially supports an extension of the communal coping hypothesis (Sullivan et al., 2001a).
The different spouse response and spousal support findings may be interpreted within a cognitive-behavioral-interpersonal framework. The communal coping hypothesis suggests that ICPs catastrophize to garner intimacy and closeness; however, ICPs in the early stages of pain may be sending the message that they want or need support from their spouses specifically aimed at the alleviation of pain. Over time, ICPs may habituate to pain-specific support, spouses may habituate to the ICPs’ catastrophizing, or both. Pain may demand increasing amounts of attention over time, in turn distracting ICPs from attending to spouse responses. At longer pain durations, catastrophizing may result in diminished perceptions of spousal support not specific to pain because ICPs did not obtain the more intimate relationship that they desired earlier in the illness. Adapting interactional approaches concerning depression (e.g. Coyne, 1976; Giesler and Swann, 1999) to the problem of pain, catastrophizing may also drive spouses away because they are irritated by the ICPs’ inability to direct their attention away from the pain or because they realize that their attempts at helping have not been successful. Thus, overall spousal support is less available. These hypothesized interaction patterns are tentative because this was a cross-sectional study and it is unclear whether spouses are truly providing the amount of support that ICPs perceive. Furthermore, it is unclear if catastrophizing influences actual support, changes ICPs’ perceptions over time, or both. Additional research may address these issues and whether ICPs prefer more closeness and intimacy as opposed to pain-specific support from their spouses.
Some hypothesized relationships between catastrophizing and perceived support were not supported. It was surprising that pain catastrophizing was not significantly related to perceived negative spouse responses since the depression literature theorizes that others often respond to a distressed person in negative ways (e.g. Coyne, 1976). Perhaps, negative pain-specific responses may occur in reaction to pain behaviors that may be the result of more private pain catastrophizing. In addition, pain duration did not interact with catastrophizing in relating to perceived general support or perceptions of negative and distracting spouse responses. The passage of time may simply not affect the relationships between pain catastrophizing and these other forms of support. Others who provide general support (e.g. friends, extended family) may have less close or frequent contact with the patient so that the accumulated time spent with the patient is not as great as for spouses. With regard to perceived distracting spouse responses, some ICPs may attribute distraction attempts to the spouses’ irritation with the patient or avoidance of the pain problem. Frequent negative interactions directly and indirectly related to the pain may create an interpersonal atmosphere in which the patient makes generalizations about the lack of overall support received from the spouse, especially over longer periods of time. Additional studies must address these hypotheses. Nevertheless, these results suggest that the moderation of pain duration on pain catastrophizing is limited to spousal support that is more clearly positive in nature.
The fact that neither marriage duration nor the difference between marriage and pain duration was a significant moderator of catastrophizing implies that the absolute pain duration may be an important element in the relationship between pain cognitions and interpersonal processes. For instance, duration of pain might influence ICPs’ interactional styles regardless of whether they have a partner when the pain began. ICPs who develop chronic pain prior to marriage may select partners who are particularly responsive to their pain. These same partners may tire of this type of caregiving interaction as the relationship matures. It is also possible that the onset of pain while dating a future spouse changes the nature of interpersonal interaction between partners. In the current study, it is not known if pain problems began before or after ICPs met their spouses and this is another possible moderator of catastrophizing to be explored in the future.
Catastrophizing was also related to psychological distress as found by previous researchers (e.g. Bishop and Warr, 2003; Grant et al., 2002; Keefe et al., 1989; Rosenstiel and Keefe, 1983; Turner et al., 2000). However, pain duration did not moderate this relationship. This was surprising because similar interpersonal processes were thought to be at work with catastrophizing and psychological distress as with catastrophizing and support. The strong relationship between catastrophizing and distress may have prevented significant moderation effects. In addition, duration of pain may not be as important as the duration of pain-related helplessness in the catastrophizing-distress association. It is likely that helplessness about the pain does not begin until several unsuccessful treatment attempts, which may occur several years after pain onset.
Integrating the depression and pain literatures, it was also hypothesized that pain catastrophizing would be related to less perceived support at longer pain durations because of elevated psychological distress. While the mediator analyses could not be conducted because the statistical prerequisites for investigating mediation were not met, other analyses showed that (a) distress did not mediate the effect of catastrophizing on support at different pain durations and (b) distress did not significantly mediate the main effect of catastrophizing on the support variables. Overall these results suggest that the effect of catastrophizing is independent of the effect of distress, providing further support for the notion that catastrophizing and distress are two related yet independent constructs (Sullivan et al., 2001b).
There were several limitations of this study. First, although typical of interaction results, the interaction effect sizes were small to medium. Further research will be needed to replicate these findings and determine whether the sizes of the effects vary depending on other study characteristics. Second, it is unclear whether these findings are generalizable to unmarried ICPs, patients attending pain clinics, and ICPs in the community who may not be willing or able to participate in research studies. An advantage of a community sample such as this one is that there was a wide range of pain durations so that analyses were not compromised by restricted range. Third, pain-specific support from persons other than the spouse were not assessed and ICPs were not directed on the general support measure to report only about support received from people other than their spouses. Therefore, more work is needed to determine the full extent to which catastrophizing and support from others are related. Fourth, change over time or causal directions cannot be concluded from the cross-sectional design of this study. Longitudinal studies can address questions regarding the relationships between changes in pain duration and amount of pain catastrophizing.
In sum, the current study provided some support for the communal coping hypothesis and demonstrates that moderating variables such as pain duration are important in explicating the relationship between pain-related cognitions and the interpersonal context. Other studies also suggest the importance of moderators and the communal coping hypothesis. For instance, Giardino et al. (2003) revealed a stronger relationship between catastrophizing and support in spinal cord injury patients who lived with a partner than those who did not. Additional studies on the moderators and mediators of pain catastrophizing may result in a more comprehensive model of pain catastrophizing. With regard to treatment, reductions in pain catastrophizing are related to subsequent improvements in depression (Burns et al., 2003; Jensen et al., 2001). Future treatment research may also indicate that consideration of pain duration and relationship functioning is beneficial. It is possible that reductions in catastrophizing might be related to improved relationship functioning. Targeting pain catastrophizing earlier rather than later in the illness may enhance interactions so that spouses are not focused solely on the pain problem.
Acknowledgements
This research was supported by grants R03 MH61569-01 and K01 MH MH066975-01. Annmarie Cano, Department of Psychology, Wayne State University. The author thanks Heather Foran, Jennifer Hanawalt, Ayna Johansen, and Michelle Roos for their help in conducting this study.
References
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Warr D. Coping, catastrophizing and chronic pain in breast cancer. J Behav Med. 2003;26:265–81. doi: 10.1023/a:1023464621554. [DOI] [PubMed] [Google Scholar]
- Burns JW, Kubilus A, Bruehl S, Harden RN, Lofland K. Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. J Consult Clin Psychol. 2003;71:81–91. doi: 10.1037//0022-006x.71.1.81. [DOI] [PubMed] [Google Scholar]
- Cano A, Weisberg J, Gallagher M. Marital satisfaction and pain severity mediate the association between negative spouse responses to pain and depressive symptoms in a chronic pain patient sample. Pain Med. 2000;1:35–43. doi: 10.1046/j.1526-4637.2000.99100.x. [DOI] [PubMed] [Google Scholar]
- Cano A, Gillis M, Heinz W, Geisser M, Foran H. Marital functioning, chronic pain, and psychological distress. Pain. 2004;107:99–106. doi: 10.1016/j.pain.2003.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Coyne JC. Depression and the response of others. J Abnorm Psychol. 1976;85:186–93. doi: 10.1037//0021-843x.85.2.186. [DOI] [PubMed] [Google Scholar]
- Crombez G, Eccleston C, Baeyens G, Eelen P. When somatic information threatens, catastrophic thinking enhances attentional interference. Pain. 1998;75:187–98. doi: 10.1016/s0304-3959(97)00219-4. [DOI] [PubMed] [Google Scholar]
- Cutrona CE. Ratings of social support by adolescents and adult informants: Degree of correspondence and predication of depressive symptoms. J Person Soc Psychol. 1989;57:723–30. doi: 10.1037//0022-3514.57.4.723. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW. The provision of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in personal relationships. Vol. 1. JAI Press; Greenwich, CT: 1987. pp. 37–67. [Google Scholar]
- Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125:356–66. doi: 10.1037/0033-2909.125.3.356. [DOI] [PubMed] [Google Scholar]
- Flor H, Kerns R, Turk DC. The role of spouse reinforcement, perceived pain, and activity levels of chronic pain patients. J Psychosom Res. 1987;31:251–9. doi: 10.1016/0022-3999(87)90082-1. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: a practical method for grading the state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Cano A, Foran H. Psychometric properties of the mood and anxiety symptom questionnaire in chronic pain patients. University of Michigan; Ann Arbor, MI: 2003. Unpublished manuscript. [DOI] [PubMed] [Google Scholar]
- Giardino ND, Jensen MP, Turner JA, Ehde D, Cardenas DD. Social environment moderates the association between catastrophizing and pain among persons with a spinal cord injury. Pain. 2003;106:19–25. doi: 10.1016/s0304-3959(03)00226-4. [DOI] [PubMed] [Google Scholar]
- Giesler RB, Swann WB. Striving for Confirmation: The Role of Self-Verification in Depression. In: Joiner T, Coyne JC, editors. The Interactional Nature of Depression. American Psychological Association; Washington, DC: pp. 189–217. [Google Scholar]
- Grant LD, Long BC, Willms JD. Women's adaptation to chronic back pain: Daily appraisals and coping strategies, personal characteristics and perceived spousal responses. J Health Psychol. 2002;7:545–64. doi: 10.1177/1359105302007005675. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM. Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J Consult Clin Psychol. 2001;69:655–62. doi: 10.1037//0022-006x.69.4.655. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Alfano MS, Metalsky GI. When depression breeds contempt: Reassurance seeking, self-esteem, and rejection of depressed college students by their roommates. J Abnorm Psychol. 1992;101:165–73. doi: 10.1037//0021-843x.101.1.165. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Brown GK, Wallston KA, Caldwell DS. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37:51–6. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- Keppel G. Design and analysis: a researcher's handbook. 2nd ed. Prentice-Hall, Inc; Englewood Cliffs, NJ: 1982. [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale multidimensional pain inventory. Pain. 1985;23:345–56. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Haythornthwaite J, Southwick S, Giller EL., Jr The role of marital interaction in chronic pain and depressive symptom severity. J Psychosom Res. 1990;34:401–8. doi: 10.1016/0022-3999(90)90063-a. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Jacob MC. Assessment of the psychosocial context of the experience of chronic pain. In: Turk DC, Melzack R, editors. Handbook of pain assessment. Guilford Press; New York: 1992. pp. 235–53. [Google Scholar]
- Romano JM, Turner JA, Jensen MP, Friedman LS, Bulcroft RA, Hops H, Wright SF. Chronic pain patient-spouse behavioral interactions predict patient disability. Pain. 1995;63:353–60. doi: 10.1016/0304-3959(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Bishop S, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:432–524. [Google Scholar]
- Sullivan MJL, Tripp DA, Santor D. Gender differences in pain and pain behavior: the role of catastrophizing. Cognit Ther Res. 2000;24:121–34. [Google Scholar]
- Sullivan MJL, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001a;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan MJL, Rodgers WM, Kirsch I. Catastrophizing, depression and expectancies for pain and emotional distress. Pain. 2001b;91:147–54. doi: 10.1016/s0304-3959(00)00430-9. [DOI] [PubMed] [Google Scholar]
- Thorn BE, Ward LC, Sullivan MJL, Boothby JL. Communal coping model of catastrophizing: conceptual model building. Pain. 2003;106:1–2. doi: 10.1016/s0304-3959(03)00228-8. [DOI] [PubMed] [Google Scholar]
- Turk DC, Kerns RD, Rosenberg R. Effects of marital interaction on chronic pain and disability: examining the down side of social support. Rehab Psychol. 1992;37:259–74. [Google Scholar]
- Turner JA, Jensen MP, Romano JM. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85:115–25. doi: 10.1016/s0304-3959(99)00259-6. [DOI] [PubMed] [Google Scholar]
- Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. Pain. 2002;96:319–24. doi: 10.1016/S0304-3959(01)00463-8. [DOI] [PubMed] [Google Scholar]
- Van Damme S, Crombez G, Eccleston C. Disengagement from pain: the role of catastrophic thinking about pain. Pain. 2004;107:70–6. doi: 10.1016/j.pain.2003.09.023. [DOI] [PubMed] [Google Scholar]
- Wade TD, Kendler KS. The relationship between social support and major depression: cross-sectional, longitudinal, and genetic perspectives. J Nerv Ment Dis. 2000;188:251–8. doi: 10.1097/00005053-200005000-00001. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Mood and Anxiety Symptom Questionnaire. University of Iowa, Department of Psychology; Iowa City, IA: 1991. Unpublished manuscript. [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. J Abnorm Psychol. 1995a;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptoms scales. J Abnorm Psychol. 1995b;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]