Abstract
Disturbances in mineral metabolism play a central role in the development of renal bone disease. In a 54-wk, randomized, open-label study, 119 hemodialysis patients were enrolled to compare the effects of sevelamer hydrochloride and calcium carbonate on bone. Biopsy-proven adynamic bone disease was the most frequent bone abnormality at baseline (59%). Serum phosphorus, calcium, and intact parathyroid hormone were well controlled in both groups, although calcium was consistently lower and intact parathyroid hormone higher among patients who were randomly assigned to sevelamer. Compared with baseline values, there were no changes in mineralization lag time or measures of bone turnover (e.g., activation frequency) after 1 yr in either group. Osteoid thickness significantly increased in both groups, but there was no significant difference between them. Bone formation rate per bone surface, however, significantly increased from baseline only in the sevelamer group (P = 0.019). In addition, of those with abnormal microarchitecture at baseline (i.e., trabecular separation), seven of 10 in the sevelamer group normalized after 1 yr compared with zero of three in the calcium group. In summary, sevelamer resulted in no statistically significant changes in bone turnover or mineralization compared with calcium carbonate, but bone formation increased and trabecular architecture improved with sevelamer. Further studies are required to assess whether these changes affect clinical outcomes, such as rates of fracture.
Patients with chronic kidney disease (CKD) typically have abnormal bone histology. Alterations in bone turnover, mineralization, and volume in renal patients depend on several factors. In particular, disturbances in calcium-phosphate, parathyroid hormone (PTH), and vitamin D metabolism are important in the development of renal osteodystrophy (ROD).
The pattern of ROD observed in patients with stage 5 CKD has changed in recent years. Previously, observed bone conditions in renal patients in order of prevalence were mixed uremic osteodystrophy (MUO), predominant hyperparathyroid bone disease (HPBD), and aluminum-related osteomalacia and adynamic bone disease (ABD); however, reduced use of aluminum has resulted in a decline in the occurrence of osteomalacia. Concurrently, there has been an increase in ABD without aluminum toxicity and less MUO.1–3 This has been attributed to greater use of calcium-based phosphate binders, which may result in oversuppression of PTH, especially when used with calcitriol or calcitriol analogues.4–6
Calcium-based binder use has also been linked with progression of vascular calcification.7 Evidence suggests that ABD may predispose patients to soft tissue and vascular calcification.8 The use of non–calcium-based phosphate binders, such as sevelamer hydrochloride, may reduce the oversuppression of PTH and so help prevent ABD and cardiovascular calcifications. Studies have shown that sevelamer attenuates progression of vascular calcification and prevents reduction in thoracic vertebral bone mineral density.7,9,10
Bone biopsy is the recognized gold standard for the diagnosis and evaluation of renal bone disease.11–13 Previous reports assessing changes in vertebral bone with phosphate binders by electron-beam tomography (EBT) did not assess changes in bone histology.9,10 Thus, a study using bone biopsies was conducted to compare the effects of sevelamer hydrochloride and calcium carbonate on bone histology.
RESULTS
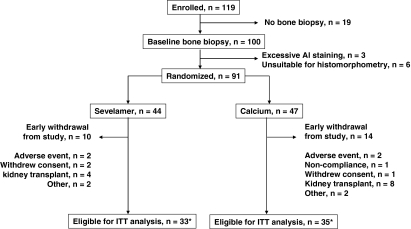
Disposition of patients is shown in Figure 1. A total of 119 patients were enrolled, 100 of whom had a baseline bone biopsy. Ninety-one of these were randomly assigned to receive sevelamer (n = 44) or calcium-based binders (n = 47), and 68 had a second bone biopsy after 1 yr (sevelamer n = 33; calcium n = 35).
Figure 1.
Disposition of patients. The intention-to-treat (ITT) population was defined as all patients who were randomly assigned, received one or more doses of study medication, and had a second bone biopsy. One patient in the sevelamer group completed treatment but did not have a second bone biopsy and so was excluded from the ITT analysis. Two patients in the calcium group withdrew from the study early but received one or more doses of study medication and had a second bone biopsy and so were included in the ITT analysis.
Baseline demographics and clinical characteristics were comparable between groups (Table 1). Almost all patients (98%) received calcium carbonate in the 30 d before screening, with 93% treated with calcium-based binders as monotherapy.
Table 1.
Baseline characteristicsa
| Characteristic | Sevelamer (n = 33) | Calcium (n = 35) | P |
|---|---|---|---|
| Gender (M/F; n [%]) | 22/11 (67/33) | 18/17 (51/49) | 0.23 |
| Race | >0.99 | ||
| white | 32 (97) | 34 (97) | |
| black | 1 (3) | 1 (3) | |
| Age (yr; mean ± SD) | 55.5 ± 15.4 | 53.9 ± 13.7 | 0.53 |
| Menopausal status (n [%]) | 0.0097 | ||
| premenopausal | 0 (0) | 8 (47) | |
| postmenopausal | 11 (100) | 9 (53) | |
| BMI (kg/m2; mean ± SD) | 23.5 ± 3.5 | 25.3 ± 3.8 | 0.09 |
| Smoker (n [%]) | 8 (24) | 3 (9) | 0.10 |
| Diabetes (n [%]) | 2 (6) | 8 (23) | 0.08 |
| Hypertension (n [%]) | 24 (73) | 25 (71) | >0.99 |
| Primary cause of stage 5 CKD (n [%]) | 0.18 | ||
| hypertension | 2 (6.1) | 6 (17.1) | |
| glomerulonephritis | 8 (24.2) | 7 (20.0) | |
| diabetes | 2 (6.1) | 7 (20.0) | |
| pyelonephritis | 3 (9.1) | 3 (8.6) | |
| polycystic kidneys | 3 (9.1) | 2 (5.7) | |
| interstitial nephrosis | 4 (12.1) | 0 (0) | |
| other | 11 (33.3) | 10 (28.6) | |
| Dialysis vintage (mo; median [range]) | 23 (4 to 222) | 25 (2 to 181) | 0.49 |
| Phosphate binder use (in 30 d before screening; n [%]) | 33 (100) | 35 (100) | 0.07 |
| calcium carbonate | 31 (94) | 32 (91) | |
| sevelamer | 1 (3) | 1 (3) | |
| calcium carbonate + sevelamer | 1 (3) | 0 (0) | |
| calcium carbonate + aluminum | 0 (0) | 2 (6) | |
| Vitamin D use (in 12 mo before screening; n [%]) | 22 (67) | 24 (69) | 1.0 |
BMI, body mass index.
Dosages of study medication increased in both groups during the study. Mean daily sevelamer dosage increased from 3.3 ± 2.0 to 5.0 ± 2.7 g after 1 yr, and calcium increased from 3.8 ± 2.2 to 4.0 ± 2.5 g. Compliance assessed by pill count was comparable between the treatment groups (sevelamer 92%; calcium 95%). No patient received aluminum rescue therapy for treatment-resistant hyperphosphatemia during the study. None of the patients received parent vitamin D or ergo- or cholecalciferol. At baseline, 14 (42%) patients in the sevelamer group and 16 (46%) in the calcium group received active vitamin D metabolites or analogs. All of these patients, with the exception of one patient in the sevelamer group who received α-calcidiol for the duration of the study and one patient in the calcium group who received paricalcitol for a 2-wk period, were given calcitriol. The median weekly change in calcitriol or analogue dosage significantly increased from baseline to end of study in the sevelamer group compared with the calcium group (2.0 versus 0.0 μg intravenously, calcitriol or calcitriol equivalents; P = 0.027). An increase in vitamin dosage was possible in 19 (58%) patients who were treated with sevelamer compared with 11 (31%) patients who were treated with calcium. In general, both treatments were well tolerated with adverse event profiles consistent with patients’ underlying renal disease.
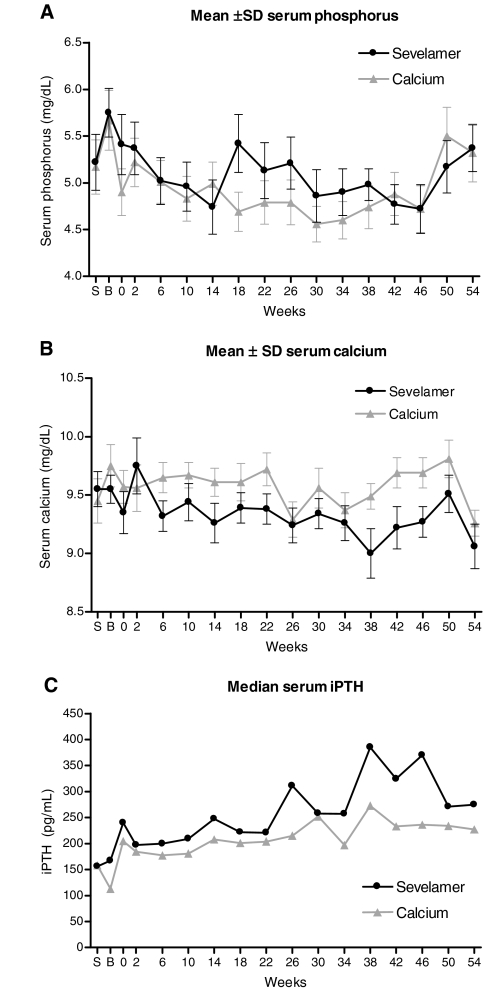
Biochemical Parameters
Biochemical parameters are summarized in Table 2. Serum phosphorus levels were well controlled with both treatments with no significant changes within or between groups (Figure 2A). Serum calcium and intact PTH (iPTH) were also well controlled, and mean values remained within the recommended Kidney Disease Outcomes Quality Initiative (K/DOQI) ranges in both groups (Figure 2, B and C); however, serum calcium was consistently lower whereas serum iPTH was consistently higher with sevelamer. Serum 25-OH D and 1,25-OH2 D levels were low at baseline in both groups, and small but comparable median increases from baseline were observed with both sevelamer and calcium (2.2 versus 1.9 ng/ml [P = 0.53] and 1.7 versus 0.2 ng/ml [P = 0.27], respectively). Total and LDL cholesterol significantly decreased within the sevelamer but not the calcium group, and the difference between treatments was significant (total cholesterol P = 0.03; LDL cholesterol P < 0.01). HDL cholesterol increased in both groups similarly, without difference between groups. Serum bicarbonate levels were similar in both groups at all time points.
Table 2.
Changes in serum biochemical parameters
| Parameter | Sevelamer (n = 33)
|
Calcium (n = 35)
|
Pa | ||
|---|---|---|---|---|---|
| Baseline | 1 Yr | Baseline | 1 Yr | ||
| Phosphorus (mg/dl; mean ± SD) | 5.8 ± 1.5 | 5.4 ± 0.1.4 | 5.7 ± 1.8 | 5.3 ± 1.9 | 0.78 |
| Calcium (mg/dl; mean ± SD) | 9.6 ± 0.7 | 9.1 ± 1.1 | 9.8 ± 1.0 | 9.3 ± 0.7b | 0.22 |
| iPTH (pg/ml; median [range]) | 167 (3 to 1958) | 275 (34 to 3890) | 113 (4 to 1369) | 227 (28 to 3636)b | 0.55 |
| 25-OH D (ng/ml; median [range]) | 16.3 (5.0 to 34.6) | 20.0 (5.4 to 53.2)b | 16.6 (5.0 to 35.3) | 17.4 (5.0 to 49.1) | 0.53 |
| 1,25-OH2 D (pg/ml; median [range]) | 6.4 (5.0 to 22.4) | 8.1 (4.5 to 83.5) | 11.8 (5.0 to 42.9) | 13.7 (4.5 to 61.5) | 0.27 |
| Total cholesterol (g/L; mean ± SD) | 1.65 ± 0.38 | 1.40 ± 0.34b | 1.72 ± 0.41 | 1.66 ± 0.41 | 0.03 |
| LDL cholesterol (g/L; mean ± SD) | 1.03 ± 0.34 | 0.68 ± 0.30b | 1.07 ± 0.37 | 1.00 ± 0.31 | <0.01 |
| HDL cholesterol (g/L; mean ± SD) | 0.50 ± 0.12 | 0.55 ± 0.14b | 0.43 ± 0.12 | 0.49 ± 0.15b | 0.87 |
| Bicarbonate (mmol/L; mean ± SD) | 19.3 ± 3.9 | 20.4 ± 3.3 | 19.7 ± 3.8 | 21.2 ± 4.1 | 0.34 |
| BSAP (μg/L; median [range]) | 11.5 (3.9 to 65.2) | 19.1 (3.9 to 174.0)b | 10.6 (3.4 to 80.1) | 12.7 (4.5 to 185.0) | 0.19 |
| Osteocalcin (ng/ml; median [range]) | 68.5 (2.9 to 896) | 84.2 (15.2 to 595) | 45.8 (2.4 to 308) | 123 (7.6 to 1122)b | 0.54 |
| N-telopeptides (nM; median [range]) | 135 (7 to 1200) | 298 (11 to 1200)b | 72 (8 to 1200) | 132 (10 to 1200)b | 0.87 |
Between-group difference in change from baseline assessed using Wilcoxon rank sum test.
P< 0.05 for within-group change from baseline assessed using Wilcoxon signed rank test. Initial lipid levels measured at screening, not baseline.
Figure 2.
Serum phosphorus (A), serum calcium (B), and serum iPTH (C) during 1 yr of treatment with sevelamer or calcium.
Serum bone-specific alkaline phosphatase (BSAP) significantly increased from baseline at 6 mo (P = 0.001) and at 1 yr (P = 0.02) with sevelamer but not calcium, but there were no differences between groups at either time point. Osteocalcin increased significantly from baseline in the calcium group, but there was no significant difference between treatments. Serum N-telopeptide increased significantly from baseline in both groups but without significant between-group differences.
Bone Turnover and Mineralization
Changes in parameters of bone mineralization and turnover are summarized in Table 3. Mineralization lag time was comparable between groups at baseline and 1 yr with no significant changes within or between groups. Osteoid thickness significantly increased in both groups with no significant between-group differences in change from baseline.
Table 3.
Changes in bone mineralization, bone turnover, and trabecular architecturea
| Parameter | Sevelamer (n = 33)
|
Calcium (n = 35)
|
Pb | ||
|---|---|---|---|---|---|
| Baseline | 1 Yr | Baseline | 1 Yr | ||
| Bone mineralization | |||||
| mineralization lag time in lamellar bone (d) | 28.2 (9.4 to 175.9) | 36.1 (0 to 153.7) | 26.1 (0.4 to 155.0) | 40.8 (2.4 to 493.8) | 0.54 |
| osteoid thickness (μm) | 9.3 (3.8 to 37.7) | 10.5 (4.8 to 16.5)c | 9.6 (4.1 to 24.0) | 10.7 (5.7 to 27.8)d | 0.71 |
| Bone turnover | |||||
| Acf (/yr) | 0.36 (0.04 to 1.84) | 0.43 (0.02 to 2.41) | 0.39 (0 to 1.54) | 0.45 (0 to 1.97) | 0.76 |
| bone formation rate/bone surface (mm3/cm2 per yr) | 1.6 (0.1 to 8.8) | 2.3 (0.2 to 13.9)e | 2.1 (0 to 8.5) | 2.5 (0.4 to 14.0) | 0.82 |
| no. of osteoblasts/bone perimeter (/100 mm) | 136.0 (0 to 882.5) | 148.2 (2.8 to 1690.6) | 87.2 (3.1 to 1109.7) | 180.8 (6.4 to 1268.1) | 0.99 |
| no. of osteoclasts/bone perimeter (/100 mm) | 31.6 (0.1 to 499.7) | 39.6 (1.2 to 172.9) | 21.4 (3.1 to 183.0) | 34.4 (0 to 223.6) | 0.72 |
| Trabecular architecture | |||||
| cancellous bone volume/tissue volume (%) | 18.4 (0.2 to 66.9) | 19.8 (10.9 to 38.9) | 21.7 (11.2 to 35.0) | 24.0 (11.5 to 59.1) | 0.10 |
| trabecular thickness (μm) | 105.7 (1.7 to 144.6) | 106.7 (70.5 to 191.9) | 119.1 (62.6 to 171.7) | 114.7 (0.6 to 188.2) | 0.96 |
| trabecular separation (μm) | 486.2 (11.8 to 773.5) | 466.5 (229.6 to 841.6) | 418.4 (247.7 to 963.9) | 385.0 (3.3 to 671.4) | 0.46 |
Data are median (range).
Between-group difference in change from baseline.
P = 0.030 versus baseline.
P = 0.026 versusbaseline.
P = 0.019 versusbaseline.
There were no significant changes within or between groups in activation frequency (Acf), number of osteoblasts/bone perimeter, or number of osteoclasts/bone perimeter. Bone formation rate/bone surface significantly increased from baseline in the sevelamer group (P = 0.019) but not in the calcium group. At baseline, three patients were excluded from the study because of stainable aluminum at >20% of the trabecular surface, and there were no patients with stainable bone aluminum at end of the study.
Trabecular Architecture
Cancellous bone volume was significantly higher in the calcium group than in the sevelamer group at baseline (P = 0.033) and 1 yr (P = 0.029), but there were no significant changes from baseline within (sevelamer P = 0.09; calcium P = 0.11) or between groups. Trabecular thickness was significantly higher in the calcium group (P = 0.02) at baseline, although below normal in both groups. There was no difference in change from baseline between groups after 1 yr. Trabecular separation, a parameter indicating connection between trabeculae that is microarchitecture of cancellous bone, was comparable between groups at baseline and 1 yr with no significant differences in change from baseline within or between groups. The majority of patients had normal trabecular separation at baseline (sevelamer 67%; calcium 74%). In patients with abnormally high (>550 μm) baseline trabecular separation, seven of 10 patients in the sevelamer group had normal trabecular separation after 1 yr, whereas separation remained >550 μm in all three calcium patients (P = 0.07).
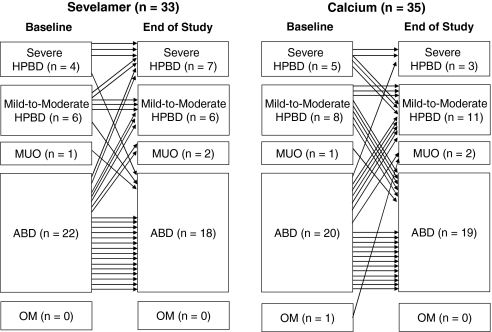
Shifts between Groups of Renal Bone Disease
At baseline, ABD was the most frequent condition in both the sevelamer (n = 22; 67%) and calcium (n = 20; 57%) groups. Severe predominant HPBD was diagnosed in four (12%) patients in the sevelamer group and five (14%) in the calcium group. Mild to moderate HPBD was found in six (18%) patients in the sevelamer group and eight (23%) patients in the calcium group. One patient in each group had MUO. Only a single patient, in the calcium group, had osteomalacia.
At the end of the study, three (9%) patients in the sevelamer group fell to the ABD category (from severe HPBD [n = 1], from mild to moderate HPBD [n = 1], and from MUO [n = 1]). In contrast, in the calcium group, nine (26%) patients fell to a lower bone turnover category (from severe HPBD to mild to moderate HPBD [n = 3], from mild to moderate HPBD to ABD [n = 5], and from MUO to ABD [n = 1]; Figure 3). The majority of patients still had ABD, and no patient developed osteomalacia.
Figure 3.
Changes in types of bone disease (based on qualitative evaluation of bone). OM, osteomalacia.
DISCUSSION
A high prevalence of ABD was observed in this study, with almost 60% of patients having an Acf <0.49/yr at baseline. This is consistent with reports of increasing prevalence of ABD in the past two decades,1–3 an increase that has coincided with the widespread use of calcium-based binders combined with more aggressive use of vitamin D analogs.4,5 Excluding patients with serum phosphorus values >8.1 mg/dl could not have had a major influence on these results because only two patients were excluded because of such severe hyperphosphatemia.
Importantly, the high prevalence of ABD was observed despite most patients’ being treated in accordance with K/DOQI guidelines and having serum mineral parameters within recommended ranges.11 Almost all (98%) patients were on calcium carbonate before the study, 65% had received calcitriol, and average dialysis vintage was >3.5 yr. This may explain why median serum iPTH levels were relatively low (150 to 300 pg/ml) at baseline. The frequent observation of ABD with median PTH values of 150 to 400 pg/ml in this study reaffirms the value of bone biopsies during dialysis in patients with intermediate PTH values.14
Although there were no differences between groups, bone formation rate significantly increased from baseline in the sevelamer group but not the calcium group. Moreover, seven of 10 sevelamer patients with abnormally high baseline trabecular separation moved into normal range compared with none of the calcium-treated patients (P = 0.07). BSAP, an index of bone formation, increased from baseline in the sevelamer group, whereas N-telopeptide, a parameter of bone resorption, increased in both treatment groups. This indicates that the osteocalcin increase seen in the calcium group is mainly reflective of increased bone resorption with the accompanied release of osteocalcin from bone. Effects of sevelamer and calcium on bone mineralization were comparable.
Although some changes in histomorphometric parameters were suggestive of increased bone turnover with sevelamer, most (53%) patients still had ABD after 1 yr of treatment with no differences between groups with regard to change in bone disease classification. This is consistent with the intransigent nature of ABD, which, once established, means that any improvements in bone histology occur very slowly; however, changes in biochemical parameters may forecast improvements in bone histology. Interpretation of biochemical markers of bone is limited when the markers are renally excreted. This applies to osteocalcin and N-telopeptides, whereas BSAP is not retained in CKD.
Previous studies have suggested that sevelamer may have a positive effect on bone mass and turnover compared with calcium. In a 1-yr randomized trial of 111 hemodialysis patients, calcium treatment resulted in a significant reduction in thoracic vertebral bone mineral density as measured by EBT compared with sevelamer.9 Calcium was also associated with lower levels of PTH, BSAP, and osteocalcin. Although bone biopsies were not performed, these results suggest that calcium-treated patients may have been more likely to develop adynamic bone than sevelamer-treated patients. Similar findings after 2 yr were reported by Asmus et al.10 Moreover, a study of 28 hemodialysis patients with ABD reported that switching treatment from calcium to sevelamer resulted in biochemical changes, suggesting improved bone turnover in 18% of patients after 6 mo and 32% of patients after 1 yr.15
It has been reported that low bone turnover predisposes to the development of extraosseous calcifications.8 Vascular calcification is common in CKD and is a predictor of all-cause and cardiovascular mortality.16–18 Similarly, reduced bone mass has been shown to predict mortality risk in long-term hemodialysis patients.19 Using EBT, an inverse relationship between bone density and extent of vascular calcification has been observed in patients on hemodialysis.9,20
25-OH D and 1,25-OH2 D were low at baseline and end of the study in both treatment groups. The use of calcitriol or vitamin D analogs was higher in the sevelamer group than in the calcium group, with a significantly greater increase in change in median weekly dosage and more patients with an increase in dosage. 25-OH D blood levels did not fall in either group, indicating that there was no binding of 25-OH D by sevelamer. Although well controlled in both groups, mean serum calcium was consistently lower with sevelamer, which may explain the greater use of vitamin D analogs in this group. Increased vitamin D use together with higher PTH levels could explain the increased bone formation rates seen with sevelamer. Retrospective studies have suggested that use of calcitriol or paricalcitriol may be associated with reduced cardiovascular mortality and a survival advantage in patients who are on dialysis.21,22 The potential for increased use of calcitriol or vitamin D analogs in patients who are treated with sevelamer may thus be associated with important clinical benefits.
In summary, this study shows that phosphate control with sevelamer resulted in no statistically significant changes in bone turnover or bone mineralization compared with calcium-based binders; however, bone formation was significantly increased with sevelamer, which was associated with improved trabecular architecture. Further studies are required to assess whether increased bone formation results in higher bone volume and reduced fracture rates.
CONCISE METHODS
This was a 54-wk, randomized, open-label study to compare the effects of sevelamer hydrochloride and calcium carbonate on bone turnover, mineralization, and volume. Adult patients (≥18 yr) who were on hemodialysis 3 times/wk (≥3 mo) and stable serum phosphorus ≤8.1 mg/dl (≤2.6 mmol/L) for ≥1 mo before screening and were receiving treatment with a phosphate binder were enrolled at 16 centers in Portugal. Patients were required to have stable serum phosphorus ≤8.1 mg/dl (≤2.6 mmol/L) because higher levels were considered indicative of noncompliance with phosphate binder therapy. Other exclusion criteria included use of aluminum-based binders in the previous year (≥3 consecutive months), treatment with medications that are known to affect bone metabolism (e.g., corticosteroids, antiseizure or thyroid agents, bisphosphonate, calcitonin), tetracycline allergy, alcohol or drug abuse, and any significant concurrent clinical condition. The use of aluminum- or magnesium-based antacids was not permitted during the study, with the exception of aluminum rescue therapy (maximum 4 wk) for treatment-resistant hyperphosphatemia. The use of calcium other than prescribed as study drug was not permitted. Written informed consent was obtained from all patients, and the study was conducted in accordance with the Declaration of Helsinki and approved by independent ethics committees at each of the participating centers.
Study Design
At screening, patients underwent physical examination and review of medical history and previous medication. Within 3 wk of screening, eligible patients had baseline transiliac bone biopsies taken from the right or left anterior iliac crest in an alternating manner after double tetracycline labeling of bone. Patients who had <20% stainable aluminum (aurin tricarboxylic acid stain) at the trabecular surface and whose biopsy was suitable for histomorphometry were stratified according to qualitatively assessed bone turnover (high versus low/normal) and randomly assigned to treatment with either sevelamer or calcium in a 1:1 manner. Randomization was performed centrally by an independent study coordinator, with a maximum period of 6 wk allowed between bone biopsy and start of treatment.
During the 54-wk treatment phase, patients received sevelamer hydrochloride (Renagel 800-mg tablets; Genzyme, Cambridge, MA) or calcium carbonate (Salusif 500- or 1000-mg tablets; Lab de Produtos Químicos e Farmacêuticos Lda, Lisbon, Portugal) three times a day with meals. Number of tablets per meal could be adjusted to reflect phosphorus content of the meal, as long as the daily dosage was maintained. Starting dosage was individualized by substituting the phosphate binder used by the patient at screening with sevelamer or calcium on a gram-per-gram basis. Two weeks after randomization and every 4 wk thereafter, serum phosphorus, calcium, and iPTH were assessed together with adverse events and any changes in concomitant medication. When required, the dosage of phosphate binder was titrated to achieve a serum phosphorus of 3.2 to 5.0 mg/dl (1.00 to 1.60 mmol/L). Serum calcium (adjusted for albumin) was maintained at <10.4 mg/dl (<2.60 mmol/L) by adjustment of calcitriol or calcitriol analogue and/or calcium dosage if necessary. Calcitriol and calcitriol analogue treatment could also be titrated to maintain levels of serum iPTH at 150 to 300 pg/ml. The choice of vitamin D compound to be used was not specified and was at the discretion of the individual physician. No parent vitamin D or calcidiol was given. At the end of treatment, a second bone biopsy, from the iliac crest of the opposite site, was performed.
As in previous studies of sevelamer, neither clinical investigators nor patients were blinded to treatment because it would have been possible to identify by the lower incidence of hypercalcemia and decrease in serum LDL cholesterol associated with sevelamer. Differences in taste, smell, and appearance of tablets may also have resulted in identification of treatment modality. Compliance was assessed by pill counts.
Bone Biopsies, Mineralized Bone Histology, and Bone Morphometry
Bone biopsies were taken at baseline and end of study. For double labeling of bone, patients received oral tetracycline hydrochloride 500 mg twice daily for 2 d followed by a 10-d tetracycline-free interval and another course of tetracycline hydrochloride at the same dosage for 4 d. Transiliac bone biopsies were performed after an additional 4 d with bone samples (0.5 cm diameter × 1 to 2 cm length) being taken from the anterior iliac crest. All bone biopsies were performed at designated study centers in Lisbon (A.F.) and Porto (J.M.F.).
Iliac crest bone samples were fixed with ethanol at room temperature, dehydrated, and embedded in methylmethacrylate as described previously.13 Serial sections of 3- and 7-μm thickness were cut with a Microm microtome equipped with a carbide-edged knife (HM360; Microm, Walldorf, Germany). Sections were stained with the modified Masson-Goldner trichrome stain,23 the aurin tricarboxylic acid stain,24 and solochrome azurine,25 used to demonstrate the extent of aluminum deposits at the bone-osteoid interface. Unstained sections were prepared for phase-contrast and fluorescence light microscopy. Qualitative assessment of bone was performed at the study start to stratify patients by bone turnover status before randomization and at the study end to categorize patients by renal bone disease type. In addition, at the end of the study, histomorphometry for static and dynamic parameters of bone structure, formation, and resorption using the Osteoplan II system (C. Zeiss, New York, NY) was done at a magnification of ×200. All bone samples were processed and analyzed at the Bone Diagnostic and Research Laboratory, University of Kentucky Medical Center (Lexington, KY), without knowledge of the treatment arm. All parameters were in compliance with the recommendations of the nomenclature committee of the American Society of Bone and Mineral Research.26
The primary efficacy end points were (1) changes from baseline in mineralization lag time in lamellar bone and osteoid thickness and (2) changes in bone turnover as measured by Acf, number of osteoblasts/bone perimeter, number of osteoclasts/bone perimeter, and bone formation rate/bone surface. Secondary end points were the percentages of patients who developed (1) osteomalacia (mineralization lag time >100 d and osteoid thickness >20 μm),13 (2) predominant HPBD (Acf >0.72/yr, presence of woven osteoid and fibrosis, osteoblasts >200/100 mm, and osteoclasts >53/100 mm), and (3) ABD (Acf <0.49/yr and osteoid thickness <20 μm). Changes from baseline in trabecular microarchitecture (cancellous bone volume, trabecular thickness, and trabecular separation) were also assessed.
Blood samples were taken before dialysis (at screening, 6 mo, and 1 yr) and assessed at a central laboratory (Laboratorio de Análisis, Dr. Echevarne, Barcelona, Spain). Serum phosphorus, calcium (adjusted for albumin), iPTH (Immulite 2500 Intact PTH; Diagnostics Products Corp., Madrid, Spain), and bicarbonate were measured at screening, baseline, randomization, 2 wk after randomization, and then every 4 wk until the end of the study. Vitamin D (25-OH D and 1,25-OH2 D; RIA, Sorin Biomedica, Barcelona, Spain), BSAP (RIA, IZASA, Madrid, Spain), osteocalcin (RIA, IZASA), and N-telopeptide (type 1 collagen; ELISA; Ortho-Clinical Diagnostics, Buckinghamshire, UK) were measured at baseline, 6 mo, and 1 yr.
Statistical Analyses
Acf was chosen for determination of sample size because it has the largest variance among the studied histomorphometric parameters. On this basis, it was estimated that a sample size of 32 patients would provide 97% power to detect a significant difference (P < 0.01) between treatments, based on the assumption that 0.16/yr (within-group SD ±0.08) is the smallest difference that would be considered clinically meaningful; however, because a high dropout rate was expected, a target enrollment of 100 patients was selected.
Baseline characteristics were compared between groups using the Wilcoxon rank sum test for continuous variables and Fisher exact test for categorical variables. When any baseline characteristics were significantly different between groups, an adjusted treatment difference in the change from baseline to end of study was provided based on multiple linear regression models. Changes from baseline to end of study were assessed using Wilcoxon signed rank tests and compared between groups using the Wilcoxon rank sum test for continuous variables and Fisher exact test for categorical variables. All probability tests were two-sided and tested at the α = 0.05 level of significance. The primary population for the analysis was the intent-to-treat population, which included all patients who were randomly assigned, received one or more doses of study medication, and had a second bone biopsy.
DISCLOSURES
A.F. is a member of a speaker bureau for Genzyme Corp. and an advisor for Abbott; J.M.F. is a consultant for Genzyme Portugal and Amgen Portugal; R.M.H. and A.D. are employees of Genzyme Corp.
Acknowledgments
This study was supported by Genzyme Corp.
Data from this study were presented at the XLIII Congress of the European Renal Association–European Dialysis and Transplant Association; July 15 through 18, 2006; Glasgow, UK.
Other members of the Sevelamer Study Group were Patricia Martins, Centro Renal da Prelada, Porto; Antonio Morais Sarmento, CMDR-Centro Médico Doenças Renais, Porto; Jorge Dickson, Sociedade Portuguesa de Diálise Amadora, Amadora; Berta De Carvalho, UniNefro, Sto. Tirso; Odete Pereira, Nefronorte-Centro Renal do Norte em Paredes’ Paredes; Ana Ventura, NefroNorte-Centro Renal da Régua-Peso da Régua, Peso da Régua; and Vasco Miranda, Dinefro, Maia.
We thank Guodong Wang, Richard M. Wheaton, and Juliana Van Willigen for excellent technical support.
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1.Monier-Faugere MC, Malluche HH: Trends in renal osteodystrophy: A survey from 1983 to 1995 in a total of 2248 patients. Nephrol Dial Transplant 11[Suppl 3]: 111–120, 1996 [DOI] [PubMed] [Google Scholar]
- 2.Couttenye MM, D'Haese PC, Deng JT, Van Hoof VO, Verpooten GA, De Broe ME: High prevalence of adynamic bone disease diagnosed by biochemical markers in a wide sample of the European CAPD population. Nephrol Dial Transplant 12: 2144–2150, 1997 [DOI] [PubMed] [Google Scholar]
- 3.Malluche HH, Mawad H, Monier-Faugere MC: The importance of bone health in end-stage renal disease: Out of the frying pan, into the fire? Nephrol Dial Transplant 19[Suppl 1]: i9–i13, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Malluche HH, Monier-Faugere MC: Risk of adynamic bone disease in dialyzed patients. Kidney Int Suppl 38: S62–S67, 1992 [PubMed] [Google Scholar]
- 5.Pei Y, Hercz G, Greenwood C, Segre G, Manuel A, Saiphoo C, Fenton S, Sherrard D: Risk factors for renal osteodystrophy: A multivariant analysis. J Bone Miner Res 10: 149–156, 1995 [DOI] [PubMed] [Google Scholar]
- 6.Cannata Andia JB: Adynamic bone and chronic renal failure: An overview. Am J Med Sci 320: 81–84, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Chertow GM, Burke SK, Raggi P, Treat to Goal Working Group: Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int 62: 245–252, 2002 [DOI] [PubMed] [Google Scholar]
- 8.London GM, Marty C, Marchais SJ, Guerin AP, Metivier F, de Vernejoul MC: Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15: 1943–1951, 2004 [DOI] [PubMed] [Google Scholar]
- 9.Raggi P, James G, Burke SK, Bommer J, Chasan-Taber S, Holzer H, Braun J, Chertow GM: Decrease in thoracic vertebral bone attenuation with calcium-based phosphate binders in hemodialysis. J Bone Miner Res 20: 764–772, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Asmus HG, Braun J, Krause R, Brunkhorst R, Holzer H, Schulz W, Neumayer HH, Raggi P, Bommer J: Two year comparison of sevelamer and calcium carbonate effects on cardiovascular calcification and bone density. Nephrol Dial Transplant 20: 1653–1661, 2005 [DOI] [PubMed] [Google Scholar]
- 11.National Kidney Foundation: K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis 42[Suppl 3]: S1–S201, 2003 [PubMed] [Google Scholar]
- 12.Martin KJ, Olgaard K, Coburn JW, Coen GM, Fukagawa M, Langman C, Malluche HH, McCarthy JT, Massry SG, Mehls O, Salusky IB, Silver JM, Smogorzewski MT, Slatopolsky EM, McCann L, Bone Turnover Work Group: Diagnosis, assessment, and treatment of bone turnover abnormalities in renal osteodystrophy. Am J Kidney Dis 43: 558–565, 2004 [DOI] [PubMed] [Google Scholar]
- 13.Malluche HH, Faugere MC: Atlas of Mineralized Bone Histology, New York, Karger, 1986
- 14.Qi Q, Monier-Faugere MC, Geng Z, Malluche HH: Predictive value of serum parathyroid hormone levels for bone turnover in patients on chronic maintenance dialysis. Am J Kidney Dis 26: 622–631, 1995 [DOI] [PubMed] [Google Scholar]
- 15.Hyodo T, Wakai H, Takemura T, Taira T, Hidai H, Tsuchida M, Fujita T, Yoshida K, Baba S, Sakai T: Treatment of adynamic bone disease with the complete replacement from calcium carbonate to sevelamer hydrochloride [in Japanese]. Clin Calcium 15[Suppl 1]: 15–22, 2005 [PubMed] [Google Scholar]
- 16.Blacher J, Guerin AP, Pannier B, Marchais SJ, London GM: Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension 38: 938–942, 2001 [DOI] [PubMed] [Google Scholar]
- 17.London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H: Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant 18: 1731–1740, 2003 [DOI] [PubMed] [Google Scholar]
- 18.Adragao T, Pires A, Lucas C, Birne R, Magalhaes L, Goncalves M, Negrao AP: A simple vascular calcification score predicts cardiovascular risk in haemodialysis patients. Nephrol Dial Transplant 19: 1480–1488, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Taal MW, Roe S, Masud T, Green D, Porter C, Cassidy MJ: Total hip bone mass predicts survival in chronic hemodialysis patients. Kidney Int 63: 1116–1120, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Braun J, Oldendorf M, Moshage W, Heidler R, Zeitler E, Luft FC: Electron beam computed tomography in the evaluation of cardiac calcification in chronic dialysis patients. Am J Kidney Dis 27: 394–401, 1996 [DOI] [PubMed] [Google Scholar]
- 21.Shoji T, Nishizawa Y: Vitamin D and survival of hemodialysis patients [in Japanese]. Clin Calcium 14: 64–68, 2004 [PubMed] [Google Scholar]
- 22.Teng M, Wolf M, Ofsthun MN, Lazarus JM, Hernan MA, Camargo CA Jr, Thadhani R: Activated injectable vitamin D and hemodialysis survival: A historical cohort study. J Am Soc Nephrol 16: 1115–1125, 2005 [DOI] [PubMed] [Google Scholar]
- 23.Goldner J: A modification of the Masson trichrome technique for routine laboratory purposes. Am J Pathol 14: 237–243, 1938 [PMC free article] [PubMed] [Google Scholar]
- 24.Lillie PD, Fullmer HM: Histopathologic Technique and Practical Histochemistry, 4th Ed., New York, McGraw Hill, 1976
- 25.Denton J, Freemont AJ, Ball J: Detection of distribution of aluminium in bone. J Clin Pathol 37: 136–142, 1984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parfitt AM, Drezner MK, Glorieux FH, Kanis JA, Malluche HH, Meunier PJ, Ott SM, Recker RR: Bone histomorphometry: Standardization of nomenclature, symbols, and units. J Bone Miner Res 2: 595–610, 1987 [DOI] [PubMed] [Google Scholar]