Abstract
Carpal tunnel syndrome is one of the most common peripheral neuropathies. It affects mainly middle aged women. In the majority of patients the exact cause and pathogenesis of CTS is unclear. Although several occupations have been linked to increased incidence and prevalence of CTS the evidence is not clear. Occupational CTS is uncommon and it is essential to exclude all other causes particularly the intrinsic factors such as obesity before attributing it to occupation. The risk of CTS is high in occupations involving exposure to high pressure, high force, repetitive work, and vibrating tools. The classic symptoms of CTS include nocturnal pain associated with tingling and numbness in the distribution of median nerve in the hand. There are several physical examination tests that will help in the diagnosis of CTS but none of these tests are diagnostic on their own. The gold standard test is nerve conduction studies. However, they are also associated with false positive and false negative results. The diagnosis of CTS should be based on history, physical examination and results of electrophysiological studies. The patient with mild symptoms of CTS can be managed with conservative treatment, particularly local injection of steroids. However, in moderate to severe cases, surgery is the only treatment that provides cure. The basic principle of surgery is to increase the volume of the carpal tunnel by dividing transverse carpal ligament to release the pressure on the median nerve. Apart from early recovery and return to work there is no significant difference in terms of early and late complications and long-term pain relief between endoscopic and open carpal tunnel surgery.
INTRODUCTION
Carpal tunnel syndrome (CTS) is one of the most common upper limb compression neuropathies1–5. CTS account for approximately 90% of all entrapment neuropathies. It is due to an entrapment of the median nerve in the carpal tunnel at the wrist (Figure 1). An estimated one million adults from the United States (annually) have CTS requiring medical treatment6 and the cost to the Health Care system is high. In 1995, Palmer et al estimated that between 400,000 and 500,000 cases of CTS require operative treatment annually in the States, with an economic cost in excess of $2 billion per year7. The surgical decompression rates for UK are 43 to 74 per 100,000 per year 8.
Fig 1.
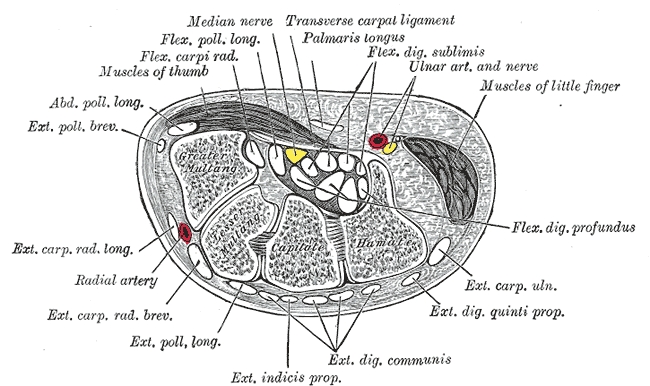
Cross section across wrist (Reproduced, with permission from Bartleby.com: Gray, Henry. Anatomy of the Human Body. Philadelphia: Lea & Febiger, 1918.)
The incidence and prevalence varies, 0.125% – 1% and 5 – 16%, depending upon the criteria used for the diagnosis6,9–14. It is a condition of middle-aged individuals and affects females more often than males. Since its first description by Phalen in the 1950s15, several studies have reported marked female preponderance and a peak incidence around 55 to 60 years6,11,16. In the first population based study, Stevens et al noted that the mean age at diagnosis was 50 years for men and 51 years for women11. In a recent surveillance study from Canterbury and Huddersfield, UK, Bland et al reported an annual incidence of 139.4 cases per 100,000 in females and 67.2 cases per 100,000 in males, with a female to male ratio of 2.0717.
It is one of the most widely recognised occupational health conditions; particularly in industries where work involves high force/pressure and the repetitive use of vibrating tools. Einhorn and Leddy estimated an incidence of 1% in the general population and 5% of workers in certain industries which require repetitive use of the hands and wrists12. In 1999, the US Bureau of Labour Statistics, reported that the median number of days away from work was highest for CTS (27days) when compared to any other major disabling illnesses and injuries18. In addition, estimates by the National Institute for Occupational Safety and Health (NIOSH) suggest that 15 to 20% of Americans are at risk of developing Cumulative Trauma Disorders (CTDs) 19.
AETIOLOGY
There are two distinct varieties of CTS - acute and chronic. The acute form is relatively uncommon and is due to a rapid and sustained rise of pressure in the carpal tunnel. This is most commonly associated with a fracture of the radius as Sir James Paget described in 185419. It is also associated with burns, coagulopathy, local infection and injections. The chronic form is much more common and symptoms can persist for months to years. However, in only 50% of cases is the cause identified, and can be divided into local, regional and systemic causes as summarised in Table I. Carpal tunnel syndrome is common in pregnant women20–23. It is commonly diagnosed during third trimester of pregnancy and it is often bilateral. In the majority of patients symptoms will resolve either spontaneously or will respond to conservative treatment after delivery20,24,25.
Table I.
Various non-occupational causes of Carpal Tunnel Syndrome
| A. Local causes |
|---|
|
| B. Regional causes |
|---|
|
| C. Systemic causes |
|---|
|
ROLE OF OCCUPATION
CTS is the most common form of Repetitive Trauma Disorder (RTD). In 1995, there were approximately 308,000 trauma-related musculoskeletal disorders, representing nearly 62% of all occupational illness cases reported to the US Bureau of Labour Statistics26. Brain et al were the first to implicate occupation as a causal factor in CTS27. At risk occupations include, grinders, cashiers, and meat packers, workers sewing car seats, aircraft engineers, grocery store workers, and small part assembly liners.
The physical factors implicated and extensively studied in relation to occupational CTS include repetition, force, posture, external pressure, and vibration. Repetition is the most widely recognized risk factor for occupational CTS. In epidemiological studies high repetition is defined either by the frequency of the task or the percentage of time spent on repetitive work. A high repetitive job is defined as one which involves the repetitive use of awkward wrist movements lasting less than 30s or when more than 50% of work time is spent performing tasks that involve repetitive awkward wrist movements28.
Experimental studies have shown a higher incidence of CTS in workers who are involved in high force and repetitive work compared to workers who are not28–31. Silverstein et al examined the association between high force / repetitive movements and CTS among 652 workers from 39 jobs from seven different industrial areas28. The authors noted a prevalence of 5.6% among workers in high force and high repetitive jobs compared to 0.6% among workers in low force and low repetitive jobs. The authors showed occupation to be a risk factor only when high force and high repetition are present, but the accuracy of their estimated ratio of 15.5 (95% confidence interval, 1.7–141.5) suffered from a small sample size. High repetitiveness seems to be a greater risk factor than high force but neither was statistically significant alone28. In a case–control study, Armstrong & Chaffin compared patients with CTS to asymptomatic people amongst 18 sewing machine operators and noted that cases that used pinch grip (opposition of the thumb and the distal joints of four fingers) exerted more force than controls32. The authors also noted that cases tended to use non-neutral postures more often and exerted more force in these postures32.
Several epidemiological studies have shown that force is an independent risk factor for CTS, but the dose–response relationship is not clear. In a cross-sectional study by Latko et al, a dose–response relationship was observed between the prevalence of CTS and level of repetition33. In the study by Silverstein et al 28 force was a weaker risk factor than repetition, but in the report by Chiang et al29 force was a stronger risk factor than repetition. Force and repetition increased the risk of CTS in a cumulative way in the Silverstein study. The odds ratio for high force and high repetition group was 15.5 in the Silverstein study. However, Chiang et al showed odds ratio for repetition was 1.1 and did not find a significant association between repetition and force29.
Several studies examining carpal tunnel pressure (CTP) in healthy subjects indicate that the greatest increase in CTP occurs following wrist flexion and extension34,35. In an experimental study on 17 healthy volunteers, Rempel et al measured intra-compartmental pressures using a saline filled catheter introduced into the carpal tunnel36. The authors noted highest mean intra- compartmental pressure (55mm Hg) during full supination and 90 degree metacarpophalangeal (MCP) joint flexion and lowest pressure at 45 degrees of pronation and 45 degrees of MCP joint flexion. The authors speculated that the increased carpal tunnel pressure at full supination and at 90 degree MCP flexion changes the orientation of the tendons, thereby, increasing the volume of the carpal tunnel predisposing to CTS. The authors suggested that the lowest pressures achieved by position should be considered in job and tool design36. In a review of 15 cross-sectional studies involving 32 occupational or exposure groups and six-case studies, Hagberg et al noted a high prevalence of CTS in occupations requiring high force and high repetitive manual movements37. In a review, NIOSH found a strong association between physical factors such as force, repetition, and vibration but did not find a stronger association between non-neutral postures and CTS38.
Occupational risk factors alone do not explain the occurrence of CTS and it is proposed that a combination of several factors is involved. The majority of CTS is attributable to patient related factors (intrinsic risk factors). Several studies have noted that the occurrence of CTS is correlated with unhealthy habits and lifestyle39,40. This was supported by an analysis that showed that 81.5% of the explainable variation in electro-physiologically defined CTS was attributable to body mass index, age, and wrist depth to width ratio, whereas only 8.29% was due to job related factors41. In a study comparing workers with and without CTS, Nathan and colleagues noted that there was a 19% greater lifetime use of tobacco, 75% greater history of alcohol abuse, and 5% greater use of caffeine in workers with CTS36. Furthermore, the authors reported that, current tobacco, caffeine, and alcohol consumption independently predicted 5% of the risk for CTS in female workers42. Several studies have noted high incidence of CTS in patients with high body mass index39,43–45. Garland et al found that gender was a more predictive risk factor for CTS than exposure to high risk occupations46. In a series of 654 hands with CTS, Phalen did not observe any relation between CTS and occupation. Furthermore, he argued that occupational trauma is seldom the precipitating factor in the production of CTS15. It is important to establish the nature of risk factor and the interaction between intrinsic and extrinsic factors. In a longitudinal study of predictors of CTS in industrial workers over a period of 17yrs, Nathan et al did not find an obvious relationship between the incidence of carpal tunnel syndrome and repetitive work. However, the authors noted high incidence of carpal tunnel syndrome in overweight people and in females47.
One of the major drawbacks of studies that show a positive association between occupation and CTS is the wide variety of criteria used to diagnose CTS. Studies conducted in the 1980s depended on patients' self-reported symptoms and physical signs to establish the diagnosis of CTS. Physical signs in CTS have poor reproducibility and poor correlation with symptoms. Ideally, the diagnosis of CTS should be based on combination of symptoms, physical signs and nerve conduction studies. Furthermore, studies relied upon patients to report the degree of occupational exposure. Spielholz et al showed that direct observation and direct measurement of working practices are much more reliable methods of assessment of occupational exposure leading to CTS48. The most often sited publication linking the occupation exposure to high repetitive and force and the increased incidence of CTS relied on patient reported symptoms and physical examination for the diagnosis of CTS. Furthermore, the authors also did not define what constitutes high force and repetition28.
Despite the use of much more rigorous methods to establish the diagnosis of CTS, conflicting results were published in the 1990s linking occupation and CTS. Stetson et al examined workers from several industries and noted significantly lower sensory amplitudes and longer motor and sensory latencies on nerve conduction studies in occupations involving high repetition and force49. Osorio et al studied 56 grocery store workers and found strong associations between forceful and repetitive wrist movements and the prevalence of CTS50. However, several other studies did not find any substantial evidence linking specific occupations and the prevalence or severity of impaired sensory conduction of the median nerve at the carpal tunnel42,51. Moore and Garg et al videotaped work practices of workers from a pot-processing factory. The authors subsequently reviewed workers' medical records and identified all patients with various upper limb neuropathies including CTS. The authors found no significant association between ergonomic factors and the CTS (Relative risk = 2.8, P = 0.44, 23)52. However, the most recent systematic literature review on the role of occupation in carpal tunnel syndrome by Palmer et al, found that the regular use of hand-held vibrating tools increased the risk of CTS by more than 2-fold53. The authors also found substantial evidence for high risk of CTS in occupations requiring high repetitive flexion and extension at wrist and also forceful grip53. However, the authors did not find evidence between the work on keyboard and computers and CTS.
PATHOPHYSIOLOGY
The exact pathogenesis of CTS is not clear. Several theories have been put forward to explain the symptoms and impaired nerve conduction studies. The most popular ones are mechanical compression, micro-vascular insufficiency, and vibration theories. According to mechanical compression theory, symptoms of CTS are due to compression of the median nerve in the carpal tunnel. The major drawback of this theory is that it explains the consequences of compression of the nerve but does not explain the underlying aetiology of mechanical compression. Brain and colleagues attributed the symptoms of CTS to spontaneous median nerve compression in the carpal tunnel27. The term ‘spontaneous’ was used due to lack of clear association between wrist joint deformities and symptoms. The compression was believed to be mediated by several factors such as exertion strain, overuse, hyperfunction, repeated or prolonged wrist extension, prolonged grasping of tools, and unaccustomed manual work27.
The micro-vascular insufficiency theory proposes that the lack of blood supply leads to depletion of nutrients and oxygen to the nerve causing it to slowly lose its ability to transmit nerve impulses. Scar and fibrous tissue eventually develop within the nerve. Depending on the severity of injury, changes in the nerve and muscles may be permanent. The characteristic symptoms of CTS, particularly tingling, numbness and acute pain, along with acute and reversible loss nerve conduction are thought to be secondary to ischemia of the affected nerve segment. Seiler et al showed (by laser Doppler flowmetry) how normal pulsatile blood flow within the median nerve was restored within 1 min of transverse carpal ligament release. The authors concluded that ischemia likely plays a significant role in the aetiology of CTS54. A number of experimental studies support the theory of ischemia due to externally applied compression and due to increased pressure in the carpal tunnel30. The development of ischemia and, therefore, symptoms, will vary according to the integrity of the blood supply of the nerve and the systolic blood pressure. Kiernan et al found that the conduction slowing in the median nerve can be explained by ischemic compression alone and may not always be attributable to disturbed myelination55. Tucci et al noted five times higher levels of interleukin-6, maloionaldehyde bis- (diethyl acetal) and prostaglandin E2 at the time of surgery in patients with CTS compared to asymptomatic volunteers56. The authors concluded that such alteration may be the result of oxidative changes following repetitive ischemia and reperfusion injury.
According to the vibration theory the symptoms of CTS could be due to the effects of long-term use of vibrating tools on the median nerve in the carpal tunnel30. Lundborg et al noted epineural oedema in the median nerve within days following exposure to vibrating hand-held tools. Furthermore, the authors also noted similar change following mechanical, ischemic, and chemical trauma. Interestingly, the authors also report animal studies that show a temporary accumulation of smooth axoplasmic structures and deranged axoplasmic structures following a short exposure to a vibrating force57. These changes were first noted in unmyelinated fibres that serve sympathetic activity; a loss of which could reduce micro-vascular flow to the median nerve leading to disruption of its myelin sheath and decreased motor conduction velocity57.
CLINICAL FEATURES
The symptoms vary depending upon the severity of the disease. In early stages, patients usually complain of symptoms due to the involvement of the sensory component of the median nerve and only later report symptoms from involvement of motor fibres. The most common symptom is burning pain associated with tingling and numbness in the distribution of median nerve distal to wrist. The portion of the hand involved is classically the thumb, index and middle fingers, and radial half of the ring finger. Patients are often awoken by pain in the middle of the night and report hanging their hand out of bed or shaking it vigorously in order to relieve their pain. Patients may report pain, tingling and numbness of the whole hand, but careful questioning will identify that the little finger is rarely involved as it is innervated by the ulnar nerve. Occasionally, however, all five fingers can be involved if the ulnar nerve is affected at same time. Symptoms of nocturnal paraesthesia are reported to be 51–96% sensitive and 27–68% specific58–61. Less common symptoms include a feeling of clumsiness and weakness in the affected hand that is often made worse by activity or work. Patients may also complain of pain radiating to the forearm, elbow or even the shoulder. In some patients shoulder pain may be the presenting symptom but they will never have any objective evidence of sensory changes above the wrist.
In Kendall's series of 327 patients, 313 (95.7%) reported paresthesia; 118 (38%) reported nocturnal symptoms only, 178 (58%) reported symptoms during the day and night, but worse at night, and 17 (5%) reported symptoms during the day only62. In the Yamaguchi et al series, 99% of the 433 surgical patients reported paresthesia63. In Phalen's experience, the typical history was that of a gradual onset of numbness and paresthesia15.
SIGNS
Several tests have been described which help in the diagnosis of CTS. None of these tests are diagnostic on their own. Most of the tests are complementary to each other rather than diagnostic of CTS. A combination of symptoms, signs and diagnostic tests should be taken into account when the diagnosis of CTS is made. The presence or absence of characteristic physical findings has limited diagnostic value. The various tests are Tinel's sign, Phalen's sign, square wrist sign, closed fist sign, flick sign, Katz hand diagram, flexion and extension of wrist test, pressure provocation test, and tourniquet test. There are limited studies that have evaluated the diagnostic use of square wrist sign, flick sign, closed fist sign, and tourniquet test and hence these tests are not discussed in detail in this article. However, it is sufficient to say that prior to routine use of these tests; further evidence is required to support their effectiveness in the diagnosis of CTS. Diminished pinprick sensation (hypalgesia) in the distribution of median nerve compared to the pinprick sensation over the ipsilateral little finger is a very useful diagnostic test in patients with CTS than abnormalities of other sensory modalities.
Tinel's sign
In this test, the examiner taps lightly over the site of the median nerve at the distal wrist crease. Development of tingling or discomfort in the fingers supplied by the median nerve constitutes a positive sign. Tinel described this sign in 191564. He noted that a tingling sensation occurred when an injured nerve was percussed over its proximal stump and speculated that this was a sign of axonal degeneration and intended his sign to be used in patients after blunt traumatic injury to follow the course of the regenerating nerve65–67. Tinel's sign is not a precise test and several factors can influence the outcome of the test. Firstly, its efficacy is reduced, as patients with CTS will have continually regenerating nerves at the distal wrist crease. The other limiting factor is the amount of pressure used to elicit the sign. Testing technique is important when the physician is eliciting Tinel's sign, and subtle differences in test performance probably account for some of the discrepancies in reported prevalence. It is difficult to quantify precisely how much pressure should be used to elicit the sign. The use of too much force or a sharp blow over a normal median nerve will produce finger tingling. This must not be interpreted as the presence of Tinel's sign. The Tinel's sign is associated with sensitivities of 23% to 67%, and specificities of 55% to 100%59,60,65,67–71. In a review, Kuschner et al summarised the frequency of Tinel's sign and reported that it is positive from 8% to 100% of CTS patients67. Tinel's sign is the least accurate test according to Mondelli et al, who did not find a combination of signs more useful than a single sign alone71.
Phalen's test
Phalen and Kendrick described this test in 195715. Flexion of the wrist causes compression of the nerve between the transverse carpal ligament (TCL) and flexor tendons in the carpal tunnel, causing paresthesia in the median nerve distribution70,72 reproducing the patient's symptoms. Phalen performed the test by having the patient hold the forearm vertically with the elbows resting on the table and then allowing both hands to drop with complete wrist flexion for approximately one minute. The test is considered positive when paresthesia develops in less than one minute. Patients with advanced CTS often note paresthesia in less than 20 seconds. The reported sensitivity ranges between 10% and 91% and specificity between 33% and 100%59,60,68,69,73–75.
Katz hand diagram
This is a self–administered diagram, which depicts both the dorsal and palmar aspect of the patient's hands and arms. Patients use this diagram to mark the specific location of their symptoms, characterising them as pain, numbness or tingling, or other. The diagnosis is graded as classic, probable, possible or unlikely to be CTS based on criteria that appear in the hand diagram60,76. In diagrams classified as classic or probable the sensitivity of the test is 80% and the specificity is 90% for the diagnosis of CTS76,77. Katz himself reported a sensitivity of 64% and a specificity of 73%76.
Square wrist sign
Kuhlman et al reported that a square-shaped wrist, where the anterior-posterior dimension of the wrist (at the distal wrist crease) divided by the medio-lateral dimension is greater than 0.7065,78 and weakness of the abductor pollicis brevis were the two most sensitive signs (69 and 66% respectively). This test is associated with a sensitivity of 47% to 69% and specificity of 73% to 83%65,78.
The tethered Median Nerve stress test
LaBan described this test in 1986. It is performed by hyper-extending the supinated wrist and the distal interphalangeal joint of the index finger for a minute. Patients with chronic carpal tunnel syndrome experience pain on the volar aspect of proximal forearm79. LaBan noted that hyper extension of index finger causes distal excursion of the median nerve more than hyperextension of the adjacent fingers80. Raudino evaluated this test in 140 patients with electro- physiologically confirmed CTS and noted that the test was positive in 60 hands (42.8%) compared to the 56.4% positive rate with Phalen's sign and 42% positive rate with the Tinel's sign81.
Pressure provocation test
A positive result in this test is the presence of pain, tingling and numbness in the distribution of the median nerve when the examiner presses with his/her thumb on the palmar aspect of the patient's wrist at the level of the carpal tunnel for 60 seconds. The test is seldom positive. The reported sensitivity is between 28% and 63% and specificity is between 33% and 74%59,65,72,73.
Tourniquet test
A positive result is the development of paresthesia in the distribution of the median nerve when a blood pressure cuff around the patient's arm is inflated to above systolic pressure for a minute or two. The irritated and compressed median nerve is thought to be more susceptible to ischemia than the normal median nerve. However, even normal individuals can also develop the same symptoms and it is difficult to evaluate, especially in mild cases of CTS. The tourniquet's test sensitivity lies between 21% and 52% with a specificity between 36% and 87%59,69.
MOTOR EXAMINATION
Thenar atrophy is a late sign and signifies significant functional loss. Finger weakness associated with an inability to pinch or frequent dropping of grasped objects follows involvement of the motor component. Long-term involvement leads to thenar muscle atrophy (Figs 2 and 3) with associated loss of thumb abduction and opposition strength. Diminished sensation to pinprick in the median nerve distribution always precedes thenar atrophy. Thenar atrophy is seldom noticed by patients and may not be obvious even to the examiner when examined by looking down onto the palm. However, it will be readily appreciated by comparing both palms together (Fig 2)15. In Phalen's series the atrophy of abductor pollicis brevis, opponens pollicis and flexor pollicis brevis was noted in 41% of hands15. Abductor pollicis brevis is the most commonly affected muscle and testing its function is useful in making the diagnosis of CTS.
Fig 2.
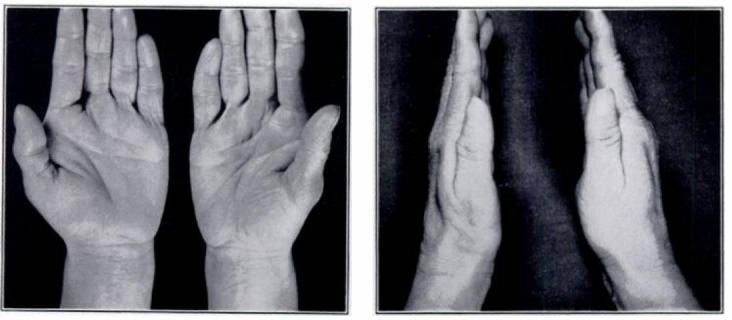
Picture showing moderate thenar atrophy of the left hand in a woman with bilateral carpal tunnel syndrome (Reproduced, with permission from George S. Phalen. The Carpal-Tunnel Syndrome: Seventeen Years' Experience In Diagnosis And Treatment Of Six Hundred Fifty-Four Hands. J Bone Joint Surg Am 1966; 48:211)
Fig 3.

Picture showing moderate thenar atrophy of the right hand in a man with bilateral carpal tunnel syndrome
DIAGNOSIS
Symptoms are often difficult to interpret in patients with CTS. Patients often have difficulty in describing their symptoms, and physicians may have difficulty in interpreting the symptoms. Self-administered tests, such as the Katz diagrams may help reduce these potential sources of errors and bias. The combination of clinical symptoms and signs with electro-diagnostic findings is the most valid way of diagnosing CTS15,82,83.
The role of Nerve Conduction Studies
The nerve conduction studies (NCS) measure the sensory and motor nerve conduction velocity in the median nerve at the level of the wrist. The sensory component of the median nerve is affected much earlier than the motor component and in early stages of CTS there is usually a delay in the sensory nerve conduction velocity. Sensory nerve conduction delay is measured by placing an electrode near the base of the ring finger following which the median nerve is stimulated approximately 13cm proximal to the recording electrode. The antidromic sensory potentials are recorded and measured. The motor nerve conduction velocity from elbow to wrist is measured using surface electrodes.
Median nerve conduction studies are the gold standard diagnostic tests with sensitivities between 49% and 84% and specificities of 95% and 99%84–86. In entrapment neuropathies there will be a delay in the conduction velocity at the point of compression due to the demyelination of the nerve. In patients with clinical symptoms suggestive of CTS with normal sensory conduction velocity, measurement of both motor and sensory conduction velocity increases the diagnostic yield by 10%87. Chang et al found that, in patients with normal sensory and motor conduction velocities, measuring the latency between the median and ulnar nerve for the ring finger and comparing it to the median and radial nerve latency for the thumb increases the diagnostic yield by another 10%87. NCS not only allow a diagnosis of CTS but also help in the diagnosis of other conditions presenting with similar symptoms e.g. cervical radiculopathy, polyneuropathy, other median nerve entrapment syndromes74,88–90.
Although nerve conduction studies are the gold standard test for the confirmation of diagnosis of CTS, they have certain limitations. A small percentage of asymptomatic individuals can have positive NCS. Similarly, a small percentage of patients can have negative NCS despite symptoms suggestive of CTS. Atroshi et al randomly surveyed 2466 individuals in Sweden to find out the incidence of CTS in general population9. 14.4% complained of pain, tingling and numbness in the distribution of the median nerve. However, only 4.9% of individuals with neuropathic symptoms had positive NCS. Furthermore, 18% of asymptomatic subjects had abnormal NCS9. Bingham et al examined 1021 applicants for industrial jobs and noted that 17.5% of the job applicants had abnormal NCS91. However, only 10% of these applicants actually had symptoms suggestive of CTS. In severe CTS cases, NCS results may not correlate with the clinical findings due to the varying nature of the impairment in different nerve fibres. In addition, nerve conduction studies will not accurately predict the recovery following release of the carpal tunnel, though neither do any of the other investigations predict this with any certainty91. Therefore these studies suggest that NCS alone should not be used to diagnose, rather it should be based on presence of clinical symptoms, physical findings and positive nerve conduction studies taken together.
The role of ultrasound in the diagnosis of carpal tunnel syndrome
The diagnosis of CTS is based mainly on clinical symptoms and signs and nerve conduction studies. However, as 13–27% of patients will have a normal NCS92, alternative diagnostic tests such as ultrasound (US) and magnetic resonance imaging (MRI) are useful.
In a prospective study, Keles examined the role of US in 35 patients with a NCS confirmed diagnosis of CTS and compared it to 40 normal wrists. US measured the cross-sectional area (CSA) of the median nerve, bowing of the flexor retinaculum (FR) and flattening of the flexor retinaculum93. The CSA of the median nerve and bowing of the FR were significantly increased in patients with NCS positive CTS when compared to controls. The flattening of the FR had no correlation with diagnosis of CTS. Koyuncuoglu studied the role of US in 59 patients with clinical diagnosis of CTS with negative NCS findings by comparing their results with US findings in 30 normal wrists. They found a CSA of larger than 10.5mm in 18 patients compared to one wrist in the control group94. El Miedany et al compared the results of US with NCS in a group of patients with CTS against a control group and observed a high degree of correlation between the US findings and NCS in diagnosing and in assessing the severity of CTS. US also helped to identify the underlying cause of CTS and thus facilitated planning of treatment95.
TREATMENT
There are several treatment options and they can be broadly categorised into surgical and non-surgical.Non-surgical methods are effective in patients with mild to moderate CTS. They are indicated in patients with no muscle weakness or atrophy, absent denervation (on electromyography needle examination), and with only a mild abnormality on nerve conduction studies96. Pregnant women with CTS rarely require surgical treatment. In the majority of patients symptoms will resolve either spontaneously or will respond to conservative treatment after delivery23–25.
The various non-surgical methods include: use of hand brace, splinting of the wrist, ultrasonic therapy, laser therapy, oral steroids, non-steroid anti-inflammatory drugs (NSAIDs), oral vitamin B6, local injection of corticosteroids with, or without, insulin, work place modifications and yoga etc. Description of the role of each type of non-surgical treatment option is beyond the scope of this review. In the recent Cochrane review, O'Connor et al looked at the available evidence about the role of various non-surgical treatment options in mild to moderate CTS97. They concluded that a significant short-term benefit could be gained with oral steroids, wrist splinting, local ultrasound therapy, yoga and carpal bone mobilization. However, the authors did not find any evidence to support the role of other treatment methods such as the use of a hand brace, exercises, usage of ergonomic key boards, oral diuretics and oral NSAIDs97.
Steroid injection into the wrist is often successful. It may cause symptoms to worsen temporarily but can produce complete or significant pain relief in 60 to 70% of patients for weeks to years96,98–100. In a randomized, single blind controlled study Hui et al evaluated the role of steroid injection in patients with idiopathic CTS confirmed by NCS101. The primary outcome of the study was symptomatic relief measured by a global symptom score, which rated symptoms on a scale of 0 (no symptoms) to 50 (most severe). The authors randomized 50 patients, 25 into steroid and 25 into the open surgical group. The authors noted greater symptomatic relief in surgical group at 20 weeks follow-up. Furthermore, surgical decompression resulted in greater improvement in median nerve distal motor latencies and sensory nerve conduction velocity 101. One of the major complications of steroid injection is iatrogenic injury to the median nerve. The safest location of injection is not clear. Though Racasan et al report that the safest location for the steroid injection is through the flexor retinaculum tendon102. Agarwal et al evaluated the role of methyl prednisolone acetate injection in 40 patients with mild idiopathic CTS. Patients were evaluated at 3 and 12 months103. The authors noted marked improvement of symptoms in 93.7% patients at 3 months follow up. Furthermore, they also found a significant improvement in the mean values of the distal motor and sensory latency at the wrist at 3 months. At 16 months median follow up 79% continued to have improvement in their symptoms and only 16.6% patients suffered a relapse of their symptoms following an initial response103. In a randomized controlled trial, Ly-Pen et al compared the role of local steroid injection with open surgery. The authors noted that local steroid injection was better than surgical decompression for the symptomatic relief from nocturnal paresthesia at 3 and 6 months. At 12 months follow up local steroids injection was as effective as surgical decompression104.
Surgery
Surgery consists of division of transverse carpal ligament. This reduces the pressure on the median nerve by increasing the space in the carpal tunnel. Surgery is indicated in almost all patients with moderate to severe CTS. An absolute indication for CT release (CTR) is muscular atrophy105. Two different types of surgical approaches are in use for the treatment of CTS; open and endoscopic release. Open CTR (OCTR) is the traditional option and still the recommended method of surgical treatment for idiopathic CTS. It was first performed by Herbert Galloway in 1924, though since then several modifications have been made to refine it106. The classic OCTR uses a curved longitudinal inter-thenar incision, approximately 4 to 5 cm in length107. It involves opening of subcutaneous tissue, superficial fascia and transverse carpal ligament and 2 to 3 cm of distal forearm fascia under direct vision. The canal also inspected for mass lesions and anatomical abnormalities.
Open carpal tunnel release is easy to perform and in majority of patients it leads to good symptomatic relief with a low complication rate. In a series of 32 patients who underwent OCTR over a period of four years, 88% of patients reported good functional and symptomatic improvement108. The well recognised early complications are incomplete release of TCL, neuropraxia or injury to the median or ulnar nerve, inadvertent entry to Guyon's canal (the tunnel between the pisiform and hamate bone and the ligament connecting both bones), injury to the palmar cutaneous or recurrent motor branch of the median nerve and injury to the superficial palmar arch or ulnar artery109. These complications are rare as surgery is performed under direct vision. The late complications are scar tenderness, loss of grip strength, pillar pain, and rarely reflex sympathetic dystrophy and bow stringing of flexor tendons. Pillar pain is a frequent complication of both open and endoscopic release procedures. The pillar pain is characterised by pain or tenderness in the thenar or hypothenar eminence or radial and ulnar tenderness. The incidence varies between 6 and 36%110,111. It delays resumption of daily activities, return to work, and causes emotional distress all leading to an increased cost to health care system112. The exact aetiology of pillar pain is not clear. However, the pain could be secondary to alteration of the carpal arch structures113, oedema of the tissues superficial to TCL, injury to the cutaneous branches of the palm114, or could be due to relaxation of the muscles of opposition and pinch following sectioning of TCL115.
To minimise post-operative complications and reduce length of hospital stay, several modifications to the length, location and shape of the incision in OCTR have been described. One of the modifications of classical OCTR is to make a limited transverse incision of ≤ 2cm in the same location as classical OCTR. Another modification is a limited open release performed by Atik et al in 2001116. The overall success rate of OCTR is more than 95% with a complication rate of less than 3%117. Studies have found no difference between patients who undergo bilateral simultaneous OCTR when compared to patients who undergo consecutive operations in terms of the post-operative complication rate, hospital stay, time to return work and the overall cost118.
As in other fields of surgery, less invasive techniques have been introduced into carpal tunnel surgery to facilitate earlier return to work and reduce post-operative pain and the first endoscopic carpal tunnel release was performed by Okutsu and his colleagues in Japan in 1987119. Since its introduction several modifications of the technique have been described in the literature. There are several endoscopic approaches but the underlying principle is the same; to release transverse carpal ligament. ECTR techniques can be broadly divided into single portal and dual portal techniques depending on the number of ports used to access the carpal tunnel. The two most commonly used techniques are single-portal technique described by Agee121 and two-portal technique described by Chow120. It is beyond the scope of this review to go into details of each technique. The reported success rates for surgical treatment range from 70 to 90%. In an extensive review of all articles on ECTR covering six different types of techniques, Jimenez et al found that the endoscopic release techniques offer similar success and complication rate as open surgery117. The overall success rate for ECTR was 96.52% with a complication rate of 2.67% and a failure rate of 2.61%117. The most common complications noted by the authors were paresthesia of the ulnar and median nerves, injury to superficial palmar arch, reflex sympathetic dystrophy, flexor tendons lacerations and incomplete division of TCL117. The Cochrane database group reviewed all available evidence from randomized controlled trials comparing various surgical techniques in terms of efficacy in relieving symptoms, promoting early return to work and post-operative complications and found no strong evidence to favour alternative surgical techniques against the standard open technique. Specifically, they found conflicting evidence in support of endoscopic release leading to an earlier return to work and/or activities of daily living when compared to open CTR122. These findings have been replicated by another meta-analysis study of randomized controlled trials comparing endoscopic and open carpal tunnel decompression which also found no conclusive evidence favouring ECTR with regard to symptom relief and return to work123. However, they found that ECTR was associated with reduced scar tenderness and increase in pinch grip and pinch strength at 12 weeks follow up123.
Evaluation of response following surgery
One of the major problems in assessing the effectiveness of various treatment methods is a lack of agreed outcome assessment criteria. Several outcome assessment measures have been used to measure the outcome or effectiveness of treatment and can be broadly divided into those that assess patient bodily activities and function and those that assess activity and participation. The most commonly used are self-reported symptoms questionnaires, hand diagrams, records of daily activity at work and at leisure time, return to work, complications, NCS, and quality of life questionnaires. Some patient outcome questionnaires assess the whole upper limb function rather than the wrist alone e.g. the patient evaluation measure (PEM)124 and the Disabilities of the Arm, Shoulder and hand (DASH)125. Short-Form-36 (SF-36) measures generic quality of life126. Whilst the only disease specific questionnaire that assesses both functional and activity and participation outcome measures is Boston Carpal Tunnel Questionnaire (BCTQ)127.
The role of NCS in predicting the outcome of surgery is not clear. In a randomized controlled trial, Schrijver et al compared the outcome measures for the severity of complaints with results of NCS and found that nerve conduction studies improved significantly at 12 months128. However, there was only a modest correlation between the improvement in NCS and relief of symptoms following surgery. The authors concluded that patients do not require routine nerve conduction studies following CTR. However, they have recommended the routine use NCS when studying the effects of treatment for CTS 128. Several other studies have shown that NCS improve following surgery 129. Rider et al used a patients rated survey, gap detection test and a rapid pinch and release task to evaluate the response following the carpal tunnel release. The authors found significant improvements in the performance of these tests within the short-term following surgery. He concluded that these tests are good alternatives to NCS in assessing outcome following surgery. The gap detection sensory thresholds test estimates minimum width needed for detection of gap on smooth work surface by probing with one finger130. The gap detection test measures the functional aspects of carpal tunnel syndrome e.g. detection of scratches and surface defects. The rapid pinch and release test measures psychosomatic performance in terms of speed and force control by using an Aluminum strain gauge dynamometer131,132.
In a review of 28 randomized controlled trials of surgical treatment for CTS, Joersch- Herold et al noted that the self-reported symptom resolution, grip or pinch strength and return to work were the more frequently assessed outcomes measures. In addition, the authors noted that majority of the studies used quality of life measures such as SF-36 that measured the psychosocial impact of CTS. Authors concluded that the majority of the studies used outcome measures that mainly assess body structure and functional outcomes but not outcome measures of activity and participation133,134. In a systematic review of 92 studies published over a period of 11 years, Gummesson et al noted that only 4.1% of studies reported outcomes on activity and participation. Furthermore, the studies which included health-related quality of life limited the outcome measure to number of days taken to return to work134.
The BCTQ questionnaire was first introduced in 1993 by Levine et al135. BCTQ is a carpal tunnel syndrome specific outcome assessment questionnaire. It assesses not only the severity of symptoms but also the functional status in patients who have undergone carpal tunnel release. The BCTQ questionnaire has two components. The first part is a Symptom Severity Scale with 11 questions. The second is Functional Status Scale with 8 items that are rated for degree of difficulty on a five-point scale. Each scale generates a final score that ranges from 1 to 5, with a higher score indicating a greater disability. BCTQ has been used extensively as an outcome measure following CTS treatment. It is highly reliable, reproducible and a valid outcome assessment tool. In a systematic review of 10 studies which examined the psychometric properties of BCTQ, Leite et al concluded that BCTQ is highly reliable, responsive, and should replace any other non-standardized methods of assessment127.
CONCLUSIONS
Occupational CTS is uncommon and it is essential to exclude all other causes particularly the intrinsic factors such as obesity before attributing it to occupation. The risk of CTS is high in occupations involving exposure to high pressure, high force, repetitive work, and vibrating tools. The diagnosis of CTS should be based on symptoms and signs and nerve conduction studies. Surgery is the only treatment that provides cure in moderate to severe cases. Apart from early recovery and return to work there is no difference in the early and late complications and the outcome between open and endoscopic surgical decompression.
The authors have no conflict of interest.
REFERENCES
- 1.Eversmann WW., Jr . Entrapment and compression neuropathies. In: Green DP, editor. Operative hand surgery vol 2. New York: Churchill Livingstone; 1993. pp. 1341–85. [Google Scholar]
- 2.Omer GE., Jr Median nerve compression at the wrist. Hand Clin. 1992;8(2):317–24. [PubMed] [Google Scholar]
- 3.Blanc PD, Faucett J, Kennedy JJ, Cisternas M, Yelin E. Self-reported carpal tunnel syndrome: predictors of work disability from the National Health Interview Survey Occupational Health Supplement. Am J Ind Med. 1996;30(3):362–8. doi: 10.1002/(SICI)1097-0274(199609)30:3<362::AID-AJIM16>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 4.Patterson JD, Simmons BP. Outcomes assessment in carpal tunnel syndrome. Hand Clin. 2002;18(2):359–63. doi: 10.1016/s0749-0712(01)00002-6. viii. [DOI] [PubMed] [Google Scholar]
- 5.Katz JN, Simmons BP. Clinical practice. Carpal tunnel syndrome. N Engl J Med. 2002;346(23):1807–12. doi: 10.1056/NEJMcp013018. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka S, Wild DK, Seligman PJ, Behrens V, Cameron L, Putz-Anderson V. The US prevalence of self-reported carpal tunnel syndrome: 1988 National Health Interview Survey data. Am J Public Health. 1994;84(11):1846–8. doi: 10.2105/ajph.84.11.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palmer DH, Hanrahan LP. Social and economic costs of carpal tunnel surgery. Instr Course Lect. 1995;44:167–72. [PubMed] [Google Scholar]
- 8.Burke FD. Carpal tunnel syndrome: reconciling “demand management” with clinical need. J Hand Surg [Br] 2000;25(2):121–7. doi: 10.1054/jhsb.1999.0328. [DOI] [PubMed] [Google Scholar]
- 9.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153–8. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 10.de Krom MC, Knipschild PG, Kester AD, Thijs CT, Boekkooi PF, Spaans F. Carpal tunnel syndrome: prevalence in the general population. J Clin Epidemiol. 1992;45(4):373–6. doi: 10.1016/0895-4356(92)90038-o. [DOI] [PubMed] [Google Scholar]
- 11.Stevens JC, Sun S, Beard CM, O'Fallon WM, Kurland CM. Carpal tunnel syndrome in Rochester, Minnesota, 1961 to 1980. Neurology. 1988;38(1):134–8. doi: 10.1212/wnl.38.1.134. [DOI] [PubMed] [Google Scholar]
- 12.Einhorn N, Leddy JP. Pitfalls of endoscopic carpal tunnel release. Orthop Clin North Am. 1996;27(2):373–80. [PubMed] [Google Scholar]
- 13.Ferry S, Pritchard T, Keenan J, Croft CM, Silman CM. Estimating the prevalence of delayed median nerve conduction in the general population. Br J Rheumatol. 1998;37(6):630–5. doi: 10.1093/rheumatology/37.6.630. [DOI] [PubMed] [Google Scholar]
- 14.Prick JJ, Blaauw G, Vredeveld JW, Oosterloo SJ. Results of carpal tunnel release. Eur J Neurol. 2003;10(6):733–6. doi: 10.1046/j.1468-1331.2003.00663.x. [DOI] [PubMed] [Google Scholar]
- 15.Phalen CM. The carpal-tunnel syndrome. Seventeen years' experience in diagnosis and treatment of six hundred fifty-four hands. J Bone Joint Surg Am. 1966;48(2):211–28. [PubMed] [Google Scholar]
- 16.Mondelli M, Giannini F, Giacchi M. Carpal tunnel syndrome incidence in a general population. Neurology. 2002;58(2):289–94. doi: 10.1212/wnl.58.2.289. [DOI] [PubMed] [Google Scholar]
- 17.Bland JD, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991–2001. J Neurol Neurosurg Psychiatry. 2003;74(12):1674–9. doi: 10.1136/jnnp.74.12.1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics. News: lost-work time injuries and illnesses: Characteristics and resulting time away from work. United States: Bureau of Labour Statistics; 2001. [Google Scholar]
- 19.Melhorn JM. CTD: carpal tunnel syndrome, the facts and myths. Kans Med. 1994;95(9):189–92. [PubMed] [Google Scholar]
- 20.Stolp-Smith KA, Pascoe MK, Ogburn PL., Jr Carpal tunnel syndrome in pregnancy: frequency, severity, and prognosis. Arch Phys Med Rehabil. 1998;79(10):1285–7. doi: 10.1016/s0003-9993(98)90276-3. [DOI] [PubMed] [Google Scholar]
- 21.Bahrami MH, Rayegani SM, Fereidouni M, Baghbani M. Prevalence and severity of carpal tunnel syndrome (CTS) during pregnancy. Electromyogr Clin Neurophysiol. 2005;45(2):123–5. [PubMed] [Google Scholar]
- 22.Sax TW, Rosenbaum RB. Neuromuscular disorders in pregnancy. Muscle Nerve. 2006;34(5):559–71. doi: 10.1002/mus.20661. [DOI] [PubMed] [Google Scholar]
- 23.Finsen V, Zeitlmann H. Carpal tunnel syndrome during pregnancy. Scand J Plast Reconstr Surg Hand Surg. 2006;40(1):41–5. doi: 10.1080/02844310500410351. [DOI] [PubMed] [Google Scholar]
- 24.Turgut V, Cetinşahinahin M, Turgut M, Bölükbaşi O. The management of carpal tunnel syndrome in pregnancy. J Clin Neurosci. 2001;8(4):332–4. doi: 10.1054/jocn.2000.0761. [DOI] [PubMed] [Google Scholar]
- 25.Mondelli V, Rossi S, Monti E, Aprile I, Caliandro P, Pazzaglia C, et al. Long term follow-up of carpal tunnel syndrome during pregnancy: a cohort study and review of the literature. Electromyogr Clin Neurophysiol. 2007;47(6):259–71. [PubMed] [Google Scholar]
- 26.Bernard BP, editor. Musculoskeletal disorders and workplace factors. 1997 A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity, and low back. NIOSH Publication No 97 – 141. U.S. Department of Health and Human Services, Public Health Service Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; Available from: http://www.cdc.gov/niosh/docs/97-141/97-141pd.html.
- 27.Brian WR, Wright AD. Spontaneous compression of both median nerves in the carpal tunnel. Lancet. 1947;1:277–82. doi: 10.1016/s0140-6736(47)90093-7. [DOI] [PubMed] [Google Scholar]
- 28.Silverstein BA, Fine LJ, Armstrong TJ. Occupational factors and carpal tunnel syndrome. Am J Ind Med. 1987;11(3):343–58. doi: 10.1002/ajim.4700110310. [DOI] [PubMed] [Google Scholar]
- 29.Chiang HC, Chen SS, Yu HS, Ko YC. The occurrence of carpal tunnel syndrome in frozen food factory employees. Gaoxiong Yi Xue Ke Xue Za Zhi. 1990;6(2):73–80. [PubMed] [Google Scholar]
- 30.Viikari-Juntura E, Silverstein B. Role of physical load factors in carpal tunnel syndrome. Scand J Work Environ Health. 1999;25(3):163–85. doi: 10.5271/sjweh.423. [DOI] [PubMed] [Google Scholar]
- 31.Stetson DS, Silverstein BA, Keyserling WM, Wolfe WA, Albers JW. Hypothesis relating cumulative trauma to the median nerve with sub-clinical nerve conduction deficits. Am J Ind Med. 1995;27(2):309–10. doi: 10.1002/ajim.4700270216. [DOI] [PubMed] [Google Scholar]
- 32.Armstrong TJ, Chaffin DB. Carpal tunnel syndrome and selected personal attributes. J Occup Med. 1979;21(7):481–6. [PubMed] [Google Scholar]
- 33.Latko WA, Armstrong TJ, Franzblau A, Ulin SS, Werner RA, Albers JW. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. Am J Ind Med. 1999;36(2):248–59. doi: 10.1002/(sici)1097-0274(199908)36:2<248::aid-ajim4>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 34.Werner R, Armstrong TJ, Bir C, Aylard MK. Intracarpal canal pressures: the role of finger, hand, wrist and forearm position. Clin Biomech (Bristol, Avon) 1997;12(1):44–51. doi: 10.1016/s0268-0033(96)00044-7. [DOI] [PubMed] [Google Scholar]
- 35.Ham SJ, Kolkman WF, Heeres J, den Boer JA. Changes in the carpal tunnel due to action of the flexor tendons: visualization with magnetic resonance imaging. J Hand Surg [Am] 1996;21(6):997–1003. doi: 10.1016/s0363-5023(96)80307-8. [DOI] [PubMed] [Google Scholar]
- 36.Rempel D, Bach JM, Gordon L, So Y. Effects of forearm pronation/supination on carpal tunnel pressure. J Hand Surg [Am] 1998;23(1):38–42. doi: 10.1016/S0363-5023(98)80086-5. [DOI] [PubMed] [Google Scholar]
- 37.Hagberg M, Morgenstern H, Kelsh M. Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scand J Work Environ Health. 1992;18(6):337–45. doi: 10.5271/sjweh.1564. [DOI] [PubMed] [Google Scholar]
- 38.Putz-Anderson Vern, Bernard Bruce P., Burt Susan E., Cole Libby L., Fairfield-Estill Cheryl, Fine Lawrence J., et al. 1997. Musculoskeletal Disorders and Workplace Factors: A Critical Review of Epidemiologic Evidence for Work-Related Musculoskeletal Disorders of the Neck, Upper Extremity, and Low Back: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health.
- 39.Lam N, Thurston A. Association of obesity, gender, age and occupation with carpal tunnel syndrome. Aust N Z J Surg. 1998;68(3):190–3. doi: 10.1111/j.1445-2197.1998.tb04743.x. [DOI] [PubMed] [Google Scholar]
- 40.Becker J, Nora DB, Gomes I, Stringari FF, Seitensus R, Panosso JS, et al. An evaluation of gender, obesity, age and diabetes mellitus as risk factors for carpal tunnel syndrome. Clin Neurophysiol. 2002;113(9):1429–34. doi: 10.1016/s1388-2457(02)00201-8. [DOI] [PubMed] [Google Scholar]
- 41.Gerr F, Letz R. Risk factors for carpal tunnel syndrome in industry: blaming the victim? J Occup Med. 1992;34(11):1117–9. doi: 10.1097/00043764-199211000-00016. [DOI] [PubMed] [Google Scholar]
- 42.Nathan PA, Meadows KD, Doyle LS. Occupation as a risk factor for impaired sensory conduction of the median nerve at the carpal tunnel. J Hand Surg [Br] 1988;13(2):167–70. doi: 10.1016/0266-7681_88_90130-1. [DOI] [PubMed] [Google Scholar]
- 43.Bland JD. The relationship of obesity, age, tunnel syndrome: more complex than was thought? Muscle Nerve. 2005;32(4):527–32. doi: 10.1002/mus.20408. [DOI] [PubMed] [Google Scholar]
- 44.Moghtaderi A, Izadi S, Sharafadinzadeh N. An evaluation of gender, body mass index, wrist circumference and wrist ratio as independent risk factors for carpal tunnel syndrome. Acta Neurol Scand. 2005;112(6):375–9. doi: 10.1111/j.1600-0404.2005.00528.x. [DOI] [PubMed] [Google Scholar]
- 45.Boz C, Ozmenoglu M, Altunayoglu V, Velioglu S, Alioglu Z. Individual risk factors for carpal tunnel syndrome: an evaluation of body mass index, wrist index and hand anthropometric measurements. Clin Neurol Neurosurg. 2004;106(4):294–9. doi: 10.1016/j.clineuro.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 46.Garland FC, Garland CF, Doyle EJ, Jr., Balazs LL, Levine R, Pugh WM, et al. Carpal tunnel syndrome and occupation in U.S. Navy enlisted personnel. Arch Environ Health. 1996;51(5):395–407. doi: 10.1080/00039896.1996.9934428. [DOI] [PubMed] [Google Scholar]
- 47.Nathan PA, Istvan JA, Meadows KD. A longitudinal study of predictors of research-defined carpal tunnel syndrome in industrial workers: findings at 17 years. J Hand Surg [Br] 2005;30(6):593–8. doi: 10.1016/j.jhsb.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 48.Spielholz P, Silverstein B, Morgan M, Checkoway H, Kaufman J. Comparison of self-report, video observation and direct measurement methods for upper extremity musculoskeletal disorder physical risk factors. Ergonomics. 2001;44(6):588–613. doi: 10.1080/00140130118050. [DOI] [PubMed] [Google Scholar]
- 49.Stetson DS, Silverstein BA, Keyserling WM, Wolfe RA, Albers JW. Median sensory distal amplitude and latency: comparisons between non-exposed managerial/professional employees and industrial workers. Am J Ind Med. 1993;24(2):175–89. doi: 10.1002/ajim.4700240205. [DOI] [PubMed] [Google Scholar]
- 50.Osorio AM, Ames RG, Jones J, Castorina J, Rempel D, Estrin W, et al. Carpal tunnel syndrome among grocery store workers. Am J Ind Med. 1994;25(2):229–45. doi: 10.1002/ajim.4700250209. [DOI] [PubMed] [Google Scholar]
- 51.Schottland JR, Kirschberg GJ, Fillingim R, Davis VP, Hogg F. Median nerve latencies in poultry processing workers: an approach to resolving the role of industrial “cumulative trauma” in the development of carpal tunnel syndrome. J Occup Med. 1991;33(5):627–31. [PubMed] [Google Scholar]
- 52.Moore JS, Garg A. Upper extremity disorders in a pork processing plant: relationships between job risk factors and morbidity. Am Ind Hyg Assoc J. 1994;55(8):703–15. doi: 10.1080/15428119491018592. [DOI] [PubMed] [Google Scholar]
- 53.Palmer KT, Harris EC, Coggon D. Carpal tunnel syndrome and its relation to occupation: a systematic literature review. Occup Med (Lond) 2007;57(1):57–66. doi: 10.1093/occmed/kql125. [DOI] [PubMed] [Google Scholar]
- 54.Seiler JG, 3rd, Milek MA, Carpenter GK, Swiontkowski MF. Intraoperative assessment of median nerve blood flow during carpal tunnel release with laser Doppler flowmetry. J Hand Surg [Am] 1989;14(6):986–91. doi: 10.1016/s0363-5023(89)80048-6. [DOI] [PubMed] [Google Scholar]
- 55.Kiernan MC, Mogyoros I, Burke D. Conduction block in carpal tunnel syndrome. Brain. 1999;122(5):933–41. doi: 10.1093/brain/122.5.933. [DOI] [PubMed] [Google Scholar]
- 56.Tucci MA, Barbieri RA, Freeland AE. Biochemical and histological analysis of the flexor tenosynovium in patients with carpal tunnel syndrome. Biomed Sci Instrum. 1997;33:246–51. [PubMed] [Google Scholar]
- 57.Lundborg G, Dahlin LB, Danielsen N, Hansson HA, Necking LE, Pyykko I. Intraneural edema following exposure to vibration. Scand J Work Environ Health. 1987;13(4):326–9. doi: 10.5271/sjweh.2033. [DOI] [PubMed] [Google Scholar]
- 58.Szabo RM, Slater RR, Jr., Farver TB, Stanton DB, Sharman WK. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg [Am] 1999;24(4):704–14. doi: 10.1053/jhsu.1999.0704. [DOI] [PubMed] [Google Scholar]
- 59.Buch-Jaeger N, Foucher G. Correlation of clinical signs with nerve conduction tests in the diagnosis of carpal tunnel syndrome. J Hand Surg [Br] 1994;19(6):720–4. doi: 10.1016/0266-7681(94)90244-5. [DOI] [PubMed] [Google Scholar]
- 60.Katz JN, Larson MG, Sabra A, Krarup C, Stirrat CR, Sethi R, et al. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990;112(5):321–7. doi: 10.7326/0003-4819-112-5-321. [DOI] [PubMed] [Google Scholar]
- 61.Gupta SK, Benstead TJ. Symptoms experienced by patients with carpal tunnel syndrome. Can J Neurol Sci. 1997;24(4):338–42. doi: 10.1017/s0317167100033023. [DOI] [PubMed] [Google Scholar]
- 62.Kendall WW. Results of treatment of severe carpal tunnel syndrome without internal neurolysis of the median nerve. J Bone Joint Surg Am. 1988;70(1):151. [PubMed] [Google Scholar]
- 63.Yamaguchi DM, Lipscomb PR, Soule EH. Carpal Tunnel Syndrome. Minn Med. 1965;48:22–33. [PubMed] [Google Scholar]
- 64.Hoffmann P, Buck-Gramcko D, Lubahn JD. The Hoffmann-Tinel sign. 1915. J Hand Surg [Br] 1993;18(6):800–5. doi: 10.1016/0266-7681(93)90249-f. [DOI] [PubMed] [Google Scholar]
- 65.Kuhlman KA, Hennessey WJ. Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil. 1997;76(6):451–7. doi: 10.1097/00002060-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 66.Gelmers HJ. The significance of Tinel's sign in the diagnosis of carpal tunnel syndrome. Acta Neurochir (Wien) 1979;49(3–4):255–8. doi: 10.1007/BF01808965. [DOI] [PubMed] [Google Scholar]
- 67.Kuschner SH, Ebramzadeh E, Johnson D, Brien WW, Sherman R. Tinel's sign and Phalen's test in carpal tunnel syndrome. Orthopedics. 1992;15(11):1297–302. doi: 10.3928/0147-7447-19921101-08. [DOI] [PubMed] [Google Scholar]
- 68.Gerr F, Letz R, Harris-Abbott D, Hopkins LC. Sensitivity and specificity of vibrometry for detection of carpal tunnel syndrome. J Occup Environ Med. 1995;37(9):1108–15. doi: 10.1097/00043764-199509000-00012. [DOI] [PubMed] [Google Scholar]
- 69.Golding DN, Rose DM, Selvarajah K. Clinical tests for carpal tunnel syndrome: an evaluation. Br J Rheumatol. 1986;25(4):388–90. doi: 10.1093/rheumatology/25.4.388. [DOI] [PubMed] [Google Scholar]
- 70.Heller L, Ring H, Costeff H, Solzi P. Evaluation of Tinel's and Phalen's signs in diagnosis of the carpal tunnel syndrome. Eur Neurol. 1986;25(1):40–2. doi: 10.1159/000115985. [DOI] [PubMed] [Google Scholar]
- 71.Mondelli M, Passero S, Giannini F. Provocative tests in different stages of carpal tunnel syndrome. Clin Neurol Neurosurg. 2001;103(3):178–83. doi: 10.1016/s0303-8467(01)00140-8. [DOI] [PubMed] [Google Scholar]
- 72.Burke DT, Burke MA, Bell R, Stewart GW, Mehdi RS, Kim HJ. Subjective swelling: a new sign for carpal tunnel syndrome. Am J Phys Med Rehabil. 1999;78(6):504–8. doi: 10.1097/00002060-199911000-00002. [DOI] [PubMed] [Google Scholar]
- 73.De Smet L, Steenwerckx A, Van den Bogaert G, Cnudde P, Fabry G. Value of clinical provocative tests in carpal tunnel syndrome. Acta Orthop Belg. 1995;61(3):177–82. [PubMed] [Google Scholar]
- 74.Kaufman MA. Differential diagnosis and pitfalls in electrodiagnostic studies and special tests for diagnosing compressive neuropathies. Orthop Clin North Am. 1996;27(2):245–52. [PubMed] [Google Scholar]
- 75.Bruske J, Bednarski M, Grzelec H, Zyluk A. The usefulness of the Phalen test and the Hoffmann-Tinel sign in the diagnosis of carpal tunnel syndrome. Acta Orthop Belg. 2002;68(2):141–5. [PubMed] [Google Scholar]
- 76.Katz JN, Stirrat CR, Larson MG, Fossel AH, Eaton HM, Liang MH. A self-administered hand symptom diagram for the diagnosis and epidemiologic study of carpal tunnel syndrome. J Rheumatol. 1990;17(11):1495–8. [PubMed] [Google Scholar]
- 77.Katz JN, Stirrat CR. A self-administered hand diagram for the diagnosis of carpal tunnel syndrome. J Hand Surg [Am] 1990;15(2):360–3. doi: 10.1016/0363-5023(90)90124-a. [DOI] [PubMed] [Google Scholar]
- 78.Radecki P. A gender specific wrist ratio and the likelihood of a median nerve abnormality at the carpal tunnel. Am J Phys Med Rehabil. 1994;73(3):157–62. doi: 10.1097/00002060-199406000-00003. [DOI] [PubMed] [Google Scholar]
- 79.LaBan V, Friedman NA, Zemenick GA. “Tethered” median nerve stress test in chronic carpal tunnel syndrome. Arch Phys Med Rehabil. 1986;67(11):803–4. [PubMed] [Google Scholar]
- 80.LaBan MM, MacKenzie JR, Zemenick GA. Anatomic observations in carpal tunnel syndrome as they relate to the tethered median nerve stress test. Arch Phys Med Rehabil. 1989;70(1):44–6. [PubMed] [Google Scholar]
- 81.Raudino F. Tethered median nerve stress test in the diagnosis of carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 2000;40(1):57–60. [PubMed] [Google Scholar]
- 82.Stevens JC. AAEE minimonograph #26: The electrodiagnosis of carpal tunnel syndrome. Muscle Nerve. 1987;10(2):99–113. doi: 10.1002/mus.880100202. [DOI] [PubMed] [Google Scholar]
- 83.Rempel D, Evanoff B, Amadio PC, de Krom M, Franklin G, Franzblau A, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88(10):1447–51. doi: 10.2105/ajph.88.10.1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Practice parameter for electro diagnostic studies in carpal tunnel syndrome (summary statement). American Academy of Neurology, American Association of Electro diagnostic Medicine, and American Academy of Physical Medicine and Rehabilitation. Neurology. 1993;43(11):2404–5. doi: 10.1212/wnl.43.11.2404. [DOI] [PubMed] [Google Scholar]
- 85.Practice parameter for carpal tunnel syndrome (summary statement). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1993;43(11):2406–9. [PubMed] [Google Scholar]
- 86.Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993;16(12):1392–414. doi: 10.1002/mus.880161220. [DOI] [PubMed] [Google Scholar]
- 87.Chang MH, Liu LH, Lee YC, Wei SJ, Chiang HL, Hsieh PF. Comparison of sensitivity of transcarpal median motor conduction velocity and conventional conduction techniques in electro diagnosis of carpal tunnel syndrome. Clin Neurophysiol. 2006;117(5):984–91. doi: 10.1016/j.clinph.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 88.Dawson DM. Entrapment neuropathies: clinical overview. Hosp Pract (Minneap) 1995;30(8):37–40. 43–4. doi: 10.1080/21548331.1995.11443241. [DOI] [PubMed] [Google Scholar]
- 89.Spinner RJ, Bachman JW, Amadio PC. The many faces of carpal tunnel syndrome. Mayo Clin Proc. 1989;64(7):829–36. doi: 10.1016/s0025-6196(12)61756-x. [DOI] [PubMed] [Google Scholar]
- 90.Haig AJ, Tzeng HM, LeBreck DB. The value of electro diagnostic consultation for patients with upper extremity nerve complaints: a prospective comparison with the history and physical examination. Arch Phys Med Rehabil. 1999;80(10):1273–81. doi: 10.1016/s0003-9993(99)90029-1. [DOI] [PubMed] [Google Scholar]
- 91.Bingham RC, Rosecrance JC, Cook TM. Prevalence of abnormal median nerve conduction in applicants for industrial jobs. Am J Ind Med. 1996;30(3):355–61. doi: 10.1002/(SICI)1097-0274(199609)30:3<355::AID-AJIM15>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 92.Bodofsky EB, Wu KD, Campellone JV, Greenberg WM, Tomaio AC. A sensitive new median-ulnar technique for diagnosing mild Carpal Tunnel Syndrome. Electromyogr Clin Neurophysiol. 2005;45(3):139–44. [PubMed] [Google Scholar]
- 93.Keles I, Karagulle Kendi AT, Aydin G, Zog SG, Orkun S. Diagnostic precision of ultrasonography in patients with carpal tunnel syndrome. Am J Phys Med Rehabil. 2005;84(6):443–50. doi: 10.1097/01.phm.0000163715.11645.96. [DOI] [PubMed] [Google Scholar]
- 94.Koyuncuoglu HR, Kutluhan S, Yesildag A, Oyar O, Guler K, Ozden A. The value of ultrasonographic measurement in carpal tunnel syndrome in patients with negative electro diagnostic tests. Eur J Radiol. 2005;56(3):365–9. doi: 10.1016/j.ejrad.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 95.El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford) 2004;43(7):887–95. doi: 10.1093/rheumatology/keh190. [DOI] [PubMed] [Google Scholar]
- 96.McGrath MH. Local steroid therapy in the hand. J Hand Surg [Am] 1984;9(6):915–21. doi: 10.1016/s0363-5023(84)80080-5. [DOI] [PubMed] [Google Scholar]
- 97.O'Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1) doi: 10.1002/14651858.CD003219. CD003219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gelberman RH, Aronson D, Weisman MH. Carpal-tunnel syndrome. Results of a prospective trial of steroid injection and splinting. J Bone Joint Surg Am. 1980;62(7):1181–4. [PubMed] [Google Scholar]
- 99.Green DP. Diagnostic and therapeutic value of carpal tunnel injection. J Hand Surg [Am] 1984;9(6):850–4. doi: 10.1016/s0363-5023(84)80065-9. [DOI] [PubMed] [Google Scholar]
- 100.Giannini F, Passero S, Cioni R, Paradiso C, Battistini N, Giordano N, et al. Electrophysiologic evaluation of local steroid injection in carpal tunnel syndrome. Arch Phys Med Rehabil. 1991;72(10):738–42. [PubMed] [Google Scholar]
- 101.Hui AC, Wong S, Leung CH, Tong P, Mok V, Poon D, et al. A randomized controlled trial of surgery vs. steroid injection for carpal tunnel syndrome. Neurology. 2005;64(12):2074–8. doi: 10.1212/01.WNL.0000169017.79374.93. [DOI] [PubMed] [Google Scholar]
- 102.Racasan O, Dubert T. The safest location for steroid injection in the treatment of carpal tunnel syndrome. J Hand Surg [Br] 2005;30(4):412–4. doi: 10.1016/j.jhsb.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 103.Agarwal V, Singh R, Sachdev A, Wiclaff, Shekhar S, Goel D. A prospective study of the long-term efficacy of local methyl prednisolone acetate injection in the management of mild carpal tunnel syndrome. Rheumatology (Oxford) 2005;44(5):647–50. doi: 10.1093/rheumatology/keh571. [DOI] [PubMed] [Google Scholar]
- 104.Ly-Pen D, Andreu JL, de Blas G, Sanchez-Olaso A, Millan I. Surgical decompression versus local steroid injection in carpal tunnel syndrome: a one-year, prospective, randomized, open, controlled clinical trial. Arthritis Rheum. 2005;52(2):612–9. doi: 10.1002/art.20767. [DOI] [PubMed] [Google Scholar]
- 105.Harris CM, Tanner E, Goldstein MN, Pettee DS. The surgical treatment of the carpal-tunnel syndrome correlated with preoperative nerve-conduction studies. J Bone Joint Surg Am. 1979;61(1):93–8. [PubMed] [Google Scholar]
- 106.Amadio PC. The first carpal tunnel release? J Hand Surg [Br] 1995;20(1):40–1. doi: 10.1016/s0266-7681(05)80013-0. [DOI] [PubMed] [Google Scholar]
- 107.Taleisnik J. The palmar cutaneous branch of the median nerve and the approach to the carpal tunnel. An anatomical study. J Bone Joint Surg Am. 1973;55(6):1212–7. [PubMed] [Google Scholar]
- 108.Badger SA, O'Donnell ME, Sherigar JM, Connolly P, Spence RAJ. Open Carpal Tunnel Release – still a safe and effective operation. Ulster Med J. 2008;77(1):21–23. [PMC free article] [PubMed] [Google Scholar]
- 109.Seiler JG, 3rd, Barnes K, Gelberman RH, Chalidapong P. Endoscopic carpal tunnel release: an anatomic study of the two-incision method in human cadavers. J Hand Surg [Am] 1992;17(6):996–1002. doi: 10.1016/s0363-5023(09)91045-0. [DOI] [PubMed] [Google Scholar]
- 110.Mirza MA, King ET, Jr., Tanveer S. Palmar uniportal extrabursal endoscopic carpal tunnel release. Arthroscopy. 1995;11(1):82–90. doi: 10.1016/0749-8063(95)90093-4. [DOI] [PubMed] [Google Scholar]
- 111.Katz JN, Fossel KK, Simmons BP, Swartz RA, Fossel AH, Koris MJ. Symptoms, functional status, and neuromuscular impairment following carpal tunnel release. J Hand Surg [Am] 1995;20(4):549–55. doi: 10.1016/S0363-5023(05)80265-5. [DOI] [PubMed] [Google Scholar]
- 112.Seradge H, Seradge E. Piso-triquetral pain syndrome after carpal tunnel release. J Hand Surg [Am] 1989;14(5):858–62. doi: 10.1016/s0363-5023(89)80090-5. [DOI] [PubMed] [Google Scholar]
- 113.Ludlow KS, Merla JL, Cox JA, Hurst LN. Pillar pain as a postoperative complication of carpal tunnel release: a review of the literature. J Hand Ther. 1997;10(4):277–82. doi: 10.1016/s0894-1130(97)80042-7. [DOI] [PubMed] [Google Scholar]
- 114.Wilson KM. Double incision open technique for carpal tunnel release: an alternative to endoscopic release. J Hand Surg [Am] 1994;19(6):907–12. doi: 10.1016/0363-5023(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 115.Hunter JM. Recurrent carpal tunnel syndrome, epineural fibrous fixation, and traction neuropathy. Hand Clin. 1991;7(3):491–504. [PubMed] [Google Scholar]
- 116.Atik TL, Smith B, Baratz ME. Risk of neurovascular injury with limited-open carpal tunnel release: defining the “safe-zone”. J Hand Surg [Br] 2001;26(5):484–7. doi: 10.1054/jhsb.2001.0583. [DOI] [PubMed] [Google Scholar]
- 117.Jimenez DF, Gibbs SR, Clapper AT. Endoscopic treatment of carpal tunnel syndrome: a critical review. J Neurosurg. 1998;88(5):817–26. doi: 10.3171/jns.1998.88.5.0817. [DOI] [PubMed] [Google Scholar]
- 118.Wang AA, Hutchinson DT, Vanderhooft JE. Bilateral simultaneous open carpal tunnel release: a prospective study of postoperative activities of daily living and patient satisfaction. J Hand Surg [Am] 2003;28(5):845–8. doi: 10.1016/s0363-5023(03)00257-0. [DOI] [PubMed] [Google Scholar]
- 119.Okutsu I, Ninomiya S, Takatori Y, Ugawa Y. Endoscopic management of carpal tunnel syndrome. Arthroscopy. 1989;5(1):11–8. doi: 10.1016/0749-8063(89)90084-4. [DOI] [PubMed] [Google Scholar]
- 120.Chow JC. Endoscopic release of the carpal ligament: a new technique for carpal tunnel syndrome. Arthroscopy. 1989;5(1):19–24. doi: 10.1016/0749-8063(89)90085-6. [DOI] [PubMed] [Google Scholar]
- 121.Agee JM, McCarroll HR, Jr., Tortosa RD, Berry DA, Szabo RM, Peimer CA. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg [Am] 1992;17(6):987–95. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 122.Scholten RJ, Gerritsen AA, Uitdehaag BM, van Geldere D, de Vet HC, Bouter LM. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2004;4 doi: 10.1002/14651858.CD003905.pub2. CD003905. [DOI] [PubMed] [Google Scholar]
- 123.Thoma A, Veltri K, Haines T, Duku E. A systematic review of reviews comparing the effectiveness of endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;113(4):1184–91. doi: 10.1097/01.prs.0000110202.08818.c1. [DOI] [PubMed] [Google Scholar]
- 124.Dias JJ, Bhowal B, Wildin CJ, Thompson JR. Assessing the outcome of disorders of the hand. Is the patient evaluation measure reliable, valid, responsive and without bias? J Bone Joint Surg Br. 2001;83(2):235–40. doi: 10.1302/0301-620x.83b2.10838. [DOI] [PubMed] [Google Scholar]
- 125.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 126.Derogatis LR, Lipman RS, Covi L, Rickels K. Factorial invariance of symptom dimensions in anxious and depressive neuroses. Arch Gen Psychiatry. 1972;27(5):659–65. doi: 10.1001/archpsyc.1972.01750290069013. [DOI] [PubMed] [Google Scholar]
- 127.Leite JC, Jerosch-Herold C, Song F. A systematic review of the psychometric properties of the Boston Carpal Tunnel Questionnaire. BMC Musculoskelet Disord. 2006;7:78. doi: 10.1186/1471-2474-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Schrijver HM, Gerritsen AA, Strijers RL, Uitdehaag BM, Scholten RJ, de Vet HC, et al. Correlating nerve conduction studies and clinical outcome measures on carpal tunnel syndrome: lessons from a randomized controlled trial. J Clin Neurophysiol. 2005;22(3):216–21. [PubMed] [Google Scholar]
- 129.Naidu SH, Fisher J, Heistand M, Kothari MJ. Median nerve function in patients undergoing carpal tunnel release: pre- and post-op nerve conductions. Electromyogr Clin Neurophysiol. 2003;43(7):393–7. [PubMed] [Google Scholar]
- 130.Radwin RG, Sesto ME, Zachary SV. Functional tests to quantify recovery following carpal tunnel release. J Bone Joint Surg Am. 2004;86-A(12):2614–20. doi: 10.2106/00004623-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 131.Jeng OJ, Radwin RG, Rodriquez AA. Functional psychomotor deficits associated with carpal tunnel syndrome. Ergonomics. 1994;37(6):1055–69. doi: 10.1080/00140139408963718. [DOI] [PubMed] [Google Scholar]
- 132.Radwin RG, Wertsch JJ, Jeng OJ, Casanova J. Ridge detection tactility deficits associated with carpal tunnel syndrome. J Occup Med. 1991;33(6):730–6. doi: 10.1097/00043764-199106000-00016. [DOI] [PubMed] [Google Scholar]
- 133.Jerosch-Herold C, Leite JC, Song F. A systematic review of outcomes assessed in randomized controlled trials of surgical interventions for carpal tunnel syndrome using the International Classification of Functioning, Disability and Health (ICF) as a reference tool. BMC Musculoskelet Disord. 2006;7:96. doi: 10.1186/1471-2474-7-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gummesson C, Atroshi I, Ekdahl C. The quality of reporting and outcome measures in randomized clinical trials related to upper-extremity disorders. J Hand Surg [Am] 2004;29(4):727–34. doi: 10.1016/j.jhsa.2004.04.003. discussion 735–7. [DOI] [PubMed] [Google Scholar]
- 135.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–92. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]


