Abstract
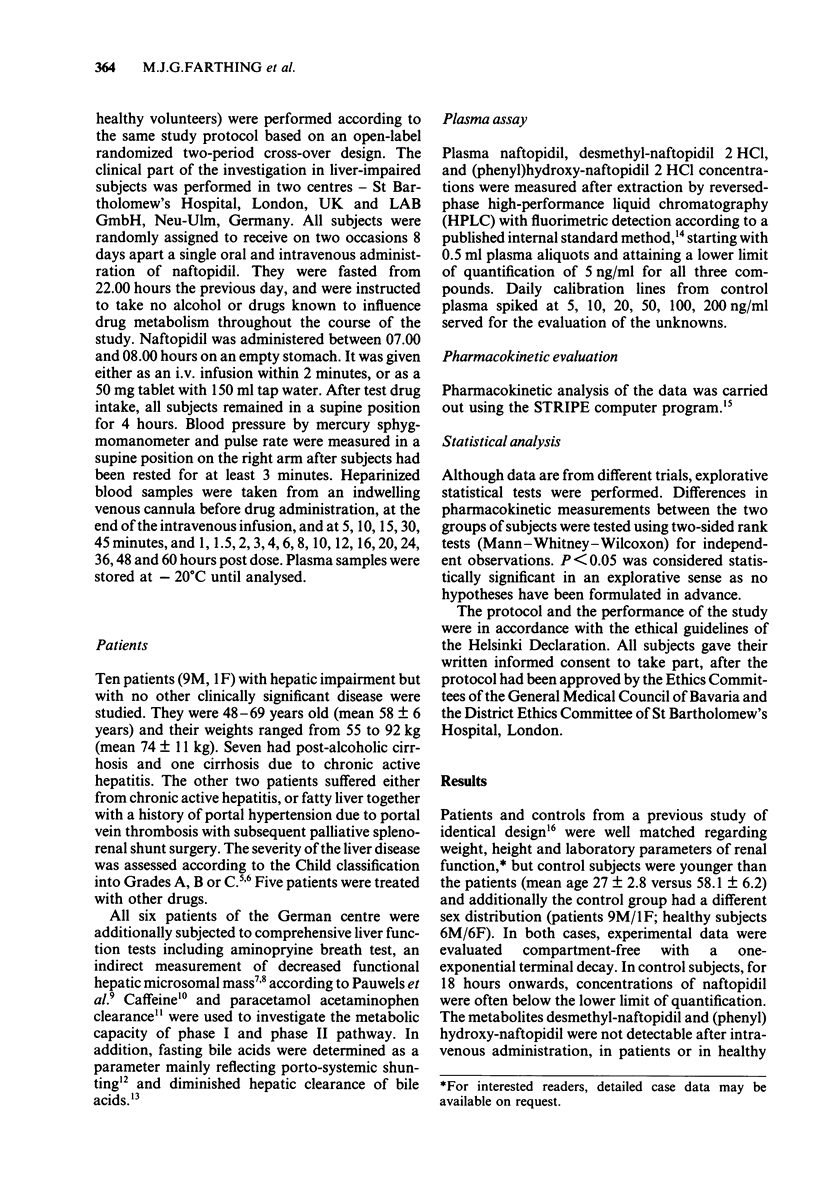
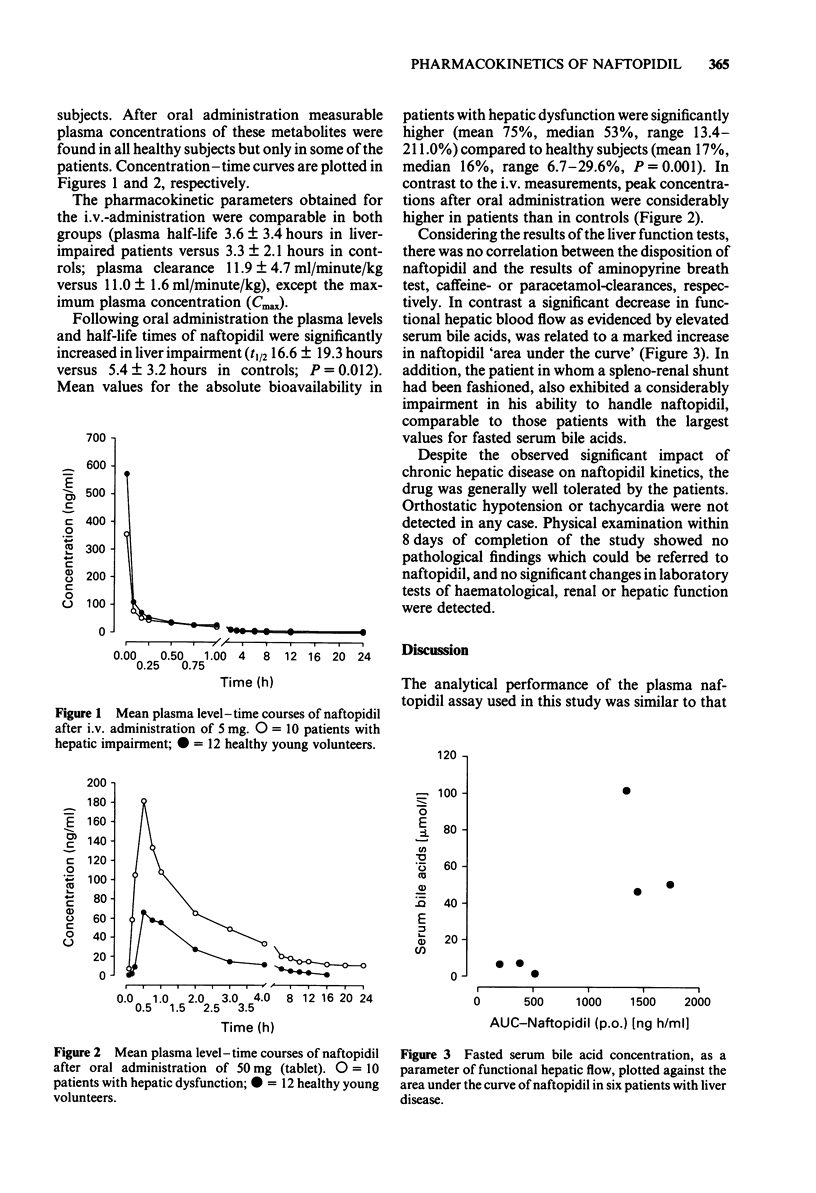
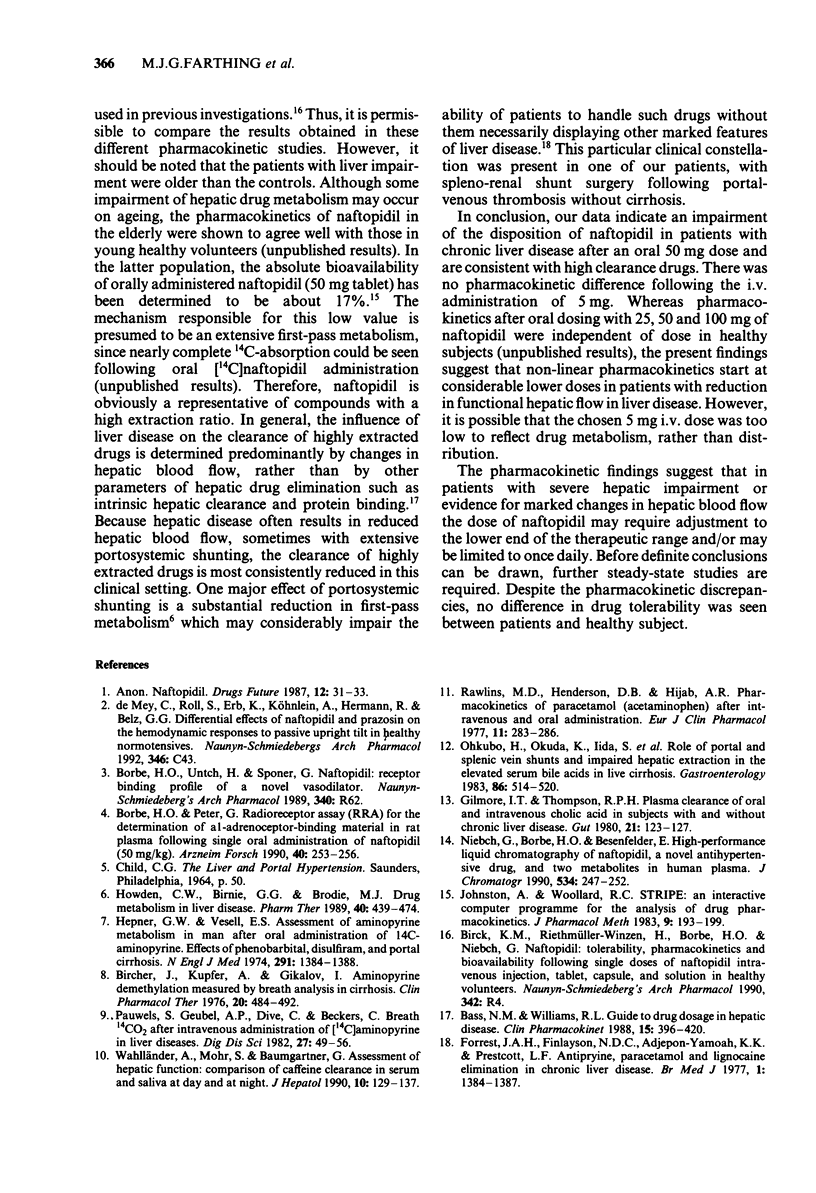
The pharmacokinetics of naftopidil, a novel alpha-1 adrenoceptor-blocking antihypertensive, were investigated in ten patients (9M/1F) with hepatic dysfunction after oral administration (50 mg, tablet) and after an intravenous infusion of 5.0 mg over 2 minutes. Results were compared to a control group of 12 healthy subjects (6M/6F) of a previous investigation, which was carried out according to the identical study protocol. The pharmacokinetic parameters obtained for the i.v. administration were comparable in both groups (half life 3.6 +/- 3.4 hours in liver-impaired subjects versus 3.3 +/- 2.1 hours in controls; clearance 11.9 +/- 4.7 ml/minute/kg versus 11.0 +/- 1.6 ml/minute/kg). Following oral administration the plasma levels and half-life times of naftopidil were significantly increased in liver impairment (t1/2 16.6 +/- 19.3 hours versus 5.4 +/- 3.2 hours in controls; P = 0.012). Mean values for the absolute bioavailability in patients with hepatic dysfunction were significantly higher (mean 75%, median 53%, range 13.4-211.0%) compared to healthy subjects (mean 17%, median 16%, range 6.7-29.6%, P = 0.001). Reduction of functional hepatic blood flow in chronic liver disease or, as evidenced in one case as a consequence of shunt surgery, is the probable cause of the observed alteration in naftopidil kinetics. This phenomenon occurred only following the oral 50 mg dose whereas the intravenous 5 mg dose obviously still could be normally handled. Naftopidil demethylation and hydroxylation were both less and non-uniformly affected. The pharmacokinetic findings suggest that in patients with severe hepatic impairment or evidence for marked changes in hepatic blood flow the dose of naftopidil may require adjustment to the lower end of the therapeutic range and/or may be limited to once daily. However, before definite conclusions can be drawn, further steady-state studies are required. Despite the pharmacokinetic discrepancies no difference in drug tolerability was seen between patients and healthy subjects.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bass N. M., Williams R. L. Guide to drug dosage in hepatic disease. Clin Pharmacokinet. 1988 Dec;15(6):396–420. doi: 10.2165/00003088-198815060-00004. [DOI] [PubMed] [Google Scholar]
- Bircher J., Küpfer A., Gikalov I., Preisig R. Aminopyrine demethylation measured by breath analysis in cirrhosis. Clin Pharmacol Ther. 1976 Oct;20(4):484–492. doi: 10.1002/cpt1976204484. [DOI] [PubMed] [Google Scholar]
- Borbe H. O., Peter G. Radioreceptor assay for the determination of alpha 1-adrenoceptor-binding material in rat plasma following single oral administration of naftopidil. Arzneimittelforschung. 1990 Mar;40(3):253–256. [PubMed] [Google Scholar]
- Forrest J. A., Finlayson N. D., Adjepon-Yamoah K. K., Prescott L. F. Antipyrine, paracetamol, and lignocaine elimination in chronic liver disease. Br Med J. 1977 May 28;1(6073):1384–1387. doi: 10.1136/bmj.1.6073.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmore I. T., Thompson R. P. Plasma clearance of oral and intravenous cholic acid in subjects with and without chronic liver disease. Gut. 1980 Feb;21(2):123–127. doi: 10.1136/gut.21.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepner G. W., Vesell E. S. Assessment of aminopyrine metabolism in man by breath analysis after oral administration of 14C-aminopyrine. Effects of phenobarbital, disulfiram and portal cirrhosis. N Engl J Med. 1974 Dec 26;291(26):1384–1388. doi: 10.1056/NEJM197412262912605. [DOI] [PubMed] [Google Scholar]
- Johnston A., Woollard R. C. STRIPE: an interactive computer program for the analysis of drug pharmacokinetics. J Pharmacol Methods. 1983 May;9(3):193–199. doi: 10.1016/0160-5402(83)90038-4. [DOI] [PubMed] [Google Scholar]
- Niebch G., Borbe H. O., Besenfelder E. High-performance liquid chromatography of naftopidil, a novel antihypertensive drug, and two metabolites in human plasma. J Chromatogr. 1990 Dec 14;534:247–252. doi: 10.1016/s0378-4347(00)82170-2. [DOI] [PubMed] [Google Scholar]
- Ohkubo H., Okuda K., Iida S., Ohnishi K., Ikawa S., Makino I. Role of portal and splenic vein shunts and impaired hepatic extraction in the elevated serum bile acids in liver cirrhosis. Gastroenterology. 1984 Mar;86(3):514–520. [PubMed] [Google Scholar]
- Pauwels S., Geubel A. P., Dive C., Beckers C. Breath 14CO2 after intravenous administration of [14C]aminopyrine in liver diseases. Dig Dis Sci. 1982 Jan;27(1):49–56. doi: 10.1007/BF01308121. [DOI] [PubMed] [Google Scholar]
- Rawlins M. D., Henderson D. B., Hijab A. R. Pharmacokinetics of paracetamol (acetaminophen) after intravenous and oral administration. Eur J Clin Pharmacol. 1977 Apr 20;11(4):283–286. doi: 10.1007/BF00607678. [DOI] [PubMed] [Google Scholar]
- Wahlländer A., Mohr S., Paumgartner G. Assessment of hepatic function. Comparison of caffeine clearance in serum and saliva during the day and at night. J Hepatol. 1990 Mar;10(2):129–137. doi: 10.1016/0168-8278(90)90041-o. [DOI] [PubMed] [Google Scholar]



