Abstract
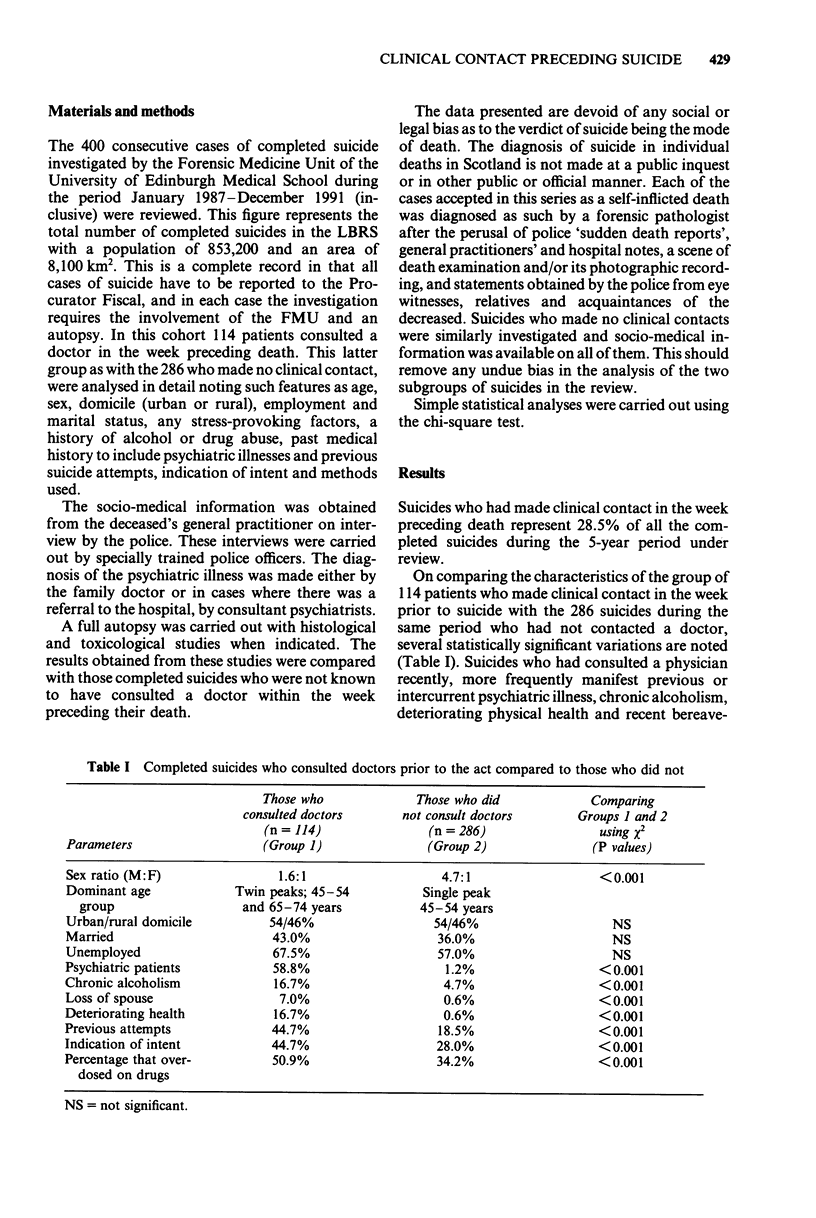
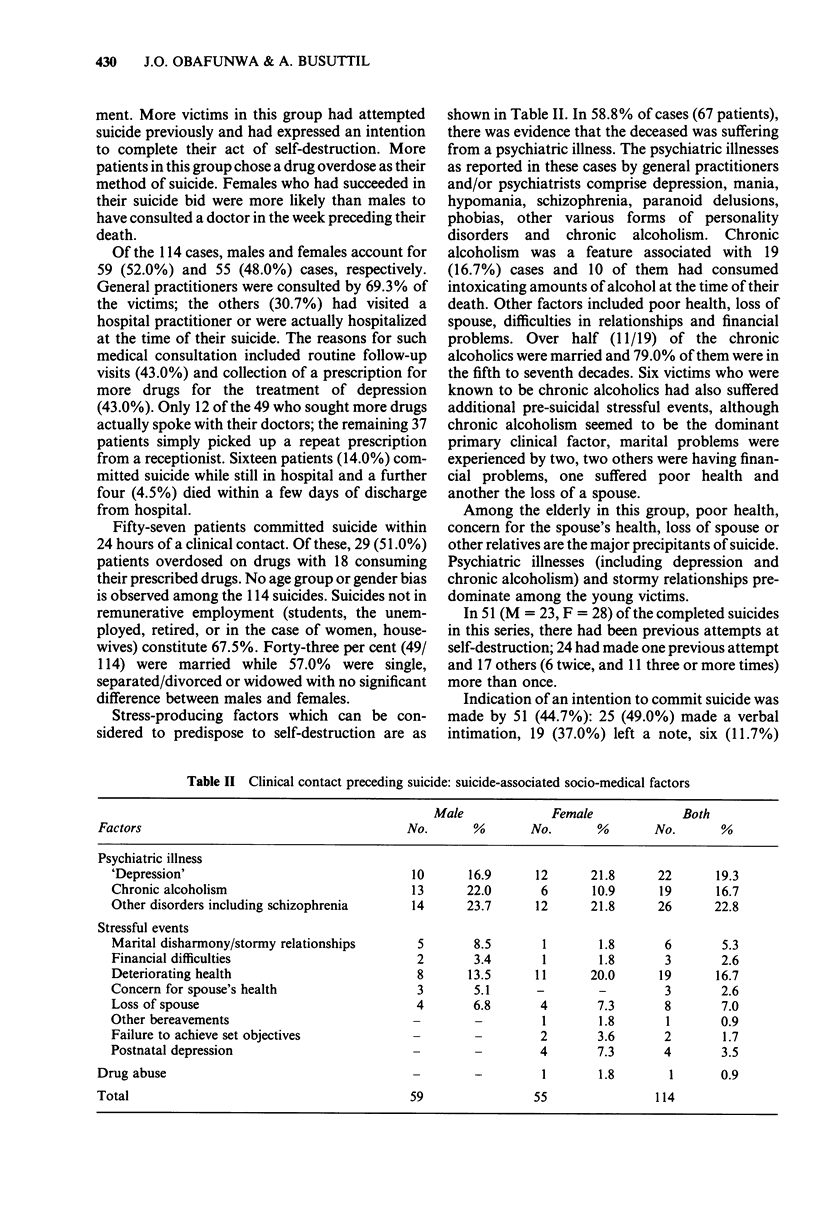
Of the 400 consecutive completed suicides investigated over a 5-year period, 114 (28.5%) who had consulted a doctor in the week preceding death were specifically reviewed and compared with those who did not. The study comprised an analysis of the medical history, the scene of death and a complete autopsy with histological and toxicological examination and the identification of features which occurred more frequently in this group when compared with other suicides not contacting their doctors. Suicide-associated factors include psychiatric illness (58.8%), deteriorating health (16.7%), and a loss of spouse (7.0%); all these features were manifested by this group of suicides more frequently than by those who made no clinical contact (P < 0.001). A pre-indication of suicidal intention was made by 45% of these patients. This feature, as with previous attempts, occurred more commonly in patients who consulted a doctor (P < 0.001). Drug overdose was the most common suicidal method chosen (50.9%) and anti-depressants predominated (35%); 78% of those who overdosed ingested prescribed drugs. Poisoning was more common in this group (P < 0.001). Half of the victims committed suicide within 24 hours following consultation; of these, 51% overdosed on drugs with 61% of them ingesting their prescribed drugs. Of these 114 cases, the final consultation in 43% was to collect more drugs. All suicidal threats should be taken seriously, and particular care should be taken in prescribing and dispensing medication which may be fatal in overdose.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barraclough B., Bunch J., Nelson B., Sainsbury P. A hundred cases of suicide: clinical aspects. Br J Psychiatry. 1974 Oct;125(0):355–373. doi: 10.1192/bjp.125.4.355. [DOI] [PubMed] [Google Scholar]
- Crombie I. K. Trends in suicide and unemployment in Scotland, 1976-86. BMJ. 1989 Mar 25;298(6676):782–784. doi: 10.1136/bmj.298.6676.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein R. B., Black D. W., Nasrallah A., Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Arch Gen Psychiatry. 1991 May;48(5):418–422. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- Nordentoft M., Breum L., Munck L. K., Nordestgaard A. G., Hunding A., Laursen Bjaeldager P. A. High mortality by natural and unnatural causes: a 10 year follow up study of patients admitted to a poisoning treatment centre after suicide attempts. BMJ. 1993 Jun 19;306(6893):1637–1641. doi: 10.1136/bmj.306.6893.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ROBINS E., MURPHY G. E., WILKINSON R. H., Jr, GASSNER S., KAYES J. Some clinical considerations in the prevention of suicide based on a study of 134 successful suicides. Am J Public Health Nations Health. 1959 Jul;49(7):888–899. doi: 10.2105/ajph.49.7.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutz W., von Knorring L., Wålinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand. 1989 Aug;80(2):151–154. doi: 10.1111/j.1600-0447.1989.tb01318.x. [DOI] [PubMed] [Google Scholar]
- Squires T. J., Busuttil A. Elderly suicides in the Lothian and borders region of Scotland, 1983-1988. Med Sci Law. 1991 Apr;31(2):137–146. doi: 10.1177/002580249103100209. [DOI] [PubMed] [Google Scholar]
- Winokur G., Black D. W. Suicide--what can be done? N Engl J Med. 1992 Aug 13;327(7):490–491. doi: 10.1056/NEJM199208133270710. [DOI] [PubMed] [Google Scholar]



