Abstract
Background:
Behavior change is integral to the prevention and treatment of many disorders associated with deleterious lifestyles. Rigorous scientific testing of behavior change interventions is an important goal for nursing research.
Approach:
The stage model for behavioral therapy development is recommended as a useful framework for evaluating behavior change strategies. The NIH model specifies three stages from initial testing of novel behavioral therapies to their dissemination in community settings. Definitions of each step in a Stage I trial and a case example of Mindfulness-Based Stress Reduction (MBSR) in therapeutic community treatment are provided.
Results:
It is feasible to adapt a behavioral therapy such as MBSR using the stage model framework. Steps in the process include: (a) determining pilot study design and describing the population; (b) modifying the intervention and developing the manual; (c) training the teachers; (d) implementing a pilot study; and (e) monitoring treatment integrity.
Discussion:
The development of behavior therapies requires the same scientific rigor used in pharmacotherapy research. Stage I of the model enables consideration of the “dose” of a behavioral intervention necessary to achieve behavior change in a defined population. The stage model offers an excellent approach to achieving rigor in a variety of potentially useful therapies of interest to nurse researchers.
Keywords: behavior change intervention, mindfulness-based stress reduction, substance abuse treatment, therapeutic community
Behavior change is integral to the prevention and treatment of the many disorders caused, or compounded, by deleterious lifestyles or risky behaviors. Conditions such as obesity, hypertension, diabetes, and substance abuse are examples of health problems that generally require behavior change. Discovering therapies that enhance and support behavior change is an important goal for nursing research. One advance in behavioral therapies research over the past 3 decades comes from the substance abuse field: the development of a conceptual framework and the necessary structure to evaluate behavioral therapies with the same scientific rigor used in pharmacotherapy trials. This framework, the stage model, established by the National Institute of Drug Abuse and now recognized by other institutes, specifies the stages from initial testing of novel behavioral therapies to their dissemination in community settings. The three stages of the model are depicted in Table 1.
TABLE 1.
The Stage Model of Behavioral Therapies Development
| Stage I | Pilot and feasibility testing of new treatments involving manual preparation, therapist training protocols, and treatment integrity procedures. |
| Stage II | Efficacy testing of promising fully developed treatments. |
| Stage III | Effectiveness testing of treatments in community settings involving issues of transportability, implementation, and acceptability (Carroll & Onken, 2005). |
There is a growing body of literature to support the utility of the stage model in the development of behavioral therapies such as contingency management, cognitive behavioral therapy, couples and family therapy, and motivational interviewing (Carroll & Onken, 2005). Behavioral therapy platforms, used alone or in combination, are required to support pharmacotherapy trials for substance use (Carroll, Kosten, & Rounsaville, 2004). The primary purpose of this report is to describe the stage model as a method for behavioral therapies research, focusing on the critical first stage, therapy development. Application of the model will be illustrated with a case example, the process of standardizing mindfulness-based stress reduction (MBSR) for substance abuse treatment in a therapeutic community.
The Stage I Trial
As with the testing of new medications, the central goal for behavioral therapies trials is formal efficacy and safety testing, usually in a randomized control trial (RCT). Efficacy must be established before the therapy can be considered for application in different populations and settings. The stage model, however, takes into consideration the fact that behavioral therapies trials do not begin and end with the RCT, the designated goal of Stage II. The model defines an orderly progression of studies from feasibility (Stage I) to efficacy (Stage II) to transportability (Stage III; Carroll & Onken, 2005; Rounsaville & Carroll, 2001; Table 1). Stage I, the focus of this presentation, is the creative first step in the process. Stage I studies permit researchers to generate new therapies, or adapt existing ones, often based on clinical observations of behavior change or on principles of neuroscience (Carroll & Onken, 2005). Stage I studies specify the theoretical rationale for the therapy, hypothesizing how the therapy might be expected to influence the change process. The rationale must be logical and consistent with principles of behavioral science.
There are two phases of this stage, a development and a testing phase: (a) Stage Ia, development, includes writing the manual, identifying the target population, establishing training and monitoring procedures for therapists, and selecting appropriate outcome measures to capture anticipated behavior change; and (b) Stage Ib, testing, involves conducting a pilot study of the nearly completed new therapy (Rounsaville & Carroll, 2001). The pilot study is conducted to determine: (a) patient acceptance of the new therapy; (b) the researcher's ability to recruit the target population; (c) feasibility of delivering the therapy under proposed conditions; (d) clinically significant change in patient outcomes; and (e) the sample size needed to contrast the new therapy with a comparison group in a larger Stage II trial (Rounsaville & Carroll, 2001). The data from a Stage I trial contribute to consideration of the “dose” of behavioral therapy necessary to affect change.
Designing the pilot study for a Stage I trial can be complex and challenging. Standard behavioral comparison groups do not exist in the same precise manner as does placebo treatment used in pharmacological trials. Hence, a variety of control group situations have been used in Stage Ib pilot trials: no treatment or wait list controls; treatment as usual; historical controls; and an active reference condition. The choice of a comparison group depends on the type of treatment being evaluated and the research questions being addressed (Rounsaville & Carroll, 2001). Essentially, the two objectives of a Stage I study are to: (a) define the critical elements of a new behavioral treatment; and (b) pilot-test the treatment before proceeding to formal efficacy testing in Stage II. A case example, MBSR in therapeutic community treatment, follows. A brief overview of MBSR and therapeutic community treatment is presented to enable understanding of each and to clarify the rationale for the study.
Approach and Application
Therapeutic Communities
Therapeutic communities play an important role in the treatment of substance use disorders. These therapeutic communities offer a unique approach: a highly structured environment in which the community is the key agent for behavior change. The major goal of the therapeutic community is to encourage and support social learning, which fosters changes in behavior and attitude and the more elusive phenomenon of change in world view and self-image (De Leon, 2000). Studies have shown that individuals who complete therapeutic community treatment have lower levels of substance use, criminal behavior, unemployment, and depression than they had prior to treatment (Martin, Butzin, Saum, & Inciardi, 1999; Simpson, Joe, & Brown, 1997; Simpson, Joe, Fletcher, Hubbard, & Anglin, 1999; Wexler, Melnick, Lower, & Peters, 1999).
For individuals whose lives have been characterized by impulsiveness and lack of self-control, therapeutic community treatment is restrictive and intrinsically stressful, an arduous process described by residents as requiring unique strategies to cope with recovery in this long-term residential setting (Marcus, 1998). The dropout rate is significant, often as high as 50%, with attrition highest within the first 30 to 60 days (De Leon, Hawke, Jainchill, & Melnick, 2000). Research has shown that stress is associated with initiation of substance use in vulnerable individuals and with relapse following abstinence (Sinha, 2001). Given that successful outcomes for therapeutic communities are correlated highly with time in treatment (De Leon et al., 2000; Fals-Stewart & Schafer, 1992; Toumbourou, Hamilton, & Fallon, 1998), adding stress reduction techniques to the therapeutic community curriculum may assist clients in managing the inherently stressful environment and prevent attrition.
Mindfulness-Based Stress Reduction
A number of studies document the potential utility of MBSR in reducing stress in a variety of clinical and non-clinical populations (Bishop, 2002). It is a specific meditation program founded in 1979 by Jon Kabat-Zinn at the University of Massachusetts (Kabat-Zinn, 1990). The 8-week program is designed to help participants foster the skill of bringing nonjudgmental attention to their present-moment experience. Originally designed to teach patients with chronic physical and mental problems how to improve their health and lives, MBSR is now being used as an adjunct to treatment in a wide range of disorders. With the exception of prior studies by the current authors (Marcus, Fine, & Kouzekanani, 2001; Marcus et al., 2003), there are no reports of MBSR with clients in recovery from substance use disorders in therapeutic community treatment. Yet, MBSR holds particular promise for clients in this setting because it is a generic approach to stress reduction focusing on commonalities among individuals, emphasizing common human experiences such as breathing, proprioception, thoughts, and emotions.
Moreover, consistent with the therapeutic community treatment modality, MBSR encourages the practitioner to see the self as a whole person rather than as an illness or affliction, identifying what is right rather than what may be wrong. Mindfulness-based stress reduction emphasizes seeing one's situation as it is, not trying to fix it but working with and accepting the complex situation of the moment (Salmon, Santorelli, & Kabat-Zinn, 1998). This is a major attitudinal shift for those who have continually tried to change their circumstances, particularly those who have used psychoactive substances to alter those circumstances, an attitudinal shift that is also at the core of the therapeutic community philosophy of right living. Recognizing the congruence between MBSR and the therapeutic community philosophy, a Stage I trial was designed to standardize MBSR for therapeutic community treatment and to pilot-test the effect on stress, progression through treatment, global and internalized self-change, and retention in a therapeutic community.
The study fits the criteria for a Stage I trial because it allows adaptation of an existing behavioral therapy, MBSR, to improve or enhance a standard modality, therapeutic community treatment. The goal of the approach is to structure the intervention (MBSR) in a way that is feasible and meaningful for the setting; it is also important to assure that the intervention is delivered consistently so that it can be replicated in other settings. The exemplar study was designed in two phases: Stage Ia, determining a pilot study design, describing the population in the standard modality (therapeutic community treatment), modifying the intervention, developing the manual, and training the teachers; and Stage Ib, implementing a pilot study of MBSR as an adjunct to therapeutic community curriculum, monitoring treatment integrity, and comparing control and intervention data. The study was approved by the institutional review board of the university. Each phase of Stage I trials will be illustrated through use of the MBSR–therapeutic community case example.
Determining Pilot Study Design and Describing the Population
A basic tenet of therapeutic community treatment is that the community is part of the method; each resident is expected to observe and report on the behaviors of fellow residents, making a randomized control trial impractical in this setting. Other options, including a treatment-as-usual comparison group at another facility, were considered. However, it was difficult to find another treatment facility with a comparable population. After weighing the advantages and disadvantages of other study designs, a historical control was selected. During Stage Ia, data were collected on study variables to describe the target population, individuals receiving standard therapeutic community treatment, for later comparison with responses of individuals receiving MBSR in addition to standard therapeutic community treatment. Study variables included measures of stress, global self-change, internalized self-change, progression through the therapeutic community, and retention. These data were collected at five time points: on admission; and then at the first, third, sixth, and ninth months of therapeutic community treatment. The measures used to address the study variables are listed in Table 2.
TABLE 2.
Measuring Study Variables: Stress, Change, Progression
| Measures | Properties of Measures |
|---|---|
| Measures of Stress | |
| Salivary Cortisol | 0, 30, 45, 60 minutes after awakening |
| Perceived Stress Scale (PSS) (Cohen, Kamerk, & Mermelstein 1983) | 10 items |
| Symptoms of Stress Inventory (SOSI) (Leckie & Thompson, 1979) | 10 subscales, measures physical, psychological, behavioral response to stress |
| Measures of Global Self-Change | Measure client response to TC along four broad categories: developmental, socialization, psychological, community membership |
| Client Assessment Inventory (CAI) | |
| Client Assessment Summary (CAS) | |
| Staff Assessment Summary (SAS) (Kressel et al., 2000) | |
| Measure of Internalized Self Change | Participants asked to write about stress for 15 minutes |
| Written Narrative | |
| Word use analyzed with Linguistic Inquiry and Word Count (LIWC) software (Pennebaker, Francis, & Booth, 2001) |
|
| Measure of Progression | TC participants receive points toward program completion in six categories: (a) individual counseling; (b) behavior; (c) job responsibility; (d) education; (e) social skills; (f) physical fitness |
| TC Treatment Point System |
Note. TC = therapeutic community.
Modifying the Intervention and Developing the Manual
Further Stage Ia goals were to align the MBSR program with the orientation curriculum of the therapeutic community and to develop a plan to integrate it into the critical early stage of treatment when attrition is generally highest. The therapeutic community orientation curriculum consists of rules and tools for right living emphasizing four dimensions for client change: developmental, socialization, psychological, and community member (Kressel, DeLeon, Palij, & Rubin, 2000). Although MBSR is a generic stress reduction program, it is congruent with these therapeutic community change dimensions, particularly as they relate to self-regulation, awareness, insight, problem-solving, and sense of well-being. The usual MBSR manual outlines eight sessions as described in Kabat-Zinn's (1990) original work and adapted by Segal, Williams, and Teasdale (2002). The manual specifies each step in the delivery of the intervention. Each session has a theme, a proposed sequence of activities, and a list of classroom resources and participant handouts. A variety of meditative activities is offered so that individuals of varying temperaments may find aspects of the program that are compatible with their personal learning style (Salmon et al., 1998). The practices include: mindful movement and the body scan; mindful eating; seeing and hearing meditation; sitting meditation; and walking meditation.
Adapting MBSR to the therapeutic community setting called for changes in delivery format and content. Session duration was increased to 3 hours and the number of sessions was reduced from eight to six so that classes could be completed within the orientation phase of the therapeutic community treatment. Moreover, MBSR session themes had to be arranged in an order that corresponded with the presentation of therapeutic community concepts or maxims. An outline of the resulting six-session MBSR program integrated with the therapeutic community program is shown in Table 3. The six-session MBSR therapeutic community manual was completed during Stage Ia. However, development of the manual progressed over the entire course of the Stage I trial. The original was contextualized over the course of implementation in Stage Ib so that participant response guided continuing manual development.
TABLE 3.
Mindfulness-Based Meditation Classes Aligned With Therapeutic Community Concepts
| Class | Theme | Therapeutic Community Concepts | |
|---|---|---|---|
| Session I | Introduction to Mindfulness—Reawakening to Life | Reducing the tendency to operate on automatic pilot, becoming awake | MBSR as a tool for treatment Right living is being in the personal present, the here and now “To be awake is to be alive” |
| Session II | Perceptions and Their Effect on the Ability to Respond Creatively | The universality of the wandering mind, how thoughts influence experience, sense of community | “Keep it simple” or focusing on one thing at a time. “Letting go” Community as method |
| Session III | Cultivating a Sense of Wonder and Appreciation in Life Through Mindfulness | Bringing awareness to the sense of wonder developed through being present to our experience | “You get back what you put in” or focusing on participating fully in the therapeutic community |
| Session IV | Stress Reactivity and Opportunities for Responding Differently | Noticing how the body responds to stress, how thoughts affect stress reactions and behaviors, and how to handle stress | “Remember who you are” or remembering the basic goodness and potential of one's inner self in coping with stresses |
| Session V | Allowing and Letting Be—Handling Emotions with Mindfulness | Befriending one's emotions and handling them in a different way, acceptance | “It's better to understand than to be understood” or learning by listening and accepting others |
| Session VI | Making the Practice Your Own | Emphasizing the importance of taking responsibility for one's own mindfulness practice | “No gain without pain” or anything worth having is worth working for (De Leon, 2000; Kabat-Zinn, 1990; Segal et al., 2002) |
Note. MBSR = mindfulness-based stress reduction.
Training the Teachers
Training teachers or therapists to deliver a standardized intervention is a key feature of behavioral therapy trials. There is empirical evidence to suggest that competence prior to training predicts competence in the training phase (Henry, Schacht, Strupp, Butler, & Binder, 1993; Rounsaville, Chevron, Weissman, Prusoff, & Frank, 1986; Siqueland et al., 2000). Hence, a long-term personal practice of mindfulness meditation was considered to be a critical attribute for teachers in this study. In addition, each of the teachers completed the 7-day intensive training program for health professionals offered by the Center for Mindfulness, University of Massachusetts Medical School. Further teacher preparation included 6 hours of training on the therapeutic community method, a thorough orientation to the use of the manual, and a 6-week internship during which they observed and participated while an experienced, certified MBSR teacher conducted the first series of classes in the intervention phase of the study. Each class during the observation period was followed by a 2-hour review of class activities. Once the teachers began conducting their own classes, they continued to meet weekly, individually and as a group, with the certified teacher to discuss their experiences and receive supervision. Therefore, training was an ongoing process requiring thoughtful attention during the intervention phase of the trial.
Implementing a Pilot Study
The primary purpose of Stage Ib for the case example was to pilot-test the addition of MBSR to standard therapeutic community treatment. The individuals admitted to the therapeutic community during Stage Ib were given an opportunity to participate in the study which, in this phase, included the MBSR intervention. New MBSR sessions were initiated every 2 weeks. In addition to class attendance, participants were encouraged to practice meditation 6 days a week and to independently complete homework exercises. Workbooks and audio compact discs were provided for the written exercises and for guiding meditation practice, respectively. Space was designated within the therapeutic community to accommodate meditation practice. Participants were asked to maintain a log to track the amount of time spent in formal meditation practice. At the end of the MBSR class series, the participants were asked to evaluate the experience and its contribution to recovery in the therapeutic community setting. Data collection in this stage of the study included the same assessment battery and administration time schedule as described for the historical controls in Stage Ia.
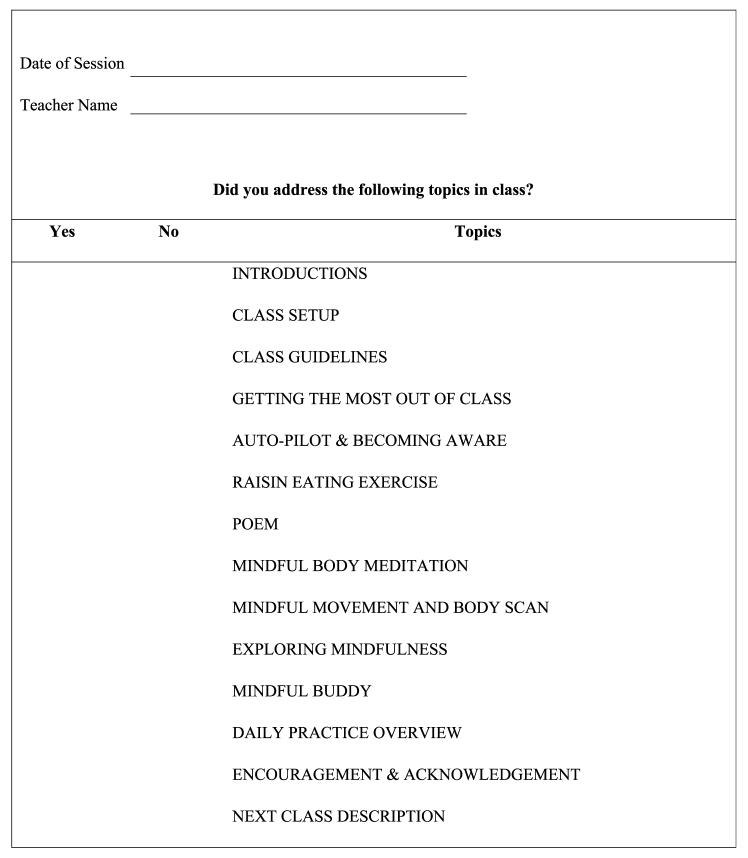
Monitoring Treatment Integrity
Treatment integrity, or fidelity, is critical to maintaining the internal and external validity of the research (Resnick et al., 2005). Internal validity is compromised if the intervention does not adhere to the designated protocol. Without a standardized protocol, the intervention cannot be replicated, which reduces external validity (Resnick et al., 2005). The Yale Adherence and Competence Scale (YACS; Carroll et al., 2000) was used as a guide to establish the treatment integrity plan and to design an appropriate checklist for the specific intervention activities. The YACS allows rating of both general and unique elements of behavioral treatments for drug use disorders. The items are scored for both adherence (how much each component of the treatment occurred in the session) and competence (how well the therapist delivered the treatment). All MBSR classes were audiotaped, and the checklists were used by two independent reviewers to identify potential discrepancies in delivery of the intervention protocol. A version of the checklist was completed by the MBSR teachers after each class, providing a regular reminder, or adherence prompt, of the specified elements of the session. These checklists were used in weekly supervisory sessions with the certified MBSR teacher. An example of one of the checklists used by the teachers to address the content covered in the session is provided in Figure 1.
FIGURE 1.
Mindfulness-Based Stress Reduction Teacher Checklist (Session 1).
Comparing Control and Intervention Data
The final step in Stage I of a behavioral therapy trial is to evaluate the effects of the intervention on selected outcome variables. In this case example, the intervention was MBSR and the outcome variables included stress, global self-change, internalized self-change, progression, and retention in the therapeutic community. When data collection is complete, changes in the outcome variables during the MBSR condition will be compared to changes in the historical control condition.
Discussion
In this paper, an application of Stage I of a behavioral therapies trial to develop and evaluate MBSR therapy for a TC treatment setting is described. The trial methods included careful selection of study design and definition of the target population; creation of a manual or protocol defining each treatment session; comprehensive teacher training methods, including a thorough plan for monitoring teacher competence and manual adherence; and implementation of a pilot study. These methods will enable consideration of the dose of behavioral intervention necessary to facilitate change in the defined population. Evaluation of both dose and effectiveness of the therapy must rely on skilled, consistent delivery of the intervention. Only then is it possible for the research team to progress to a Stage II therapeutic community study with confidence in the study outcomes, and the variables identified as indicators of behavior change. For instance, if improved outcomes in the MBSR group are found in this Stage I trial, the next step might be a Stage II large-scale efficacy trial in one or multiple therapeutic community sites. A Stage III trial might involve testing the effectiveness of training therapeutic community staff to deliver MBSR as a standard component of treatment. The Stage I trial lays the groundwork for thorough investigation of the therapy in future research.
The stage model offers an excellent approach to achieving rigor in evaluating potentially useful behavioral therapies of interest to practicing nurses. Mindfulness-based stress reduction, other stress reduction programs, and educational interventions designed to assist individuals to engage in healthy lifestyle behaviors are but a few examples. The model is a means for exploring new ways to assist clients in changing behavior and for gathering scientific evidence on the effectiveness of current practice approaches that may not have been subjected to testing.
Acknowledgments
This research was funded by NIH/NIDA R01 DA017719, awarded to Dr. Marianne T. Marcus.
References
- Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64:71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Kosten TR, Rounsaville BJ. Choosing a behavioral therapy platform for pharmacotherapy of substance users. Drug and Alcohol Dependence. 2004;75:123–134. doi: 10.1016/j.drugalcdep.2004.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter T, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Onken LS. Behavioral therapies for drug abuse. American Journal of Psychiatry. 2005;162(8):1452–1460. doi: 10.1176/appi.ajp.162.8.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Kamerk T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- De Leon G. The therapeutic community: Theory, model, and method. Springer; New York: 2000. [Google Scholar]
- De Leon G, Hawke J, Jainchill N, Melnick G. Therapeutic communities: Enhancing retention in treatment using “Senior Professor” staff. Journal of Substance Abuse Treatment. 2000;19:375–382. doi: 10.1016/s0740-5472(00)00124-0. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Schafer J. The relationship between length of stay in drug-free therapeutic communities and neurocognitive functioning. Journal of Clinical Psychology. 1992;48(4):539–543. doi: 10.1002/1097-4679(199207)48:4<539::aid-jclp2270480416>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Henry WP, Schacht TE, Strupp HH, Butler SF, Binder JL. Effects of training in time-limited dynamic psychotherapy: Mediators of therapists' responses to training. Journal of Consulting and Clinical Psychology. 1993;61(3):441–447. doi: 10.1037//0022-006x.61.3.441. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. Dell Publishing; New York: 1990. [Google Scholar]
- Kressel D, De Leon G, Palij M, Rubin G. Measuring client clinical progress in therapeutic community treatment: The therapeutic community Client Assessment Inventory, Client Assessment Summary, and Staff Assessment Summary. Journal of Substance Abuse Treatment. 2000;19:267–272. doi: 10.1016/s0740-5472(00)00108-2. [DOI] [PubMed] [Google Scholar]
- Leckie MS, Thompson E. Symptoms of stress inventory. University of Washington; Seattle: 1979. [Google Scholar]
- Marcus MT. Changing careers: Becoming clean and sober in a therapeutic community. Qualitative Health Research. 1998;8(4):466–480. [Google Scholar]
- Marcus MT, Fine M, Kouzekanani K. Mindfulness-based meditation in a therapeutic community. Journal of Substance Use. 2001;5:305–311. [Google Scholar]
- Marcus MT, Fine M, Moeller FG, Khan MM, Pitts K, Liehr P. Changes in stress levels following mindfulness-based stress reduction in a therapeutic community. Addictive Disorders and Their Treatment. 2003;2:63–68. [Google Scholar]
- Martin SS, Butzin CA, Saum CA, Inciardi JA. Three year outcomes of the therapeutic community treatment for drug involved offenders in Delaware: From prison to work release to aftercare. The Prison Journal. 1999;79(3):294–320. [Google Scholar]
- Pennebaker JW, Francis ME, Booth RJ. Linguistic inquiry and word count (LIWC2001) Erlbaum; Mahwah, NJ: 2001. [Google Scholar]
- Resnick B, Inguito P, Orwig D, Yahiro JY, Hawkes W, Werner M, et al. Treatment fidelity in behavior change: A case example. Nursing Research. 2005;54:139–143. doi: 10.1097/00006199-200503000-00010. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM. A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science and Practice. 2001;8(2):133–142. [Google Scholar]
- Rounsaville BJ, Chevron ES, Weissman MM, Prusoff BA, Frank E. Training therapists to perform interpersonal psychotherapy in clinical trials. Comprehensive Psychiatry. 1986;27(4):364–371. doi: 10.1016/0010-440x(86)90012-x. [DOI] [PubMed] [Google Scholar]
- Salmon PG, Santorelli SF, Kabat-Zinn J. Intervention elements promoting adherence to mindfulness-based stress reduction programs in the clinical behavioral medicine setting. In: Shumaker SA, Schron EB, Ockene JK, McBee WL, editors. The handbook of health behavior change. 2nd ed. Springer; New York: 1998. pp. 239–266. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. The Guilford Press; New York: 2002. [Google Scholar]
- Simpson DD, Joe DW, Brown BS. Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive Behaviors. 1997;11:294–307. [Google Scholar]
- Simpson DD, Joe GW, Fletcher BW, Hubbard RL, Anglin MD. A national evaluation of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 1999;56:507–514. doi: 10.1001/archpsyc.56.6.507. [DOI] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology. 2001;158:343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Siqueland L, Crits-Christoph P, Barber JP, Butler SF, Thase M, Najavits L, et al. The role of therapists characteristics in training effects in cognitive, supportive–expressive, and drug counseling therapies for cocaine dependence. Journal of Psychotherapy Practice and Research. 2000;9:123–130. [PMC free article] [PubMed] [Google Scholar]
- Toumbourou JW, Hamilton M, Fallon B. Treatment level progress and time spent in treatment in the prediction of outcomes following drug-free therapeutic community treatment. Addiction. 1998;93(7):1051–1064. doi: 10.1046/j.1360-0443.1998.937105110.x. [DOI] [PubMed] [Google Scholar]
- Wexler HK, Melnick G, Lower L, Peters J. Three-year reincarnation outcomes of Amity in-prison therapeutic community and aftercare in California. The Prison Journal. 1999;79:321–336. [Google Scholar]