Abstract
There is recent evidence that acute coronary syndrome (ACS) patients with first time incident major depressive disorder (MDD) and those with recurrent MDD represent different subtypes among individuals with ACS and comorbid depression. However, few studies have examined whether or not these subtypes differ in coronary artery disease (CAD) severity. We assessed whether those with incident MDD (in-hospital MDD and negative for history of MDD) or recurrent MDD (in-hospital MDD and a positive history of MDD) differ in angiographically documented CAD severity. Within 1 week of admission for ACS, 88 patients completed a clinical interview to assess current and past diagnosis of MDD. CAD severity was assessed in all patients by coronary angiography. A hierarchical regression analysis showed that neither in-hospital MDD status, nor history of MDD were significant predictors of CAD severity, but the interaction term between in-hospital MDD status and history of MDD was a significant predictor of CAD severity, after controlling for age, sex and ethnicity. Follow-up analyses showed that patients with first-time, incident MDD had significantly more severe CAD compared to patients with recurrent MDD (p = 0.043). To conclude, our study adds to the growing evidence that patients with incident MDD should be considered as a clinically distinct subtype from those with recurrent MDD. Possible mechanisms for differing CAD severity by angiogram between these two subtypes are proposed and implications for prognosis and treatment are discussed.
Keywords: Acute Coronary Syndrome, Coronary Artery Disease, Myocardial Infarction, Angiogram, Incident Major Depressive Disorder, Recurrent Major Depressive Disorder
Extensive research has shown that comorbid major depressive disorder (MDD) after an acute coronary syndrome (ACS) event is an independent prognostic marker of increased morbidity and mortality (Barth et al., 2004; van Melle et al., 2004). About one in five ACS patients meets criteria for MDD (Thombs et al., 2006), and of these MDD patients, 50% or more have had depression symptoms in the past. Recent evidence suggests that patients who experience depression after ACS for the first time (incident depression) may represent a clinically distinct subtype when compared with depressed ACS patients who have had depressive symptoms in the past (recurrent depression).
The literature indicates that the extent to which comorbid MDD after ACS impacts future medical prognosis might be dependent on whether patients experience incident or recurrent depression. However, the evidence is mixed as to which group (incident or recurrent depression) is at greater ACS recurrence and/or mortality risk.
Lespérance et al. found that among patients with a positive history of MDD who were experiencing a recurrent episode of MDD assessed within one week of a myocardial infarction (MI), 40% died compared to 10% of those experiencing depression for the first time (incident MDD) at index MI (Lesperance et al., 1996). In a study of 526 post-ACS patients, a history of depression – present in 26.7% of all patients – was associated with significantly more frequent angina, greater physical limitation and worse quality of life after 7 months (Rumsfeld et al., 2003). However, this study provides limited prognostic information given that outcome measures neither include hard cardiovascular events nor data on mortality.
In contrast, two other studies have found that only first time incident depression at the time of hospitalization was predictive of future cardiac events or mortality, but a history of depression was not. Grace and colleagues studied 750 post-ACS patients and found that 5 year mortality was highest among patients with incident depressive symptoms (as assessed by self-report) at time of hospitalization, and lowest in patients with a history of depressive symptomatology and no increased co-morbid depressive symptoms(Grace et al., 2005). Recently, de Jonge et al reported similar findings for a psychiatric diagnosis of MDD in a sample of 468 post-MI patients: only patients with incident, but not those with recurrent MDD had an increased risk of second cardiovascular events across a mean follow-up of 2.5 years (de Jonge et al., 2006).
It is not known why co-morbid depressive symptoms and / or co-morbid MDD in post-ACS patients are associated with recurrent cardiovascular events and mortality. One explanation is that worse cardiovascular outcome in this population is due to more severe coronary artery disease (CAD). Typically, studies have found no relation between the severity of comorbid depressive symptoms at the time of ACS and various CAD severity markers, such as LVEF, Holter registration or angiography (Frasure-Smith et al., 1995; Ladwig et al., 1991; Strik et al., 2004). However, most studies employed distal measures of CAD – measurements of cardiac function such as ejection fraction or Killip Class - and did not make a distinction between patients with incident vs. recurrent depression.
One previous study of CAD severity in patients with coronary artery disease who had comorbid depression suggests that individuals with incident depression differ from those with a history of depression. In a sample of 39 recently diagnosed CAD patients who met criteria for MDD, those with a depression history had less severe CAD in comparison to those without a depression history (Freedland et al., 1992). CAD severity was assessed by direct visualization of coronary arteries via angiogram, recorded as the number of occluded coronary arteries (>50% stenosed). It seems that incident MDD is associated with higher CAD severity, whereas in patients with a history of MDD, a new MDD episode is not associated with the severity of CAD. However, this study did not include the full spectrum of ACS patients and the difference in CAD severity between incident and recurrent MDD patients was only significant at a p-level of 0.07.
The aim of the present study was to further investigate the existence of two subtypes - post-ACS patients with incident versus recurrent MDD - by comparing CAD severity in these two groups using angiography, a more proximal measure of CAD obtained by direct visualization of the coronary vessels. Based on previous studies, we hypothesized that incident MDD patients would have more severe CAD than would recurrent MDD patients, within 1 week post-ACS.
METHODS
Study Sample
Patients were enrolled from the Coronary Psychosocial Patient Evaluation Study (COPES), an observational cohort study designed to investigate the etiology and naturalistic course of depressive symptoms in the 3-month period after an ACS event. Patients were eligible for inclusion in COPES if they had been hospitalized for an ACS event (either acute myocardial infarction with or without ST-segment elevation or unstable angina) and scored between 0 and 4 (indicative of no depressive symptoms) or 10 or higher (at least mild depressive symptoms) on the Beck Depression Inventory (BDI) within 1 week after the index ACS event (Frasure-Smith et al., 1995; Lesperance et al., 2002). Additionally, they had to be enrolled at one of our site hospitals, Mount Sinai Hospital, where angiogram data were available.
Exclusion criteria were terminal non-cardiac illness, active suicidal or homicidal ideation, current psychotic disorder, current alcohol and/or substance abuse, insufficient proficiency in English or Spanish language, and cognitive impairment as indicated by a Mini-Mental State (Folstein et al., 1975) examination score less than 24 (for educational level of 8th grade or higher) or less than 17 (for educational level of 8th grade or lower). The study was carried out in accordance with the latest version of the Declaration of Helsinki. Informed consent of the participants was obtained after the study had been fully explained. The Institutional Review Board of the study hospital (Mount Sinai Hospital, New York, NY) approved the study.
A cohort of 88 patients was recruited between May 2003 and March 2004 at Mount Sinai Hospital, New York NY, who had angiogram and depression history data available (see Figure 1). Patients for whom these data were not available did not significantly differ from patients for whom these data were available on age, gender, ethnicity and depressive symptom severity (all p > .60).
Figure 1.
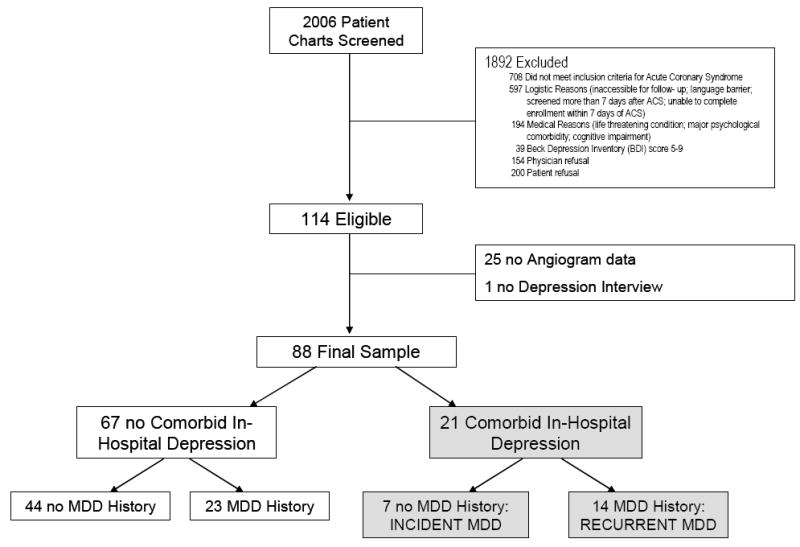
Participant Enrollment and Major Depressive Disorder Status within 1 Week of Admission for ACS
Note: MDD = Major Depressive Disorder
Assessment of Depression History and Concurrent Severity of Depressive Symptoms
All patients were interviewed with an abbreviated version of the Depression Interview and Structured Hamilton (Freedland et al., 2002). This version included the full clinical interview to assess the presence of major depressive disorder (MDD) and minor depression, according to the DSM-IV. To reduce patient burden, the Hamilton severity rating was omitted from the interview. Depression history was assessed after the current symptoms had been assessed, by asking the screening question: “Have you ever been depressed before?” If patients said yes or were uncertain, they were then probed further to estimate whether a patient had fulfilled DSM-IV criteria for a positive history of MDD. This was evaluated by assessing whether a reported depressive episode lasted at least 2 weeks, was sufficiently severe to affect functioning, and/or DSM diagnostic symptoms were likely present at that time.
Comorbid depressive symptom severity was assessed with the Beck Depression Inventory (BDI) (Beck, 1993). The BDI consists of 21 items describing cognitive-affective and somatic depression symptoms. Patients rated the extent to which each symptom had been present within the past 2 weeks on a 4-point scale (0-3).
Assessment of Coronary Artery Disease Stenosis Severity
For each patient, angiogram data were extracted from the Mount Sinai Hospital Electronic Data Repository. The selected angiogram for each patient was performed within one month of the depression interview, and was analyzed by a board-certified interventional cardiologist, blinded to depression status. The main coronary arteries analyzed included the left anterior descending, left circumflex and right coronary artery. Three measures were derived from coronary angiography: (1) number of vessels stenosed >50%, (2) presence of left main obstruction >50%, and (3) presence of three vessel disease (three main vessels >50% stenosed). A cut-off of greater than 50% vessel stenosis was used to define significant obstructive CAD based on standardized criteria (Ringqvist et al., 1983, Smith, 2005) and based on similar criteria in studies utilizing angiography (Rutledge et al, 2001).
CAD stenosis severity was determined as follows: 0 = no vessels significantly diseased (with > 50% stenosis); 1 = only one vessel diseased (without left main disease); 2 = two vessels diseased (without left main disease); 3 = three vessels diseased and/or left main disease.
Statistical Analyses
A hierarchical regression analysis was conducted to predict CAD severity. To test the hypothesis that the relationship between depression in hospital and CAD severity differed according to whether or not patients had a history of depression, an interaction term between MDD history and comorbid MDD for CAD severity was computed. Age, gender and ethnicity were entered as covariates in a first step, in a second step, comorbid MDD and MDD history were entered, and in a third step, the interaction term between the two. We used SPSS 12.0 statistical software (SPSS Inc, Chicago, IL). Two-tailed tests of significance were employed.
RESULTS
Of the 88 patients, 21 (23.9%) had comorbid MDD at the time of hospitalization for ACS. Of these, 14 (66.7%) had a history of MDD (recurrent MDD), and 7 (33.3%) experienced depression for the first time (incident MDD, see Figure 1).
Characteristics of incident vs. recurrent MDD patients are displayed in Table 1. The two patient groups did not differ on age, gender, race, ethnicity and severity of depressive symptoms (BDI score).
Table 1.
Baseline Characteristics of Patients with Incident vs. Recurrent Major Depressive Disorder
| Variable | Incident MDD
(n = 7) |
Recurrent MDD
(n = 14) |
P† |
|---|---|---|---|
| Age – yr | 53.57 ± 9.43 | 56.21 ± 11.23 | .60 |
| Female, no. (%) | 3 (42.9) | 9 (64.3) | .40 |
| White, no. (%) | 4 (57.1) | 7 (50) | .76 |
| Hispanic, no. (%) | 6 (85.7) | 7 (50) | .17 |
| BDI score | 26.43 ± 14.83 | 27.36 ± 10.37 | .87 |
Data are expressed as means ± SD or number (percentage).
Continuous variables were compared using F-test. Categorical variables were compared with χ2 statistics. Exact 2-sided significance levels are reported.
Note: MDD = Major Depressive Disorder; BDI = Beck Depression Inventory; CAD = Coronary Artery Disease
Results of a hierarchical regression analysis are displayed in Table 2. Neither comorbid MDD at time of hospitalization for ACS, nor history of MDD predicted CAD severity. The interaction between comorbid MDD and history of MDD, as predicted, was significant. Follow-up analyses showed that patients with first time in-hospital (incident) MDD had significantly more severe CAD compared to patients with recurrent MDD (Figure 2).
Table 2.
Hierarchical Regression Analysis Predicting Coronary Artery Disease Severity
| Predictor | B (SE) | ΔR2 | P |
|---|---|---|---|
| Step 1 | .03 | ||
| Age | 0.02 (0.01) | .08 | |
| Sex (1 = male; 2 = female) | 0.02 (0.22) | .94 | |
| Ethnicity (1 = non-Hispanic; 2 = Hispanic) | 0.08 (0.26) | .77 | |
| Step 2 | .00 | ||
| Comorbid, in-hospital MDD | 0.17 (0.11) | .12 | |
| History of MDD | 0.25 (0.26) | .33 | |
| Step 3 | .05 | ||
| Comorbid MDD × History of MDD | 0.28 (0.13) | .04 |
Note: MDD = Major Depressive Disorder
Figure 2.
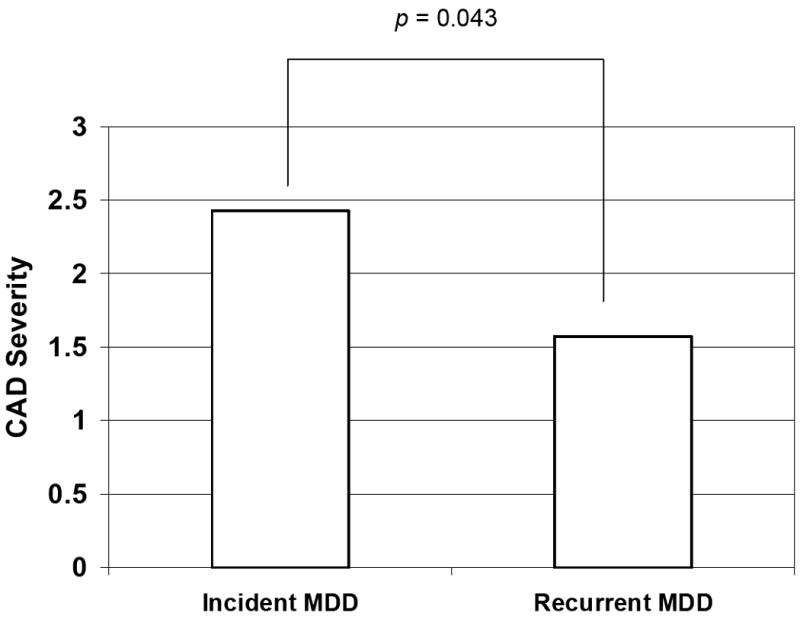
Coronary artery disease severity in patients with incident vs. recurrent in-hospital Major Depressive Disorder
Note: CAD severity ranges from 0 to 3: 0 = no vessels significantly diseased (with > 50% stenosis); 1 = only one vessel diseased (without left main disease); 2 = two vessels diseased (without left main disease); 3 = three vessels diseased and/or left main disease
Depressive symptom severity (assessed with the BDI) was positively associated with CAD severity only in patients with incident MDD, albeit at a non-significant p-level due to the small sample size (r = .38, p = .40). In contrast, there was clearly no relation between depressive symptom severity and CAD severity in patients with recurrent MDD (r = -.05, p = .88).
DISCUSSION
Our findings support our hypothesis that ACS patients with incident depression have significantly more severe CAD than those with recurrent depression. These results arise from direct visualization of the coronary vessels and support findings from one previous study which has shown more severe CAD in the incident depression subtype although only at trend level (Freedland, 1992). Even though the sample size in the present study was modest, the prevalence of the two depression types is comparable to that in other studies (Grace et al., 2005; de Jonge et al., 2006). The significant difference in CAD severity adds to mounting evidence that two subtypes exist in depressed ACS patients – patients with incident versus recurrent depression. The mechanisms underlying these differences must be explored in future studies.
One possible explanation for our results is that ACS patients without a history of depression have normal vulnerability to depression, but because their CAD or ACS event is more severe than those patients with past episodes of depression, they experience a first time reactive depression in response to the significant physiologic and psychological stress. A study by Spijkerman et al. (2005) demonstrated the important relationship between disease severity and development of depression in patients without a history of depression. They examined the relationship between MI severity and the development of new MDD over a period of one year in 468 post-MI patients who were not depressed at the time of the MI presentation. It was shown that several indirect measures of MI severity (revascularization during hospitalization, poorer left ventricular ejection fraction and arrhythmic events) were related to the onset of MDD during the first year after the MI in patients who had never had an MDD episode before (Spijkerman et al., 2005). In contrast, MI severity did not predict the recurrence of MDD during that year in patients who with a history of MDD.
Even though the severity of an MI is only poorly correlated with CAD severity as measured by angiogram, the above study provides interesting evidence that incident MDD can be triggered by underlying cardiac disease, whereas in patients with a lifetime history of MDD, disease severity is not a MDD trigger. Likely, in these patients, comorbid MDD have a different etiology. Recurrent depression in ACS patients more likely resembles depression seen in the general population. Common risk factors for depression in the general population such as lower educational level and higher neuroticism are also seen in non-incident post-MI depressed patients (De Jonge et al., 2006.) Unlike ACS patients with incident depression, individuals with recurrent depression may experience an exacerbation of a previously existing vulnerability which is triggered by the ACS. Therefore, the level of CAD/ACS severity may take on less significance in their depression onset than in the case of first-time depressed ACS patients.
Another tentative explanation for our finding that ACS patients with incident depression appear to have more advanced coronary vascular disease is that these patients may be more vulnerable to a certain type of depression termed vascular depression. A subset of depressive disorders that occurs for the first time in old age, vascular depression is considered a consequence of microvascular lesions secondary to atherosclerosis in subcortical and prefrontal regions within the brain. This theory has been supported by MRI evidence in patients with geriatric depression of a higher incidence of white matter hyperintensities, representing deep white matter lesions of vascular origin (Camus et al., 2004). Further support for the vascular depression subtype comes from a study by Rapp et al. which compared late-onset geriatric major depression to recurrent geriatric depression and found significantly more cardiovascular comorbidity (greater number of comorbid cardiovascular and cerebrovascular diagnoses) in the patients experiencing depression for the first time in their older age (Rapp et al., 2005). These findings suggest a relationship between depression that presents for the first time late in life and the degree of cardiovascular disease. Although a direct comparison cannot be drawn between the geriatric depression population and the incident MDD post-ACS population in our study, Rapp’s results suggest that a subtype of depression exists which is highly associated with greater extent of vascular disease. It is possible that the post-ACS patients in our study with incident depression and with more severe atherosclerotic coronary vessels concurrently have more severe vascular disease in the brain and are thus more prone to vascular depression. The ACS event may serve as the trigger for vascular depression onset. However, this theory is speculative at this point and it is entirely possible that vascular depression also exists in recurrent depression. Future research should first compare the prevalence of white matter hyperintensities in incident and recurrent depression within post-ACS patients. A question is whether there is a strong relationship between coronary vascular disease and similar vascular pathology in the brain, which could be answered by correlating CAD severity indicators, such as the one examined in this study, with the degree of white matter hyperintensities in the brain.
One way of indirectly exploring if the vascular depression hypothesis has any substantiation in our sample would have been to examine Mini-Mental-State Examination score differences among our incident and recurrent MDD patients. However, a limitation of our study was that these eligibility MMSE scores were not preserved, and so are not available for this exploratory analysis.
An important limitation in our study is that angiogram only measures visibly stenotic vessels. It is now known that ACS events such as unstable angina, acute myocardial infarction or sudden cardiac death can be caused by thrombotic occlusions overlying ruptured plaques that are not significantly stenotic (Virmani, 2000 and Naghavi, 2003). Instead these plaques undergo positive (“expansive” or “outward”) remodeling, a compensatory increase in the external elastic membrane as the plaque expands. This positive remodeling results in a minimal impingement of the plaque into the lumen, concealing the presence of substantial atherosclerotic disease on angiographic studies. Therefore, it is possible that our ACS patients with recurrent depression have greater atherosclerotic coronary disease than is immediately evident on angiogram.
Another possible limitation of our study is that depression history was assessed retrospectively by patient interview. Using the DISH, 37 patients out of 88 (42%) had a history of MDD. This prevalence rate is slightly higher than the range of published prevalence rates, but our population may be different from others in the literature given the greater number of Hispanic patients in our sample.
Our study adds to the growing evidence that two subtypes of depression exist within the post-ACS depressed population: first time or incident depression and recurrent depression. Recognition of these two groups has important implications for prognosis in post-ACS depression. Recent studies have shown that it is only incident depression that increases risk of poor cardiovascular outcome in post-ACS patients. Post-ACS patients with incident depression should therefore be identified so that appropriate attention and management can ensue. It is worth noting that there are two recent reports of female patient samples, one disease-free and one with suspected myocardial ischemia, in which a reported history of depression or treatment history for depression predicted coronary calcification or cardiac risk (Agatisa, 2005 and Rutlegde, 2006, respectively). These are obviously different patient samples than ours, and the results point to the possibility that the risks for ACS incidence are possibly different than those for recurrence of an ACS event. However, it remains clear that the characterization of subtypes of depression (eg incident vs recurrent) is an important distinction to better understand the cardiac risk of patients with these different depression patterns.
Finally, it may be beneficial to approach treatment differently in these two subtypes. The SADHART and CREATE trials of antidepressants in depressed cardiac patients both showed the response rates for drug versus placebo were greater in patients who had a prior history of MDD, whereas patients experiencing their first major depressive episode showed no difference between drug and placebo (Lesperance, 2007; Glassman, 2002). It remains unclear whether this lack of greater drug response compared to placebo in the incident depressed group represents a different etiology of that depression (such as depression reactive to coronary disease severity, or vascular depression), thus explaining resistance to traditional depression treatment. Another possibility is that incident depression may be characterized as a reactive depression to the cardiac event and therefore exhibits a more robust placebo response and higher likelihood of remitting spontaneously, thus narrowing the drug-placebo difference. Regardless, these subtypes should be identified so that optimal treatment may be tested.
Acknowledgments
Data collection and manuscript preparation were financially supported by grants HC-25197, HL-076857, and HL-04458 from the National Heart, Lung, and Blood Institute, Bethesda, Md.
Footnotes
Conflict of Interest: NONE
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agatisa PK, Matthews KA, Bromberger JT, Edmundowicz D, Chang YF, Sutton-Tyrrell K. Coronary and aortic calcification in women with a history of major depression. Archives of Internal Medicine. 2005;165:1229–1236. doi: 10.1001/archinte.165.11.1229. [DOI] [PubMed] [Google Scholar]
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a Risk Factor for Mortality in Patients With Coronary Heart Disease: A Meta-analysis. Psychosomatic Medicine. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Camus V, Kreahenbuhl H, Preisig M, Bula CJ, Waeber G. Geriatric depression and vascular diseases: what are the links? Journal of Affective Disorders. 2004;81:1–16. doi: 10.1016/j.jad.2003.08.003. [DOI] [PubMed] [Google Scholar]
- de Jonge P, van den Brink RHS, Spijkerman TA, Ormel J. Only Incident Depressive Episodes After Myocardial Infarction Are Associated With New Cardiovascular Events. Journal of the American College of Cardiology. 2006;48:2204–2208. doi: 10.1016/j.jacc.2006.06.077. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-Month Prognosis After Myocardial Infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- Freedland KE, Carney RM, Lustman PJ, Rich MW, Jaffe AS. Major depression in coronary artery disease patients with vs. without a prior history of depression. Psychosomatic Medicine. 1992;54:416–21. doi: 10.1097/00006842-199207000-00004. [DOI] [PubMed] [Google Scholar]
- Freedland KE, Skala JA, Carney RM, Raczynski JM, Taylor CB, Mendes de Leon CF, Ironson G, Youngblood ME, Krishnan KR, Veith RC. The Depression Interview and Structured Hamilton (DISH): rationale, development, characteristics, and clinical validity. Psychosomatic Medicine. 2002;64:897–905. doi: 10.1097/01.psy.0000028826.64279.29. [DOI] [PubMed] [Google Scholar]
- Glassman AH, O’Connor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. Journal of the American Medical Association. 2002;288:701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- Grace SL, Abbey SE, Kapral MK, Fang J, Nolan RP, Stewart DE. Effect of Depression on Five-Year Mortality After an Acute Coronary Syndrome. The American Journal of Cardiology. 2005;96:1179–1185. doi: 10.1016/j.amjcard.2005.06.052. [DOI] [PubMed] [Google Scholar]
- Ladwig KH, Kieser M, Konig J, Breithardt G, Borggrefe M. Affective disorders and survival after acute myocardial infarction. Results from the post-infarction late potential study. European Heart Journal. 1991;12:959–64. [PubMed] [Google Scholar]
- Lesperance F, Frasure-Smith N, Talajic M. Major depression before and after myocardial infarction: its nature and consequences. Psychosomatic Medicine. 1996;58:99–110. doi: 10.1097/00006842-199603000-00001. [DOI] [PubMed] [Google Scholar]
- Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-Year Risk of Cardiac Mortality in Relation to Initial Severity and One-Year Changes in Depression Symptoms After Myocardial Infarction. Circulation. 2002;105:1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- Lesperance F, Frasure-Smith N, Koszycki D, et al. The CREATE Infestigators. Effects of citalopram ant interpersonal psychotherapy on depression in patients with coronary artery disease. Journal of the American Medical Association. 2007;297:367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- Naghavi M, et al. From Vulnerable Plaque to Vulnerable Patient: Part I. Circulation. 2003;108:1664–1672. doi: 10.1161/01.CIR.0000087480.94275.97. [DOI] [PubMed] [Google Scholar]
- Rapp MA, Dahlman K, Sano M, Grossman HT, Haroutunian V, Gorman JM. Neuropsychological Differences Between Late-Onset and Recurrent Geriatric Major Depression. American Journal of Psychiatry. 2005;162:691–698. doi: 10.1176/appi.ajp.162.4.691. [DOI] [PubMed] [Google Scholar]
- Ringqvist I, Fisher LD, Mock M, et al. Prognostic value of angiographic indices of coronary artery disease from the Coronary Artery Surgery Study (CASS) J Clin Invest. 1983;71:1854–66. doi: 10.1172/JCI110941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumsfeld JS, Magid DJ, Plomondon ME, Sales AE, Grunwald GK, Every NR, Spertus JA. History of depression, angina, and quality of life after acute coronary syndromes. American Heart Journal. 2003;145:493–9. doi: 10.1067/mhj.2003.177. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, Reichek N, Rogers WJ, Merz NB, Sopko G, Cornell CE, Sharaf B, Matthews KA. History of Anxiety Disorders Is Associated With a Decreased Likelihood of Angiographic Coronary Artery Disease in Women With Chest Pain: The WISE Study. Journal of the American College of Cardiology. 2001;37:780–785. doi: 10.1016/s0735-1097(00)01163-3. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Olson MB, Reis SE, Owns J, Kelsey SF, Pepine C, Mankad S, Rogers WJ, Merz NB, Sopko G, Cornell CE, Sharaf B, Matthew KA, Vaccarino V. Depression Symptom Severity and Reported Treatment History Combine to Predict Cardiac Risk in Women with Suspected Myocardial Ischemia. Archives of General Psychiatry. 2006;63:874–880. doi: 10.1001/archpsyc.63.8.874. [DOI] [PubMed] [Google Scholar]
- Smith Sidney C., Jr . ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention. American College of Cardiology Foundation and the American Heart Association, Inc; 2005. [Google Scholar]
- Spijkerman TA, de Jonge P, van den Brink RH, Jansen JH, May JF, Crijns HJ, Ormel J. Depression following myocardial infarction: first-ever versus ongoing and recurrent episodes. General Hospital Psychiatry. 2005;27:411–17. doi: 10.1016/j.genhosppsych.2005.05.007. [DOI] [PubMed] [Google Scholar]
- Strik JJ, Lousberg R, Cheriex EC, Honig A. One year cumulative incidence of depression following myocardial infarction and impact on cardiac outcome. Journal of Psychosomatic Research. 2004;56:59–66. doi: 10.1016/S0022-3999(03)00380-5. [DOI] [PubMed] [Google Scholar]
- Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. Journal of General Internal Medicine. 2006;21:30–8. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, van den Brink RH, van den Berg MP. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosomatic Medicine. 2004;66:814–22. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from Sudden Coronary Death. Arteriosclerosis, thrombosis, and vascular biology. 2000;20:1262–1275. doi: 10.1161/01.atv.20.5.1262. [DOI] [PubMed] [Google Scholar]


